Abstract
Hypothesis
It was hypothesized that laser-Doppler vibrometry measurements of umbo velocity in aerated middle ears with conductive loss can differentiate ossicular interruptions, stapes fixations, and mallear fixations. More generally, we hypothesize that laser-Doppler vibrometry measurements of umbo velocity can give information about how differences in the impedance that the ossicles work against affect middle-ear function.
Background
Laser-Doppler vibrometry is a well-established research tool for exploring middle-ear function. The authors wished to investigate its potential as a clinical tool for differential diagnosis of the cause of conductive hearing loss.
Methods
Laser-Doppler vibrometry was used to investigate the relationship between the sound-induced velocity of the tympanic membrane at the umbo and the cause of conductive hearing loss when the tympanic membrane was normal and the middle ear was aerated. The results of measurements in 17 adult ears before exploratory tympanotomy were compared with the surgically determined cause of the hearing loss. The authors also measured the motion of the umbo in 10 patients who had undergone successful small-fenestra stapedectomy procedures. In all the studied ears, pure-tone audiograms were measured at the time of laser-Doppler vibrometry testing.
Results
There were clear statistical differences between the umbo velocity in normal ears and in ears with different ossicular pathologic conditions. There was also a clear separation of the results between ears with ossicular interruptions and ossicular fixation. The pattern of laser-Doppler vibrometry measurements in poststapedectomy ears approximated the pattern in ears with ossicular interruptions.
Conclusion
Comparison of laser-Doppler vibrometry results and audiometry may be a sensitive and selective indicator of ossicular pathologic conditions as well as a useful tool for investigating middle ear function.
Keywords: Laser-Doppler vibrometry, Conductive hearing loss, Middle ear function, Audiometry
Laser-Doppler vibrometry (LDV) has been used to investigate middle ear function in animals (1–3), human temporal bones (4–10), and living humans (11–18). Most investigations using LDV in living humans have been concerned with the sound-induced motion of the tympanic membrane in normal ears (11–16), but some studies have investigated tympanic membrane motion in patients with hearing loss (11,16,18) as well as intraoperative measurements of ossicular motion (17). Although the direct measurement of tympanic membrane mobility seems to be a natural tool for investigating conductive hearing loss, little work has been published to explore its possibilities.
The potential utility of LDV in the differential diagnosis of conductive hearing loss with an intact tympanic membrane is of interest, because neither otology, audiometry, nor tympanometry can reliably differentiate different ossicular pathologic conditions before surgery (19,20), Reliable presurgical diagnosis of ossicular interruption, stapes fixation, and mallear fixation would permit better preoperative counseling and better surgical planning, and may help decrease the incidence of surgical failures.
In the current study, we report preoperative LDV measurements from 17 patients with conductive hearing loss and a normal, intact tympanic membrane. The LDV measurements of the velocity of the tympanic membrane made near the umbo demonstrated a correlation between preoperative tympanic membrane mobility and the intraoperative diagnosis of ossicular interruption or fixation. We also report postsurgical measurements of the mobility of the tympanic membrane after small-fenestra stapedectomy in 10 ears.
PATIENTS AND METHODS
Our methods were approved by the Human Studies Committee of the Massachusetts Eye and Ear Infirmary. The methods were designed for use in adult patients in the outpatient setting. The laser is a noncontact device. The only instrument in contact with the patient was a standard otologic speculum used to view the tympanic membrane. The duration of the entire measurement session, from patient entry to exit, was less than 10 minutes. There was no discomfort, and no anesthesia was necessary.
Laser and stimulus assembly
The stimulus and measurement system is schematized in Figure 1. The patient lay supine on an examination table with head turned to raise the ear to be measured. An otologist (S.N.M.) positioned a standard otology microscope to observe the tympanic membrane. Mounted on the microscope was a laser-vibrometer and aiming-prism assembly (a Polytec HLV-1000; Polytec PI, California, U.S.A.). A glass-backed sound coupler and ear speculum, with associated sound source and probe-tube microphone, was placed in the ear canal to allow visualization of the umbo and the light reflex of the tympanic membrane (15). The tip of the soft silicone probe tube was generally within 5 mm of the tympanic membrane. No attempt was made to achieve a tight seal between the speculum and the ear canal. The joystick-controlled prism mounted under the microscope objective was used to position the 0.1-mm laser spot just anterior and inferior to the umbo, at the apex of the light reflex. The laser spot was confocal with the microscope. The area of the light reflex near the umbo was chosen (1) to maximize the light reflected back to the laser measurement system without the use of reflectors placed on the tympanic membrane, and (2) to measure velocity near the umbo, the most peripheral part of the ossicular chain. A series of three to seven measurements was initiated when the laser was focused on the measurement site. (The laser, aiming prism assembly, and ear coupler are available from Polytec PI for approximately $50,000 US. The stimulus generation, recording, and analysis system described below was custom assembled but could be reproduced for approximately $20,000 US.)
FIG. 1.
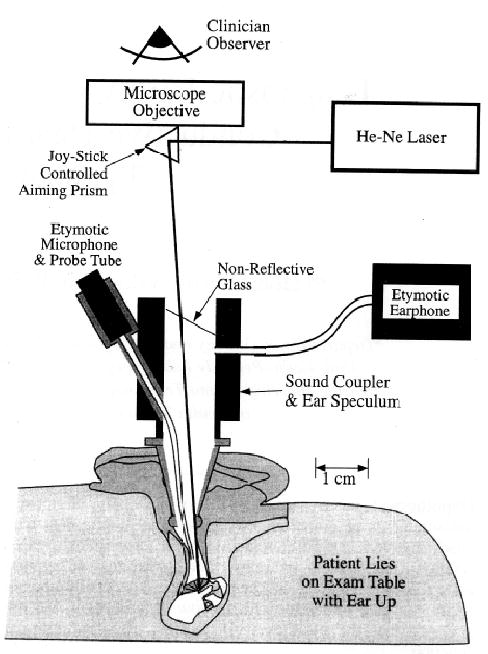
Laser-Doppler vibrometer–based measurement system, consisting of a helium-neon laser, controlling hardware, and a joystick-controlled aiming prism. Both the laser and the prism are mounted on a standard operating microscope, allowing the clinician observer to see and focus the laser at a point in the viewing field. The laser and the microscope are confocal. A standard stainless Steel speculum couples to the glass-backed sound coupler with attachments for a sound source and a probe tube microphone The long nylon probe tube is threaded through the coupler and terminates approximately 5 mm beyond the speculum tip. The clinician places the coupler/speculum so as to view the umbo and the light reflex. The laser is then positioned on the naturally reflective light reflex to get adequate reflected light back to the sensor in the laser assembly. A too-low reflectivity leads to poor signal to noise on the laser channel.
