Abstract
BACKGROUND We wanted to determine whether an intervention to enhance partner support helps as an adjunct to a smoking cessation program.
METHODS We undertook a meta-analysis of English-language, randomized controlled trials of smoking cessation interventions through July 2002 using the following data sources: Cochrane Tobacco Addiction Group specialized register, Cochrane controlled trials register, CDC Tobacco Information and Prevention Database, MEDLINE, Cancer Lit, EMBASE, CINAHL, PsycINFO, ERIC, PsycLIT, Dissertation Abstracts, SSCI and HealthSTAR, with reviews of bibliographies of included articles. Included were trials that assessed a partner support component with a minimum follow-up of 6 months. The outcomes measured were abstinence and biochemical assessment at 6 to 9 months and more than 12 months after treatment. Partner Interaction Questionnaire scores were primary and secondary outcomes.
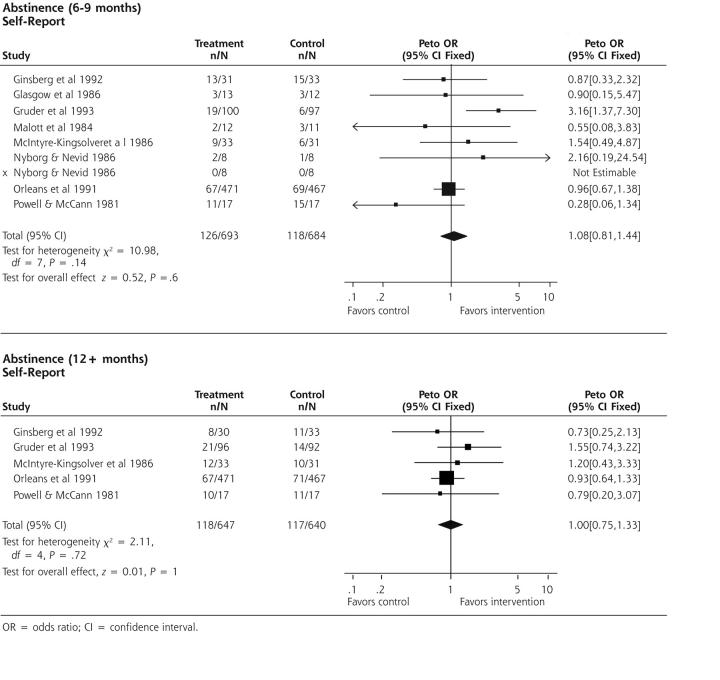
RESULTS Nine studies (31 articles) met inclusion criteria. Partner definition varied among studies. All studies included self-reported smoking cessation rates, but there was limited biochemical validation of abstinence. For self-reported abstinence at 6 to 9 months after treatment, the Peto odds ratio (OR) = 1.08 (95% confidence interval [CI], 0.81–1.44) and at 12 months Peto OR = 1.0 (95% CI, 0.75–1.34). Sensitivity analysis of studies using live-in, married, and equivalent-to-married partners found a higher odds ratio at 6 to 9 months after treatment, Peto OR = 1.64 (95% CI, 0.5–4.64). Sensitivity analysis of studies reporting significant increases in partner support found at 6 to 9 months after treatment Peto OR = 1.83 (95% CI, 0.9–3.47); and at 12 months Peto OR =1.22 (95% CI, 0.67–2.23).
CONCLUSIONS Interventions to enhance partner support showed the most promise for clinical practice when implemented with live-in, married, and equivalent-to-married partners. Such interventions should focus on enhancing supportive behaviors, while minimizing behaviors critical of smoking.
