Abstract
Objectives
To compare the mortality rate in regulated and unregulated facilities, controlling for confounding variables, and investigate the effect of care quality on residents' length of survival.
Data Sources/Study Setting
At baseline, subjects were assessed in their living environment with respect to their functional autonomy, cognitive abilities, and quality of care. Vital status, disease-related information, and hospitalization data were retrieved three years later from the subjects' medical files.
Study Design
A three-year follow-up study of 299 residents from 88 long-term care facilities located in the province of Quebec, Canada. The effect of regulatory status and quality of care on length of survival was investigated by means of multivariable Cox proportional hazards regression models, from both traditional and competing risks perspectives.
Principal Findings
Controlling for age, comorbidity, and baseline functional abilities, a resident's length of survival is not significantly influenced by the regulatory status of the facility in which he or she lived at baseline. However, residents with poor quality ratings at baseline had shorter survival times than those provided with good care. Median survival was 28 months among residents classified as receiving inadequate care compared to 41 months for those adequately cared for (p = 0.0217).
Conclusions
The study suggests that quality of care has a much stronger influence on resident outcomes than regulation per se. This finding underscores the relevance of testing innovative interventions aimed at improving the quality of care provided in long-term care facilities, regardless of their regulatory status.
Keywords: Regulatory status, quality of care, mortality, long-term care, aged
As the population ages, growing numbers of older adults require long-term care to overcome their disabilities and impairments. The vast majority of these individuals would prefer to remain in the community with the help of their family and support from home care services. However, as impairment levels and care needs increase, many elderly are compelled to leave their homes and move into residential care facilities. The quality of care provided in these homes has been a major concern for a number of years. In response to highly publicized cases of inadequate care in nursing homes, several countries introduced legislative changes in regulations governing the long-term care industry and increased their monitoring of the care provided (Kane 1988; Hunt and Uys 1990; Braithwaite et al. 1992; Shapiro and Tate 1995).
While evidence regarding the positive effects of these changes was starting to accrue (AGS Clinical Practice Committee 2000; Berlowitz et al. 2000), governments were faced with a new challenge: reducing health care expenditures devoted to the care of the elderly. Pressure to contain costs led many jurisdictions to limit the use of publicly subsidized long-term beds to those with high-skill needs by restricting their availability and tightening eligibility criteria (Doty 1993). These developments, coupled with an unprecedented demand for long-term beds, have greatly encouraged the proliferation of unregulated residential care facilities (Goodman, Pynoos, and Stevenson 1988; Baggett and Adler 1990; Eckert and Lyon 1991).
By definition, unregulated homes are not subject to government control, which raises the issue of the quality of care they provide (Shapiro 1999). Recently, we conducted a study comparing regulated and unregulated facilities with regard to the level of disability of the residents and the quality of their care. The study was conducted in the province of Quebec, Canada, where unregulated facilities house 60 percent of the dependent older population. In Quebec, regulation sets minimum staffing levels and safety requirements. Through periodic survey inspections, the province measures compliance with the requirements and specifies actions to be taken when problems are identified. By contrast, unregulated homes will only be inspected when a resident or family member launches a formal complaint.
Findings from the study are described in detail elsewhere (Bravo et al. 1998;, Bravo Dubois et al. 1999). In short, unregulated homes were found to care for a population with considerable functional and cognitive impairments. In addition, more than 25 percent of the facilities were judged to experience major difficulties in responding promptly and adequately to the needs of their residents, a situation attributed in part to a lack of qualified and experienced care providers (Bravo, De Wals et al. 1999).
Our study provided some insight into the situation that prevails in unregulated homes. However, results were limited by the cross-sectional design of the study that precludes any statement regarding the effect of regulatory status and quality of care on resident outcomes. In its landmark report, the Institute of Medicine (1986) stressed the importance of an outcome-oriented approach in assessing the effect of the quality of long-term care. Yet few studies have prospectively examined the links between regulatory status, care quality, and patient outcome. To partially fill this void, we added a longitudinal dimension to our previous study for the two-fold purpose of (1) comparing the adjusted mortality rate in regulated and unregulated facilities, and (2) investigating the effect of care quality on residents' length of survival.
