Abstract
Background
A majority of patients with cancer who are seriously ill have a preference of dying at home. However, only a minority of patients actually die at home in most Western countries.
Aim
To explore factors associated with place of death in an unselected population of patients with cancer.
Design of study
Case-control study.
Setting
County of Funen, Denmark.
Method
Register linkage from six Danish healthcare registers.
Results
The GP's home visit during the last 3 months before death was inversely associated with dying in hospital (adjusted odds ratio [OR] = 0.08, 95% confidence interval [CI] = 0.06 to 0.12) and so were community nurses visiting the home (OR = 0.36, 95% CI = 0.26 to 0.48). Furthermore, being married (OR = 0.68, 95% CI = 0.56 to 0.85), and age at death of 40–65 years (OR = 0.70, 95% CI = 0.56 to 0.90) seemed to have an effect. Hospital death was associated with survival time of less than 1 month (OR = 2.27, 95% CI = 1.69 to 3.13). Type of cancer, sex, or residence (urban versus rural) were not associated with a hospital death in this multivariate analysis.
Conclusions
Dying at home was, to a higher extent, associated with GP visit and, to a lesser extent, community nurse visit than with clinical and sociodemographic characteristics of patients with cancer. In our view, these findings indicate the importance of the GP in particular. To increase the opportunity to die at home, more research is needed on the role of the GP and the interface between GPs and other providers of health care at home for patients who are terminally ill with cancer.
Keywords: family practice, health services research, neoplasm, palliative care, place of death
INTRODUCTION
Dying at home and remaining at home for as long as possible are of great importance to a majority of patients who are seriously ill with cancer and their families.1-3 However, only a minority of patients actually die at home in most Western countries.4-6
Factors influencing place of death in unselected populations of patients with cancer are not fully understood. A series of epidemiological studies have found associations between home death and age, sex, type of cancer and survival time,7-9 but the findings have not been consistent. Randomised trials evaluating different home-based palliative programmes10-11 have found that palliative care interventions, such as specially trained staff, enabled more patients to die at home. Those studies were, however, based on small, selected populations and effectiveness remained unclear12-13 until recently, when a review found a small quantitative benefit of intervention with palliative teams.14 However, there is lack of assessment of the influence of non-specialised community services, such as, general practice and community nurse services.
The Danish National Health Care system is divided into three administrative levels, where the responsibility for the financing and managing of hospitals lies with 15 administrative units (14 counties and one hospital authority for the capital). GPs are self-employed but paid through taxes in a blended remuneration system with capitation fee and fee for service.15 Community nurse services and nursing homes are owned by the 271 municipalities.
The aim of this study was to explore factors associated with place of death in an unselected population of patients dying from cancer and, in particular, to explore whether GP and community nurse services were associated with place of death adjusted for patient-related factors.
METHOD
Population registers
The setting of the study was the County of Funen in Denmark, with a population of 470 000. We obtained data from Danish population-based registers through use of the unique identification number assigned to everyone living in Denmark, thus ensuring accurate, individual-based linkage of information between registers. More specifically, we used information from four national registers and two local registers: the Danish Cancer Register,16 the Danish National Register of Causes of Death,17 the National Discharge Register,18 the civil registration system,19 The Billing Database of the Health Administration of the County of Funen, and registrations of community nurse activities.
Patients
The study sample was composed of all patients who died due to cancer in the County of Funen between 1 January 1996 and 31 December 1998. The Danish Cancer Register goes through a profound validation process. Data in this study represents the latest validated data at the time of writing. Data were collected from 3 months prior to death. After an initial description of place of death in the total cohort, we excluded the population living in nursing homes at the beginning of the observation period as well as those who moved to nursing homes during the whole 3-month period (Figure 1). The cohort used in the analysis, therefore, comprised of those who were resident at home (n = 4092).
Figure 1.
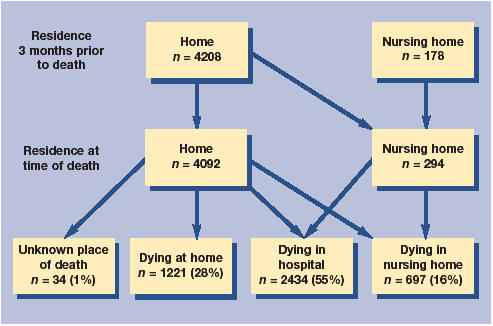
Place of death and change of residence during the last 3 months of life for patients with cancer (n = 4386).
