Abstract
Objective
To describe the relative importance of health care market structure and county-level demographics in determining rates of hospice use.
Data Sources
Medicare claims data for a cohort of elderly patients newly diagnosed with lung cancer, colon cancer, stroke, or heart attack in 1993, followed for up to five years, and linked to Census and Area Resource File data.
Study Design
Variation between markets in rates of hospice use by patients with serious illness was examined after taking into account differences in individual-level data using hierarchical linear models. The relative explanatory power of market-level structure and local demographic variables was compared.
Data Collection Methods
The cohort was defined within the Medicare hospital claims data using validated algorithms to detect incident cases of disease with a three-year lookback. Use of hospice was determined by linkage at an individual level to the Standard Analytic Files for Hospice through 1997. Individual-level data was linked to the Area Resource File using county identifiers present in the Medicare claims.
Principal Findings
There is substantial variation in hospice use across markets. This variation is not explained by differences in the major components of health care infrastructure: the availability of hospital, nursing home, or skilled nursing facilities, nor by the availability of HMOs, doctors, or generalists.
Conclusions
Intercounty heterogeneity in hospice use is substantial, and may not be related to the set-up of the medical care system. The important local factors may be local preferences, differences in the particular mix of services provided by local hospices, or differences in community leadership on end of life-issues; many of these differences may be amenable to educational efforts.
Keywords: Terminal care, elderly, small-area variation, inequality
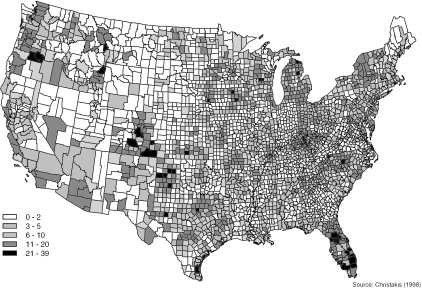
Hospice offers substantial benefits to patients at the end of life. It can be delivered in a patient's home, facilitating at-home death (Moinpour and Polissar 1989; Mor and Hiris 1983). Hospice care optimizes relief of pain and other symptoms (Greer et al. 1986) as well as patient and family satisfaction (Dawson 1991; Kane et al. 1985; Wallston et al. 1988). Hospice use before death also appears to decrease the burden of bereavement in surviving spouses (Christakis and Iwashyna 2002). Thus, hospice facilitates many things patients say they want at the end of life (Steinhauser et al. 2000). Despite these many benefits, hospice appears to be underutilized. Although physicians feel that patients should spend about 12 weeks with hospice services, (Iwashyna and Christakis 1998) the median duration in 1993 was only 30 days (Christakis and Iwashyna 2000). Likewise, there is enormous variation in the proportion of elderly decedents who have used hospice across counties, as shown in Figure 1 (Christakis 1998). In 1996, rates of hospice use among decedents varied more than 11-fold between metropolitan statistical areas. (Virnig et al. 2000).
Figure 1.
Percentage of Total Deaths that Were Cared for Under the Medicare Hospice Benefit in 1993, by County
The roots of this variation are complex. Some lie within the physician–patient dyad. There is substantial variation across diagnoses in the use of hospice: cancer patients are disproportionately represented among hospice users (Iwashyna, Zhang, and Christakis 2002). This may be related to differences in the predictability of the natural history of the diseases (Teno et al. 2001). The substantial complexity of prognosis appears to play a key role in explaining delayed referral (Christakis 1999; Lynn, Teno, and Harrell 1995). Demographic and other characteristics, such as age, sex, ethnicity, dementia-status, and drug-abuse history all appear to influence referral to hospice; it is not clear to what degree these differences result from differences in preferences for end-of-life care, differences in the natural history of disease, or differences in treatment recommendations (Christakis and Iwashyna 2000). On the patient's side, the perception of a shorter prognosis (Weeks et al. 1998) and a greater impact of the disease on family members are both associated with preferences for palliative care (Covinsky et al. 1994).
Is there a role for market factors in whether and when hospice is used? There has been very little work looking at the influence of market-level factors on rates of hospice use; in contrast, the variation between markets in the utilization of other types of health care has been well documented in the small-area variations literature. The important influence of factors such as the availability of hospital beds and HMO (health maintenance organization) penetration on many health care decisions is well known (Wennberg and Cooper 1998). In previous studies, greater numbers of hospital days per capita were associated with greater levels of in-hospital death (Pritchard et al. 1998) and lower hospice use (Virnig et al. 2000). In contrast, greater numbers of hospital beds have also been shown to be associated with longer receipt of hospice care among hospice users (Christakis and Iwashyna 2000). Increased hospice use among decedents before death has also been associated with higher HMO enrollment and greater numbers of doctors per capita (Virnig et al. 2000).
However, the existing market-factor literature has in general been hampered by methodological problems related to the fact that the objects of study exist at two levels: individual patients and the markets they live in. Analysis solely at one level necessarily introduces strong limitations into the interpretations at the other level. In order to solve this problem, we used hierarchical linear modeling to look at the influence of individual-level and market-level variables on individual hospice use (Bryk and Raudenbush 1992). This lets us control at the individual level for primary diagnosis and comorbidity burden, as well as traditional demographics. At the same time, we can examine county-level indicators of market structure as well as indicators of the relative wealth of the county—a potential confounder. Most importantly, this approach lets us test not merely whether proposed factors are associated with hospice use net of individual factors but also the degree to which those associations explain observed variation in hospice use between counties.