Methods
Study Population
Initiated in September 1996, the baseline study involved 301 residents from 88 facilities (36 regulated, 52 unregulated) selected according to a stratified two-stage random sampling scheme. The study was restricted to individuals aged 65 and older who experienced some difficulties with at least two activities of daily living and had been living in a facility for at least three months. The number of residents selected from a given facility varied with its size and ranged from 2 in those housing less than 10 residents to 10 in those caring for more than 60 residents. All facility managers elected to take part in the study, as did 96 percent of the sampled residents.
Baseline Data Collection and Instruments
Baseline data were collected by experienced nurses and social workers who gathered sociodemographic information on the residents, measured their level of functional and cognitive impairment, and assessed the quality of their care. Functional status was assessed with the revised version of the Functional Autonomy Measurement System (SMAF [Système de Mesure de l'Autonomie Fonctionelle]) (Hébert, Carrier, and Bilodeau 1988), and cognitive abilities with the Modified Mini-Mental State (3MS) examination (Teng and Chui 1987). The SMAF evaluates the subject's ability to accomplish 29 functions covering five sectors of activity: activities of daily living, mobility, communication, mental functions, and instrumental activities of daily living. Each function is rated on an ordinal scale ranging from 0 (complete autonomy) to 3 (total dependency) for a maximum score of 87. The 3MS is a revised version of Folstein's MMSE (Folstein, Folstein, and McHugh 1975). It comprises 15 items assessing orientation to place and time, attention, memory, language, and visuographic abilities. Total scores range from 0 (worst) to 100 (best).
Care quality was measured with the QUALCARE Scale, a validated multidimensional instrument comprising 54 items that assess care in six areas: environmental, physical, medical management, psychosocial, human rights, and financial (Phillips, Morrison, and Chae 1990a; 1990b; Bravo et al. 1995). Each item is rated on a five-point scale, with one representing best possible care and five the worst possible care, taking into account the resident's health care needs. Averaging the 54 ratings leads to a global quality score specific to each resident.
Follow-up
Three years after the baseline study, facility managers were recontacted to establish the whereabouts of their residents and their vital status. Subjects were then classified into one of four categories: deceased in the baseline facility, deceased after a transfer to another facility, still living in the baseline facility, or living in a new facility. In the context of the Canadian health care system, older adults entering a residential care facility rarely return home. They may however move to another facility following an increase in their health care needs.
The exact date of death from any cause for subjects who had died since the baseline assessment was retrieved from the subjects' medical records. Medical files were reviewed for two other purposes: first, to collect hospitalization data with the objective of describing the utilization of public acute care services by the residents; and second, to retrieve disease-related information suspected of altering the risk of mortality. The Charlson Comorbidity Index (Bravo et al. 2002) was used for that latter purpose. Data were collected retrospectively, over a 3.5-year window, starting six months prior to the subject's baseline assessment.
The baseline and follow-up components of the study were both approved by the Ethics Review Board of the Sherbrooke University Geriatric Institute. Access to a subject's medical file was preceded by an informed consent signed by the subject or his or her legal guardian or advocate.
Statistical Analyses
Cox proportional hazards (PH) regression models (Collett 1994) were constructed to address the two objectives of the current study. The time origin was set at the date of the baseline assessment. Survival was measured in months from the time origin to the date of death, the date of transfer to a new facility, or the end of the study. Subjects who were still alive at three years were treated as censored observations. Residents who moved to a new facility were censored at the date of transfer, except those who died less than three months following their relocation.
An underlying assumption of survival analysis is that censoring is noninformative, that it is independent of true survival times (Collett 1994). Yet, one would expect many residents to be transferred just prior to death, following a worsening of their health condition. This would imply that censoring is informative, being linked to the outcome under study. In this instance, Gelman et al. (1990) recommend reanalyzing the data under a competing risks perspective. This entails analyzing time to the first event (transfer or death), restricting censoring to subjects who are still living in the same facility at the end of follow-up. One then proceeds to compare the observed percentage of residents who experienced each competing event by means of a polychotomous logistic regression (Hosmer and Lemeshow 1989). Hence, all analyses were conducted in duplicates, first from a traditional approach, and second adopting a competing risks perspective. All reported p values are two-sided. Data management and analyses were performed using SUDAAN software, release 7.5 (Research Triangle Institute 1997), which takes the sampling design into account.