How this fits in
A majority of patients with late-stage cancer wish to die at home or at least spend as much time as possible at home. In most Western countries, however, only a minority of patients actually die at home. The results of this large population-based study showed that home visits conducted by GPs were strongly associated with the possibilities of patients with cancer to die at home. Patient-related factors such as age, sex, and type of cancer do not appear to affect the place of death.
A breakdown of the patients shows that 2399 of these patients died in hospital and 438 died in nursing homes. For 34 patients the place of death was unknown. A total of 2871 patients, therefore, did not die at home, unlike the 1221 control patients. The patients who died in nursing homes in the analysis cohort were those on a temporary respite stay, whose deaths could reasonably be considered as institutional deaths.
Cancer diagnosis, age at diagnosis, and other details of diagnosis were obtained from the Danish Cancer Register. Data on the frequency of consultations with GP were collected from The Billing Database of the Health Administration of the County of Funen, an administrative register of all GP activity. As a result of the automatic deletion of records more than 5 years old, the analysis was limited to deaths that occurred between 27 March 1997 and 31 December 1998. This subgroup was, however, compatible with the total study group. Community nurse activity was extracted from administrative data files in the provincial capital, Odense. From the National Discharge Register, containing information about all citizens diagnosed or treated in a hospital setting, we obtained date and type of admissions, ambulatory contacts, and operations. Demographic variables and information on change of residence were obtained from the civil registration system.
Data analysis
We estimated the odds ratio (OR) of dying in hospital by logistic regression models, and calculated 95% confidence intervals (CIs). In the models we adjusted for potential confounding factors, such as type of cancer, duration of disease, severity of disease by number of ambulatory contacts, sex, age, marital status, number of children, geographic area, and citizenship. Cancer diagnoses were grouped in six categories: four separate categories for the four most frequent cancers (lung, breast, colon/rectum, prostate), one category for the haematological cancers (the course of which are rapid and treatment-intense), and one final category containing other cancers. We calculated the survival time by subtracting the date of diagnosis from the date of death and subsequently dichotomised the result (less than 1 month, more than 1 month).
GP activities were measured by number and type of contacts (surgery consultation, telephone consultation, home visit, and out-of-hours services in general practice cooperatives). Community nurse activity was measured in a subanalysis in the provincial capital, and patients were dichotomised as those who were with and without nurse contact. Time at home was calculated as days not hospitalised from diagnosis to death, left censored at 90 days; that is, the number of days possible to receive home visits. The home visit rate was calculated by the number of home visits divided by time at home in the last 90 days before death. A multivariate logistic model was fitted using the rate of home visits along with previously identified predictors. Further, a matched case-control study was conducted.
Among those who died in hospital we found the date of the ultimate admission and matched this date with randomly chosen controls (home deaths). The matching process allowed identification of 423 randomly selected cases with a corresponding control in the analysed cohort. From this, we compared the ultimate period at home for cases with matching controls. We then adjusted for the previous explored covariates. Finally, we described the population not receiving home visits. All analyses were conducted using Stata 8.
RESULTS
During the 3-year study period, 4386 adult patients (aged at least 18 years of age) died with cancer considered the primary cause of death. Figure 1 shows the place of residence, the place of death, and migration patterns of patients with cancer in the 3 months prior to death. In the total cohort only 28% died at home, 55% died in hospital, 16% in nursing homes, and for 1% the place of death was unknown. Some 9% (438) were temporarily admitted to nursing homes where they died. In the analysis of patients who were resident at home at the time of death, 2871 died in a hospital, nursing home, or an unknown place; controls consisted of 1221 patients, who died at home.
Table 1 shows patient characteristics for those who died in hospital or in nursing homes and the controls, who died at home. In the univariate analyses we found a higher proportion of women than men dying at home in the 40–65 year age group. Being married and having children made it less likely that a patient would die in hospital, although we found no association with geographic locations. On the other hand, we found that GP home visits and visits by community nurses to be strongly inversely associated with hospital death and we found an association between dying in hospital and short survival time as well as haematological cancer.
Table 1.
