Abstract
BACKGROUND We undertook a literature review to produce evidence-based recommendations for nonsurgical family physician management of carpal tunnel syndrome (CTS).
METHODS Study design was systematic review of randomized controlled trials (RCTs) on CTS treatment. Data sources were English publications from all relevant databases, hand searches, and guidelines. Outcomes measured were nonsurgical management options for CTS.
RESULTS We assessed 2 systematic reviews, 16 RCTs, and 1 before-and-after study using historical controls. A considerable percentage of CTS resolves spontaneously. There is strong evidence that local corticosteroid injections, and to a lesser extent oral corticosteroids, give short-term relief for CTS sufferers. There is limited evidence to indicate that splinting, laser-acupuncture, yoga, and therapeutic ultrasound may be effective in the short to medium term (up to 6 months). The evidence for nerve and tendon gliding exercises is even more tentative. The evidence does not support the use of nonsteroidal ant-iinflammatory drugs, diuretics, pyridoxine (vitamin B6), chiropractic treatment, or magnet treatment.
CONCLUSIONS For those who are not able to get surgery or for those who do not want surgery, there are some conservative modalities that can be tried. These modalities include ones for which there is good evidence. It would be reasonable to try some of the techniques with less evidence if the better ones are not successful. Reconsideration of surgery must always be kept in mind to avoid permanent nerve damage.
Keywords: Carpal tunnel syndrome, preoperative care, review literature
INTRODUCTION
Carpal tunnel syndrome (CTS) is the most commonly occurring peripheral nerve compression syndrome, with a 10% lifetime risk of development.1 It most often occurs after the age of 30 years, with women affected more than men by a factor of 3 to 1.2 A US study of 1,016 patients at the Mayo Clinic found an incidence (cases per 100,000 person-years) of 99 (crude) overall. The age-adjusted rates were 52 for men, 149 for women, and 105 for both sexes combined.2
CTS involves median nerve compression at the level of the wrist. Median nerve entrapment can result in sensory and motor impairment, as well as pain in the hand and or arm. There is no single reference standard for diagnosis of the syndrome, and a combination of symptoms, signs, and tests should be used to characterize the disorder.1 Distinction should be made between CTS (a clinical syndrome involving a cluster of symptoms) and distal median neuropathy (a structural abnormality with pathophysiological findings on nerve conduction studies). It should be noted that distal median neuropathy can sometimes be asymptomatic; conversely, patients with CTS can occasionally have normal nerve conduction study results.
Although most cases are idiopathic (have no identifiable cause),3 CTS is also associated with a number of systemic conditions, including rheumatoid arthritis, hypothyroidism, diabetes mellitus, acromegaly, gout, and pregnancy.1,4 Because the carpal tunnel runs between the transverse carpal ligament and the carpal bones, damage to this region can result from a number of compression lesions, including local trauma, overuse of the hand or wrist, or prolonged improper positioning. Occupational causes contribute to the occurrence of CTS. Even though there has been a large increase in the reporting of work-related repetitive strain injuries during the past 2 decades, only about 2% of these are CTS.5
There is strong evidence of a positive association between exposure to a combination of risk factors (such as force and repetition) and CTS.6 Evidence is reported of a positive association of CTS and highly repetitive work alone or in combination with other factors and forceful work and with work involving hand and wrist vibration.6,7 Epidemiologic surveillance data also consistently indicate that the highest rates of CTS occur with job tasks that have high work demands for intensive manual exertion—for example, in meatpackers, poultry processors, and automobile assembly workers.6
Insufficient evidence of a positive association has been found between posture and CTS.6 Self-diagnosis of prolonged hand discomfort as CTS is very common,8 and keyboard workers who develop hand pain may have CTS wrongly diagnosed. Although the incidence of diagnosed CTS has increased during the past 20 years,2 and public attention has focused on excessive keyboard use,9 frequent computer use has not yet been established as a cause of CTS.6 One survey of employees who were frequent computer users found that their frequency of CTS was similar to that in the general population.10
Many patients report spontaneous recovery. Others do not access surgical options because of waiting times and cost of surgery, or they prefer not to embark on surgery. For these patients, short-term nonsurgical management may be desirable. There is, however, a risk of permanent damage to the median nerve; hence, primary care physicians need to consider nonsurgical options with caution.