Stimulus generation and response measurement
Stimulus generation and response measurement were managed via a DOS-controlled Intel computer with an Ariel DSP16+ board (Ariel Corporation, NJ, U.S.A.) with two digital-to-analog outputs and two analog-to-digital inputs. The board was controlled via Sysld software (Sysld Inc., CA). With a keystroke command, an acoustic stimulus, consisting of a nine-tone complex, 1.1 second in duration, was generated by the earphone coupled to the speculum (Fig. 1). Each of the nine tonal components was a harmonic of a 100-Hz base frequency. The frequencies of the nine stimulus components were 300, 500, 700, 1,000, 1,500, 2,000, 3,000, 4,000, and 6,000 Hz. The phases of the nine components were fixed from stimulus to stimulus but were randomly arranged within the stimulus. The stimulus sounded like a dissonant chord. A manual attenuator was used to vary the level of the stimulus. Measurements were usually performed at the maximum stimulus level of approximately 90 dB SPL.
Synchronous with the sound stimulus, the DSP-16+ analog-to-digital converters digitized the voltage output from the probe microphone and the laser demodulator/controller (Polytec HLV-1000). (The demodulator/controller output voltage was proportional to the instantaneous velocity of the tympanic membrane.) These digitized waveforms were then separated into various frequency components by spectral analysis using Fourier transforms (Fig. 2), The transforms covered the range from 100 Hz to 12,000 Hz with a resolution of 100 Hz and showed the microphone and velocity responses at the nine stimulus frequencies as well as at the in-between frequencies. Comparisons of the microphone and laser output voltages at the stimulus frequencies (the signal) with the output voltages at the in-between frequencies (an estimate of noise) allowed calculations of the signal-to-noise ratio of each stimulus component within each measurement. The determination of the signal-to-noise ratio was crucial to our analyses because small motions of the patient’s head, relative to the microscope and laser, produced large fluctuations in the amount of light reflected back toward the laser, with associated large variations in the noise on the laser output channel. The size of the signal and noise in each measurement was monitored by observation of the spectrum of the laser output. Measurements were generally repeated until there were three measurements with low noise floor. With one exception, only data gathered with at least a 20-dB signal-to-noise ratio are presented in this article. The exception is a case of small umbo velocities caused by mallear fixation, wherein we accepted data with a 10-dB signal-to-noise ratio.
FIG. 2.
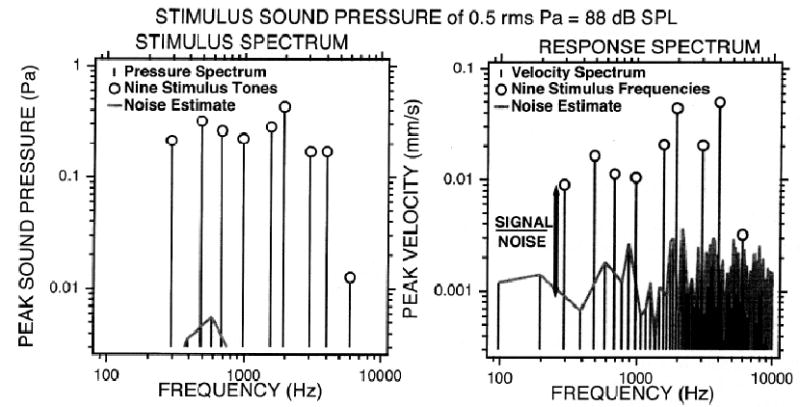
Sound stimulus and laser response spectra from a typical measurement. The sound pressure of the total stimulus was 88 dB SPL. Left, spectrum of the stimulus sound pressure. Right, spectrum of the velocity response. The frequency resolution of each spectrum is 100 Hz. Spectrum lines with magnitudes less than the minimum value of the ordinates are not plotted. Spectral lines at the nine stimulus frequencies are marked with circles. The noise estimate is created by connecting the lines at the nonstimulus frequencies. The noise about each stimulus frequency is determined by averaging the nonstimulus lines adjacent to the stimulus frequencies. Whereas the noise in the sound pressure stimulus was low throughout, the noise in the velocity response signal varied from measurement to measurement depending on the stability of the subject’s head and the amount of light reflected back to the laser during the measurement.
The result of each of the LDV and probe-microphone measurements was the calculation of the umbo-velocity transfer function. The transfer function was defined as the complex ratio of the measured velocity to the measured sound pressure in the ear canal near the tympanic membrane. The complex nature of the transfer function is due to the potential for differences between the phases of the velocity and sound pressure; this phase difference is reported as the angle of the transfer function. These phase differences tell us something about the mechanics determining the response, e.g., a phase angle of positive 0.25 periods (or 90 degrees) is consistent with a stiffness-bound system where umbo displacement (the integral of velocity) is in phase with the sound pressure.
Subjects
Presurgical group
This group consisted of 17 ears of adult patients with intact, normal tympanic membranes, aerated middle ears, and significant conductive hearing loss; the average air-bone gap at 500, 1,000, 2,000, and 4,000 Hz was 26.5 dB with a standard error of the mean of 3.6 dB (Table 1). Each patient underwent a complete otologic examination, including standard pure-tone audiometry, and was scheduled to undergo middle-ear surgery by one of the four otologists at the Massachusetts Eye and Ear Infirmary (Drs. Nadol, McKenna, Rauch, and Merchant). Laser-Doppler vibrometry was usually performed on the day of the audiogram and preceded surgery by 2 days to 2 weeks. In 15 of the 17 cases, the otologist performed the surgical procedure with no knowledge of the LDV results. In 2 cases with unusual histories, the otologist requested the results of the LDV measurements before surgery. The diagnoses determined during surgery included fixed footplate resulting from otosclerosis (12 ears), epitympanic fixation of the malleus and incus caused by tympanosclerosis (1 ear), fracture of the malleus neck (1 ear), and erosion of the long process of the incus resulting in a fibrous union between the incus and stapes (3 ears). The presurgical audiometric data from the 12 patients with stapes fixation (four-tone average air-bone gap of 25.5 ± 4.5 dB), 1 patient with fixed malleus and incus (four-tone average air-bone gap of 13.8 dB) and the 4 patients with confirmed ossicular interruption and fibrous union (four-tone average air-bone gap of 32.5 ± 6.8 dB) are given in Tables 2, 3, and 4.
TABLE 1.