Characteristics of patients and controls.
| Institutional death (patients) (n = 2871, [%]) | Home death (controls) (n = 1221, [%]) | |
| Sex: | ||
| Male | 1490 (52) | 655 (54) |
| Female | 1381 (48) | 566 (46) |
| Age at death (years): | ||
| 18–39 | 35 (1) | 12 (1) |
| 40–65 | 717 (25) | 349 (29) |
| >65 | 2119 (74) | 860 (70) |
| Marital status: | ||
| Married | 1882 (66) | 916 (75) |
| Widowed, divorced or single | 989 (34) | 305 (25) |
| Children: | ||
| 0 | 1353 (47) | 505 (41) |
| ≥1 | 1518 (53) | 716 (59) |
| Primary cancer: | ||
| Lung | 609 (21) | 277 (23) |
| Colon/rectum | 273 (10) | 133 (11) |
| Breast | 205 (7) | 117 (10) |
| Prostate | 175 (6) | 90 (7) |
| Haematological | 109 (4) | 20 (1) |
| Others | 1500 (52) | 584 (48) |
| Time of diagnosis to death: | ||
| > 1 month | 2253 (78) | 1117 (91) |
| < 1 month | 618 (22) | 104 (9) |
| Geographic area: | ||
| Urban | 2209 (77) | 956 (78) |
| Rural | 662 (23) | 265 (22) |
| Nationality: | ||
| Danish | 2850 (99) | 1208 (99) |
| Other | 21 (1) | 13 (1) |
We examined the association of these variables in an adjusted multiple logistic regression model (Table 2). The strongest association was the GP paying at least one home visit during the last 3 months, but community nurse visits also had an impact. If we made a separate analysis excluding all GP services in the last 14 days, for example, the difference between the two groups declined but were still significant: OR = 0.52, 95% CI = 0.43 to 0.63. When we analysed the last period at home before last admission in a matched case-control study, matched according to time of final admittance and adjusted for the previous explored covariates, we retrieved the significant association: OR = 0.22, 95% CI = 0.15 to 0.41. The odds of hospital death consistently decreased with the rate of home visits by a GP, and the home visit rate was a strong predictor of home death (Table 3). The patients not receiving home visits (n = 653) were younger (67 years versus 73 years, t-test: P<0.001), spent shorter time at home (65 days versus 71 days, t-test: P<0.001), and more had children (65% versus 50%, Fischer's Exact test: P<0.001).
Table 2.
Associations with hospital death.
| Crude Odds ratio (95% CI) | Adjusted Odds ratio (95% CI) | |
| GP: | ||
| No home visits | 1.00 | 1.00 |
| Home visits | 0.09a (0.06 to 0.13) | 0.08a (0.06 to 0.12) |
| Community nurse: | ||
| No contact | 1.00 | 1.00 |
| Contact | 0.32a (0.24 to 0.42) | 0.36a (0.26 to 0.48) |
| Sex: | ||
| Male | 1.00 | 1.00 |
| Female | 0.96 (0.81 to 1.15) | 0.92 (0.74 to 1.14) |
| Age at death (years): | ||
| 18–39 | 0.98 (0.45 to 2.17) | 0.61 (0.24 to 1.52) |
| 40–65 | 0.86 (0.70 to 1.04) | 0.70a (0.56 to 0.90) |
| >65 | 1.00 | 1.00 |
| Marital status: | ||
| Single, divorced, widowed | 1.00 | 1.00 |
| Married | 0.65a (0.53 to 0.78) | 0.68a (0.56 to 0.85) |
| Number of children: | ||
| 0 | 1.00 | 1.00 |
| ≥1 | 0.83 (0.69 to0.99) | 0.86 (0.70 to1.06) |
| Primary cancer: | ||
| Lung | 0.87 (0.68 to1.09) | 0.99 (0.77 to1.25) |
| Colon/rectum | 0.78 (0.58 to 1.02) | 0.79 (0.58 to 1.09) |
| Breast | 0.66 (0.49 to 0.92) | 0.73 (0.51 to 1.05) |
| Prostate | 0.87 (0.62 to1.23) | 1.04 (0.71 to 1.54) |
| Haematological | 1.43 (0.81 to2.56) | 1.35 (0.74 to 2.50) |
| Others | 1.00 | 1.00 |
| Time of diagnosis to death: | ||
| >1 month | 1.00 | 1.00 |
| <1 month | 2.94a (2.17 to 3.85) | 2.27a (1.69 to 3.13) |
| Geographic area: | ||
| Urban | 1.08 (0.87 to 1.32) | 1.09 (0.87 to 1.35) |
| Rural | 1.00 | 1.00 |
P<0.05.
