Abstract
To promote the range of interventions for building family/general practice (family medicine) research capacity, we describe successful international examples. Such examples of interventions that build research capacity focus on diseases and illness research, as well as process research; monitor the output of research in family/general practice (family medicine); increase the number of family medicine research journals; encourage and enable research skills acquisition (including making it part of professional training); strengthen the academic base; and promote research networks and collaborations. The responsibility for these interventions lies with the government, colleges and academies, and universities. There are exciting and varied methods of building research capacity in family medicine.
Keywords: Family practice, research, evidence-based practice, research capacity building
INTRODUCTION
In this issue, we see how family/general practice (family medicine) research is necessary, and the different forms it might take. This article focuses on research capacity building, examining the barriers to research and the means of overcoming them.
Family medicine research is important, not only for its own sake but also because it improves patient care, enables teachers to contribute to their discipline, and stimulates intellectual rigor and critical thinking.
Gaps in the evidence that clinicians need in making decisions must be filled to best manage patient care problems. Research in family medicine will help fill these gaps by addressing specifically those areas where evidence is lacking.
Good teachers contribute to the body of knowledge they teach, and research is the main avenue for this contribution. The following two barriers to this process are specific to family medicine: (1) family medicine academics and academic departments tend to be underfunded, and (2) there is less continuity between undergraduate and postgraduate training of family/general practitioners (family physicians), splitting the critical intellectual mass. This loss of continuity occurs structurally in several countries (United Kingdom, Australia, New Zealand, and South Africa), where the university teachers who taught the undergraduates do not provide postgraduate training. It also occurs functionally in many countries, because of the strong emphasis on hospital work in young physicians—a special problem for a discipline set in the community.
Research stimulates intellectual rigor and critical thinking generally. A strong research tradition is the most direct route to enhance the intellectual rigor of the discipline and the individual physicians’ critical thinking skills. Better critical thinking leads to more research, better quality care, and enhanced intellectual rigor.
LEVELS OF RESEARCH ENGAGEMENT
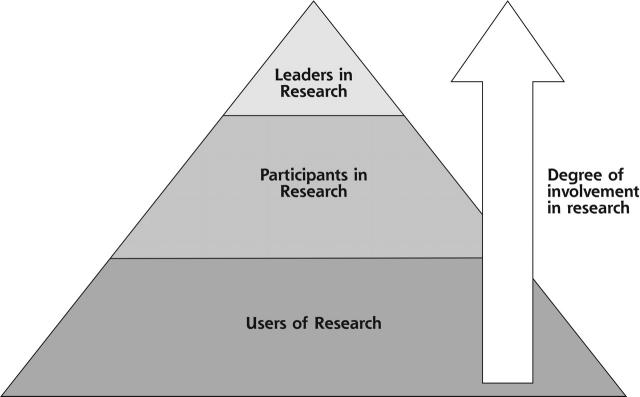
It is worth establishing at what level family medicine wants to build research capacity, as shown in Figure 1▶.1 Clinicians can be engaged in research as users, participants, and leaders. Ideally, all levels should be active. Within each level clinicians can be engaged in research to a greater (ideal) or lesser extent. Attention should be focussed on encouraging and facilitating clinicians to be engaged at the highest order within each level.
Figure 1.
Glasziou’s triangle: different levels of research engagement.
Reprinted from Del Mar C. Sexual dysfunction in the Australian population. Aust Fam Physician 2001;30:1094–1095. Reprinted with permission of Australian Family Physician.
For example, all clinicians use research evidence in their clinical practice (the base level of the triangle). Some clinicians simply subconsciously incorporate into their clinical practice research evidence from drug representatives, medical newspapers, lectures by specialists, and discussions with their colleagues.2
The highest order of users consciously seek the best available research evidence and appraise and combine it with clinical experience and patient values to inform their clinical decision making (the principals of evidence-based medicine).3
Attention to increasing the volume of conscious users will encourage critical enquiry among family physicians, highlight the evidence gaps, and perhaps inspire clinicians to address these gaps through involvement or instigation of research. Such attention in turn might move some clinicians up the triangle from users to participants and perhaps even to leaders in research.
HISTORICAL FIGURES IN FAMILY MEDICINE RESEARCH
Family medicine research has a long and important history that is dominated by individual physicians. Examples include Edward Jenner (1749–1823), who developed vaccination against smallpox; Sir James McKenzie (1853–1925), who developed the forerunner of the electrocardiogram; William Pickles (1885–1969), who characterized infectious hepatitis, and Bornholm disease; and F. J. Huygen, who undertook psychological studies in general practice.