Keywords: Smoking, smoking cessation, social support
INTRODUCTION
Smoking remains the leading cause of preventable disease and death in the United States, causing more than 400,000 deaths annually.1 Smoking cessation is an important behavior change that can haveconsiderable effects on health outcomes. The initiation, maintenance, and cessation of smoking are strongly influenced by other family members. Smokers are more likely to marry smokers, to smoke the same number of cigarettes as their spouse, and to quit at the same time.2 In addition, married smokers have higher quit rates than those who are divorced, widowed, or have never married.3 Several studies have shown that support from the spouse is highly predictive of successful smoking cessation.4–7 In particular, support involving cooperative behaviors, such as talking the smoker out of smoking the cigarette, and reinforcement, such as expressing pleasure at the smoker’s efforts to quit, predict successful quitting.7,8 Negative behaviors, such as nagging the smoker and complaining about smoking, are predictive of relapse.9,10
Family interventions have become a standard part of most substance abuse programs. Initial trials of partner support for smoking cessation, however, have been disappointing. In reviewing their own studies of social support interventions for smoking cessation, Lichtenstein and colleagues11 stated that their interventions did not improve smoking cessation rates, nor were they able to improve the level of partner support, although support from a spouse has been shown to be highly predictive of successful smoking cessation.4,5 More recently published clinical trials12,13 have not shown partner support to have a significant effect on smoking cessation. One recent systematic review, which addressed the effectiveness of partner or social support interventions in smoking cessation, concluded that these interventions may be of some benefit.14 This review, however, included studies of partner support with varied lengths of follow-up, with no meta-analysis to take into consideration the diverse nature of the studies.14
This meta-analysis was conducted to fill the void in smoking cessation literature. The study focuses on interventions that enhance partner support with outcomes assessed after at least 6 months.
METHODS
Search Strategy
Randomized controlled studies that referred to smoking cessation with the use of partner support were identified from the following databases: Cochrane Tobacco Addiction Group specialized register (July 2002), Cochrane controlled trials register (July 2002), CDC and Prevention-Tobacco Information and Prevention Database (July 2002), MEDLINE (1966 to July 2002), Cancer Lit (1966 to July 2002), EMBASE (1974 to July 2002), CINAHL (1966 to July 2002), PsycINFO (1861 to July 2002), ERIC, PsycLIT, and Dissertation Abstracts (1861 to July 2002), SSCI (1972 to July 2002), and HealthSTAR (1975 to July 2002). The search strategy included the following terms: “smoking cessation,” “smoking/pc, th [Prevention & Control, Therapy],” “family support/ or marriage support/ or spouse support/ or partner support/ or sexual partners support/ or buddy/ or friend/ or cohabitees /coworker.” The bibliographies of all included articles were reviewed for additional trials. Researchers and experts in the field of smoking cessation were consulted for unpublished sources.
Selection Criteria
Inclusion criteria for this review were randomized controlled clinical trials that compared a smoking cessation intervention which included a partner support component with an otherwise identical intervention with no partner component. The follow-up of 6 months or more included smokers of any age or sex (regardless of their initial level of nicotine dependency, recruited from any setting) and partners, defined as spouses, friends, coworkers, buddies, or other significant others who supported the smokers as a component of the cessation program to which they were assigned.
Partner support interventions included training smokers in obtaining social support, encouraging increased contacts between smokers and supportive partners, providing training or written materials to partners to assist them in engaging in supportive behaviors, or intervening with smoker-partner pairs in couple therapy or in larger groups to encourage supportive interactions.
The primary outcome was self-reported abstinence of the smoker or biochemical assessment (carbon monoxide levels, saliva cotinine and thiocyanate measurements) assessed at least 6 months after initiation of treatment. Also considered was the intermediate outcome of the level of partner support as assessed by the Partner Interaction Questionnaire (PIQ) or other method.
Each article was given a quality score using the Jadad 5-point scale,15 which assigns 1 point for each of the following: a randomized study, the method to generate the randomization sequence was mentioned, a double-blind study, the masking method was described and appropriate (eg, identical placebo), and intention-to-treat analysis was utilized. None of the studies reviewed was described as double-blind, because partner support is an interactive process, so each study could receive a maximum total of only 4 points. All studies were described as randomized. Six studies received a score of 2 points,12,13,16,17 and 3 studies received a score of 1 point because they did not include a description of withdrawals or dropouts.18,19 Allocation concealment was unclear for the studies in this review. Biochemical validation was intended as a primary outcome but was not performed in every study. Only 4 studies used saliva cotinine-thiocyanate validation.13,18,20,21
Two reviewers (EP, FT) independently assessed the validity of the studies and extracted data using a structured form. A third investigator resolved discrepancies. Abstinence was the primary outcome and Peto odds ratios (ORs) were used as the summary effect measure using a 95% confidence interval (CI). The PIQ scores were also analyzed to assess partner support.