Results
Only two subjects could not be located three years after their enrollment in the study. Both were from an unregulated facility. The baseline characteristics of the 299 remaining subjects are presented in Table 1, by regulatory status. Subjects were predominantly female, older than 80 years of age, widowed, with less than 8 years of education. Length of residency at baseline ranged from 3 months to 36 years (median: 3 years). Subjects suffered from 0 to 9 medical conditions. The most prevalent condition was dementia (46.8 percent), closely followed by urinary problems (44.1 percent) and chronic pulmonary disease (30.7 percent). Residents were also quite impaired at baseline, both cognitively and functionally, especially those living in a regulated facility. As shown in Table 1, the average quality rating assigned to residents from unregulated homes was slightly worse than that attributed to subjects living in regulated facilities. The difference however was not statistically significant.
Table 1.
Baseline Characteristics of the Subjects, Stratified by the Regulatory Status of Their Facility*
| Regulated Facilities N=124 | Unregulated Facilities N=175 | p value | |
|---|---|---|---|
| Age (in years) | 84.76±0.51 | 83.17±0.70 | 0.0696 |
| Female gender | 67.3% | 67.6% | 0.9694 |
| Marital status | |||
| Single | 20.0% | 15.4% | |
| Married | 18.6% | 16.1% | |
| Widowed | 52.4% | 62.0% | |
| Divorced/separated | 9.0% | 6.5% | 0.3866 |
| Years of schooling | |||
| None | 3.5% | 3.8% | |
| 7 or less | 68.2% | 60.8% | |
| 8 to 12 | 20.9% | 24.2% | |
| 13 or more | 7.4% | 11.2% | 0.6625 |
| Length of residency (in years) | 4.93±0.46 | 3.78±0.54 | 0.1109 |
| Comorbidity Index (a higher score implies greater comorbidity) | 2.38±0.15 (n = 121) | 2.81±0.21 (n = 170) | 0.1051 |
| Cognitive functioning (3MS score from 0 [worst] to 100 [best]) | 37.57±5.09 (n = 115) | 62.36±1.58 (n = 164) | <0.0001 |
| Functional autonomy (SMAF score from 0 [complete autonomy] to 87 [total dependency]) | 49.09±2.32 | 29.62±1.03 | <0.0001 |
| Global quality rating (QUALCARE score from 1 [best possible care] to 5 [worst possible care]) | 1.47±0.09 | 1.61±0.06 | 0.1830 |
Values are weighted percentages or weighted means±standard errors.
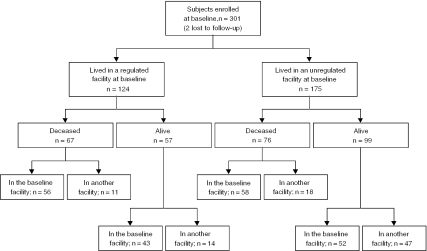
Vital status information is provided in Figure 1. Sixty-seven residents (59.8 percent) from regulated facilities died during the follow-up period, compared to 76 (43.3 percent) from their unregulated counterparts. In both cases, the majority of deaths occurred in the baseline facility. Most subjects who died following a relocation had been transferred to a regulated facility. Among the subjects alive three years after enrolling in the study, 88.6 percent of those sampled from a regulated facility were still living in the same facility relative to 53.7 percent for their unregulated counterparts. Most transfers of subjects still alive at the end of follow-up were to a regulated facility and were motivated by an increase in the residents' health care needs.
Figure 1.