Table 3.
Association of rate of GP home visits with hospital death.
| Rate of home visits (per month) | Crude Odds ratio (95%CI) | Adjusted Odds ratio (95%CI) |
| 0 | 1.00 | 1.00 |
| 0.1–0.5 | 0.15 (0.10 to 0.23) | 0.14 (0.09 to 0.21) |
| 0.6–1 | 0.12 (0.08 to 0.18) | 0.11 (0.07 to 0.17) |
| 1–2 | 0.08 (0.05 to 0.11) | 0.07 (0.05 to 1.00) |
| 2–4 | 0.06 (0.04 to 0.09) | 0.06 (0.04 to 0.08) |
| >4 | 0.05 (0.03 to 0.06) | 0.05 (0.03 to 0.08) |
DISCUSSION
Summary of main findings
Our findings indicate that home visits conducted by GPs were strongly associated with the possibilities of a home death for patients with cancer and a similar trend was found for visits by community nurses. Furthermore, in agreement with previous studies,4,7-9 we found that dying at home was associated with marital status and age, and was inversely associated with short survival time (less than 1 month from diagnosis). These associations were, however, much weaker than the association with home visits.
Comparison with existing literature
Our results based on a Danish cohort fit well with recent studies, although those studies were not population-based as was ours. These studies showed that the GP's support of patients with end-stage cancer and home visits were associated with dying at home.20,21 Dying at home, however, is only one element of a ‘good death’. For example pain, symptom management, preparation for death, and opportunity to achieve a sense of completion22 are other elements of a ‘good death’. This type of study cannot illuminate all aspects of the quality of end-of-life care, however place of death can imply some of the elements.
Strengths and limitations of this study
The study had the strength of being a large population-based study with high data quality. First of all, the personal identification number from the Danish Civil Registration Register ensured reliable linkage of information. The validity of the Danish Cancer Register is high compared with other disease registers23 and the National Discharge Register concerning the administrative data has been validated finding agreement of 98.5%.18 The information about GP services was retrieved from the National Health Insurance data, which is used for remuneration of GPs and validated successively by the health authorities.
Our results should, however, be interpreted with caution. First of all, as the study is retrospective it potentially suffers from the typical weaknesses of such studies: reversal of causality, misclassification of exposure, and selection bias of cases and/or controls. Although the design of the study is retrospective, we are, by using the dates in the registers, sure that the exposure of interest, home visits by GP, and contacts with district nurse, occurs before the outcome, place of death. Furthermore, by analysing all cancer deaths in a well-defined region and timeframe we are sure that our study is not biased from differential selection of either cases or controls on the basis of their exposure status.
The most ideal design would be a prospective study but this would be difficult to conduct without risk of substantial bias. Prediction of a patient death can not be precise,24 that is, entry to a prospective study will introduce selection bias. Furthermore, it would be unethical to preclude a GP home visit if requested by the patient.
Attrition due to deterioration of the condition, drop-outs, and small sample size25,26 is a well-known problem in palliative care research, and can hamper conduction of prospective randomised clinical trials. The major problem induced by the retrospective data collection is the left censoring, that is, restricting the analysis to the last 3 months. We had to introduce left censoring (date of death minus 3 months) to get good data quality but as a consequence we cannot allow for any events prior to the 3 months before death in our study. We did, however, find similar results for those diagnosed less than 3 months before death and those who were given a diagnosis prior to the 3 months before death.
The patient's preference for a home death is a known predictor of dying at home,27 but we do not have information recorded on this in our data. As such, we cannot rule out whether the strong association between GPs paying a home visit and dying at home is a marker of such a decision being made either by the GP and the patients jointly, or by the patient alone to achieve death at home. In spite of this, we consider our results interesting, as the established dose–response relationship would seem to confirm the usefulness of GPs' visits for implementing such a decision.
In relation to care from other sources, the existence of an informal carer is also a known predictor of dying at home.8 We tried to account for this by including proxy variables (marital status, children, sex, and age) in the analyses and found that the association between GP home visits and place of death was unchanged.