The aim of our study was to conduct a systematic review of the literature and produce evidence-based recommendations for nonsurgical family physician management of CTS.
METHODS
The review included randomized controlled studies that assessed the efficacy of nonsurgical treatment of CTS. Non-English papers were excluded because translations were not available. The restriction to English language studies is unlikely to cause any bias, as a recent assessment reported that non-English papers are likely to be of low quality and could introduce bias into a review.11
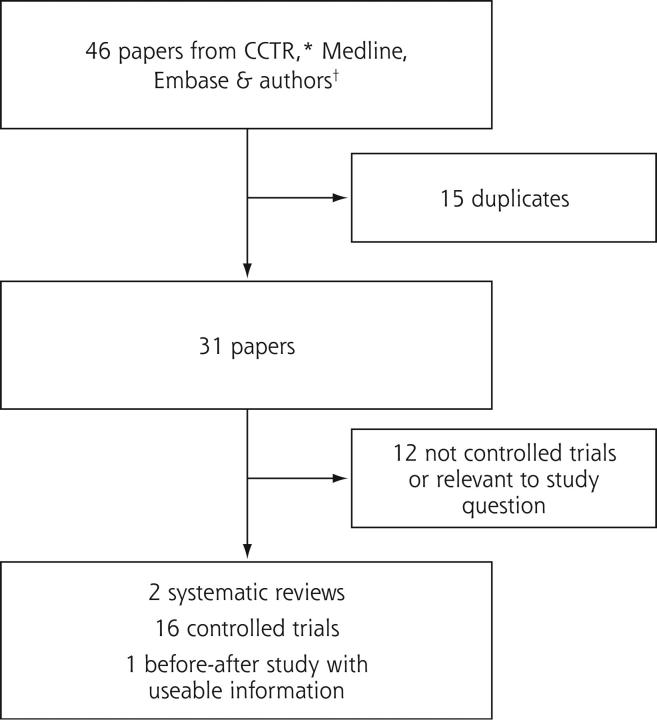
Relevant studies were identified using Cochrane Library and controlled trials register, MEDLINE (1966 to 2002), and EMBASE (1980 to 2002). The review also included international guidelines, computer searches based on key words, hand searching for references from previously retrieved articles and communication with international authors to obtain unpublished material. Figure 1 ▶ displays the search summary.
Figure 1.
Summary of search results.
The relevant papers were selected by one author (FG) and critiqued by both authors. The key papers were entered into evidence tables. The quality of their methods was assessed with the PEDro (Physiotherapy Evidence Database) scale, which gives a total score of 10 possible points.12,13 The key aspects of quality were whether the studies were randomized, allocation was concealed, reasonable follow-up was achieved, and maintenance of blinding where appropriate. Any disagreements were resolved by discussion. Studies require a score of at least 3 to be included in the analysis. Other more general comments on blinding are shown in Appendix 1, which is available online at http://www.annfammed.org/cgi/content/full/2/3/267/DC1.14–30 The strength of the evidence was graded using the Scottish Intercollegiate Guidelines Network (SIGN) revised grading system (Appendix 2, which is available online at http://www.annfammed.org/cgi/content/full/2/3/267/DC1).31 SIGN was formed in 1993 to improve the effectiveness and efficiency of clinical patient care by developing evidence-based guidelines prepared by a multiprofessional group.
RESULTS
The quality of the methods ranged widely, from 3 to 10 (Table 1 ▶).14–15,27–30 There is limited evidence that a significant percentage of cases of idiopathic CTS will resolve without treatment.3,32 High response rates to placebo treatments suggest rates of 50% or more. The small number of studies and the wide range of outcomes made statistical pooling unfeasible.
Table 1.