Beyond this analytic innovation, this is the first study to use a nationally representative, prospectively defined cohort to analyze the decision to use hospice. We looked at Medicare patients newly diagnosed in 1993 with four conditions: lung cancer, colon cancer, stroke, or myocardial infarction. These conditions were chosen to be typical of the most common causes of death that have a predictably high lethality following a terminal period (so that hospice use could reasonably be considered), and that can be reliably ascertained in the Medicare claims with adequate numbers of events for the type of analyses we propose here. We followed these patients forward for up to five years, by which point more than three-quarters had died, and assessed whether or not those who died used hospice during their terminal period. To our knowledge, virtually all previous work on hospice referral has looked only at “numerator” samples, consisting of those patients who actually went to hospice.
Hypotheses
Concretely, we propose to evaluate the following hypotheses:
H1. There is substantial intercounty variation in hospice use rates net of individual-level compositional differences.
H2. This variation is primarily explained by differences in the market structure—in particular, markets with greater numbers of hospital beds, greater numbers of nursing home beds, greater numbers of skilled nursing facility beds (all on a per person, older than age 65 basis), and relatively more specialists than generalists, will tend to have lower levels of hospice use.
We will examine whether or not patients with incident disease during 1993 who died before December 31, 1997, used hospice in all counties in which at least some patients used hospice.
This work has implications for understanding the key determinants of end-of-life care. If H1 is true, this implies that the variation in hospice use is not an intrinsic component of the variability in time courses of patients and its attendant prognostic challenges, but rather that there is a “social” or “behavioral” component that is analytically important as well. If H2 is true, this suggests that the social component is strongly governed by incentives and structures within the medical system—and this implies that the application of other incentives typically used in the health care setting may be appropriate to modifying patterns of hospice use. If H1 is true and H2 is false, then there are substantial differences between markets in their use of hospice that are not associated with differences in health care market structure. If that is so, the variation is likely explainable by differences in local culture. That is, within locales, nearby patients and physicians are similar in their choices about hospice use; this may be the result of differences in local values about care at the end of life, differences in the attractiveness of the particular hospices in an area, or differences in the availability, views, and quality of local leadership on end-of-life issues.
Methods
COSI Cohort Construction
The subjects analyzed here are drawn from the Care after the Onset of Serious Illness (COSI) dataset, a dataset we have built based on Medicare claims. Medicare data capture 96 percent of the American population older than 65 (Hatten 1980). The claims miss select populations such as those receiving care from the Veterans' Administration, those overseas, those still in the labor force and insured through their job, and those still in the active-duty military. The COSI dataset contains clinical, demographic, and other information about a population-based cohort of 1,241,935 elderly patients identified at the time of initial diagnosis with a serious illness in 1993. In the first stage of data development, a cohort of all patients newly diagnosed with one of 13 diagnoses were identified: cancer of the lung, colon, pancreas, urinary tract, liver or biliary tract, head or neck, or central nervous system, as well as leukemia or lymphoma, stroke, congestive heart failure, hip fracture, or myocardial infarction (MI). For the purposes of the current study, we focused on the conditions that account for the leading causes of death in the United States: stroke, MI, colon cancer, or lung cancer (U.S. Census Bureau 1997). This research was approved by the University of Chicago Human Subjects Committee.
Briefly, the development of the COSI cohort relies initially on 1993 inpatient hospitalization records. Extensive detail is available elsewhere (Christakis, Iwashyna, and Zhang 2002). These records, contained in the MedPAR file, represent a complete enumeration of hospitalizations for Medicare beneficiaries occurring during 1993. For individuals who had a hospitalization with one of the above 13 conditions in 1993, we used well-described methods to ascertain whether their condition could be considered incident or prevalent; we included in COSI only those malignancies that were deemed incident at the time of their first hospitalization for one of the above conditions after reviewing three prior years of claims (McBean, Babish, and Warren 1993; McBean, Warren, and Babish 1994). In the case of heart attack and stroke, we used similar approaches to include only new events for a patient; we could exclude claims that were for follow-up of old events. (Benesch et al. 1997; Krumholz et al. 1998; Lauderdale et al. 1993) All other diseases that patients may have had (for example, as noted on prior hospitalizations for other conditions) were also collected and were treated as comorbidities. (Charlson et al. 1987; Deyo, Cherkin, and Ciol 1992; Zhang, Iwashyna, and Christakis 1999).
With follow-up until December 31, 1997, we used the claims to ascertain all subsequent inpatient and outpatient health care use of these patients and their living spouses. Pertinently for this project, we noted whether and when patients were enrolled in hospice care using the Standard Analytic Files for hospice. Mortality follow-up for all cohort members was achieved with the highly accurate and complete Vital Status file maintained by the Health Care Financing Administration (HCFA), updated as of June 1999. As a proxy for patients' economic status, we used the patients' zip code of residence at the time of diagnosis to link to the 1990 Census and observe the median income of residents of that zip code, a technique that has been validated (Hofer et al. 1998) but that also has important limitations (Geronimus and Bound 1998; Geronimus, Bound and Neidert 1996; Robinson 1950). As a separate proxy for patients' economic status, for each individual, we were able to ascertain whether they were recipients of Medicaid (Clark and Hulbert 1998; Escarce et al. 1993). Note that this second variable may also be related to nursing home use.
County-level variables were extracted from the Area Resource File (ARF). They include the number of hospital beds, skilled nursing facility beds, and nursing home beds, all included on a per-1,000-people-65-and-older basis. (Population estimates in the ARF are derived from the Census.) Other (county-level) medical infrastructure variables included the total number of hospitals, the number of physicians per capita, the percentage of physicians who were generalists, and the fractions of individuals in HMOs. We also included the median income in 1993, the percentage of those who were employed who worked in white collar industries in 1993, population density in 1993 (as quartiles), and percentage of deaths in the county in 1990–1993 that were due to cancer, as recorded on the death certificates.
