Abstract
PURPOSE The impact of comorbidity on use of primary care and specialty services is poorly understood. The purpose of this study was to determine the relationship between morbidity burden, comorbid conditions, and use of primary care and specialist services
METHODS The study population was a 5% random sample of Medicare beneficiaries, taken from 1999 Medicare files. We analyzed the number of ambulatory face-to-face patient visits to primary care physicians and specialists for each diagnosis, with each one first considered as the “main” one and then as a comorbid diagnosis to another. Each patient was categorized by extent of total morbidity burden using the Johns Hopkins Adjusted Clinical Group case-mix system.
RESULTS Higher morbidity burden was associated with more visits to specialists, but not to primary care physicians. Patients with most diagnoses had more visits, both to primary care and specialist physicians for comorbid diagnoses than for the main diagnosis itself. Although patients, especially those with high morbidity burdens, generally made more visits to specialists than to primary care physicians, this finding was not always the case. For patients with 66 diagnoses, primary care visits for those diagnoses exceeded specialist visits in all morbidity burden groups; for patients with 87 diagnoses, specialty visits exceeded primary care visits in all morbidity burden groups.
CONCLUSION In the elderly, a high morbidity burden leads to higher use of specialist physicians, but not primary care physicians, even for patients with common diagnoses not generally considered to require specialist care. This finding calls for a better understanding of the relative roles of generalists and specialists in the US health services system.
Keywords: Comorbidity; primary care use, general/specialist care
INTRODUCTION
The impact of comorbidity on use of services is poorly understood One study of Medicare beneficiaries found a relationship between the number of comorbid chronic conditions and total costs of care, frequency of ambulatory-care–sensitive hospitalizations, and the occurrence of complications of care.1 Another study found the salience of primary care services in the presence of several diagnoses both in children and adults by showing that the average number of primary care visits was greater than the number of visits to specialists, for the diagnosis itself as well as for comorbid conditions.2 Only a few diagnoses were studied, however, and the population was limited to individuals younger than 65 years of age, when comorbidities occur less frequently.
To understand better the challenges of coexisting diagnoses, we examined the frequency of primary care physician and specialist visits in persons aged 65 years and older in the context of their overall morbidity burdens. Consistent with our earlier study with a limited number of diagnoses in younger adults,2 we expected to find that visits to primary care physicians dominate visits to specialists, and that the less frequent the problem, the greater proportion of visits to specialists.3
METHODS
Data Source and Study Population
We conducted a retrospective analysis of administrative claims data for Medicare beneficiaries using the Standard Analytic File, a 5% nationally random sample of Medicare beneficiaries aged 65 years and older in 1999. To be included in the study, the individual had to be a US resident, not enrolled in an HMO during any month while alive, and have both Part A and Part B Medicare coverage for each month the person was alive. A total of 1,133,030 persons had valid diagnoses in either the inpatient or outpatient files.
Because there is no way to identify a main diagnosis from administrative data, we included all medical diagnoses from the line-item physician supplier form, except for diagnoses with CPT codes associated with radiographic and laboratory services (CPT codes 36000-36493 and 70000-87999). All diagnoses were recoded into a collapsed diagnosis system (EDCs), which are groups of similar conditions that are likely to be seen by the same type of physician, eg, urologic conditions (http://acg.jhsph.edu). Diagnoses with a frequency of less than 0.03 per 1000 (ie, fewer than 50 people) were excluded, thus leaving a total of 179 diagnoses for the analysis.
The Johns Hopkins Adjusted Clinical Group (ACG) case-mix system (http://www.acg.jhsph.edu) separated Medicare beneficiaries into lowest, intermediate, and highest degree of overall morbidity burden.* This approach first assigns all diagnoses given to each patient in a year into 1 of 32 groups, each relatively homogeneous with regard to likelihood of persistence, severity, and likely use of services. During the course of the year, users of services theoretically could have as few as 1 diagnosis and as many as 32 different types of morbidity. Second, patients with various combinations of types of diagnoses are assigned to 1 of 89 mutually exclusive cells (ACGs) reflecting their pattern and number of different types of diagnoses, ie, their morbidity burden. We then divided Medicare patients into 3 approximately equal-sized morbidity burden groups: lowest (persons with fewer than 6 types of conditions), intermediate (6 to 9 different types), and highest (persons with 10 or more types of conditions).
Family physicians and general internists (without a subspecialty self-designation, but including geriatricians) were considered primary care physicians. All others were considered specialists.
Data Analysis
Each physician contact in an outpatient facility, emergency department, or physician practice setting represented a visit in this analysis.