Quality Scores of Studies in Systematic Review
| Scores in PEDro Scale* | ||||||||||||
| Author | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total Score γ |
| Aigner & Fielka, 199814 | − | + | ? | ? | + | ? | ? | ? | ? | + | − | 3 |
| Carter et al, 200215 | + | + | + | + | + | + | + | − | ? | + | + | 8 |
| Chang et al, 199816 | + | + | + | + | + | + | + | + | ? | + | − | 8 |
| Dammers et al, 199917 | + | + | ? | + | + | + | + | + | + | + | + | 9 |
| Davis et al, 199818 | + | + | − | + | − | − | − | − | + | + | + | 5 |
| Ebenbichler et al, 199819 | + | + | ? | + | + | + | ? | − | + | + | + | 7 |
| Elbaz et al, 199420 | − | + | ? | + | + | + | + | ? | ? | + | ? | 6 |
| Garfinkel et al, 199821 | + | + | + | + | ? | − | + | − | − | + | − | 5 |
| Herskovitz et al, 199522 | + | + | ? | + | + | + | + | − | − | + | − | 6 |
| O’Gradaigh & Merry, 200023 | + | + | ? | + | + | ? | − | ? | ? | + | − | 4 |
| Ozdogan & Yazici, 198424 | + | + | ? | + | + | + | + | − | ? | + | + | 7 |
| Oztas et al, 199825 | + | + | ? | + | + | ? | ? | ? | ? | + | + | 5 |
| Spooner et al, 199327 | + | + | ? | + | + | + | + | + | ? | + | + | 8 |
| Stransky et al, 198928 | − | + | ? | ? | + | ? | ? | + | ? | − | − | 3 |
| Walker et al, 200029 | + | + | ? | + | − | − | − | − | ? | + | + | 5 |
| Wong et al, 200130 | + | + | + | + | + | + | + | + | + | + | + | 10 |
* Column numbers correspond to the following on the PEDro scale:
| ||||||||||||
γ The total score is determined by counting the number of criteria that are satisfied, except that scale item I is not used to generate the total score, giving a total score out of 10.
+ Indicates the criterion was clearly satisfied; − indicates that it was not; ? indicates that it is unclear whether criterion was satisfied.
A Cochrane systematic review found that local steroid injection for CTS significantly improved symptoms for a period up to 1 month after treatment.17,20,24,33 This finding has also been confirmed in a more recent randomized controlled trial (RCT).23 One 1994 study reported that in cases of mild idiopathic CTS, no significant difference was found between steroid injection and placebo, but 63% of patients experienced symptomatic improvement irrespective of whether they received steroid injection or placebo.20
Two RCTs16,22 have found short-term relief of symptoms with the use of oral corticosteroids.3 One RCT has found that 10 days of oral corticosteroid is significantly less effective than local steroid injection in achieving symptom relief at 12 weeks.30 Table 2 ▶ displays the characteristics of effective nonsurgical treatments.
Table 2.
Effective Nonsurgical Treatments for Carpal Tunnel Syndrome
| Treatment | Initial Success | Long-Term Success | Evidence | Advantages | Disadvantages |
| Local corticosteroid injection | 20/24 (86%) responded | Within 1 year, 50% required surgery | Systematic review33; 4 RCTs17,20,23,24 | Effective symptom relief; some patients may not progress to surgery | Local steroid affords only temporary relief |
| Oral steroid | Significant short-term symptom reduction | Unknown | 2 RCTs16,22 | Effective short-term symptom relief; some patients may not progress to surgery | Potential adverse reactions to oral corticosteroids |
| Waning of effect over 8 weeks | |||||
| Less effective than steroid injection30 |
There are no RCTs comparing wrist splinting with no treatment. One RCT suggested that full-time was better than nighttime splint use.29 One prospective study found that neutral angle splints were more effective than those set in extension, because an angle splint decreases the potential for the nerve to be stretched.34 A systematic review concluded that all splinting studies had serious methodological failings.35 A more recent RCT comparing splinting with surgery found the latter was more effective than splinting on all outcome symptom measures at 3 months, and by 18 months 41% of the patients in the splint group had received surgical intervention.36
One large RCT found short- to medium-term benefit of ultrasound treatment in mild-to-moderate idiopathic CTS compared with placebo,19 and another smaller RCT found no significant difference.25 There is very limited evidence that a yoga-based intervention might give some symptom relief in CTS.21 A small randomized, single-blinded study found laser-acupuncture resulted in a significant reduction in night pain compared with placebo laser.14 This RCT is the only one available, and only a conference abstract is available in the Cochrane database.