Air-bone gaps prior to exploratory tympanotomy
| 250 Hz | 500 Hz | 1,000 Hz | 2,000 Hz | 4,000 Hz | 4-tone averagea | |
|---|---|---|---|---|---|---|
| N | 13 | 17 | 17 | 17 | 17 | 17 |
| Mean | 46.2 | 34.1 | 29.4 | 15.9 | 26.5 | 26.5 |
| Standard error | 4.9 | 3.2 | 4.0 | 4.4 | 4.7 | 3.6 |
Average of 500, 1,000, 2,000, and 4,000 Hz values
TABLE 2.
Air-bone gaps in cases with stapes fixation
| 250 Hz | 500 Hz | 1,000 Hz | 2,000 Hz | 4,000 Hz | 4-tone average | |
|---|---|---|---|---|---|---|
| N | 8 | 12 | 12 | 12 | 12 | 12 |
| Mean | 47.5 | 34.6 | 27.9 | 15.8 | 23.8 | 25.5 |
| Standard error | 5.5 | 3.7 | 5.0 | 5.3 | 5.9 | 4.5 |
TABLE 3.
Air-bone gaps in one case of malleo-incudal fixation
| 250 Hz | 500 Hz | 1,000 Hz | 2,000 Hz | 4,000 Hz | 4-tone average | |
|---|---|---|---|---|---|---|
| Ear P56L | 45 | 35 | 25 | −10 | 5 | 13.8 |
TABLE 4.
Air-bone gaps in cases with ossicular interruption or fibrous union
| 250 Hz | 500 Hz | 1,000 Hz | 2,000 Hz | 4,000 Hz | 4-tone average | |
|---|---|---|---|---|---|---|
| N | 4 | 4 | 4 | 4 | 4 | 4 |
| Mean | 43.8 | 32.5 | 35.0 | 22.5 | 40.0 | 32.5 |
| Standard error | 13.0 | 8.8 | 8.9 | 8.5 | 2.9 | 6.8 |
Poststapedectomy group
This group contained 10 ears with LDV measurements made 5 weeks to 11 years after successful small-fenestra stapedectomy with the placement of a 0.6-mm diameter Teflon-wire prosthesis, including 5 ears from the presurgical group. The surgical procedure included the placement of a small amount of Gelfoam around the lower end of the prosthesis; no vein graft was used across the fenestra (21). Each ear was examined by an otologist immediately before the LDV measurements, and an audiogram was performed. The postsurgical air-bone gaps (four-tone average of 5.2 ± 1.5 dB) from this group are summarized in Table 5.
TABLE 5.
Poststapedectomy air-bone gaps
| 250 Hz | 500 Hz | 1,000 Hz | 2,000 Hz | 4,000 Hz | 4-tone average | |
|---|---|---|---|---|---|---|
| N | 10.0 | 10.0 | 10.0 | 10.0 | 10.0 | 10.0 |
| Mean | 11.5 | 3.0 | 4.0 | 2.0 | 5.5 | 5.2 |
| Standard error | 3.3 | 1.9 | 2.3 | 2.6 | 3.2 | 1.5 |
Normal data group
In a separate study, measurements were also made in 73 normal middle ears (air-bone gaps of ≤10 dB at frequencies >250 Hz) from 48 subjects/patients. These ears included those of research subjects as well as the contralateral normal ears of some of our patients with unilateral hearing loss. The normal results have been described in a preliminary report (15), and a full publication is being prepared. The results from this group were similar to those in previous reports of LDV measurements from normal ears (12,13), Repeated LDV measurements made in this group showed good reproducibility (within a factor of 1.5) and reliability of the measurement results (15).
RESULTS
Laser-Doppler vibrometry measurements in the normal and presurgical groups
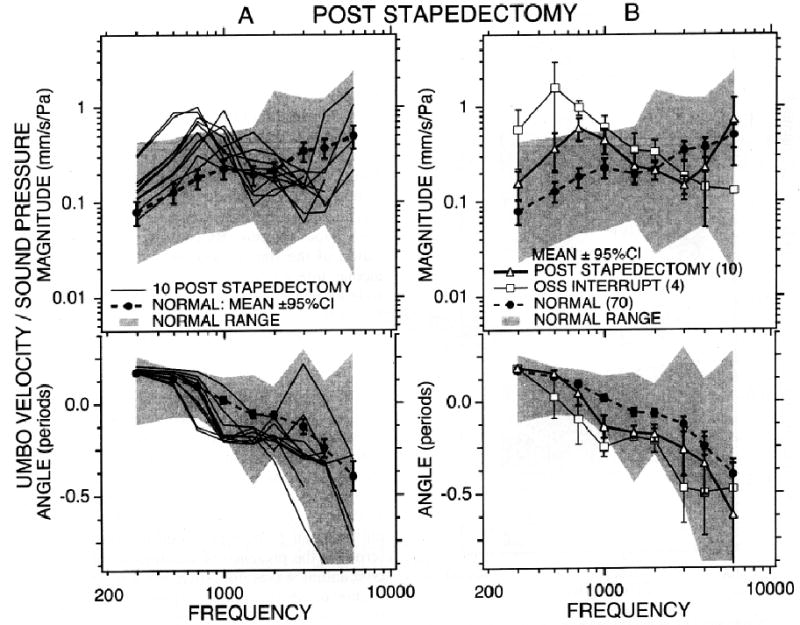
The LDV measurements showed clear differences between normal ears and ears with ossicular pathologic conditions. These differences are shown in Figures 3 and 4. Figure 3A illustrates the individuals and mean of the measurements made in the 73 normal ears. Figure 3B illustrates that the 12 cases of otosclerotic stapes-footplate fixation had velocity transfer functions that fell within the range of normal measurements but were generally lower than the normal mean magnitude and commonly had angles that were more positive than the normal mean, especially at frequencies less than or equal to 1,000 Hz. The one case of malleoincudal fixation, secondary to epitympanic tympanosclerosis, had a velocity magnitude much lower than that in either the normal group or the fixed stapes group (a factor of 3–4, equivalent to 10–12 dB, smaller than the lowest normal measurements) and an angle that was generally more positive than the normal mean.
FIG. 3.