The most important unobserved patient characteristic (apart from the preference for place of death and the care from other sources discussed above) is the patient's general need of care. We tried to account for this by adjusting for number of ambulatory contacts, type of cancer, sex, and age in the analyses. Given the size of the association, we find it unlikely that the strong association can be entirely explained by a patient's general need of care. Furthermore, the need for symptom management and with that, the need of acute care interventions by GPs including out-of-hours consultations, increases in the last weeks of life. We found, however, that the association persisted eliminating all services the last 2 weeks in the adjusted regression and in the matched case-control study, matching according to the period before the last admission of the patient.
We investigated whether the association of home visits with home death was a result of different exposure time, that is, time not in hospital. However, stratifying on time at home we found a significant adjusted and unadjusted association. Furthermore, our analysis identified the rate of home visits as a predictor of place of death which showed a strong dose–response relationship with respect to place of death. In the latter analysis the amount of time spent at home in the last 3 months is implicitly accounted for, since the rate is the number of home visits relative to time spent at home. The interpretation is, therefore, that among patients spending similar amounts of time at home, those with more home visits have a higher chance of dying at home.
Findings regarding home visits by community nurses seemed to show the same tendency as home visits by a GP, but this result is entirely based on an urban population and can only be extrapolated to the entire population with caution.
Implications for further research or clinical practice
The results of the present study could be of interest to health service planners and health authorities. The organisation and the services of the healthcare system seems more important than patient-related factors in meeting, not just the needs of patients with late-stage cancer but probably also the needs of patients with other end-stage, non-malignant disease.28 In this study, the GP seems to have an important role, especially in the last weeks before death. To increase the opportunity for patients with cancer to die at home, more research is needed on the particular role of the GP and to identify barriers for providing home visits in end-stage care.
Acknowledgments
We would like to thank G Engholm and HH Storm from the Department of Cancer Prevention & Documentation, Danish Cancer Society, for inspiring input in the planning phase and access to data from the Danish Cancer Register. We would also like to thank P Pedersen from the Municipality of Odense for access to data from the Department for the Elderly and Disabled in Odense.
Funding body
This study was funded by The Health Insurance Foundation (2001B116 and 2002B025), The Danish Research Foundation for General Practice (586-193259), and The Danish College of GPs Research Scholarship 2001
Ethics committee
None
Competing interests
None
REFERENCES
- 1.Townsend J, Frank AO, Fermont D, et al. Terminal cancer care and patients preference for place of death: a prospective study. BMJ. 1990;301:415–417. doi: 10.1136/bmj.301.6749.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Higginson IJ, Sen-Gupta GJ. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. J Palliat Med. 2000;3(3):287–300. doi: 10.1089/jpm.2000.3.287. [DOI] [PubMed] [Google Scholar]
- 3.Tiernan E, O'Connor M, O'Siorain L, Kearney M. A prospective study of preferred versus actual place of death among patients referred to a palliative care home-care service. Ir Med J. 2002;95(8):232–235. [PubMed] [Google Scholar]
- 4.Higginson I, Astin P, Dolan S. Where do patients with cancer die? Ten-year trends in the place of death of patients with cancer in England. Palliat Med. 1998;12(5):353–363. doi: 10.1191/026921698672530176. [DOI] [PubMed] [Google Scholar]
- 5.Weitzen S, Teno JM, Fennell M, Mor V. Factors associated with site of death: a national study of where people die. Med Care. 2003;41(2):323–335. doi: 10.1097/01.MLR.0000044913.37084.27. [DOI] [PubMed] [Google Scholar]
- 6.Hunt RW, Fazekas BS, Luke CG, Roder DM. Where patients with cancer die in South Australia, 1990–1999: a population-based review. Med J Aust. 2001;175(10):526–529. doi: 10.5694/j.1326-5377.2001.tb143710.x. [DOI] [PubMed] [Google Scholar]