Nerve and tendon gliding exercises are designed to restore and maximize the excursion of the median nerve through the carpal tunnel.26 These exercises involve intermittent active wrist and digital flexion and extension exercise. While one before-after study suggested some benefit,26 there have been no RCTs to evaluate the effectiveness of these exercises. Table 3 ▶ displays the characteristics of possibly effective treatments.
Table 3.
Possibly Effective Nonsurgical Treatments for Carpal Tunnel Syndrome
| Treatment | Initial Success | Long-Term Success | Evidence | Advantages | Disadvantages |
| Laser-acupuncture | Reduction in night pain but not paraesthesia | Unknown | 1 poor-quality RCT14 | Possible preoperative analgesic agent | Poor availability |
| Nerve and tendon gliding exercises | No significant difference for Phalen’s or Tinel’s sign, or nerve conduction studies | Significantly reduced rates of surgery | Before-and-after study using historical controls26 | Noninvasive | Reduced surgical rates may result from confounders |
| NNT = 4 | |||||
| Ultrasound | One study suggested improvement in both symptoms and nerve conduction studies19; other study found no significant difference25 | Unknown | 2 RCTs19,25 | Noninvasive | Expensive |
| Conflicting evidence | High dropout rate | ||||
| Wrist splinting | Neutral superior to 20o extension splinting | Unknown | 1 systematic review35 plus 1 RCT19 | No harmful effects noted | Poor compliance |
| Full-time use significantly greater improvement in nerve conduction studies but no difference in symptoms | All studies had methodological flaws | ||||
| Yoga | Significant improvement in Phalen’s sign, grip strength, and pain reduction but not Tinel’s sign, sleep disturbance, or nerve conduction studies | Unknown | RCT (single-blind)21 | Noninvasive | No changes in nerve conduction studies |
| Can be home-based treatment | |||||
| Involves high level of patient commitment | |||||
| Control group had wrist splinting. |
RCT = randomized controlled trial; NNT = number needed to treat.
There is no evidence that either nonsteroidal anti-inflammatory drugs (NSAIDs)16,18 or diuretics16 result in clinical improvement in CTS. Although initial studies were promising,37–39 recent RCT evidence does not indicate that the use of pyridoxine (vitamin B6) gives any clinical improvement over placebo in the treatment of CTS.27,28 Because all the studies to date involve small sample sizes, the relationship between pyridoxine deficiency and CTS has not been adequately established.
There is no good evidence that chiropractic treatment gives effective symptom relief. One study found that chiropractic treatment did not give improved benefit when compared with NSAID use.18 A double-blind placebo-controlled RCT found the use of a magnet for reducing pain attributed to CTS was no more effective than use of a placebo device.15 Table 4 ▶ displays the characteristics of probably ineffective treatments.
Table 4.
Probably Ineffective Nonsurgical Treatment of Carpal Tunnel Syndrome
| Treatment | Evidence | Findings |
| NSAID | 2 RCTs16,18 | No significant reduction in symptom measures |
| Diuretic | 1 RCT16 | No significant reduction in symptom measures from baseline to 4th week assessment |
| Pyridoxine | 2 RCTs27,28 | Reduced finger swelling and discomfort after movement but no difference in nocturnal pain, numbness, Phalen’s or Tinel’s signs or nerve conduction studies in one study, and no significant difference in the other study |
| Chiropractic treatment | 1 RCT18 | No significant reduction in symptom measures |
| Magnet therapy | 1 RCT15 | No difference in effect between magnet and placebo |
NSAID = nonsteriodal anti-inflammatory drug; RCT = randomized controlled trial.
Comparative details of these individual studies can be found in Appendix 1: Methods, and in Appendix 3: Outcomes (Appendix 1 and Appendix 3 are available online at http://www.annfammed.org/cgi/content/full/2/3/267/DC1).14–30,33–35
DISCUSSION
Conservative management has a place in the early management of mild to moderate CTS and may reduce the number of patients undergoing surgical intervention. Non-surgical management also has a place in those waiting for surgery or for those who choose not to have surgery.