These family physicians can serve as excellent role models for how to develop a research trajectory: they observed phenomena within their practices; concentrated on diseases; took pragmatic approaches to solving problems; and were meticulous and rigorous in their methods.4–6 They were convinced of the unique position (and duty) of family physicians to undertake the role of researcher. Emphasizing this point and promoting such exemplars to the current generation of family physicians might encourage some to adopt the role of a researcher.
RESEARCH AGENDAS—COMMISSIONED VS INVESTIGATOR-DRIVEN RESEARCH
The combination of burgeoning expenditure on health care and a realization that good primary care can arrest spiraling costs was the impetus of most western countries investing in and commissioning primary care research, particularly health services research.7,8 This research examines ways of improving delivery of health services and has an orientation that is more operational and economic than clinical research.
Workforce issues have also stimulated commissioned research. For example, in Australia, workforce research was associated with vocational registration of general practitioners.9 Additionally, many countries are concerned about geographical areas of need (inner cities in some countries and rural areas of others).
Health services research is important to community leaders and government bodies concerned with the rational allocation of limited health system resources, but such research is of limited relevance to physicians needing to know how best to care for their patients.
Preferably, family physicians will not only respond to commissioned research but also set the research agenda themselves by pursuing their own research ideas or desires regardless of whether it is perceived as a priority.
Research Agendas
In Australia, a family medicine research agenda was derived in a number of ways. One process established by the government led to a focus on health services research. Another led by general practice academics focused primarily on clinical issues.10 In the Netherlands, the Health Ministry was persuaded to set substantial funds aside for research into common clinical problems.11
Clinical research can be defined as research that attempts to inform clinical practice. It might be molecular, bench-top, based on patient contact, or epidemiological (population-based) and still qualify. Conversely, any research with these characteristics might not be classified as clinical research. It also encompasses much translation research, determining whether the outcomes of more basic research are both effective and efficient in the family medicine setting.7 Certainly clinical research is more applied than many other types of research.12
Is family medicine a process-based rather than a content-based discipline? If not content-based, what then characterizes it? The nub of the question revolves around the fact that for almost every disease there is a specialist. If the world is seen in terms of diseases, then there will be a specialist to be its expert. When a family physician researches a disease, is that physician becoming a specialist in a relevant discipline? Many public health specialists, for example, have arrived at that destination from family medicine.
Nevertheless, there are illnesses and diseases that family physicians are expert in managing, and they should be seen as experts in researching them.
INCREASING FAMILY MEDICINE RESEARCH
There are indications that the amount of family medicine research is increasing. In Australia, there was a fivefold increase in the number of family medicine published papers from the 1980s to the 1990s, with an associated increase in international publications.13 In the Netherlands, international research publications increased tenfold between 1983 – 1987 and 1988 – 1992.14 Reasons for this increase include both the maturation of the discipline and the general increase in research across all health disciplines.
On the other hand, the publication rate of family medicine is low compared with its physician base. Australian family physicians published 1 paper for every 1,000 family physicians per year during the 1990s—a deplorably low rate when compared with 60 papers published for every 1,000 surgeons, 100 for every 1,000 physicians, and 150 for every 1,000 public health physicians.15
MEASURING THE QUALITY OF FAMILY MEDICINE RESEARCH
Quality can be measured in different ways: by its scientific quality, commonly measured by the impact factor of publications and journals; and by its relevance to implementation by clinicians and policy makers, which is more difficult to measure, although the Netherlands have developed criteria and indicators for measuring societal impact of research.16,17 Developing quantitative methods of measuring research quality may help benchmarking.
International Publications
The more generalizable a research paper, the more likely it is to be accepted by an international journal. To reach local family physicians, however, the research must be published in the journals they read and in their language.18 Clearly a balance has to be established between these conflicting needs.
Publications in General Medical Journals
Family medicine research published in general medical journals is a good index of quality. Although the British Medical Journal includes a section devoted to primary care research, few other general medical journals are committed to publish family medicine research on a regular basis. Of 90 original research articles published during 1999 in the Medical Journal of Australia (Australia’s leading general medical journal), only 3% were from family medicine compared with 37% from medicine.15
Impact Factor of Family Medicine Journals
The impact factor is the ratio of the number of times a journal’s publications are cited divided by the number of articles it published in the previous 2 years. Many family medicine journals do not feature in this index, such as, for example, Australian Family Physician with its circulation of approximately 20,000, European Journal of Primary Care, or Nederlands Tijdschrift Voor Geneeskunde. Although often misused as a measure of a journal’s scientific quality,19 inclusion in this ranking system may increase the status of family medicine journals.