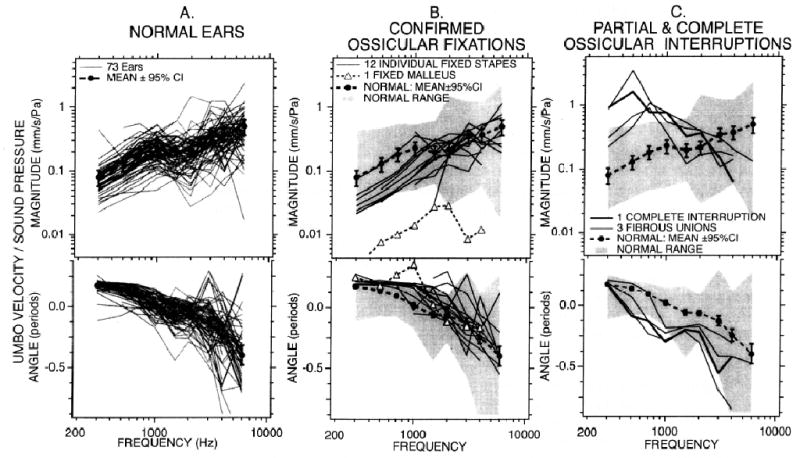
Magnitude and angle of umbo velocity transfer functions in normal ears and two patient populations. The transfer function is defined as the ratio of the laser-Doppler vibrometry (LDV) measured velocity near the umbo and the sound pressure measured near the tympanic membrane by the probe microphone. The upper plot of each panel shows the transfer function magnitude in units of mm/s/Pa (velocity/sound pressure). The lower plot shows the angle of the transfer function, which is equivalent to the phase of the velocity minus the phase of the sound pressure. Positive angles occur when the velocity leads the sound pressure; negative angles occur when the velocity lags the sound pressure. A, Normal ears. The measured transfer function in 73 individual ears with no air-bone gaps are illustrated along with the mean and the 95% confidence interval (± 1.96 times the standard error) around the mean. B, Confirmed ossicular fixations. The LDV results from 12 ears with surgically confirmed fixed stapes (due to otosclerosis) and one ear with fixed malleus and incus head (due to fibrous adhesions in the epitympanic cavity) are compared with the mean and range of the normal population. Measurements in the 12 fixed stapes cases fall within the normal range but are generally lower than the normal mean magnitude and have angles that are more positive than the normal mean. The one case of malleoincudal fixation has a velocity magnitude that is as much as a factor of 4 (12 dB) smaller than the lowest normal measurements and an angle that is generally more positive than the normal mean. C, Partial and complete ossicular interruptions. LDV results from four ears with surgically confirmed ossicular interruptions (one complete interruption at the neck of the malleus and 3 cases of erosion of the bone of the incus resulting in a fibrous attachment of the incus and stapes head) are compared with the mean and range of the normal population. These four cases have low-frequency velocities that are larger than the normal range and high-frequency magnitudes that are generally smaller than the normal mean. The angles of the four interruption cases are more negative than the normal mean but generally fall within the normal range.
FIG. 4.
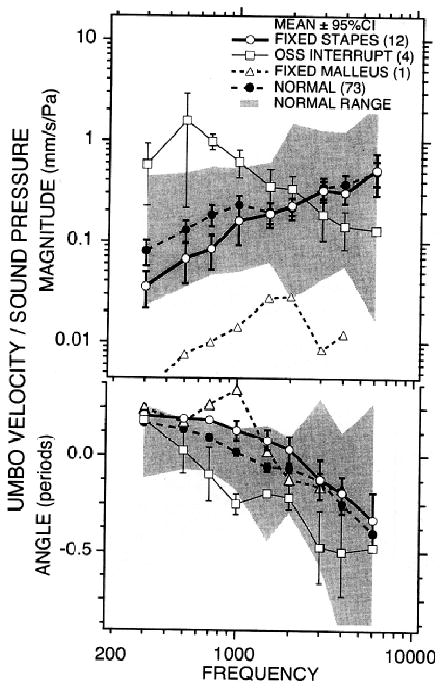
Comparison of the means and variance of the patient groups with the normal group. The four curves in each panel represent the mean magnitude and angle in four measurements groups: normal ears (n = 73), fixed stapes (n = 12), ossicular interruption (n = 4) and fixed malleus (n = 1). The shaded area shows the range of the normal measurements. The bars are the 95% confidence limits (1.95 times the standard error of the mean) about the means. Small or no overlaps between the means and confidence limits indicate significant differences between the populations.
The LDV results from 4 ears with surgically confirmed ossicular interruptions (1 complete interruption at the neck of the malleus and 3 cases of erosion of the long process of the incus resulting in a fibrous union between the incus and stapes head) are compared with the mean and range of the normal population in Figure 3C. There were no clear differences within the LDV measurements of these 4 cases. They all had low-frequency velocity magnitudes that were larger than the normal range and high-frequency magnitudes that were generally smaller than the normal mean. The angles of the four interruption cases were more negative than the normal mean but generally fell within the normal range.
The means and 95% confidence intervals of the umbo velocity transfer functions in the patient populations with different pathologic conditions are compared with the normal mean in Figure 4. This comparison demonstrates significant statistical differences between the magnitudes and angles in the normal population and those in the patient populations at many frequencies. The normal and fixed-stapes populations were significantly different in magnitude at frequencies less than 1,500 Hz and in angle at frequencies less than 3,000 Hz. (Student’s t tests demonstrated that the probability the magnitudes at frequencies <1,500 Hz and angles at frequencies <3,000 Hz were the same in the two populations was generally <1%.) At frequencies of 3,000 Hz and above, the magnitudes and angles of these two populations were statistically inseparable. The magnitudes and angles of the ossicular-interruption group were significantly different (generally at the <1% level or lower) from the normal group at most measured frequencies; the one exception was that the angles of the two groups at 300 Hz were not separable. The magnitudes and angles of the fixed-stapes and ossicular-interruption groups were statistically separable from each other (at the 2% or lower level) at all frequencies. The magnitude of the fixed-malleus case was unique in its low values at all frequencies, and extreme in its angle at 750 and 1,000 Hz. At other frequencies, the angles in the fixed-malleus case fell within the normal range.
The wide range of magnitudes and angles observed in the normal population will interfere with the diagnostic value of LDV alone in cases of stapes fixation, where the changes in stapes velocity induced by a pathologic condition are small. The larger changes in magnitude and angle seen in the cases with ossicular interruption and the extremely low magnitude in the case of malleus fixation suggest that LDV, by itself, may reliably separate these two ossicular pathologic condition from responses in normal ears.
Laser-Doppler vibrometry measurements in the poststapedectomy group
We also made LDV measurements of umbo velocity after 10 successful small-fenestra stapedectomy (21) procedures; the results are compared with the normal and ossicular-interrupted populations in Figure 5. The poststapedectomy results were generally intermediate in magnitude and angle to the normal and ossicular-interruption groups. The largest variations from normal magnitudes in the poststapedectomy ears were at frequencies of 1,000 Hz and below, whereas the angle between umbo velocity and sound pressure was most different in the poststapedectomy cases at frequencies of 1,000 Hz and above. Student’s t test analyses demonstrated statistically significant differences (at the 2% or better level) in magnitude between the normal and poststapedectomy groups at all frequencies except 1,500 and 2,000 Hz. The angles of the two groups were significantly different (at the 1% or better level) at all frequencies above 300 Hz. Statistical comparisons between the poststapedectomy and ossicular-interruption groups showed significant differences in magnitude (at the 1% level) at frequencies less than 1,000 Hz and significant differences in angle at 500, 700, and 1,000 Hz. The data in Figure 5B suggest a similarity in middle-ear mechanics in cases of ossicular interruption and stapedectomy. The idea that a small-fenestra stapedectomy, in common with ossicular interruption, acts to decrease the impedance that loads the ossicular chain will be a point of discussion.