There is strong evidence that local corticosteroid injections (level of evidence 1++ recommendation A), and to a lesser extent oral corticosteroids (level of evidence 1+ recommendation A), give short-term relief for CTS sufferers. There is conflicting evidence suggesting that therapeutic ultrasound is effective. One study found a benefit and one did not. There is insufficient evidence to evaluate whether yoga, nerve and tendon gliding exercises, or laser-acupuncture are effective modalities (unable to grade).
The evidence on wrist splinting showed that splinting at night was not as effective as full-time splinting day and night (level of evidence 1- recommendation A). Given that many patients have predominantly nocturnal symptoms, however, splinting when in bed is likely to be much more acceptable and tolerated by patients than splinting during the day.
Initial diagnosis of CTS is made on clinical symptoms. Because about 50% will resolve spontaneously, not all need to be referred for nerve conduction studies or surgical assessment. Patients with mild symptoms should be offered conservative treatment. Surgical referral should be considered in patients with symptoms that are causing persistent sleep disturbance, interfering with their ability to work, or otherwise adversely affecting their lifestyle.
Our review indicates that conservative treatment options are limited. In those cases clearly related to occupational job tasks, such as highly repetitive forceful work or work involving hand and wrist vibration, the patient should be advised to modify the activities or movements that caused the CTS. Steroid injection is the most effective nonsurgical treatment, but it can result in possible complications of nerve injury, scar, infection, allergic dermatitis, hypopigmentation, soft tissue atrophy, and tendon rupture.40 Similarly, oral corticosteroids can cause adverse reactions, including nausea, anxiety, acne, menstrual irregularities, insomnia, headaches, and mood swings. More serious adverse reactions include peptic ulcer, steroid psychosis, osteoporosis, and adrenal insufficiency.3
While the evidence of the benefits is uncertain, there are no recorded harmful effects of splinting. This low-cost option could warrant an initial trial. Similarly, no harmful effects have been documented through the use of nerve and tendon gliding exercises and yoga, and these modalities might be considered as first-line management in selected cases. Ultrasound involves some expense, and the treatment regimes prescribed are time-consuming for the patient, although there is no evidence that it causes harm. Given the limited and conflicting evidence regarding its effectiveness, its use in conservative management is questionable.
Given the potential harmful effects of NSAIDs (users of NSAIDs have about 3 times the risk of developing serious adverse gastrointestinal events compared with nonusers41) and diuretics (such as elevated serum uric acid levels provoking attacks of gout in predisposed patients; hypokalemia, and increased blood glucose levels), the rare possibility of pyridoxine excess causing a sensory neuropathy,42 and the low-risk but serious adverse outcome of permanent impairment or death from chiropractic treament43,44 in the absence of evidence showing any benefit, these modalities are not recommended in the nonsurgical treatment of CTS.
In general, the management is surgery for persistent (not resolving after 1 year) or deteriorating (worsening clinically plus or minus deterioration on nerve conduction studies) CTS. There are no RCTs comparing surgery with no treatment. Most patients improve considerably after surgery regardless of whether the release is open or endoscopic and whether there is adjunctive use of internal neurolysis.45
Surgery can be a highly effective treatment for CTS, but prediction on its outcome depends on the accuracy of the diagnosis before the surgical intervention and the timing of surgery in regard to the onset of symptoms. Current evidence indicates that earlier intervention leads to better results.46 One study showed that patients who had surgery within 3 years of the initial diagnosis were twice as likely to have symptom relief than were those whose surgery was delayed more than 3 years.47 Because CTS is usually a progressive disease, patients who have had the condition for a number of years are more likely to have advanced compression and damage to the distal median nerve, making complete symptom resolution and full recovery of hand function less likely. One study indicated that patients with intermittent symptoms of numbness and paresthesias had much better sensory recovery than those who had constant symptoms preoperatively.48
Evidence indicates that patients with advanced median nerve damage have a less positive response to surgery. Current surgical thinking, although not supported by current evidence, would suggest that surgical intervention should be considered after symptoms have been present for at least 6 months, but if indicated, surgery should have taken place within 3 years from the initial diagnosis.