Cohort Restrictions
Most counties in the United States had very few or no individuals using hospice. If no hospice provider is available in a county, then no patient can use hospice, and those patients are not at-risk for hospice use. We therefore limited ourselves to all counties in which at least 10 of the more than two million elderly who died in 1993 used hospice; there were 1,530 such counties of the total of 3,072 counties in the United States. Our cohort then consisted of all 331,880 COSI members with stroke, myocardial infarction (MI), colon cancer, or lung cancer who died before the end of follow-up on December 31, 1997, in a county in which at least 10 people used hospice in 1993. Excluded counties were less dense than included counties; they also had modestly lower medical infrastructure: numbers of hospitals, doctors per capita, and proportion specialists. Excluded counties also had somewhat different demographic characteristics: they had a lower median income, a higher median age, a higher fraction of white collar employment, and a higher fraction of deaths to cancer. Additional data on the COSI cohort's patterns of inpatient hospitalization, outpatient utilization, and mortality have been published elsewhere (Iwashyna, Zhang, and Christakis 2002).
Absence of Indicators of Hospice “Availability”
In the current analysis we do not use any indicators of hospice availability. Any such indicator would be highly endogenous. The nature of hospice care—provided in the patient's home, with relatively little specialized equipment—makes market entry quite easy. That is, there is no natural capacity constraint—no equivalent to the “hospital bed”—which would serve as an indicator of capacity that is independent of use. Instead, given that there is some provider in the vicinity of the county able to provide hospice services to patients in that county (as evidenced by actual use by at least 10 people in 1993), we assume that the desire of patients and physicians for hospice service, rather than the availability of hospice nurses or services, is the limiting factor.
Definitions of Markets and the Use of Counties as an Approximation
There are a number of difficult methodologic issues involved in defining health care markets. Some have strongly advocated the use of the Hospital Referral Regions (HRRs) (Wennberg and Cooper 1998), others the use of network-based measures (Phibbs and Robinson 1993; Sohn 1996; Succi, Lee, and Alexander 1997), and others counties. In this project we have used counties to approximate markets, as has been done in numerous other studies (Banaszak-Holl, Zinn, and Mor 1996; Hartley, Moscovice, and Christianson 1996; Kerstein, Pauly, and Hillman 1994; Lafata, Koch, and Weissert 1994; Mullan, Politzer, and Davis 1995; Murtaugh 1994; Padgett et al. 1994; Roetzheim et al. 1999; Succi, Lee, and Alexander 1997; Wholey et al. 1997). This was done for a number of reasons: (1) our experience with hospice providers suggests that counties best approximate the way they think about their market's boundaries; (2) empirical tractability and availability of data; and (3) past work suggesting that results are often (but not always) insensitive to the difference between HRRs and counties (McLaughlin et al. 1989).
Hierarchical Generalized Linear Modeling
We used two-level hierarchical modeling for individuals nested within counties (Bryk and Raudenbush 1992). Given the clustering of individuals within counties, hierarchical modeling is required to generate unbiased and efficient estimates, as well as proper standard errors, for county-level effects on individual outcomes. Such modeling can take into account (1) the influence of different sample sizes across counties, and (2) the dependence among individual outcomes clustered within the same county. Individual-level factors were modeled at level one, and county-level factors were modeled at level two. A logistic model was used at level one given that our outcome of interest, entry into hospice (or not) before death, was dichotomous. Variation between counties in odds of hospice use was assessed with a one-way ANOVA model with random effects. Predictors/adjustors of interest at level one included: demographic factors, diagnosis, and comorbidity. These variables were entered at the individual-level grand-mean centered, and the variance components of their slopes were fixed at the county-level, in order to assess for variation between counties (in odds of hospice use) adjusted for differences between counties in these individual-level factors.
At the county level, predictors/adjustors of interest were divided into two groups: county-level demographic factors and market factors. The intercept from the individual-characteristic adjusted model, representing the odds of hospice use adjusting for county variation in individual-level factors, was then modeled with these county-level variables to assess the relative proportions of variance explained by local demographic and market factors. Inspection of correlations between the county-level variables and their bivariate relationships with the individual-level intercept did not suggest evidence of multicollinearity among the predictor variables with respect to any models.
Sensitivity Analyses
In order to assess the degree to which fixed right censoring—and the consequent fact that some patients do not die while under observation—might have biased our results, we conducted several sensitivity analyses. First, we constructed two datasets to test the (implausibly large) maximal extent of bias: one where all individuals who did not die by December 31, 1997, are assumed to have used hospice, and one where all are assumed not to have used hospice. We then reexecuted our models to see if our substantive conclusions were altered. This technique is based on published descriptions (Allison 1995). As shown below, our findings were not sensitive to these different assumptions. Second, we also reexecuted our models within those counties where at least 50 Medicare patients used hospice in 1993, and found substantively identical results to those presented here. Third, we replicated our analyses within each disease group separately, and, as shown below, found substantively identical results. Fourth, we replicated our analyses looking at only 1993 decedents and only 1997 decedents to see if temporal trends in hospice use were masked in our results; as shown below, there was no important effect.
Results
Table 1 displays the individual-level sample characteristics. There were 331,880 decedents with our four diagnoses nested within 1,530 counties. Of these, 15 percent had used hospice. Furthermore, 48 percent were male; 86 percent were white; and 31 percent suffered from a malignancy, 28 percent from a stroke, and 30 percent from a heart attack. Thirty-two percent of lung cancer decedents, 31 percent of colon cancer decedents, 8 percent of stroke decedents, and 7 percent of heart attack decedents had used hospice.