Visits for each of the diagnoses given to a patient at least once during the year were summed for primary care and specialist physicians and averaged for the population. Visits for comorbid diagnoses included visits in which other diagnoses were recorded. Thus, each diagnosis was represented both as a diagnosis and, if it occurred in a patient who had another diagnosis, as a comorbid diagnosis. These visits were similarly summed and averaged.
We used paired t tests to test for differences in number of visits to primary care and specialist physicians for each diagnosis. To protect against an increased type I error associated with the large number of paired t tests, we adjusted the P values using the Hochberg’s multiple test error rate adjustment.4
RESULTS
Number of Visits by Patients With Each Diagnosis
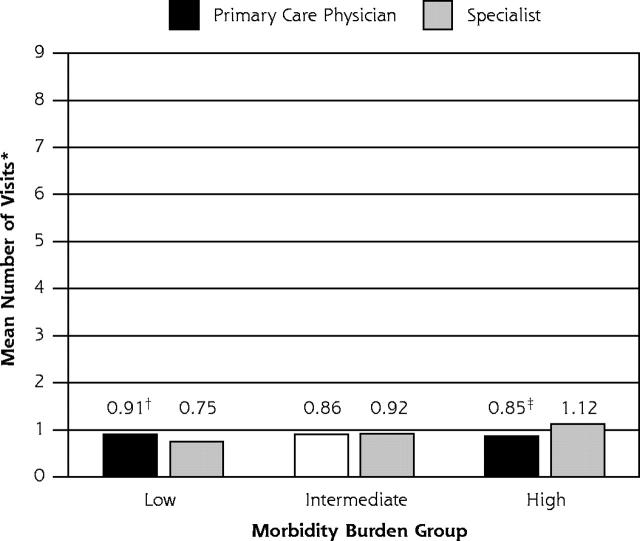
Figure 1 ▶ shows the relationship between the average number of visits to primary care physicians and specialists by patients in each morbidity burden group. For patients with the lowest morbidity burden, primary care physicians were visited significantly (P <.05) more than specialists. For those in the intermediate morbidity burden group, there were no statistically significant differences. In the highest morbidity burden group, patients visited specialists significantly more often than they visited primary care physicians (P <.01). Although the average number of visits to specialists increased with increasing morbidity burden, the mean number of visits to primary care physicians decreased with increasing morbidity burden.
Figure 1.
Average number of primary care and specialist physician visits for patients with 179 conditions, each considered as the main condition in adults aged 65 years and older, by morbidity burden.
Note: All 179 conditions were weighted to take into account differences in their prevalences.
* Per patient per year.
† P < .05, using a paired t test.
‡ P < .01, using a paired t test.
Visits Associated With Comorbid Diagnoses
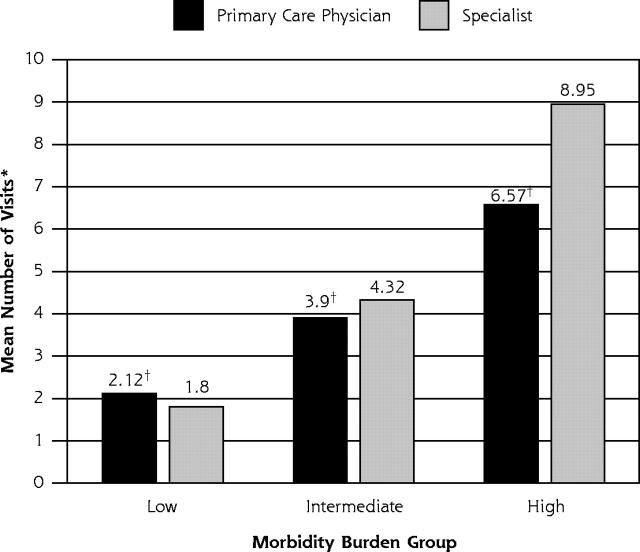
Figure 2 ▶ shows that the average number of visits for comorbid diagnoses markedly increased with increasing morbidity burden, with larger increases for specialists than for primary care physicians. Thus, the greater number of visits associated with higher morbidity burdens is associated with more visits to specialists.
Figure 2.
Average number of primary care and specialist physician visits for patients for comorbid conditions, in adults aged 65 years and older, by morbidity burden.
Note: Conditions were weighted to take into account differences in their prevalences.
* Per patient per year.
† P < .0001, using a paired t test whereby diagnoses are weighted by the number of patients.
Comparison of Figures 1 ▶ and 2 ▶ shows that, in every morbidity burden group, the mean number of visits for comorbid diagnoses far exceeded the number of visits for the individual diagnosis, both to primary care physicians and specialists. In 170 of 179 diagnoses, the mean number of physician visits to primary care physicians and specialists was greater for comorbid diagnoses than for the individual diagnosis for patients in every morbidity burden group; that is, the number of visits for other diagnoses almost always exceeded the number of visits for any single diagnosis.