FIG. 5.
Magnitude and angle of umbo velocity transfer functions in ears after successful small fenestra stapedectomy with a 0.6 mm piston. A, Comparison of laser-Doppler vibrometry (LDV) measurements in the 10 individual post-stapedectomy cases with the mean, 95% confidence interval, and range of normal measurements. B, Comparison of the mean ± 95% confidence limits in normal subjects, poststapedectomy patients, and ossicular interruption patients.
DISCUSSION
Summary of results and comparison with other reports
Our umbo velocity measurements showed statistical differences in the magnitude and phase of tympanic-membrane velocity between several groups of ears with normal tympanic membranes and aerated middle ears. Compared with normal ears, the umbos of ears with a fixed stapes had a reduced magnitude of motion and a larger phase angle at frequencies of 1,000 Hz and lower. The “fixed stapes” pattern was consistent with an increase in stiffness of the middle ear; however, the factor of approximately 1.5 (3 dB) decrease in magnitude between mean normal and mean fixed stapes ears was small compared with the factor of 10 range of magnitudes in normal ears. Such a small change in stiffness was consistent with tympanometric estimates in cases with stapes fixation and was believed to be caused by the action of the incudomallear and incudostapedial joints (22–24), where the compliant joints allow motion of the tympanic membrane even though the stapes is immobilized. The one ear with a fixed malleus and incus showed a much larger decrease in umbo velocity, more than a factor of 10 (20 dB) relative to normal, at most of the frequencies tested.
Interruption of the ossicular chain, either complete or partial, resulted in an increase in the magnitude of umbo velocity at frequencies less than 1,000 Hz and a decrease in velocity magnitude at higher frequencies. These changes in magnitude were associated with more negative angles. The changes at low frequencies were consistent with a decrease in the stiffness of the ear. The decreases in magnitude of umbo motion relative to normal values at higher frequencies suggested an increase in the magnitude of the ear’s impedance; however, how an interruption could produce an increase in middle-ear impedance was not clear. Some studies in animals have demonstrated narrow-band increases in middle-ear impedance resulting from ossicular interruption (25–29). Some of these studies have described this increase as an increase in the mass of the ear (25,26), whereas another has explained the decreased velocity magnitude and decrease in phase as a change in the spatial patterns of tympanic membrane motion (29).
One problem in comparing our interrupted-chain results with those of previous animal studies is the relatively poor frequency resolution in our measurements. In an effort to maximize the information available in a minimum amount of time, we restricted our measurements to nine frequencies that are separated by roughly half-octave intervals. Such sampling of the frequency domain is insufficient to reveal the sharply tuned middle-ear responses that are apparent in animals with interrupted ossicular chains (25–29).
The changes in umbo velocity that we report in the three presurgery groups are very similar to those reported by Huber et al. (18) in an LDV study of a similar patient base.
Significance for clinical diagnosis
The 17 presurgical cases were homogenous in the normal appearance of the tympanic membrane and in the pattern and severity of their presurgical hearing levels. All 3 patients with fibrous union of the incus and stapes had presurgical air-bone gaps that were difficult to distinguish from the typical air-bone gaps in stapes fixation. Furthermore, 2 of the stapes-fixation patients had extreme air-bone gaps of 50 to 60 dB similar to the gap observed in the 1 patient with complete ossicular interruption. The only significant difference between the air-bone gaps in the stapes-fixation and ossicular-interruption groups was seen at 4,000 Hz (the probability that the two-gaps come from the same population is less than 1 %) where the stapes-fixation group on average had an air-bone gap that was 16 db smaller (Tables 2 and 3).
The next few sections will consider whether LDV is a reliable diagnostic tool either by itself or in combination with pure-tone audiometry. Such a tool would be useful in the preoperative planning and counseling of patients with conductive hearing loss and normal tympanic membranes with aerated middle ears. LDV is quick (reliable measurements in <10 minutes) and at least as easy as tympanometry and reflectance measurements (19,30,31). Unlike tympanometry (19) and some reflectance protocol (29), LDV does not require sealing the sound source in the ear canal and varying the external-ear pressure. The relative diagnostic utility of LDV and other multi-frequency measures of middle-ear state needs to be investigated, but all these techniques have the potential to be more sensitive and specific than single-tone tympanometry (20,30,31).
Diagnostic utility of laser-Doppler vibrometry alone
Our results suggest clear statistical differences between the mean umbo velocities of groups with normal middle ears or those with various pathologic conditions (Fig. 4), but the clinical significance of individual measurements is less clear (Fig. 3). Figure 3B indicates that it would be difficult to differentiate any of the results from individual ears with stapes fixation from responses in normal ears, given the nearly complete overlapping of the ranges of the measurements in normal ears and ears with stapes fixation. By contrast, there was a clear separation of the four measurements made in ears with ossicular interruptions from the normal ranges of magnitude and angle at low frequencies (Fig. 3C). The single measurement in an ear with fixed malleus was also clearly different from the normal range.
Diagnostic utility of laser-Doppler vibrometry combined with audiometry
Although the LDV may not be a sensitive indicator of pathologic changes in cases of stapes fixation, LDV does clearly separate ossicular fixation from ossicular interruptions (Figs. 3 and 4). This separation suggests that LDV is a potentially sensitive tool for separating different ossicular pathologic conditions once audiometry determines the presence of a conductive hearing loss. The conceptual bases for such separations are shown in Figure 6, which compares presurgical air-bone gaps in three patients with different pathologic conditions with the normalized umbo velocity, the ratio (in decibels) of the umbo velocity measured in the individual ear with pathologic changes and the mean umbo velocity of normal ears.
FIG. 6.