Table 1.
Individual-Level Characteristics
| Mean | Standard Deviation | |
|---|---|---|
| Primary Diagnosis | ||
| Lung cancer | 19% | |
| Colon cancer | 12% | |
| Stroke | 38% | |
| Myocardial infraction | 30% | |
| Comorbidity Adjustment | ||
| Charlson score | 1.37 | 1.92 |
| Number of hospitalizations | 1.54 | 2.16 |
| Demographics | ||
| Age (years) | 78.9 | 7.07 |
| Male | 48% | |
| White | 86% | |
| Medicaid recipient | 15% | |
| Zip-code median income ($1,000) | 31.0 | 11.69 |
| Used hospice before death | 15% | |
Is There a County-Level Effect on Hospice Use?
A one-way ANOVA model with random effects demonstrated a statistically significant variance component of 0.236 for the intercept (X2=12209.7, 1,529 df, p<0.001), indicating significant variation between counties in the odds of hospice use when differences in individual-level characteristics between the counties are not controlled. Inclusion of all individual-level predictors yielded a variance component of 0.282 for the intercept (X2=12,497.9, 1,529 df, p<0.001). That is, individuals within a given county are more similar in their use of hospice than chance alone would explain, and adjustment for differences among the counties with respect to the individual characteristics of decedents and their medical conditions did not explain this county-level variation in hospice.
How Do Individuals' Characteristics Affect Hospice Use?
Table 2 shows the fixed effects estimates for the individual-level predictors. Controlling for other factors, older, male, and nonwhite patients were estimated to be less likely to use hospice; similarly, those who qualified for Medicaid or had lower levels of comorbidity were less likely to use hospice. Patients with cancer were much more likely to use hospice than those who have had a heart attack or a stroke. Men were 0.90 (95% OR CI: 0.88,0.92) times less likely to use hospice compared to women. Whites were 1.19 (95% OR CI: 1.15,1.23) times more likely compared to nonwhites. Those who qualified for Medicaid were 0.69 (95% OR CI: 0.66,0.72) times less likely to use hospice before death; similar effects were found for affluence as measured by the median income of one's immediate neighborhood. Lastly, the number of times an individual had been hospitalized in the last three years was negatively correlated with hospice use, while the more serious an individual's comorbidity score, the more likely that person was to receive hospice care. We emphasize that these effects are each net of the other factors in the individual-level model that takes into account the clustering within counties.
Table 2.
Individual-Level Effects on the Use of Hospice
| Odds-Ratio | Lower Bound | Upper Bound | p-value | |
|---|---|---|---|---|
| Primary Diagnosis | ||||
| Lung cancer | 1.00 | <ref> | <ref> | <ref> |
| Colon cancer | 1.05 | 1.02 | 1.08 | 0.002 |
| Stroke | 0.23 | 0.21 | 0.24 | 0.000 |
| MI | 0.18 | 0.17 | 0.18 | 0.000 |
| Comorbidity Adjustment | ||||
| Charlson score | 1.02 | 1.01 | 1.02 | 0.000 |
| Number of hospitalizations | 0.96 | 0.95 | 0.97 | 0.000 |
| Demographics | ||||
| Age (years) | 0.98 | 0.97 | 0.98 | 0.000 |
| Male | 0.90 | 0.88 | 0.92 | 0.000 |
| White | 1.19 | 1.15 | 1.23 | 0.000 |
| Medicaid recipient | 0.69 | 0.66 | 0.72 | 0.000 |
| Zip-code median income per ($1,000) | 1.01 | 1.00 | 1.01 | 0.000 |
95% confidence intervals are presented for the odds ratio.
Can the County-Level Effect Be Explained?
Table 3 displays the county-level sample characteristics. As described above, three models were examined at the county level: one including only county demographic variables, another with only market factors, and a third “combined” model including both the county demographic and market variable blocs. When the bloc of demographic predictors was used to model the intercept, in this case the log odds of going to hospice (adjusted for differences between counties in individual-level demographics, diagnoses, and morbidity), the residual variance component decreased from 0.282 to 0.275. Thus, demographics explained 2.5 percent (=1–0.275/0.282) of the variation between counties. When market factors were introduced by themselves, the variance was reduced to 0.280. Market factors explained 0.7 percent of the between-county variation. When both blocs of predictors, the demographic and the market, were included in the equation for the intercept, the remaining variance between counties was 0.273 (X 2=11992.1, 1,515 df, p<0.001). Together, the demographic characteristics of counties and those of their health care markets explained 3.2 percent of the variation among them with respect to the use of hospice.
Table 3.
Characteristics of Counties
| Mean | Standard Deviation | |
|---|---|---|
| Market Structure | ||
| Number of hospitals | 3.3 | 6.6 |
| Fraction of all doctors that are generalists | 0.5 | 0.2 |
| Hospital beds per 1,000 people >=65 | 34.1 | 127.3 |
| Nursing home beds per 1,000 people >=65 | 67.1 | 124.0 |
| SNF beds per 1,000 people >=65 | 3.1 | 8.0 |
| Doctors per 1,000 people any age | 2.7 | 18.5 |
| Fraction of population in HMOs | 0.04 | 0.16 |
| Demographics | ||
| Percentage of deaths due to cancer | 24% | 2% |
| Median income ($1,000) | 17.5 | 3.9 |
| Median age (years) | 30.6 | 3.6 |
| Percentage white collar | 50% | 9.6% |
The first columns of Table 4 show the fixed effects estimates for the level-two predictors. Controlling for other factors, three demographic factors were significant. Individuals living in counties with more white collar employees were more likely to use hospice as were individuals living in the least densely populated counties. Individuals living in a county with relatively more cancer deaths were also more likely to use hospice. None of the county-level health care market factors were significantly associated with differences in the use of hospice.