Flow chart describing the subjects' vital status three years after enrollment. Deaths occurring less than three months following a transfer were treated as if they had occurred in the baseline facility
Hospitalization data extracted from the subjects' medical files are summarized in Table 2. Residents from unregulated facilities were hospitalized much more frequently and for longer periods of time than subjects residing in regulated facilities. Sixty-seven percent of the residents from unregulated homes were hospitalized at least once for acute care, with 1 in 10 residents admitted more than 10 times. Length of hospitalization exceeded two months in 40 percent of the subjects sampled from unregulated facilities. As unregulated homes care for a less impaired population, these data likely reflect their lack of human and material resources to address the needs of a resident whose health condition deteriorates. In addition to reducing residents' quality of life, repeated admissions for acute care over long periods of time entail considerable cost to the health care system.
Table 2.
Hospitalization Data Retrieved from Subjects' Medical Records
| Regulated Facilities n=124 | Unregulated Facilities n=175 | p value | |
|---|---|---|---|
| Number of hospitalizations for acute care over the 3-year follow-up period* | |||
| 0 | 67.8% | 33.4% | |
| (0, 5) | 21.4% | 45.7% | |
| (5, 10) | 4.5% | 10.1% | |
| more than 10 | 6.2% | 10.8% | <0.0001 |
| Average number of days hospitalized for acute care over the 3-year follow-up period† | |||
| (1, 20) | 56.5% | 32.1% | |
| (20, 30) | 1.7% | 10.0% | |
| (30, 60) | 16.4% | 17.5% | |
| (60, 120) | 19.7% | 12.0% | |
| 120 or more | 5.7% | 28.4% | <0.0001 |
Defined as the number of hospitalizations while living in the baseline facility divided by the length of stay in the baseline facility and multiplied by 36 months.
Defined as the number of days hospitalized while living in the baseline facility divided by the length of stay in the baseline facility and multiplied by 36 months.
Results from univariate survival analyses are shown in Table 3, for the two analytical approaches outlined above. As expected, older age, more comorbidities, and greater cognitive and functional impairments were all found to increase the risk of death, irrespective of the analytical perspective. Baseline quality ratings are also strong predictors of event times, but not regulatory status.
Table 3.
Results from Univariate Cox PH Regression Analyses Linking Potentially Confounding Variables, Quality of Care and Regulatory Status to Mortality and Time to First Event (Transfer or Death Whichever Occurred First)
| Traditional Approach, with Time to Death as the Outcome* | Competing Risks Approach, with Time to First Event as the Outcome† | |
|---|---|---|
| Main effects‡ | ||
| Age | 1.07 (p = 0.0003) | 1.04 (p = 0.0114) |
| Comorbidity index (a higher score implies greater comorbidity) | 1.29 (p <0.0001) | 1.22 (p <0.0001) |
| Cognitive functioning (3MS score from 0 [worst] to 100 [best]) | 0.99 (p = 0.0024) | 0.99 (p = 0.0298) |
| Functional autonomy (SMAF score from 0 [complete autonomy] to 87 [total dependency]) | 1.02 (p <0.0001) | 1.01 (p = 0.0018) |
| Global quality rating (QUALCARE score from 1 [best possible care] to 5 [worst possible care]) | 1.65 (p = 0.0018) | 1.63 (p = 0.0008) |
| Regulatory status (coded 1 for regulated and 2 for unregulated) | 1.53 (p = 0.1059) | 0.85 (p = 0.4717) |
| Interactions of regulatory status (RS) with main effects§ | ||
| RS * Age | 0.6576 | 0.9517 |
| RS * Comorbidity index | 0.9887 | 0.4389 |
| RS * Cognitive functioning | 0.4628 | 0.0563 |
| RS * Functional autonomy | 0.1672 | 0.0297 |
Subjects censored at the time of transfer when applicable.
Censoring limited to subjects who were still living in the same facility at follow-up.
Values are unadjusted hazard ratios, with p value from the Wald test in parentheses.
p value from the Wald test.