Our review has revealed that both injected and oral steroids have a short-term benefit. A number of other therapies are either of poor quality or have contradictory evidence. In general, the quality of the studies was poor and the size of the studies relatively small. Future research in the form of rigorous well-conducted studies of these various therapies (laser acupuncture, nerve and tendon gliding exercises, ultrasound, wrist splinting, and yoga) would be beneficial in establishing the effectiveness or otherwise of these various treatments. There are also a number of studies that showed no benefit (NSAIDs, diuretics, pyridoxine, chiropractic, and magnet treatments), and these therapies should be avoided. For those who are not able to get or do not want surgery, some conservative modalities can be tried that include those that have good evidence of therapeutic effect. It would be reasonable to try techniques with less evidence of therapeutic effect if the better evidenced ones are not successful. Reconsidering surgery must always be kept in mind to avoid permanent nerve damage.
Acknowledgments
This study was conducted at the request and with the support of the New Zealand Accident Rehabilitation and Compensation Insurance Corporation (ARCIC) Healthwise. The opinions expressed in this report are those of the authors rather than the medical advisors. They do not necessarily represent those of the ARCIC. We would like to thank our medical advisors for their assistance in this project.
Conflict of interest: none reported
Funding support: This study was conducted with the support of the New Zealand Accident Rehabilitation and Compensation Insurance Corporation Healthwise.
REFERENCES
- 1.Practice parameter for carpal tunnel syndrome [summary statement]. Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 1993;43:2406–2409. [PubMed] [Google Scholar]
- 2.Stevens JC, Sun S, Beard CM, O’Fallon WM, Kurland LT. Carpal tunnel syndrome in Rochester, Minnesota, 1961 to 1980. Neurology. 1988;38:134–138. [DOI] [PubMed] [Google Scholar]
- 3.Marshall S. Carpal tunnel syndrome. Clin Evid. 2001;5:717–728. [Google Scholar]
- 4.Spinner RJ, Bachman JW, Amadio PC. The many faces of carpal tunnel syndrome. Mayo Clin Proc. 1989;64:829–836. [DOI] [PubMed] [Google Scholar]
- 5.Mackinnon SE, Novak CB. Repetitive strain in the workplace. J Hand Surg [Am]. 1997;22:2–18. [DOI] [PubMed] [Google Scholar]
- 6.Bernard B. Musculoskeletal Disorders (MSDs) and Workplace Factors: A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back. Cincinnati: Centers for Disease Control and Prevention National Institute for Occupational Safety and Health; 1997.
- 7.Tanaka S, Wild DK, Cameron LL, Freund E. Association of occupational and non-occupational risk factors with the prevalence of self-reported carpal tunnel syndrome in a national survey of the working population. Am J Indust Med. 1997;32:550–556. [DOI] [PubMed] [Google Scholar]
- 8.Tanaka S, Wild DK, Seligman PJ, Behrens V, Cameron L, Putz-Anderson V. The US prevalence of self-reported carpal tunnel syndrome: 1988 National Health Interview Survey data. Am J Pub Health. 1994;84:1846–1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olney RK. Carpal tunnel syndrome: complex issues with a “simple” condition. Neurology. 2001;56:1431–1432. [DOI] [PubMed] [Google Scholar]
- 10.Stevens JC, Witt JC, Smith BE, Weaver AL. The frequency of carpal tunnel syndrome in computer users at a medical facility. Neurology. 2001;56:1568–1570. [DOI] [PubMed] [Google Scholar]
- 11.Egger M, Juni P, Bartlett C, Holenstein F, Sterne J. How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study. Health Technol Assess. 2003;7:68. [PubMed] [Google Scholar]
- 12.Verhagen A, de Vet H, de Bie R, et al. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidem. 1998;51:1235–1241. [DOI] [PubMed] [Google Scholar]