Table 4.
Impact of County-Level Characteristics on Hospice Use (Coefficients that are statistically significant are in bold.)
| Sensitivity Analyses | ||||||
|---|---|---|---|---|---|---|
| Observed Data | All Censored Go to Hospice | No Censored Go to Hospice | ||||
| Coefficient | P value | Coefficient | P value | Coefficient | P value | |
| Market Structure | ||||||
| Number of hospitals | 0.0016 | 0.420 | 0.0005 | 0.436 | 0.0016 | 0.436 |
| Proportion generalists | 0.1907 | 0.092 | 0.1041 | 0.035 | 0.1591 | 0.143 |
| Hospital beds* | 0.0007 | 0.254 | 0.0004 | 0.076 | 0.0006 | 0.320 |
| Nursing home beds* | −0.0003 | 0.248 | −0.0003 | 0.003 | −0.0002 | 0.445 |
| SNF beds* | −0.0023 | 0.381 | 0.0004 | 0.680 | −0.0023 | 0.363 |
| Doctors** | −0.0135 | 0.112 | −0.0052 | 0.179 | −0.0128 | 0.099 |
| Proportion HMO penetration | 0.1472 | 0.069 | 0.0520 | 0.137 | 0.1403 | 0.060 |
| Demographics | ||||||
| % Deaths that are to cancer | 2.4787 | 0.004 | 1.3342 | 0.000 | 2.1411 | 0.008 |
| Median income ($1,000) | −0.0060 | 0.364 | −0.0020 | 0.534 | −0.0050 | 0.376 |
| Median age | 0.0047 | 0.337 | 0.0016 | 0.496 | 0.0054 | 0.241 |
| % White collar | 0.0064 | 0.045 | 0.0034 | 0.009 | 0.0051 | 0.097 |
| Pop density highest quartile | 0.0000 | <ref> | 0.0000 | <ref> | 0.0000 | <ref> |
| Pop density 3rd quartile | 0.0414 | 0.334 | 0.0371 | 0.038 | 0.0187 | 0.646 |
| Pop density 2nd quartile | 0.1023 | 0.067 | 0.0879 | 0.000 | 0.0514 | 0.331 |
| Pop density lowest quartile | 0.2815 | 0.003 | 0.1467 | 0.001 | 0.2156 | 0.014 |
| Variance | % Explained | Variance | % Explained | Variance | % Explained | |
| County-Level variation | 0.282 | 0.035 | 0.242 | |||
| After market controls | 0.280 | 0.71% | 0.034 | 0.87% | 0.241 | 0.77% |
| After demographic controls | 0.275 | 2.48% | 0.033 | 5.17% | 0.238 | 1.91% |
| After all county-level controls | 0.273 | 3.19% | 0.032 | 6.45% | 0.236 | 2.75% |
per 1000 people at least age 65.
per 1000 people, any age.
Sensitivity Analyses
The final four columns of Table 4 demonstrate the sensitivity of our results to alternative extreme assumptions about the impact of censoring on our results. We find that in all cases, significant county-level variation in hospice use remains. (The variance components in these hierarchical logistic models are dimensionless; their magnitudes can be compared within nested models, but cannot be compared across models on different datasets. Thus we cannot say whether there was “more” variation at the county-level under one set of assumptions versus the other.) We find relatively little substantively interesting difference in percentage of the variance explained by market-structure or demographic variables across different assumptions in the sensitivity analyses.
We also performed stratified analyses to ensure that differences between diseases or time from diagnosis until death were not masking effects. Of the variation between counties in the use of hospice by colon cancer patients, 5.9 percent was explained by demographic and market-structural factors. Similarly, 2.3 percent of the variation between counties by lung cancer patients, 2.7 percent of the variation between counties by myocardial infarction patients, and 7.1 percent of the variation between counties by stroke patients were explained by demographic and market-structural factors. In our cohort, all of whom were diagnosed in 1993, 4.2 percent of the variation between counties in hospice use among early decedents—those who died during 1993—was explained by demographic and market-structural factors; 10.4 percent of the variation between counties among late decedents—those who died during 1997—was explained by demographic and market-structural factors.
Discussion
The results of our analyses indicate that intercounty variation in hospice rates is not merely a function of the individual characteristics of those suffering from serious illness in each county. Even after adjusting for differences between counties with respect to individual-level demographics, disease, and morbidity, intercounty variation was considerable. That is, if hospice was available, patients within a given county were more likely to make the same choice about hospice use than were patients in other counties; there appear to be county-level effects on the use of hospice that are not simply the result of differences between counties in their composition in terms of the measured individual-level characteristics. However, at the county-level, market-structure and area demographic variables accounted for little of this intercounty variation. Among those variables that were significant, all were variables associated with patient-side preferences: the commonness of cancer deaths, the degree of white collar employment, and the population density (with rural counties using more hospice if hospice was available).