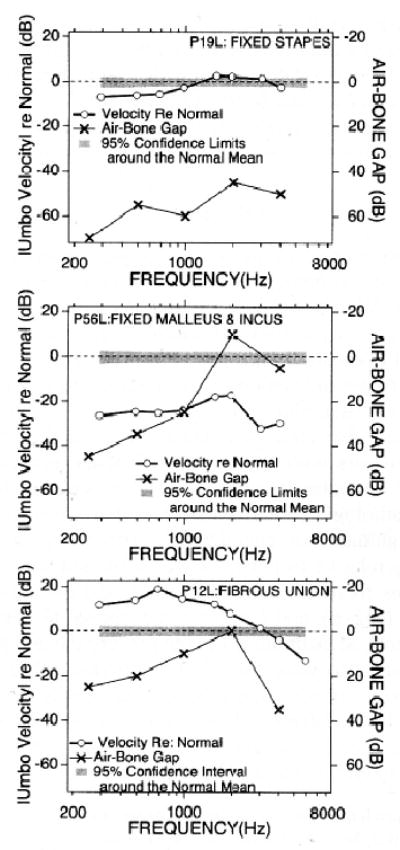
Comparisons of laser-Doppler vibrometry (LDV) changes and air-bone gaps in three cases with different ossicular pathologic features. The left-hand ordinates scale the ratio of the magnitude of the umbo velocity measured in the individual ear to the normal mean magnitude. This ratio is plotted with open circles for different individual cases in the three panels. The right-hand ordinates scales presurgical air-bone gaps (plotted with Xs) in the same ears. The three cases include fixed stapes, fixed malleus and incus, and an erosion of the bony incus with a resultant fibrous union of the incus and stapes heads.
The top panel of Figure 6 compares the presurgical audiologically determined air-bone gap and the magnitude of the presurgical normalized umbo velocity measured in one patient, who at subsequent surgery was found to have a fixed stapes footplate. The patient had a 45-dB to 60-dB presurgical conductive hearing loss, but there was only a 5-dB decrease, relative to normal, in the umbo velocity magnitude, and that only at frequencies below 1,000 Hz. We suggest that the action of the compliant ossicular joints uncoupled the motion of the umbo and the fixed stapes, allowing nearly normal motion of the tympanic membrane and umbo despite the fixed stapes and the large conductive hearing loss. Similar patterns were observed in all of our patients with stapes fixation.
The bottom panel of Figure 6 shows the conductive loss and the normalized umbo velocity magnitudes in a contrasting case of a surgically confirmed partial interruption of the ossicular chain, a fibrous union of the incus and stapes produced by resorption of the incus long process. Preoperatively, this patient had an air-bone gap that ranged from 0 to 35 dB and umbo velocity magnitudes that were 10 to 15 dB larger than normal. We suggest that the ossicular interruption reduced the load-impedance of the inner ear on the ossicular system, thereby allowing larger than normal umbo and tympanic membrane velocities. However, those larger velocities were not conducted to the stapes because of the hyper-elastic fibrous union, hence the conductive hearing loss. Similar patterns were seen in all of our cases of ossicular interruption.
Although stapes fixation and ossicular interruption lend to different changes in ossicular velocity, they both share the trait that the change in umbo velocity induced by pathologic changes is not proportional to the measured conductive hearing loss. With stapes fixation, the umbo velocity is decreased by only a fraction of the amount of the hearing loss, whereas in ossicular interruption the umbo velocity actually increases. The middle panel of Figure 6 illustrates the one case in which we saw changes of similar magnitude and direction in both conductive hearing and umbo velocity. These results are from the one confirmed case of fixation of the malleus head and incus body caused by tympanosclerosis in the epitympanum. The presurgical conductive hearing loss of 25 to 45 dB at frequencies of 1,000 Hz and lower was reasonably matched by the 25 dB reduction in umbo velocity over the same frequency range. Such similarity should be expected because the mechanism of the conductive hearing loss in this case was a decrease in the mobility of the malleus, which includes the umbo. At 2,000 Hz and higher, there were significant differences between the measured air-bone gap and the change in umbo velocity. Part of this difference may be due to the inadequacy of the air-bone gap as a measure of conductive hearing loss; ossicular pathologic changes are known to reduce bone-conduction thresholds at 2,000 Hz and higher (32), thereby leading to an underestimation of the conductive loss by the audiometric air-bone gap. Such an artificially low estimate of the conductive hearing loss by the air-bone gap can explain the mismatch between the two curves in the middle panel of Figure 6 at frequencies greater than 1000 Hz. In general, underestimation of the air-bone gap caused by decreases in bone-conduction thresholds resulting from conductive pathologic changes would affect any quantification of conductive hearing loss and confound the comparison of ossicular motion and conductive loss.
Guidelines for use of laser-Doppler vibrometry in the diagnosis of conductive hearing loss with normal tympanic membranes
The comparisons of presurgical air-bone gaps and LDV measurements of Figure 6 suggest the following guidelines for differential diagnosis of ossicular pathologic changes in cases of significant air-bone gap (>20 dB) with normal tympanic membranes and aerated middle ears:
In cases where umbo velocity is below the normal mean but within the normal range (Fig. 6, top panel), we suggest a tentative diagnosis of stapes fixation.
In cases where the umbo velocity at frequencies less than 1,000 Hz is larger than the normal mean and outside the normal range (Fig. 6, bottom panel), we suggest a tentative diagnosis of partial or complete ossicular interruption.
In cases where the umbo velocity is below the normal range and roughly proportional to the conductive loss at frequencies less than 2000 Hz (Fig. 6, middle panel), we suggest a tentative diagnosis of malleus fixation.
Tests of the validity of these guidelines require additional patient measurements and are continuing.
The guidelines suggested above assume that there is a single pathologic cause of the conductive hearing loss and do not apply to cases of multiple fixations or mixed fixation and ossicular interruption. For example, a case combining stapes fixation and ossicular interruption would be expected to display a pattern of air-bone gap and LDV umbo velocity indistinguishable from our cases of simple ossicular interruption. Other combinations of ossicular pathologic changes would give rise to patterns that are different from those described above. In cases combining malleus and stapes fixation, we might expect to see a clear decrease in umbo velocity relative to normal caused by fixed malleus (Fig. 3B; Fig. 6, middle panel) associated with a much larger air-bone gap. (The significant decrease in umbo velocity would primarily result from the malleus fixation, whereas the larger gap might be predicted by the decibel summation of the effect of the gap resulting from malleus fixation and the gap resulting from the fixed stapes.) A similar pattern of umbo velocity reduction and larger air-bone gap would also be expected in cases with a combination of malleus fixation and interruption of the incudostapedial joint. In general, in cases of multiple ossicular pathologic conditions, the LDV umbo velocity measurement will be most affected by the pathologic change closest to the umbo, whereas the air-bone gap will be at least as large as the larger gap resulting separately from the two pathologic conditions.
The LDV may also be useful in the postoperative assessment of cases with persistent or recurrent air-bone gaps; cases with fixed prostheses should show decreases in umbo velocity, whereas loose prostheses should have umbo velocities similar to our cases of ossicular interruption or successful stapedectomy. The LDV should also be a sensitive test of postoperative aeration of the middle ear. Nonaeration should reduce the velocity of the entire tympanic membrane.