RESULTS
Of the 31 articles identified for this review, 8 representing 9 studies met the inclusion criteria (a supplemental table describing the characteristics of the studies is available in the online version of this article at http://www.annfammed.org/cgi/content/full/2/2/170/DC1). The most randomized clinical trial studies were excluded because, in addition to a partner intervention, the intervention group received other smoking cessation interventions that were not received by the control group. Three studies did not have a minimum 6-month follow-up,22–24 and 4 were duplicate publications that presented portions of data from included studies.25–28
At 6 to 9 months, all studies reported the following abstinence rates: 0% to 64.7% for the intervention groups and 0% to 88.2% for control groups. The highest cessation rates were from 2 small studies.13,17 The remaining studies all had cessation rates of less than 20% for both the intervention and control groups.12,16,18–21 At more than 12 months, only 5 studies reported abstinence rates: 14.2% to 58.8% for intervention groups and 15.2% to 64.7% for the control groups.12,13,16,17,21
A fixed-effects model using the Peto odds ratio29 was used to assess the summary effect of intervention on abstinence at the posttreatment intervals because of the homogeneity of the studies. The test for heterogeneity of the studies was χ2 = 10.98 at 6 to 9 months (P = .14), and χ2 = 2.11 at 12 months (P = .72) after treatment. For all 9 trials, at 6 to 9 months the Peto OR = 1.08 (95% CI, 0.81–1.44), and at 12 months Peto OR = 1.0 (95% CI, 0.75–1.33). Summary statistics shown in Figure 1 ▶ include point estimates and 95% confidence intervals. Although several studies included live-in married or equivalent-to-married partners in their interventions, only 2 of the 9 studies provided separate and comparable data for such partners.12,19 A sensitivity analysis for these 2 studies found that at 6 to 9 months after treatment the Peto OR = 1.64 (95% CI, 0.58–4.64). There were no data reported at 12 months after treatment for both studies.
Figure 1.
Sumary statistics of the 8 articles, representing 9 studies meeting inclusion criteria.
OR = odds ratio; CI = confidence interval.
Four studies reported the number of cigarettes smoked per day at preintervention baseline.17,18,20,21 Only Glasgow et al18 and Malott et al20 reported complete data for postintervention and 6-month intervals; therefore, data were not estimable to measure summary effect. The same 2 studies reported carbon monoxide levels at preintervention baseline, postintervention, and 6-month intervals; however, data were again not estimable.
Six studies assessed PIQ scores as a measure of partner support. Three of those studies12,20,21 mentioned no difference between intervention group and control group; and 1 study18 did not report a difference between the groups. Two studies13,16 reported that partner support was increased after the partner support intervention. A sensitivity analysis of these 2 studies showed at 6 to 9 months Peto OR = 1.83 (95% CI, 0.97–3.47), and at 12 months Peto OR = 1.22 (95% CI, 0.67–2.23).
DISCUSSION
Social support is known to be an important determinant of success in smoking cessation efforts. It is therefore reasonable to expect that an intervention designed to increase support from a partner might lead to greater rates of successful smoking cessation. In our review, we were unable to show an effect with a persistence of 6 months or longer. The failure to show conclusively such an effect by an analysis of existing trials does not necessarily mean that partner support interventions are ineffective. This review included studies of a number of different partner forms, as did the comprehensive review of May and West.14 If different partner forms were examined separately, successful interventions might be identified.
Because of the nature of their specialty, family physicians are more likely to work with live-in married or common-law couples than with the other forms of partners. A sensitivity analysis was therefore performed, which indicated higher (but not significant) Peto odds ratios, suggesting enhancing smoking cessation interventions with live-in couples might be more effective than with other partner forms. Although we could not calculate the sample size needed for sufficient power, the 2 trials here comprised only 49 and 47 subjects in the treatment and control arms, respectively.