Strikingly, market variables shown to be associated with duration of hospice use in previous studies—fraction of generalists versus specialists and hospital beds—had no effect on the odds of utilizing hospice services in the first place (Christakis and Iwashyna 2000). Likewise, these variables have been shown to be associated with increased relative hospice use at the Health Service Area-level (Virnig et al. 2000). The absence of such effects in the present analyses suggests that (a) individual-level differences in diagnosis and wealth may need to be taken into account (Virnig et al used only age/sex/race standardized rates); (b) aggregate demographic factors may be more important than market structure; and (c) associations, while important, need to be considered in the context of the variation explained (past studies have not examined the overall quite low levels of variation between markets that their models explained). Of course, these differences could also be the result of the modest differences in the way the outcomes variables were defined. For example, Virnig et al. (2000) looked at the fraction of all deaths that used hospice; Christakis and Iwashyna (2000) looked at duration within hospice, not whether or not hospice was used. In contrast, we looked at the fraction of those who died after diagnosis with one of the most common serious illnesses.
A similar disjunction was noted at the individual level between variables predicting length of use of hospice (among those who use it) and variables predicting whether or not hospice was used in the first place. In prior work (Christakis and Iwashyna 2000) older, nonwhite, and poorer patients had longer stays in hospice; in contrast, they were less likely to use hospice in the present work and in that of Virnig et al. (2000). However, other individual-level inferences were confirmed. From the present denominator-based sample, we find that individuals who have cancer are more likely to use hospice than those without cancer; individuals with greater comorbidity, as measured by the Charlson score, are more likely to use hospice than those without; and women are more likely to use hospice than men. Christakis and Iwashyna (2000) had suggested that greater odds of going to hospice could be associated with earlier entry and therefore longer receipt of service after entry; the differing patterns of some determinants seen here suggest the situation may be more complicated. Clearly, additional work is necessary, looking at both the expansion of hospice into noncancer diagnoses (as Virnig et al. 2000 suggest) and at its duration of use by those who use it (Christakis and Escarce 1996).
Our study has a number of limitations. The first is that we have examined the role of hospice only in those markets in which hospice was already available. We have not studied the process by which hospice enters new markets—a process which may be related to market structure and which surely has profound effects on hospice use. Second, we have looked only within Medicare recipients, who account for a majority (more than 75 percent) but not all hospice beneficiaries. Third, we have used counties as an approximation of the relevant health care market, but other market definitions are plausible. Fourth, we have been limited to the data available within the Medicare claims. Thus, we cannot explore the likely important role of variation in social networks or kin availability in providing the structural requirements necessary for hospice use—which may also meaningfully vary across counties. Finally, we have no information about patient and family preferences for hospice use. As such, we cannot say whether the variation in rates that we observe is a normatively good thing from the perspective of respecting patients’ wishes; we can only describe the epidemiology of hospice use.
In conclusion, we find that there is substantively enormous variation in hospice rates across markets. Further, we find this variation is not the result of differences in the major components of health care infrastructure: the availability of hospital, nursing home, or skilled nursing facilities, nor the availability of HMOs, doctors, or generalists. This suggests that intercounty heterogeneity may not be related to the set-up of the medical care system. Instead, our results suggest that there is important variation between counties in some local factors that influence the choice of hospice. Those factors may be local preferences, differences in the particular mix of services provided by local hospices, or differences in community leadership on end-of-life issues. While our data do not allow us to distinguish between these hypotheses, many of these differences may be amenable to educational efforts.
Acknowledgments
The authors thank Anthony S. Bryk for comments on an earlier draft of the paper and Carolyn Fuqua for help with initial analyses.
Footnotes
This work was supported by a National Research Service Award from the NIH/National Institute on Aging (T32-AG00243) to Theodore J. Iwashyna; a National Research Service Award from the Agency for Healthcare Research and Quality (T32 HS00084-02) to Virginia W. Chang; and a grant from the National Institute on Aging (R-01 AG15326-01) to Nicholas A. Christakis.
References
- Allison PD. Survival Analysis Using the SAS System: A Practical Guide. Cary, NC: SAS Institute; 1995. [Google Scholar]
- Banaszak-Holl J, Zinn JS, Mor V. “The Impact of Market and Organizational Characteristics on Nursing Care Facility Service Innovation: A Resource Dependency Perspective.”. Health Services Research. 1996;31:97–117. [PMC free article] [PubMed] [Google Scholar]