INTERVENTIONS TO INCREASE RESEARCH IN FAMILY MEDICINE
Family medicine research may be enhanced through government interventions, university departments, colleges and academies, practice-based networks, international initiatives for cross-national efforts, and individual engagement.
Government and National Funding Bodies
Governments have traditionally supported research by funding (1) project research (ie, single-purpose research, lasting up to 3 years); (2) program research (ie, staged research, building on the results of preceding stages, often lasting 5 to 6 years); (3) scholarships or fellowships (ie, funding the research training of individuals rather than research projects or programs); and (4) infrastructure support (eg, university departments or professional colleges and academies).
Even so, national family medicine research programs might need special funding to enable them to become established because of bootstrapping problems, their track record, and bias toward basic research. Few family medicine researchers are sufficiently established to act as senior researchers (eg, doctoral supervisors). They are vulnerable because of their few numbers.20 Furthermore, success in being awarded research grants is predicated on past research success. The rich get richer, and few family physicians have a well-endowed research portfolio. Resolution of this problem requires affirmative action by government or national funding bodies. Finally, there is a funding bias toward fundamental and basic bench-top research. Family medicine, by its very nature, generates many clinical or applied research questions and is therefore susceptible to this bias.
If governments have family medicine research on their agendas, as shown by funding for research capacity building and for research activity itself, a clear message is sent to the clinical and academic communities that family medicine research is important and worthy of support.
For example, the Australian government has allocated $A50 million for 5 years (2000 to 2004) to support family medicine research—the Primary Health Care Research, Evaluation and Development Strategy (PHC-RED). This program was largely informed by the 1997 UK strategic review of research and development in primary care.20
Key elements of the strategy include the following:
A university research capacity building initiative for research skills development through academic mentoring; the development of research networks; and collaborative, multidisciplinary research
A national Primary Health Care (PHC) Research Institute to facilitate strategic and cohesive approaches for primary health care policy development and research
National Health & Medical Research Council (NHMRC) primary health care project grant allocation of dedicated additional funding to support primary health care research
NHMRC primary health care scholarships and fellowships that create financial support for those in the early to mid stages of research careers seeking to strengthen their research skills21
University Departments of Family Medicine
Universities are highly orientated to research. Activities to encourage family medicine research include aligning teaching material to reflect research activities (to stimulate students to regard the discipline of family medicine as worthy of intellectual pursuit—perhaps by promoting knowledge gaps as interesting and important opportunities for research); teaching research skills to students (for example, including research in the learning objectives of the sphere of family medicine); and funding for student vacation research projects.
A vocational route to academic family medicine can be promoted. This may be more difficult in countries with discontinuity between university and vocation-based education.
Promoting Doctorates
Doctoral (PhD) students drive much research in universities. Moreover, their arrival in a workforce establishes beachheads of expertise that can prove invaluable to the further development of research in the discipline. The contribution of an academic doctoral workforce to family medicine research has been very successful in the Netherlands.
Research Skills Training for Clinicians
Training clinicians in research skills enables and encourages family physicians to undertake research activity and potentially progress to higher research degrees. Training should cover research techniques (biostatistics, qualitative methods, and epidemiology) and the ancillary, indirect skills necessary to be an effective researcher (critical thinking, project management, and writing and communication skills).
For example, a collaborative initiative in Sweden between the university sector and regional family physicians resulted in an academic program of research training for family physicians. The part-time program aimed at practicing clinicians combined a formal course in basic research methods (assessed by written examination), and a supervised research project (assessed by oral defense). In the first 10 years of the program, 20% (138 of 700) of the family physicians in the region completed the theoretical component, with 75% of these having also completed the project. Outputs from the program include 15 articles published in English in international peer-reviewed journals, 11 published in local journals, and 17 PhD degrees (7 have defended their theses, and 10 are registered).22
For another example, in Australia the University of Queensland (with government PHC-RED funding) provides novice researcher fellowships to clinicians. These fellowships provide clinicians with funding for 1 day per week of protected time for 9 months, in addition to academic support, to enable them to develop research skills within a given project, such as a research proposal, grant application, or systematic review.