There are a number of possible other explanations for our failure to find an effect.
First, partner support may lead only to short-term but not to long-term success in smoking cessation. We excluded some trials from this review because they provided only data on short-term follow-up, even though they showed positive results within that short-term time frame.22,24
Second, the interventions used in the studies might not have been effective in actually increasing the amount of support provided by the subjects’ partners. Six of the included studies used the PIQ to assess the amount of partner support provided. This scale consists of a list of positive (supportive) and negative (critical) behaviors by the partner concerning the subject’s smoking. Of the 6 studies that measured partner support and follow-up, there was no difference in the PIQ scores between the groups in 3.12,20,21 Two studies13,16 showed an increase in PIQ scores that was associated with higher abstinence rates. The sensitivity analysis of these 2 studies reinforces this positive effect on cessation. Another study found negative interaction and criticism to be associated with lower abstinence rates, which is consistent with the findings from observational studies.20
Our review of these studies suggests that partner support—in particular, support from a live-in partner or spouse—and the absence of partner criticism may be important in smoking cessation, but that these behaviors are not easily changed by the interventions used in these studies. Because the interventions primarily used education and problem solving, the failure of these interventions to increase smoking cessation might result partly from their lack of a systemic orientation. Smoking is a complex behavior that is influenced by biological factors (nicotine addiction), individual psychological issues, and extrafamilial social relationships and pressures, as well as the couple relationship. Supportive behaviors by the spouse are part of a complex marital relationship and are probably related to overall marital quality and satisfaction. More systematic interventions using live-in partners and spouses to affect partnership interaction should be studied if partner support is a component of an existing cessation program.
CONCLUSIONS
Interventions used to enhance partner support for smoking cessation programs did not increase quit rates among all partner forms, but they might be most effective among live-in partners and spouses. Limited data from several of the randomized controlled trials suggest that for smoking cessation interventions to be more effective, they need to focus on enhancing positive and supportive behaviors and on minimizing negative and critical behaviors by the partner toward the smoker.
Conflicts of interest: none reported
REFERENCES
- 1.US Department of Health and Human Services. Reducing Tobacco Use: A Report of the Surgeon General. Washington, DC: US Department of Health and Human Services; 2000.
- 2.Venters M, Jacobs DJ, Luepker R, Maiman L, Gillum R. Spouse concordance of smoking patterns: the Minnesota Heart Survey. Am J Epidemiol. 1984;120:608–616. [DOI] [PubMed] [Google Scholar]
- 3.Waldron I, Lye D. Family Roles and Smoking. Am J Prev Med. 1989;5:136–141. [PubMed] [Google Scholar]
- 4.Graham S, Gibson R. Cessation of patterned behaviour: withdrawal from smoking. Soc Sci Med. 1971;5:319–337. [DOI] [PubMed] [Google Scholar]
- 5.Ockene JK BR, Nuttal RL, Hurwitz I, Ockene IS. Relationship of psychosocial factors to smoking behavior change in an intervention program. Prev Med. 1982;11:13–28. [DOI] [PubMed] [Google Scholar]
- 6.Gulliver S, Hughes J, Solomon L, Dey A. An investigation of self-efficacy, partner support and daily stresses as predictors of relapse to smoking in self-quitters. Addiction. 1995;90:767–772. [DOI] [PubMed] [Google Scholar]
- 7.Coppotelli H, Orleans C. Partner support and other determinants of smoking cessation maintenance among women. J Consult Clin Psychol. 1985;53:455–460. [DOI] [PubMed] [Google Scholar]