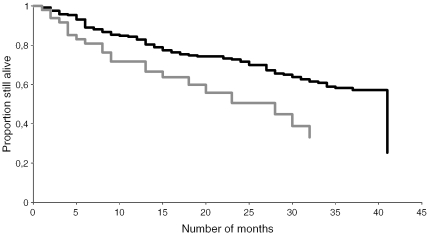
Final results from the multivariable survival analyses are shown in Table 4, first for regulatory status and second for care quality. Both analytical strategies led to similar results despite targeting a slightly different outcome. Focusing first on the traditional approach, regulatory status does not emerge as a significant predictor of mortality after adjusting for risk factors unevenly distributed between facilities. However, the global quality rating attributed to a resident at baseline appears to be a strong predictor of his or her risk of death, controlling for cognitive impairments, the only resident characteristic associated with both quality scores and outcomes. Figure 2 illustrates the effect of care quality on survival, combining residents from regulated and unregulated facilities. Median survival was 28 months among residents classified as receiving inadequate care compared to 41 months for those adequately cared for (p = 0.0217).
Table 4.
Results from Multivariable Cox PH Regression Analyses Linking Regulatory Status and Quality of Care to Mortality and Time to First Event (Transfer or Death Whichever Occurred First)
| Traditional Approach, with Time to Death as the Outcome* | Competing Risks Approach, with Time to First Event as the Outcome† | |
|---|---|---|
| Effect of regulatory status, [coded 1 for regulated and 2 for unregulated] controlling for | 1.08 (0.48, 2.42)‡ | 1.98 (0.97, 4.07) |
| Age | 1.07 (1.03, 1.11) | 1.04 (1.00, 1.07) |
| Comorbidity (a higher score implies greater comorbidity) | 1.34 (1.25, 1.45) | 1.23 (1.16, 1.30) |
| Functional autonomy (SMAF score from 0 [complete autonomy] to 87 [total dependency]) | 1.02 (1.00, 1.04) | 1.02 (1.01, 1.04) |
| Effect of care quality, (QUALCARE score from 1 [best possible care] to 5 [worst possible care]) controlling for | 1.74 (1.29, 2.34) | 1.77 (1.31, 2.40) |
| Cognitive functioning (3MS score from 0 [worst] to 100 [best]) | 0.99 (0.98, 1.00) | 0.99 (0.99, 1.00) |
Subjects censored at the time of transfer when applicable.
Censoring limited to subjects who were still living in the same facility at follow-up.
Values are adjusted hazard ratios, with 95% confidence intervals in parentheses.
Figure 2.
Adjusted Kaplan-Meier curves comparing time to death for subjects receiving adequate (QUALCARE score ≤2, black line) or inadequate (QUALCARE score >2, gray line) care. The analysis was based on the traditional approach, with residents from regulated and unregulated facilities combined. Curves depart significantly from one another according to the Wald test (p = 0.0217)
Similar results are obtained when analyzing the data from a competing risks approach. In particular, time to first event was found to be influenced by the quality rating assigned to a resident at baseline, but not by the regulatory status of the facility, although a slightly larger sample may have rendered the result statistically significant. Following Gelman et al.'s (1990) recommendation, we proceeded to identify which of the competing events (transfer or death) was influenced by a resident's quality rating. Results indicate that poor quality of care increases a resident's risk of death (p = 0.0014) as well as his or her risk of transfer (p = 0.0203). Living in an unregulated facility also increases a resident's risk of transfer (p = 0.0022) but not his or her risk of death (p = 0.6964). Hence, had we used a larger sample and found a significant effect of regulatory status with the competing risks approach, the conclusion would have been that regulatory status affects the probability that a resident will be transferred within the next three years but not the probability of his or her dying. In other words, both analytical approaches led to the same conclusion regarding the effect of regulatory status on mortality, that is, a lack of direct effect.
Discussion
This study investigated the influence of two potential risk factors for mortality in residential care facilities: regulatory status and care quality. Our results indicate that the latter is much more influential that the former, with poor quality of care shortening time to death by more than a year, irrespective of the regulatory status of the facility. This finding lends support to the contention expressed by the Institute of Medicine (1986) that regulation, by itself, does not ensure high-quality care.