Significance for middle ear mechanics
Our measurements of umbo velocity in presurgical and postsurgical ears with normal tympanic membranes and aerated middle ears support several hypotheses of ossicular function in normal ears.
The small (factor of 1.5–2 or 3–6 dB) decreases from normal umbo velocity magnitude at low frequencies in cases of stapes fixation (Figs. 3B, 4, 6) directly support previous estimates of a relatively high compliance of the ossicular joints (22,24). The flexibility of the joints allows motion of the tympanic membrane and malleus when the stapes is rigidly fixed. The small effect of stapes fixation on umbo velocity can be contrasted with the large reduction in velocity produced by fixation of the malleus head with no intervening joints between the umbo and the fixation site. Whereas the high compliance of the ossicular joints at sound frequencies has been described previously in humans (22,23), the earlier reports were based on middle-ear admittance measurements of the motion of the whole tympanic membrane in normal ears and ears with pathologic changes. Such measurements are partly confounded by the effect of the motion of “uncoupled” portions of the tympanic membrane; our measurements of umbo velocity were more direct measurements of the compliance of the joints.
Our measurements in cases of ossicular interruption and after stapedectomy demonstrate the dependence of normal middle-ear function on the cochlear load. The ossicular interruptions uncouple the middle ear from the cochlear impedance and lead to increases in the magnitude of the umbo velocity at low frequencies (Figs. 3C, 4). The same pathologic condition, however, produces a decrease in umbo velocity at frequencies above 1,000 Hz. This latter behavior fits with either an unmasking of middle-ear resonance and masslike behavior by removal of cochlear damping (22,25–26) or the unmasking of wave interactions on the tympanic membrane by the removal of cochlear damping (29).
Stapedectomy reduces the influence of the cochlear load on the middle ear by bypassing the anular ligament and by altering the middle-ear transformer mechanism (33). Removal of the effect of the anular ligament reduces the stiffness of the ear, and should increase the umbo velocity, by about a factor of two (33). The stapedectomy-induced reduction of the effective vibrating area of the footplate increases the middle-ear area ratio, where the area of the ratio of the average 60-mm2 tympanic membrane area and the 0.28-mm2 area of a 0.6-mm diameter piston is approximately 200 as opposed to the approximate factor of 20 between 60 mm2 and the 3.2-mm2 area of the normal footplate. The stapedectomy-induced increase in area ratio and the bypassing of the anular ligament impedance together reduce the impedance imposed by the inner ear on the middle ear such that equal middle-ear forces produce much larger excursions of the prosthesis compared with normal stapes motions. Indeed, to return hearing to normal by equating the volume velocities (the volume of inner-ear fluid displaced per second) at the input to the inner ear in normal and poststapedectomy ears, the stapedectomy piston (and the coupled incus) must move a factor of 10 times more than normal in magnitude to compensate for the factor of 10 change in effective footplate area. There should be a similar increase in the velocity of the coupled umbo. Our data show a factor of approximately 4 increase in the mean poststapedectomy umbo velocity relative to normal at low frequencies (Fig. 5), which is in the predicted direction but smaller in magnitude. If the change in stapedectomy piston velocity (relative to the normal stapes) tracked the measured change in mean umbo velocity (relative to normal umbo velocity), we would predict an increase in threshold of a factor of approximately 10/4 = 2.5, or approximately 8 dB from the ratio of the change in effective footplate area and the measured change in umbo velocity. This 8-dB predicted conductive hearing loss compares favorably with the 5.2-dB average poststapedectomy air-bone gap in our patient population.
CONCLUSION
Different ossicular pathologic changes result in reproducible and statistically significant alterations of umbo velocity. Whereas reduced umbo velocity seen in individual ears with stapes fixation is not easily distinguished from that in normal ears, there is a clear difference between the velocities measured in normal ears and ears with ossicular interruption or malleus fixation. There are also clear differences between the measurements in ears with either stapes fixation, malleus fixation, or ossicular interruption. The differences in these three pathologic conditions suggest that a comparison of the magnitudes of conductive hearing loss and umbo velocity relative to normal may enable ready separation of stapes fixation, malleus fixation, and ossicular interruption (Fig. 6), and a scheme is proposed to make such judgments. Measurements in the presurgical and postsurgical ears also were used to test previous observations and theories of ossicular function: the results are consistent with a relatively high compliance of the ossicular joints at acoustic frequencies and also support the transformer model of the middle-ear area ratio.
Acknowledgments
The authors thank their colleagues Drs. J. B. Nadol, M. J. McKenna, and S. D. Rauch for referring their patients for LDV measurements as well as for their comments on this manuscript; and Mike Ravicz, M.S., and Bill Peaks, Sc.D., for their contributions to this work at all levels.
Footnotes
Supported by the National Institute on Deafness and other Communicative Disorders and by Anne and Monty Wallace.