- 7.Bruera E, Russell N, Sweeney C, et al. Place of death and its predictors for local patients registered at a comprehensive cancer center. J Clin Oncol. 2002;20(8):2127–2133. doi: 10.1200/JCO.2002.08.138. [DOI] [PubMed] [Google Scholar]
- 8.Grande GE, Addington-Hall JM, Todd CJ. Place of death and access to home care services: are certain patient groups at a disadvantage? Soc Sci Med. 1998;47(5):565–579. doi: 10.1016/s0277-9536(98)00115-4. [DOI] [PubMed] [Google Scholar]
- 9.Gallo WT, Baker MJ, Bradley EH. Factors associated with home versus institutional death among patients with cancer in Connecticut. J Am Geriatr Soc. 2001;49(6):771–777. doi: 10.1046/j.1532-5415.2001.49154.x. [DOI] [PubMed] [Google Scholar]
- 10.Jordhoy MS, Fayers P, Saltnes T, et al. A palliative care intervention and death at home: a cluster randomised trial. Lancet. 2000;356:888–893. doi: 10.1016/s0140-6736(00)02678-7. [DOI] [PubMed] [Google Scholar]
- 11.Hanks GW, Robbins M, Sharp D, et al. The imPaCT study: a randomised controlled trial to evaluate a hospital palliative care team. Br J Cancer. 2002;87(7):733–739. doi: 10.1038/sj.bjc.6600522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salisbury C, Bosanquet N, Wilkinson EK, et al. The impact of different models of specialist palliative care on patients' quality of life: a systematic literature review. Palliat Med. 1999;1(13):3–17. doi: 10.1191/026921699677461429. [DOI] [PubMed] [Google Scholar]
- 13.Smeenk FW, van Haastregt JC, de Witte LP, Crebolder HF. Effectiveness of home care programmes for patients with incurable cancer on their quality of life and time spent in hospital: systematic review. BMJ. 1998;316:1939–1944. doi: 10.1136/bmj.316.7149.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higginson IJ, Finlay IG, Goodwin D, et al. Is there evidence that palliative care teams alter end-of-life experiences of patients and their caregivers? J Pain Symptom Manage. 2003;25(2):150–168. doi: 10.1016/s0885-3924(02)00599-7. [DOI] [PubMed] [Google Scholar]
- 15.Christiansen T. Organisation and financing of the Danish health care system. Health Policy. 2002;59:107–118. doi: 10.1016/s0168-8510(01)00201-9. [DOI] [PubMed] [Google Scholar]
- 16.Storm HH, Michelsen EV, Clemmensen I, Pihl J. The Danish Cancer Registry: history, content, quality and use. Dan Med Bull. 1997;44(5):535–39. [PubMed] [Google Scholar]
- 17.Juel K, Helweg-Larsen K. The Danish Register of Causes of Death. Dan Med Bull. 1999;46(4):354–357. [PubMed] [Google Scholar]
- 18.Andersen TF, Madsen M, Jørgensen J, et al. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull. 1999;46(3):263–268. [PubMed] [Google Scholar]
- 19.Malig C. The civil registration system in Denmark. Bethesda, MA: International Institute for Vital Registration and Statistics; 1996. Technical paper No 66. [Google Scholar]
- 20.Brazil K, Bedard M, Willison K. Factors associated with home death for individuals who receive home support services: a retrospective cohort study. BMC Palliat Care. 2002;1(1):2. doi: 10.1186/1472-684X-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cantwell P, Turco S, Brenneis C, et al. Predictors of home death in palliative care patients with cancer. J Palliat Care. 2000;16(1):23–28. [PubMed] [Google Scholar]
- 22.Steinhauser KE, Christakis NA, Clipp EC, et al. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–2482. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 23.Storm HH. Validity of death certificates for patients with cancer in Denmark 1977. Copenhagen: The Danish Cancer Registry; 1984. [Google Scholar]
- 24.Glare P, Virik K, Jones M, et al. A systematic review of physicians' survival predictions in terminally ill patients with cancer. BMJ. 2003;327:195. doi: 10.1136/bmj.327.7408.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaasa S, Loge JH. Quality-of-life assessment in palliative care. Lancet Oncol. 2002;3:175–182. doi: 10.1016/s1470-2045(02)00682-4. [DOI] [PubMed] [Google Scholar]
- 26.Higginson IJ, Finlay I, Goodwin D, et al. Do hospital-based palliative teams improve care for patients or families at the end of life? J Pain Symptom Manage. 2002;23(2):96–106. doi: 10.1016/s0885-3924(01)00406-7. [DOI] [PubMed] [Google Scholar]
- 27.Gyllenhammar E, Thoren-Todoulos E, Strang P, et al. Predictive factors for home deaths among patients with cancer in Swedish palliative home care. Support Care Cancer. 2003;11(9):560–567. doi: 10.1007/s00520-003-0487-z. [DOI] [PubMed] [Google Scholar]
- 28.McKinley RK, Stokes T, Exley C, Field D. Care of people dying with malignant and cardiorespiratory disease in general practice. Br J Gen Pract. 2004;54:909–913. [PMC free article] [PubMed] [Google Scholar]