To our knowledge, only one other study had among its objectives to compare regulated and unregulated facilities on outcome measures of quality (Lyon 1997). The study was restricted to small board-and-care homes in Maryland that serve a low-income, mentally ill population. Two outcomes were examined: changes in residents' health status over a three-year follow-up period and length of stay in the facility. Neither was found to vary across regulatory status. From these results, Lyon concluded that participation in a regulatory program may not ensure adequate care for vulnerable and dependent adults. This conclusion is congruent with ours, although it applies to a different population and was derived from investigating different care outcomes.
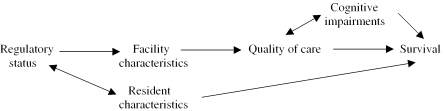
Yet, intuitively, one would expect regulation to impact on survival through improvement in care quality. This would imply the following conceptual model: regulatory status→quality of care→survival, which parallels Donabedian's well-known paradigm linking structure, process, and outcomes of care. Our results partially support this model. We have shown that quality of care does impact survival (cf. Table 3 and 4), a result concordant with that of Braun (1991). In our sample, the relationship between quality of care and survival was influenced by the resident's level of cognitive functioning. Residents with lower cognitive abilities had shorter survival times but also tended to receive care of lesser quality. This latter result was reported previously (Bravo et al. 1999b), following a multilevel analysis investigating resident- and facility-correlates of care quality. Cognitive functioning was the only resident attribute associated with the QUALCARE Scale. In that paper, quality of care was also shown to depend on a number of facility attributes such as the qualification of the staff and the number of external collaborators. Yet unregulated facilities are known to lack qualified care providers and to be quite isolated (Bravo et al. 1998). This suggests that regulatory status may not influence quality of care directly, but rather indirectly through its effect on other facility characteristics. Combining these results with the fact that unregulated homes tend to care for a less impaired population leads to the following revised yet more complex model:
Future studies should aim at testing this model in its entirety, using more sophisticated approaches such as structural equation modeling (Bollen 1989). Meanwhile, it is worth emphasizing the strengths and limitations of the current study as they impact the validity of the postulated model.
Strengths and Limitations
Our study has several strengths. First, quality assessments were based on direct observations of the residents, rather than on records kept by the facilities. Second, the way we assess quality of care does not require subjects to be able to express themselves. Hence, cognitively impaired residents—who account for almost 50 percent of the residential care population—do not have to be excluded. Third, the QUALCARE Scale taps several dimensions judged essential in assessing the quality of long-term care, such as respect for human rights, quality of caregivers' interactions, and safety of the premises (Rantz et al. 1998). The present study also has a number of methodological strengths, including its longitudinal design and high rate of follow-up. Efforts to adjust for differences in case mix between regulated and unregulated facilities constitute another methodological strength (Mukamel and Brower 1998), as does the decision to analyze the data from more than one perspective.
The current investigation has limitations as well. The first has to do with the applicability of its results. Because regulatory mechanisms vary from country to country, it remains to be seen whether our findings apply to other jurisdictions, especially those pertaining to the impact of regulatory status on resident outcomes. A second limitation of the study is that it focused attention on a unique outcome: mortality. Length of survival is an important outcome of health care services, especially in long-term care where the elderly are most vulnerable and dependent (Phillips 1991). However, a person's time of death is influenced to varying degrees by the natural course of aging and disease progression, two factors that are largely beyond the control of a residential care facility (Porell and Caro 1998). Other outcomes should thus be investigated as well, such as the rate of decline in residents' functional and cognitive abilities (Kane 1988; Rosen et al. 1999). Lastly, although this study has broadened our understanding of the complex relationships between regulatory status, quality of care, and patient outcomes, it is unlikely to have a direct effect on the quality of care currently provided to older adults. However, the finding that quality of care may have a stronger influence on resident outcomes than regulation per se suggests that future research efforts should be directed toward testing innovative interventions designed to enhance care quality rather than experimenting with new ways to enforce strict regulatory standards. Such a study is currently underway.