Colleges and National Academies
Curricula statements should address the acquisition of research skills in undergraduate and family medicine training similar to other medical disciplines, in which the acquisition of research skills is explicitly declared an essential component of training and examined. In such an institution research is mandatory.4
For example, Australian general practice registrars are expected to acquire competency in research during training. But general practice registrars wishing to do research are penalized because time spent away from clinical activities to undertake research must be added onto the end of their training period.
On the other hand, a research project is a mandatory component of the postgraduate vocational training of family physicians in Croatia. The best of the projects are published in medical journals or presented at the national family medicine conferences.
Research has often been given a low priority in the past. Strategies to redress this include committees to promote research within the organizations; scholarships; project funding (in particular, startup funding); workshops to improve research initiation and skills acquisition; and support for international collaborations (eg, the Wonca research workshop). Clearly there is possible overlap with the activities proposed earlier under universities.
Practice-Based Research Networks
Providing outreach services for family medicine research outside universities can be achieved in a number of ways. Practice-based research networks have been important in establishing research participation in a number of countries, including Israel, France, the Netherlands, Eastern Europe, United States, United Kingdom, and New Zealand.23–25 They have been referred to as the research laboratory26 of family medicine, because they provide opportunities for family physicians to identify research priorities and engage in research, offer networks for dissemination and implementation of research findings, and enable multidisciplinary research teams to address diverse research agendas.23
A notable success story is the Ambulatory Sentinel Practice Network (ASPN). For example, through collection of data from more than 1,300 patients cared for in member practices, ASPN was able to determine that following the recommendations of the consensus panel for the treatment of severe headache would result in considerable overservicing with no notable improvements in patient care.23
International Initiatives
The development of international alliances can facilitate the transfer of experience and expertise, foster research activity, fill gaps in local intellectual capacity, and increase the critical mass of leaders in family medicine research.7
One example is the Brisbane Initiative, a fledgling move to increase international collaboration for doctoral degrees (PhDs) by sharing educational resources, supervisors, and projects. Some family medicine researchers from the Netherlands, Australia, Scotland, England, and the United States are collaborating.
Another example is the Clinical Assessment of the Reliability of the Examination (CARE), a collaborative, international, Internet-based study of the accuracy and precision of the clinical examination. The premise behind CARE is that the Internet makes it relatively simple for large numbers of clinicians from different clinical settings (more than 900 clinicians from more than 80 countries are members of CARE) to enroll patients into studies of the accuracy and precision of specific elements of the history and physical examination.27
Individuals
Although many family physicians believe that research is important, they give it low priority in their work.28 Family medicine needs to demonstrate the benefits of engaging in research at any level of the involvement triangle.
CONCLUSIONS
Although family medicine has the potential to take an important role in setting and contributing to a research agenda, there are indications that family medicine research is not doing as well as it should in many parts of the world. Some possible innovations have set out different roles for different levels of the organization of family medicine. Family medicine may need to ensure that the discipline has a research portfolio that includes clinical research as well as health services research.
Recommendations
Recommendation 1.
International collaborations in family medicine research should continue.
Recommendation 2.
Governments should be made aware of (1) the prime role of family physicians in society, (2) the insecure place of family medicine research in their countries, (3) the government support necessary for stimulating family medicine research, and (4) the several ways that this can be done.
Recommendation 3.
The role of universities is important and should be enhanced by (1) increased collaboration between universities, and (2) development and promotion of international collaborations.
Recommendation 4.
Family medicine journals should be strengthened by (1) more secure citation indices, and (2) improving the quality of research published.
Recommendation 5.
The intellectual nature of family medicine should be encouraged by (1) enabling students and registrars to undertake research, (2) facilitating clinicians as participants and leaders of research, and (3) promoting the academic status of the discipline.
Acknowledgments
The following were kind enough to provide detailed feedback and examples: David Lanier MD, Center for Primary Care Research, Agency for Healthcare Research and Quality, Rockville, Maryland, USA; Julian Herrera, Universidad de Los Andes, Bogota, Colombia; Dr. Milica Katic MD, PhD, Department of Family Medicine, “Andrija Štampar” School of Public Health, Medical School University of Zagreb, Croatia; Dr. Martin Isler, Faculty Centre for General Practice (FIAM), Bernese Medical Faculty, Switzerland; Prof Chris van Weel, Department of Family Medicine, University Medical Centre, Nijmegen, the Netherlands.