- 13.Herbert RD, Gabriel M. Effects of stretching before and after exercising on muscle soreness and risk of injury: systematic review. BMJ. 2002;325:468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aigner N, Fialka C. Results of laser-acupuncture in carpal tunnel syndrome - a prospective, randomised and blinded study (presented at the 5th Annual Symposium on Complementary Healthcare, 10–12 December 1998, Exeter). FACT: Focus on Alternative and Complementary Therapies 1988;4:180. [Google Scholar]
- 15.Carter R, Hall T, Aspy CB, Mold J. The effectiveness of magnet therapy for treatment of wrist pain attributed to carpal tunnel syndrome. J Fam Pract. 2002;51:38–40. [PubMed] [Google Scholar]
- 16.Chang MH, Chiang HT, Lee SS, Ger LP, Lo YK. Oral drug of choice in carpal tunnel syndrome. Neurology. 1998;51:390–393.20. [DOI] [PubMed] [Google Scholar]
- 17.Dammers JW, Veering MM, Vermeulen M. Injection with methylprednisolone proximal to the carpal tunnel: randomised double blind trial. BMJ. 1999;319:884–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis PT, Hulbert JR, Kassak KM, Meyer JJ. Comparative efficacy of conservative medical and chiropractic treatments for carpal tunnel syndrome: a randomized clinical trail. J Manipulative Physiol Ther. 1998;21:317–326. [PubMed] [Google Scholar]
- 19.Ebenbichler GR, Resch KL, Nicolakis P, et al. Ultrasound treatment for treating the carpal tunnel syndrome: randomised “sham” controlled trial. BMJ. 1998;316:731–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elbaz A, Gagnon S, Beaumont P, et al. Carpal tunnel syndrome: a double blind study of the effect of steroid injection. J Bone Joint Surg. 1994;76-B Suppl:22. [Google Scholar]
- 21.Garfinkel MS, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher HR Jr. Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA. 1998;280:1601–1603. [DOI] [PubMed] [Google Scholar]
- 22.Herskovitz S, Berger AR, Lipton RB. Low-dose, short-term oral prednisone in the treatment of carpal tunnel syndrome. Neurology. 1995;45:1923–1925. [DOI] [PubMed] [Google Scholar]
- 23.O’Gradaigh D, Merry P. Corticosteroid injection for the treatment of carpal tunnel syndrome. Ann Rheum Dis. 2000;59:918–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ozdogan H, Yazici H. The efficacy of local steroid injections in idiopathic carpal tunnel syndrome: a double-blind study. Brit J Rheumatol. 1984;23:272–275. [DOI] [PubMed] [Google Scholar]
- 25.Oztas O, Turan B, Bora I, Karakaya MK. Ultrasound therapy effect in carpal tunnel syndrome. Arch Phys Med Rehab. 1998;79:1540–1544. [DOI] [PubMed] [Google Scholar]
- 26.Rozmaryn LM, Dovelle S, Rothman ER, Gorman K, Olvey KM, Bartko JJ. Nerve and tendon gliding exercises and the conservative management of carpal tunnel syndrome. J Hand Ther. 1998;11:171–179. [DOI] [PubMed] [Google Scholar]
- 27.Spooner GR, Desai HB, Angel JF, Reeder BA, Donat JR. Using pyridoxine to treat carpal tunnel syndrome. Randomized control trial. Can Fam Phys. 1993;39:2122–2127. [PMC free article] [PubMed] [Google Scholar]
- 28.Stransky M, Rubin A, Lava NS, Lazaro RP. Treatment of carpal tunnel syndrome with vitamin B6: a double-blind study. South Med J. 1989;82:841–842. [DOI] [PubMed] [Google Scholar]
- 29.Walker WC, Metzler M, Cifu DX, Swartz Z. Neutral wrist splinting in carpal tunnel syndrome: a comparison of night-only versus full-time wear instructions. Arch Phys Med Rehab. 2000;81:424–429. [DOI] [PubMed] [Google Scholar]
- 30.Wong SM, Hui AC, Tang A, et al. Local vs systemic corticosteroids in the treatment of carpal tunnel syndrome. Neurology. 2001;56:1565–1567. [DOI] [PubMed] [Google Scholar]
- 31.Scottish Intercollegiate Guidelines Network (SIGN) revised grading system for recommendations in evidence-based clinical guidelines. Available at: http://www.sign.ac.uk.