References
- AGS Clinical Practice Committee. “Regulation and Quality of Care Standards in Nursing Facilities.”. Journal of the American Geriatrics Society. 2000;48:1519–20. [PubMed] [Google Scholar]
- Baggett S, Adler S. “Regulating the Residential Care Industry: Historical Precedents and Current Dilemmas.”. Journal of Aging and Social Policy. 1990;2(1):15–32. [Google Scholar]
- Berlowitz DR, Bezerra HQ, Brandeis GH, Kader B, Anderson JJ. “Are We Improving the Quality of Nursing Home Care: The Case of Pressure Ulcers.”. Journal of the American Geriatrics Society. 2000;48:59–62. doi: 10.1111/j.1532-5415.2000.tb03029.x. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural Equations with Latent Variables. New York: Wiley; 1989. [Google Scholar]
- Braithwaite V, Braithwaite J, Gibson D, Makkai T. “Progress in Assessing the Quality of Australian Nursing Home Care.”. Australian Journal of Public Health. 1992;16(1):89–97. doi: 10.1111/j.1753-6405.1992.tb00032.x. [DOI] [PubMed] [Google Scholar]
- Braun BI. “The Effect of Nursing Home Quality on Patient Outcome.”. Journal of the American Geriatrics Society. 1991;39:329–38. doi: 10.1111/j.1532-5415.1991.tb02896.x. [DOI] [PubMed] [Google Scholar]
- Bravo G, Charpentier M, Dubois MF, De Wals P, Émond A. “Profile of Residents in Unlicensed Homes for the Aged in the Eastern Townships of Quebec.”. Canadian Medical Association Journal. 1998;159(2):143–8. [PMC free article] [PubMed] [Google Scholar]
- Bravo G, De Wals P, Dubois MF, Charpentier M. “Correlates of Care Quality in Long-Term Care Facilities: A Multilevel Analysis.”. Journal of Gerontology: Psychological Sciences. 1999;54B(3):P180–8. doi: 10.1093/geronb/54b.3.p180. [DOI] [PubMed] [Google Scholar]
- Bravo G, Dubois MF, Charpentier M, De Wals P, Émond A. “Quality of Care in Unlicensed Homes for the Aged in the Eastern Townships of Quebec.”. Canadian Medical Association Journal. 1999;160(10):1441–5. [PMC free article] [PubMed] [Google Scholar]
- Bravo G, Dubois MF, Hébert R, De Wals P, Messier L. “A Prospective Evaluation of the Charlson Comorbidity Index for Use in Long-Term Care Patients.”. Journal of the American Geriatrics Society. 2002;50:740–5. doi: 10.1046/j.1532-5415.2002.50172.x. [DOI] [PubMed] [Google Scholar]
- Bravo G, Girouard D, Gosselin S, Archambault C, Dubois MF. “Further Validation of the QUALCARE Scale.”. Journal of Elder Abuse and Neglect. 1995;7(4):29–48. [Google Scholar]
- Collett D. Modelling Survival Data in Medical Research. London: Chapman and Hall; 1994. [Google Scholar]
- Doty P. “International Long-Term Care: A Demographic Economic and Policy Overview.”. Journal of Cross-Cultural Gerontology. 1993;8:447–61. doi: 10.1007/BF00972571. [DOI] [PubMed] [Google Scholar]
- Eckert JK, Lyon SM. “Regulation of the Board-and-Care Homes: Research to Guide Policy.”. Journal of Aging and Social Policy. 1991;3(1/2):147–62. doi: 10.1300/J031v03n01_11. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State. A Practical Method for Grading the Cognitive State of Patients for the Clinician.”. Journal of Psychiatric Research. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gelman R, Gelber R, Henderson C, Coleman CN, Harris JR. “Improved Methodology for Analyzing Local and Distant Recurrence.”. Journal of Clinical Oncology. 1990;8(3):548–55. doi: 10.1200/JCO.1990.8.3.548. [DOI] [PubMed] [Google Scholar]
- Goodman CC, Pynoos J, Stevenson LM. “Board and Care Cast-Aways: Older Adults Outside the Long-Term Care Continuum.”. Social Work in Health Care. 1988;13:65–79. doi: 10.1300/j010v13n04_06. [DOI] [PubMed] [Google Scholar]