References
- 1.Buunen TJF, Vlaming MSMG. Laser-Doppler velocity meter applied to tympanic membrane vibrations in cat. J Acoust Soc Am. 1981;69:744–50. doi: 10.1121/1.385574. [DOI] [PubMed] [Google Scholar]
- 2.Rosowski JJ, Ravicz ME, Teoh SW, Flandermeyer D. Measurements is of middle-ear function in the Mongolian gerbil, a specialized mammalian ear. Audiol Neurootol. 1999;4:129–36. doi: 10.1159/000013831. [DOI] [PubMed] [Google Scholar]
- 3.Overstreet EH, III, Ruggero MA. Development of wide-band middle-ear transmission in the Mongolian gerbil. J Acoust Soc Am. 2002;111:261–70. doi: 10.1121/1.1420382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vlaming MSMG, Feenstra L. Studies of the mechanics of the normal human middle ear. Clin Otolaryngol. 1986;11:353–63. doi: 10.1111/j.1365-2273.1986.tb00137.x. [DOI] [PubMed] [Google Scholar]
- 5.Nishihara S, Aritomo H, Goode RL. Effect of changes in mass on middle ear function. Otolaryngol Head Neck Surg. 1993;109:899–910. doi: 10.1177/019459989310900520. [DOI] [PubMed] [Google Scholar]
- 6.Kurokawa H, Goode RL. Sound pressure gain produced by the human middle ear. Am J Otol. 1995;113:349–55. doi: 10.1016/S0194-59989570067-6. [DOI] [PubMed] [Google Scholar]
- 7.Asai M, Huber AM, Goode RL. Analysis of the best site on the stapes footplate for ossicular chain reconstruction. Acta Otolaryngol. 1999;119:356–61. doi: 10.1080/00016489950181396. [DOI] [PubMed] [Google Scholar]
- 8.Aibara R, Welsh JT, Puria S, Goode RL. Human middle-ear sound transfer function and cochlear input impedance. Hear Res. 2001;152:100–9. doi: 10.1016/s0378-5955(00)00240-9. [DOI] [PubMed] [Google Scholar]
- 9.Voss SE, Rosowski JJ, Merchant SN, Peake WT. Acoustic response of the human middle ear. Hear Res. 2000;150:43–69. doi: 10.1016/s0378-5955(00)00177-5. [DOI] [PubMed] [Google Scholar]
- 10.Gan RZ, Dyer RK, Wood MW, Dormer KJ. Mass loading on the ossicles and middle ear function. Ann Otol Rhinol Laryngol. 2001;110:478–85. doi: 10.1177/000348940111000515. [DOI] [PubMed] [Google Scholar]
- 11.Stasche N, Foth HJ, Baler A, Huthoff C. Middle ear transmission disorder: tympanic membrane vibration analysis by laser-Doppler vibrometry. Acta Otolaryngol. 1994;114:59–63. doi: 10.3109/00016489409126017. [DOI] [PubMed] [Google Scholar]
- 12.Goode RL, Ball G, Nishihara S. Measurement of umbo vibration in human subjects-methods and possible clinical applications. Am J Otol. 1993;14:247–51. [PubMed] [Google Scholar]
- 13.Goode RL, Ball G, Nishihara S, Nakamura K. Laser Doppler vibrometer (LDV): a new clinical tool for the otologist. Am J Otol. 1996;17:813–22. [PubMed] [Google Scholar]
- 14.Rodriguez JJ, Zenner H-P, Hemmert W, Burkhardt C, Gummer AW. Laservibrometrie: ein mittelohr- und Kochelaanalysator zur nicht-invasiven Untersuchung von Mittel-und Innenohrfunktions-störungen. HNO. 1997;45:997–1007. doi: 10.1007/s001060050185. [DOI] [PubMed] [Google Scholar]
- 15.Merchant SN, Whittemore KR, Poon B, Lee C-Y, Rosowski JJ. Clinical measurements of tympanic membrane velocity using laser Doppler vibrometry: preliminary results, methodological issues and potential applications. In: Rosowski JJ, Merchant SN. eds. The function and mechanics of normal, diseased and reconstructed middle ears. The Hague: Kugler, 2000:367–82.
- 16.Dyer RK, Dormer KJ, Pineda M, Conley K, Saunders J, Dennis M. The hearing laser vibrometer: initial clinical results. In; Rosowski JJ, Merchant SN, eds. The function and mechanics of normal, diseased and reconstructed middle ears. The Hague: Kugler, 2000:383–98.
- 17.Huber A, Linder T, Ferrazzini M, et al. Intraoperative assessment of stapes movement. Ann Otol Rhinol Laryngol. 2001;110:31–5. doi: 10.1177/000348940111000106. [DOI] [PubMed] [Google Scholar]
- 18.Huber AM, Schwab C, Linder T, et al. Evaluation of eardrum laser Doppler interferometry as a diagnostic tool. Laryngoscope. 2001;111:501–7. doi: 10.1097/00005537-200103000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Wilber LA, Feldman AS. The middle-ear measurement battery. In: Wilber LA, Feldman AS, eds. Acoustic impedance and admittance: the measurement of middle ear function. Baltimore: Williams & Wilkins, 1976;345–77.
- 20.Piskorski P, Keefe DH, Simmons JL, Gorga MP. Prediction of conductive hearing loss based on acoustic ear-canal response using a multivariate clinical decision theory. J Acoust Soc Am. 1999;105:1749–64. doi: 10.1121/1.426713. [DOI] [PubMed] [Google Scholar]
- 21.Schuknecht HF, Bentkover SH. Partial stapedectomy and piston prosthesis. In; Snow JB Jr. ed. Controversy in otolaryngology Philadelphia: WB Saunders, 1980:281–91.
- 22.Zwislocki J. Analysis of the middle-ear function. Part I: Input impedance. J Acoust Soc Am. 1962;34:1514–23. [Google Scholar]
- 23.Zwislocki J, Feldman AS. Acoustic impedance in pathologic ears. Washington, DC; American Speech and Hearing Association Monograph, Volume 15, 1970.
- 24.Hüttenbrink KB. The mechanics of the middle ear at static air pressures. Act Otolaryngol. 1988;451(Suppl):1–35. doi: 10.3109/00016488809099007. [DOI] [PubMed] [Google Scholar]
- 25.Møller AR. Experimental study of the acoustic impedance of the middle ear and its transmission properties. Acta Otolaryngol. 1965;60:129–49. doi: 10.3109/00016486509126996. [DOI] [PubMed] [Google Scholar]
- 26.Lynch TJ III. Signal processing by the cat middle ear: admittance and transmission, measurements and models [PhD Thesis]. Cambridge, MA: Massachusetts Institute of Technology, 1981.
- 27.Allen JB. Measurements of eardrum acoustic impedance. In: Allen JB, Hall JH, Hubbard A, et al., eds. Peripheral auditory mechanisms. New York: Springer-Verlag, 1986:44–51.
- 28.Peake WT, Rosowski JJ, Lynch TJ., III Middle-ear transmission: Acoustic vs ossicular coupling in cat and human. Hear Res. 1992;57:245–68. doi: 10.1016/0378-5955(92)90155-g. [DOI] [PubMed] [Google Scholar]
- 29.Puria S, Allen JB. Measurements and model of the cat middle ear: evidence of tympanic membrane acoustic delay. J Acoust Soc Am. 1998;104:3463–81. doi: 10.1121/1.423930. [DOI] [PubMed] [Google Scholar]
- 30.Keefe DH, Bulen JC, Arehart KH, Burns EM. Ear-canal impedance and reflection coefficient in human infants and adults. J Acoust Soc Am. 1993;94:2617–38. doi: 10.1121/1.407347. [DOI] [PubMed] [Google Scholar]
- 31.Margolis RH, Saly GL, Keefe DH. Wideband reflectance tympanometry in normal adults. J Acoust Soc Am. 1999;106:265–80. doi: 10.1121/1.427055. [DOI] [PubMed] [Google Scholar]
- 32.Carhart R. Bone conduction advances following fenestration surgery. Trans Am Acad Ophthalmol Otolaryngol. 1952;56:621–9. [PubMed] [Google Scholar]
- 33.Rosowski JJ, Merchant SN. Mechanical and acoustic analysis of middle ear reconstruction. Am J Otol. 1995;16:486–97. [PubMed] [Google Scholar]