- 32.Padua L, Padua R, Aprile I, Pasqualetti P, Tonali P, for the Italian CTSSGCts. Multiperspective follow-up of untreated carpal tunnel syndrome: a multicenter study. Neurology. 2001;56:1459–1466. [DOI] [PubMed] [Google Scholar]
- 33.Marshall S, Tardif G, Ashworth N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. 2002;CD001544. [DOI] [PubMed]
- 34.Burke DT, Burke MM, Stewart GW, Cambre A. Splinting for carpal tunnel syndrome: in search of the optimal angle. Arch Phys Med Rehab. 1994;75:1241–1244. [DOI] [PubMed] [Google Scholar]
- 35.Feuerstein M, Burrell LM, Miller VI, Lincoln A, Huang GD, Berger R. Clinical management of carpal tunnel syndrome: a 12-year review of outcomes. Am J Indust Med. 1999;35:232–245. [DOI] [PubMed] [Google Scholar]
- 36.Gerritsen A, de Vet H, Scholten R, Bertelsmann F, de Krom M, Bouter L. Splinting vs surgery in the treatment of carpal tunnel syndrome a randomized controlled trial. JAMA. 2002;288:1245–1251. [DOI] [PubMed] [Google Scholar]
- 37.Wolaniuk A, Vadhanavikit S, Folkers K. Electromyographic data differentiate patients with the carpal tunnel syndrome when double blindly treated with pyridoxine and placebo. Res Commun Chem Pathol Pharmacol. 1983;41:501–511. [PubMed] [Google Scholar]
- 38.Ellis J, Folkers K, Watanabe T, et al. Clinical results of a cross-over treatment with pyridoxine and placebo of the carpal tunnel syndrome. Am J Clin Nutr. 1979;32:2040–2046. [DOI] [PubMed] [Google Scholar]
- 39.Ellis JM, Folkers K, Levy M, et al. Response of vitamin B-6 deficiency and the carpal tunnel syndrome to pyridoxine. Proc Natl Acad Sci USA. 1982;79:7494–7498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.American Society of Plastic Surgeons (ASPS) Guidelines Committee. Carpal Tunnel Syndrome: Clinical Practice Guideline. Arlington: American Society of Plastic and Reconstructive Surgeons (ASPRS); 1998.
- 41.Gabriel SE, Jaakkimainen L, Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. A meta-analysis. Ann Intern Med. 1991;115:787–796. [DOI] [PubMed] [Google Scholar]
- 42.Bassler KH. Use and abuse of high dosages of vitamin B6. Intl J Vit Nutr Res - Suppl. 1989;30:120–126. [PubMed] [Google Scholar]
- 43.Hurwitz EL, Aker PD, Adams AH, Meeker WC, Shekelle PG. Manipulation and mobilization of the cervical spine. A systematic review of the literature. Spine. 1996;21:1746–1759; discussion 59–60. [DOI] [PubMed] [Google Scholar]
- 44.Rosner AL. Chiropractic: more good than harm or vice versa? J Manipulative Physiol Ther. 1999;22:250–253. [DOI] [PubMed] [Google Scholar]
- 45.Kluge W, Simpson RG, Nicol AC. Late complications after open carpal tunnel decompression. J Hand Surg. 1996;21:205–207. [DOI] [PubMed] [Google Scholar]
- 46.Light T. American Society for Surgery of the Hand: Hand surgery Update 2. Rosement, Ill: American Academy of Orthopedic Surgeons; 1999.
- 47.DeStefano F, Nordstrom DL, Vierkant RA. Long-term symptom outcomes of carpal tunnel syndrome and its treatment. J Hand Surg [Am]. 1997;22:200–210. [DOI] [PubMed] [Google Scholar]
- 48.Rosen B, Lundborg G, Abrahamsson SO, Hagberg L, Rosen I. Sensory function after median nerve decompression in carpal tunnel syndrome. Preoperative vs postoperative findings. J Hand Surg. 1997;22: 602–606. [DOI] [PubMed] [Google Scholar]