- Hébert R, Carrier R, Bilodeau A. “The Functional Autonomy Measurement System (SMAF): Description and Validation of an Instrument for the Measurement of Handicaps.”. Age and Ageing. 1988;17:293–302. doi: 10.1093/ageing/17.5.293. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. New York: Wiley; 1989. [Google Scholar]
- Hunt NB, Uys LR. “The Quality of Nursing Care of the Frail Aged in Selected Institutions in Eastern Cape and Natal.”. Curationis. 1990;13(1&2):21–3. doi: 10.4102/curationis.v13i1/2.283. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Improving the Quality of Care in Nursing Homes. Washington DC: National Academy of Sciences Press; 1986. [Google Scholar]
- Kane RA. “Assessing Quality in Nursing Homes.”. Clinics in Geriatric Medicine. 1988;4(3):655–66. [PubMed] [Google Scholar]
- Lyon SM. “Impact of Regulation and Financing on Small Board-and-Care Homes in Maryland.”. Journal of Aging and Social Policy. 1997;9(2):37–50. doi: 10.1300/J031v09n02_04. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Brower CA. “The Influence of Risk Adjustment Methods on Conclusions about Quality of Care in Nursing Homes Based on Outcome Measures.”. Gerontologist. 1988;38(6):695–703. doi: 10.1093/geront/38.6.695. [DOI] [PubMed] [Google Scholar]
- Phillips CJ. “Developing a Method of Assessing Quality of Care in Nursing Homes Using Key Indicators and Population Norms.”. Journal of Aging and Health. 1991;3(3):407–22. doi: 10.1177/089826439100300306. [DOI] [PubMed] [Google Scholar]
- Phillips LR, Morrison EF, Chae YM. “The QUALCARE Scale: Developing an Instrument to Measure Quality of Home Care.”. International Journal of Nursing Studies. 1990a;27(1):61–75. doi: 10.1016/0020-7489(90)90024-d. [DOI] [PubMed] [Google Scholar]
- Phillips LR, Morrison EF, Chae YM. “The QUALCARE Scale: Testing of a Measurement Instrument for Clinical Practice.”. International Journal of Nursing Studies. 1990b;27(1):77–91. doi: 10.1016/0020-7489(90)90025-e. [DOI] [PubMed] [Google Scholar]
- Porell F, Caro FG. “Facility-Level Outcome Performance Measures for Nursing Homes.”. Gerontologist. 1998;38(6):665–83. doi: 10.1093/geront/38.6.665. [DOI] [PubMed] [Google Scholar]
- Rantz MJ, Mehr DR, Popejoy L, Swygart-Stauffacher M, Hicks LL, Grando V, Conn VS, Porter R, Scott J, Maas M. “Nursing Home Care Quality: A Multidimensional Theoretical Model.”. Journal of Nursing Care Quality. 1998;12(3):30–46. doi: 10.1097/00001786-199802000-00007. [DOI] [PubMed] [Google Scholar]
- Research Triangle Institute. SUDAAN (release 7.5) statistical software. Research Triangle Park, NC: Research Triangle Institute; 1997. [Google Scholar]
- Rosen AK, Berlowitz DR, Anderson JJ, Ash AS, Kazis LE, Moskowitz MA. “Functional Status Outcomes for Assessment of Quality in Long-Term Care.”. International Journal for Quality in Health Care. 1999;11(1):37–46. doi: 10.1093/intqhc/11.1.37. [DOI] [PubMed] [Google Scholar]
- Shapiro E. “Market Forces and Vulnerable Elderly People: Who Cares?”. Canadian Medical Association Journal. 1999;159(2):151–2. [PMC free article] [PubMed] [Google Scholar]
- Shapiro E, Tate RB. “Monitoring the Outcomes of Quality of Care in Nursing Homes Using Administrative Data.”. Canadian Journal on Aging. 1995;14(4):755–68. [Google Scholar]
- Teng EL, Chui HC. “The Modified Mini-Mental State (3MS) Examination.”. Journal of Clinical Psychiatry. 1987;48(8):314–8. [PubMed] [Google Scholar]