- Benesch C, Witter DM, Jr, Wilder AL, Duncan PW, Samsa GP, Matchar DB. “Inaccuracy of the International Classification of Disease (ICD-9-CM) in Identifying the Diagnosis of Ischemic Cerebrovascular Disease.”. Neurology. 1997;49:660–4. doi: 10.1212/wnl.49.3.660. [DOI] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical Linear Models. Newbury Park, CA: Sage; 1992. [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. “A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation.”. Journal of Chronic Disease. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Christakis NA. Napp Keynote Address: Health Services Research in Palliative Care in the United States. Leeds UK: Annual Palliative Care Congress of Great Britain and Ireland; 1998. [Google Scholar]
- Christakis NA. Death Foretold: Prophecy and Prognosis in Medical Care. Chicago: University of Chicago Press; 1999. [Google Scholar]
- Christakis NA, Escarce JJ. “Survival of Medicare Patients Following Enrollment in Hospice Programs.”. New England Journal of Medicine. 1996;335:172–8. doi: 10.1056/NEJM199607183350306. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Iwashyna TJ. “The Impact of Individual and Market Factors on the Timing of Initiation of Hospice Terminal Care.”. Medical Care. 2000;38:528–41. doi: 10.1097/00005650-200005000-00009. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Iwashyna TJ. “The Impact of End-of-Life Care on Families: A Matched Cohort Study of Hospice Use by Decedents and Mortality Outcomes in Surviving Spouse.”. Social Science and Medicine. 2002 doi: 10.1016/s0277-9536(02)00370-2. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Iwashyna TJ, Zhang JX. “Care After the Onset of Serious Illness (COSI): A Novel Claims-Based Data Set Exploiting Substantial Cross-Set Linkages to Study End-of-Life Care.”. Journal of Palliative Medicine. 5(4):515–30. doi: 10.1089/109662102760269751. [DOI] [PubMed] [Google Scholar]
- Clark WD, Hulbert MM. “Research Issues: Dually Eligible Medicare and Medicaid Beneficiaries, Challenges and Opportunities.”. Health Care Financing Review. 1998;20:1–10. [PMC free article] [PubMed] [Google Scholar]
- Covinsky KE, Goldman L, Cook EF, Oye R, Desbiens N, Reding D, Fulkerson W, Connors AF, Jr, Lynn J, Phillips RS SUPPORT Investigators. “The Impact of Serious Illness on Patient's Families.”. Journal of the American Medical Association. 1994;272:1839–44. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- 14.Dawson NJ. “Need Satisfaction in Terminal Care Settings.”. Social Science and Medicine. 1991;32:83–7. doi: 10.1016/0277-9536(91)90131-u. [DOI] [PubMed] [Google Scholar]
- Deyo RA, Cherkin DC, Ciol MA. “Adapting a Clinical Comorbidity Index for Use with ICD-9-CM Administrative Databases.”. Journal of Clinical Epidemiology. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Escarce JJ, Epstein KR, Colby DC, Schwartz JS. “Racial Differences in the Elderly's Use of Medical Procedures and Diagnostic Tests.”. American Journal of Public Health. 1993;83:948–54. doi: 10.2105/ajph.83.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Bound J. “Use of Census-based Aggregate Variables to Proxy for Socioeconomic Group: Evidence from National Samples.”. American Journal of Epidemiology. 1998;148:475–86. doi: 10.1093/oxfordjournals.aje.a009673. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Bound J, Neidert LJ. “On the Validity of Using Census Geocode Characteristics to Proxy Individual Socioeconomic Characteristics.”. Journal of the American Statistical Association. 1996;91:529–37. [Google Scholar]
- Greer D, Mor V, Morris J, Sherwood S, Kidder D, Birnbaum H. “An Alternative in Terminal Care: Results of the National Hospice Study.”. Journal of Chronic Disease. 1986;39:9–26. doi: 10.1016/0021-9681(86)90103-7. [DOI] [PubMed] [Google Scholar]
- Hartley D, Moscovice I, Christianson J. “Mobile Technology in Rural Hospitals: The Case of the CT Scanner.”. Health Services Research. 1996;31:213–34. [PMC free article] [PubMed] [Google Scholar]
- Hatten J. “Medicare's Common Denominator: The Covered Population.”. Health Care Financing Review (fall) 1980:53–64. [PMC free article] [PubMed] [Google Scholar]
- Hofer TP, Wolfe RA, Tedeschi PJ, MacMahon LF, Griffith JR. “Use of Community versus Individual Socioeconomic Data in Predicting Variation in Hospital Use.”. Health Services Research. 1998;33:243–59. [PMC free article] [PubMed] [Google Scholar]
- Iwashyna TJ, Christakis NA. “Attitude and Self-Reported Practice Regarding Hospice in a National Sample of Internists.”. Journal of Palliative Medicine. 1998;1:241–8. doi: 10.1089/jpm.1998.1.241. [DOI] [PubMed] [Google Scholar]
- Iwashyna TJ, Zhang JX, Christakis NA. “Disease-Specific Patterns of Hospice and Related Healthcare Use in an Incidence Cohort of Seriously I11 Elderly Patients.”. Journal of Palliative Medicine. 2002;5(4):531–8. doi: 10.1089/109662102760269760. [DOI] [PubMed] [Google Scholar]
- Kane RL, Klein SJ, Bernstein L, Rothenberg R, Wales J. “Hospice Role in Alleviating the Emotional Stress of Terminal Patients and Their Families.”. Medical Care. 1985;23(3):189–97. doi: 10.1097/00005650-198503000-00001. [DOI] [PubMed] [Google Scholar]
- Kerstein J, Pauly MV, Hillman A. “Primary Care Physician Turnover in HMOs.”. Health Services Research. 1994;29:17–37. [PMC free article] [PubMed] [Google Scholar]
- Krumholz HM, Radford MJ, Wang Y, Chen J, Heiat A, Marciniak TA. “National Use and Effectiveness of the Beta-Blockers for Treatment of Elderly Patients after Acute Myocardial Infarction.”. Journal of the American Medical Association. 1998;280:623–9. doi: 10.1001/jama.280.7.623. [DOI] [PubMed] [Google Scholar]