Conflicts of interest: none reported
REFERENCES
- 1.Del Mar C. Publishing research in Australian Family Physician. Aust Fam Phys. 2001;30:1094–1095. [PubMed] [Google Scholar]
- 2.Armstrong D, Reyburn H, Jones R. A study of general practitioners’ reasons for changing their prescribing behaviour. BMJ. 1996;312:949–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sackett DL. Evidence-Based Medicine: How to Practice and Teach EBM. 2nd ed. New York, NY: Churchill Livingstone; 2000.
- 4.Gray DP. Research in general practice: law of inverse opportunity. BMJ. 1991;302:1380–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fry J. Profiles Of Disease : A Study in the Natural History of Common Diseases. Edinburgh: ES Livingstone; 1966.
- 6.Starfield B. Is primary care essential? Lancet. 1994;344:1129–1133. [DOI] [PubMed] [Google Scholar]
- 7.van Weel C. International research and the discipline of family medicine. Eur J Gen Pract. 1999;5:2–7. [Google Scholar]
- 8.Silagy C. Recent advances: general practice. BMJ. 1994;309:943–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Commonwealth of Australia. General Practice in Australia: 2000. 1st ed. Canberra: Commonwealth Department of Health and Aged Care; 2000.
- 10.Pond D. Priority setting and Australian general practice research. Aust Fam Physician. 2003;32:376. [PubMed] [Google Scholar]
- 11.Nederlands Huisartsen Genootschap Fund for Common Disorders. Available at: http://www.nhg.artsennet.hl. Accessed 4 August 2003.
- 12.van Weel C. General practice: a suitable place for clinical research. Eur J Gen Pract. 1995;1:6–7. [Google Scholar]
- 13.Ward A, Lopez D, Kamien M. General practice research in Australia, 1980–1999. Med J Aust. 2000;173:608–611. [DOI] [PubMed] [Google Scholar]
- 14.Knottnerus JA. Research in general practice. Lancet. 1996;347:1236–1238. [DOI] [PubMed] [Google Scholar]
- 15.Askew DA, Glasziou PP, Del Mar CB. Research output of Australian general practice: a comparison with medicine, surgery and public health. Med J Aust. 2001;175:77–80. [DOI] [PubMed] [Google Scholar]
- 16.Smith R. Measuring the social impact of research. BMJ. 2001;323:528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Royal Netherlands Academy of Arts and Sciences. The Societal Impact of Applied Health Research. Towards a Quality Assessment System. Available at: http://www.knaw.nl/publicaties/pdf/20021098.pdf.
- 18.van Weel C. Biomedical science matters for people—so its impact should be better assessed. Lancet. 2002;360:1034–1035. [DOI] [PubMed] [Google Scholar]
- 19.Smith R. Unscientific practice flourishes in science. BMJ. 1998; 316:1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mant D. R&D in Primary Care: National Working Group Report. Wetherby: NHS Executive, Department of Health; 1997.
- 21.Australian Department of Health and Ageing. The Primary Health Care Research, Evaluation and Development Strategy: General Practice Branch; 2002.
- 22.Hakansson A, Henriksson K, Isacsson A. Research methods courses for GPs: ten years’ experience in southern Sweden. Br J Gen Pract. 2000;50:811–812. [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas P, Griffiths F, Kai J, O’Dwyer A. Networks for research in primary health care. BMJ. 2001;322:588–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Green LA, Hames CG Sr, Nutting PA. Potential of practice-based research networks: experiences from ASPN. Ambulatory Sentinel Practice Network. J Fam Pract. 1994;38:400–406. [PubMed] [Google Scholar]
- 25.van Weel C, Smith H, Beasley JW. Family practice research networks. Experiences from 3 countries. J Fam Pract. 2000;49:938–943. [PubMed] [Google Scholar]
- 26.Green LA, Dovey SM. Practice based primary care research networks. They work and are ready for full development and support. BMJ. 2001;322:567–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.CARE Study. Clinical Assessment of the Reliability of the Examination (CARE). Available at: http://www.carestudy.com/CareStudy/.
- 28.Askew DA, Clavarino AM, Glasziou PP, Del Mar CB. General practice research: attitudes and involvement of Queensland general practitioners. Med J Aust. 2002;177:74–77. [DOI] [PubMed] [Google Scholar]