- 8.Mermelstein R, Lichtenstein E, McIntyre K. Partner support and relapse in smoking-cessation programs. J Consult Clin Psychol. 1983;51:465–466. [DOI] [PubMed] [Google Scholar]
- 9.Cohen S, Lichtenstein E. Partner behaviors that support quitting smoking. J Consult Clin Psychol. 1990;58:304–309 [DOI] [PubMed] [Google Scholar]
- 10.Roski J, Schmid LA, Lando HA. Long-term associations of helpful and harmful spousal behaviors with smoking cessation. Addict Behav. 1996;21:173–185 [DOI] [PubMed] [Google Scholar]
- 11.Lichtenstein E, Glasgow R, Abrams D. Social support in smoking cessation: in search of effective interventions. Behav Ther. 1986;17:607–619. [Google Scholar]
- 12.McIntyre-Kingsolver K, Lichtenstein E, Mermelstein R. Spouse training in a multicomponent smoking-cessation program. Behav Ther. 1986;17:67–74. [Google Scholar]
- 13.Ginsberg D, Hall S, Rosinski M. Partner support, psychological treatment, and nicotine gum in smoking treatment: an incremental study. The Int J Addict. 1992;27:503–517. [DOI] [PubMed] [Google Scholar]
- 14.May S, West R. Do social support interventions (“buddy systems”) aid smoking cessation? A review. Tob Control. 2000;9:415–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jadad A, Moore R, Carroll D. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. [DOI] [PubMed] [Google Scholar]
- 16.Gruder C, Mermelstein R, Kirkendol S, et al. Effects of social support and relapse prevention training as adjuncts to a televised smoking-cessation intervention. J Consult Clin Psychol. 1993;61:113–120. [DOI] [PubMed] [Google Scholar]
- 17.Powell D, McCann B. The effects of a multiple treatment program and maintenance procedures on smoking cessation. Prev Med. 1981;10:94–104. [DOI] [PubMed] [Google Scholar]
- 18.Glasgow R, Klesges R, O’Neill H. Programming social support for smoking modification: an extension and replication. Addict Behav. 1986;11:453–457. [DOI] [PubMed] [Google Scholar]
- 19.Nyborg K, Nevid J. Couples who smoke: a comparison of couples training versus individual training for smoking cessation. Behav Ther. 1986;17:620–625. [Google Scholar]
- 20.Malott J, Glasgow R, O’Neill H, Klesges R. Co-worker social support in a worksite smoking control program. J Appl Behav Anal. 1984;17:485–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orleans C, Schoenbach V, Wagner E, et al. Self-help quit smoking interventions: effects of self-help materials, social support instructions, and telephone counseling. J Consult Clin Psychol. 1991;59:439–448. [DOI] [PubMed] [Google Scholar]
- 22.Albrecht S, Stone C, Payne L, Reynolds M. A preliminary study of the use of peer support in smoking cessation programs for pregnant adolescents. J Am Acad Nurse Pract. 1998;10:119–125. [DOI] [PubMed] [Google Scholar]
- 23.Gardner P. An Investigation of Couples Training in Smoking Cessation With Implications for the Televised Delivery of Behavioral Medicine Counseling [dissertation]. Stanford, Calif: Stanford University; 1982.
- 24.West R, Edwards M, Hajek P. A randomized controlled trial of a “buddy” system to improve success at giving up smoking in a general practice. Addiction. 1998;93:1007–1011. [DOI] [PubMed] [Google Scholar]
- 25.McMahon S, Jason L. Social support in a worksite smoking intervention. Behav Modif. 2000;24:184–201. [DOI] [PubMed] [Google Scholar]
- 26.Mermelstein R, Cohen S, Lichtenstein E, Baer J, Kamarck T. Social support and smoking cessation and maintenance. J Consult Clin Psychol. 1986;54:447–453. [DOI] [PubMed] [Google Scholar]
- 27.Nyborg K. Partner Support and Type of Treatment as Variables in the Behavioral Treatment of Cigarette Smoking [dissertation]. Jamaica, NY: St. John’s University; 1985.
- 28.Schoenback V, Orleans C, Wagner E, Quade D, Salmon M, Porter C. Characteristics of smokers who enroll and quit in self-help programs. Health Ed Res. 1992;7:369–380. [Google Scholar]
- 29.Review Manager [computer program]. Version 4.1 for Windows: The Cochrane Collaboration; 2000.