- Lafata JE, Koch GG, Weissert WG. “Estimating Activity Limitation in the Noninstitutionalized Population: A Method for Small Areas.”. American Journal of Public Health. 1994;84:1813–7. doi: 10.2105/ajph.84.11.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Furner SE, Miles TP, Golderberg J. “Epidemiologic Uses of Medicare Data.”. Epidemiologic Reviews. 1993;15:319–27. doi: 10.1093/oxfordjournals.epirev.a036123. [DOI] [PubMed] [Google Scholar]
- Lynn J, Teno JM, Harrell FM. “Accurate Prognostication of Death: Opportunities and Challenges for Clinicians.”. Western Journal of Medicine. 1995;163:250–7. [PMC free article] [PubMed] [Google Scholar]
- McBean AM, Babish JD, Warren JL. “Determination of Lung Cancer Incidence in the Elderly Using Medicare Claims Data.”. American Journal of Epidemiology. 1993;137:226–34. doi: 10.1093/oxfordjournals.aje.a116663. [DOI] [PubMed] [Google Scholar]
- McBean AM, Warren JL, Babish JD. “Measuring the Incidence of Cancer in Elderly Americans Using Medicare Claims Data.”. Cancer. 1994;73:2417–25. doi: 10.1002/1097-0142(19940501)73:9<2417::aid-cncr2820730927>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- McLaughlin CG, Normolle DP, Wolfe RA, McMahon LF, Jr, Griffith JR. “Small-Area Variation in Hospital Discharge Rates: Do Socioeconomic Variables Matter?”. Medical Care. 1989;27:507–21. doi: 10.1097/00005650-198905000-00006. [DOI] [PubMed] [Google Scholar]
- Moinpour CM, Polissar L. “Factors Affecting Place of Death of Hospice and Non-hospice Cancer Patients.”. American Journal of Public Health. 1989;79:1549–51. doi: 10.2105/ajph.79.11.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Hiris J. “Determinants of Site of Death among Hospice Cancer Patients.”. Journal of Health and Social Behavior. 1983;24:375–85. [PubMed] [Google Scholar]
- Mullan F, Politzer RM, Davis CH. “Medical Migration and the Physician Workforce International Medical Graduates and American Medicine.”. Journal of the American Medical Association. 1995;273:1521–7. doi: 10.1001/jama.1995.03520430057039. [DOI] [PubMed] [Google Scholar]
- Murtaugh CM. “Discharge Planning in Nursing Homes.”. Health Services Research. 1994;28:751–69. [PMC free article] [PubMed] [Google Scholar]
- Padgett DK, Patrick C, Burns BJ, Schlesinger HJ. “Ethnic Differences in Use of Inpatient Mental Health Services by Blacks, Whites, and Hispanics in a National Insured Population.”. Health Services Research. 1994;29:135–53. [PMC free article] [PubMed] [Google Scholar]
- Phibbs CS, Robinson JC. “A Variable-Radius Measure of Local Hospital Market Structure.”. Health Services Research. 1993;28:313–24. [PMC free article] [PubMed] [Google Scholar]
- Pritchard RS, Fisher ES, Teno JM, Sharp SM, Reding DJ, Knaus WA, Wennberg JE, Lynne J SUPPORT Investigators. “Influence of Patient Preferences and Local Health System Characteristics on the Place of Death.”. Journal of the American Geriatrics Society. 1998;43:1242–50. doi: 10.1111/j.1532-5415.1998.tb04540.x. [DOI] [PubMed] [Google Scholar]
- Robinson WS. “Ecological Correlations and the Behavior of Individuals.”. American Sociological Review. 1950;15:351–7. [Google Scholar]
- Roetzheim RG, Pal N, Gonzalez EC, Ferrante JM, Van Durme DJ, Ayanian JZ, Krischer JP. “The Effects of Physician Supply on the Early Detection of Colorectal Cancer.”. Journal of Family Practice. 1999;48:850–8. [PubMed] [Google Scholar]
- Sohn M-W. Chicago: University of Chicago. Dissertation Library; 1996. “From Regional to Local Markets: Network Study of Competition in California Hospital Markets.”. [Google Scholar]
- Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. “Factors Considered Important at the End of Life by Patients, Family, Physicians and Other Care Providers.”. Journal of the American Medical Association. 2000;284:2476–82. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- Succi MJ, Lee SY, Alexander JA. “Effects of Market Position and Competition on Rural Hospital Closures.”. Health Services Research. 1997;31:679–99. [PMC free article] [PubMed] [Google Scholar]
- Teno JM, Weitzen S, Fennel ML, Mor V. “Dying Trajectory in the Last Year of Life: Does Cancer Trajectory Fit Other Diseases?”. Journal of Palliative Medicine. 2001;4(4):457–64. doi: 10.1089/109662101753381593. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. Statistical Abstract of the United States. Washington DC: Government Printing Office; 1997. [Google Scholar]
- Virnig BA, Kind S, McBean M, Fisher ES. “Geographic Variation in Hospice Use Prior to Death.”. Journal of the American Geriatrics Society. 2000;48:1117–25. doi: 10.1111/j.1532-5415.2000.tb04789.x. [DOI] [PubMed] [Google Scholar]
- Wallston KA, Burger C, Smith RA, Baugher RJ. “Comparing the Quality of Death for Hospice and Non-hospice Cancer Patients.”. Medical Care. 1988;26:177–82. doi: 10.1097/00005650-198802000-00008. [DOI] [PubMed] [Google Scholar]
- Weeks JC, Cook EF, O'Day SJ, Peterson LM, Wenger N, Reding D, Harrell FE, Kussin P, Dawson NV, Connors AF, Jr, Lynn J, Phillips RS. “Relationship between Cancer Patients’ Predictions of Prognosis and Their Treatment Preferences.”. Journal of the American Medical Association. 1998;279:1709–14. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- Wennberg JE, Cooper MM. The Dartmouth Atlas of Health Care. Chicago: American Hospital Publishing; 1998. [PubMed] [Google Scholar]
- Wholey DR, Christianson JB, Engberg J, Bryce C. “HMO Market Structure and Performance”1985–1995. Health Affairs. 1997;16:75–84. doi: 10.1377/hlthaff.16.6.75. [DOI] [PubMed] [Google Scholar]
- Zhang JX, Iwashyna TJ, Christakis NA. “The Impact of Alternative Lookback Periods and Sources of Information on Charlson Comorbidity Adjustment in Medicare Claims.”. Medical Care. 1999;37:1128–39. doi: 10.1097/00005650-199911000-00005. [DOI] [PubMed] [Google Scholar]