Differences in Focus of Primary Care and Specialty Care
The previous results reflect average number of visits associated with the 179 diagnoses. The number of primary care visits for each of the 179 diagnoses was, however, significantly greater than the number of specialist visits in all morbidity burden groups for 66 of the 179 diagnoses. The 179 diagnoses might be considered as diagnosed mainly by primary care physicians, because they were recorded more by primary care physicians than by specialists. Examples are displayed in Table 1 ▶.
Table 1.
Number of Patient Visits to Primary Care and Specialist Physicians for Diagnoses With a Primary Care Focus
| Overall Morbidity Burden | |||||||
| Lowest | Intermediate | Highest | |||||
| Diagnosis | Prevalence per 1,000 | Visits to Primary Care | Visits to Specialists | Visits to Primary Care | Visits to Specialists | Visits to Primary Care | Visits to Specialists |
| General medical examination | 395 | 0.94 | 0.24 | 0.94 | 0.33 | 0.92 | 0.41 |
| Hypertension | 314 | 1.83 | 0.27 | 1.94 | 0.35 | 2.00 | 0.48 |
| Disorders of lipoid metabolism | 117 | 1.37 | 0.20 | 1.36 | 0.23 | 1.31 | 0.30 |
| Diabetes mellitus | 115 | 2.11 | 0.49 | 2.24 | 0.72 | 2.38 | 0.97 |
| Acute lower respiratory tract infection | 94 | 1.22 | 0.10 | 1.28 | 0.14 | 1.34 | 0.22 |
| Chest pain | 91 | 0.76 | 0.53 | 0.77 | 0.63 | 0.80 | 0.75 |
| Acute upper respiratory tract infection | 67 | 1.06 | 0.11 | 1.07 | 0.14 | 1.06 | 0.22 |
| Emphysema, chronic bronchitis, | 63 | 1.31 | 0.60 | 1.49 | 0.71 | 1.64 | 0.97 |
| COPD | |||||||
| Congestive heart failure | 57 | 1.29 | 0.66 | 1.40 | 0.74 | 1.51 | 0.87 |
| Abdominal pain | 52 | 0.92 | 0.32 | 0.91 | 0.44 | 0.94 | 0.60 |
| Urinary tract infections | 47 | 0.98 | 0.38 | 0.94 | 0.53 | 0.92 | 0.69 |
| Iron deficiency, other deficiency anemias | 47 | 2.32 | 0.63 | 2.04 | 0.92 | 1.83 | 1.34 |
| Thyroid disease | 44 | 1.25 | 0.27 | 1.27 | 0.33 | 1.25 | 0.41 |
| Sinusitis | 41 | 1.04 | 0.17 | 1.03 | 0.28 | 1.00 | 0.49 |
| Vertiginous syndromes | 39 | 0.92 | 0.34 | 0.91 | 0.50 | 0.88 | 0.69 |
| Gastroesophageal reflux | 38 | 0.94 | 0.38 | 0.88 | 0.54 | 0.79 | 0.74 |
| Nonfungal infections of skin | 27 | 1.10 | 0.33 | 1.13 | 0.44 | 1.07 | 0.60 |
| Peptic ulcer disease | 27 | 0.98 | 0.30 | 0.90 | 0.43 | 0.80 | 0.61 |
| Asthma | 26 | 1.13 | 0.76 | 1.22 | 0.89 | 1.23 | 1.10 |
| Arthropathy | 25 | 1.11 | 0.28 | 1.10 | 0.33 | 1.08 | 0.43 |
| Osteoporosis | 24 | 0.97 | 0.30 | 0.93 | 0.40 | 0.89 | 0.55 |
| Contusions and abrasions | 23 | 0.92 | 0.24 | 0.89 | 0.29 | 0.88 | 0.38 |
| Diarrhea | 22 | 0.96 | 0.26 | 0.90 | 0.41 | 0.92 | 0.51 |
| Edema | 21 | 1.08 | 0.19 | 1.12 | 0.23 | 1.12 | 0.28 |
| Cough | 19 | 0.94 | 0.24 | 0.91 | 0.35 | 0.87 | 0.50 |
| Generalized atherosclerosis | 18 | 1.12 | 0.43 | 1.12 | 0.49 | 1.09 | 0.57 |
| Exanthems | 17 | 1.02 | 0.41 | 0.99 | 0.51 | 0.98 | 0.66 |
| Nonspecific signs and symptoms | 17 | 0.92 | 0.31 | 0.92 | 0.37 | 0.88 | 0.45 |
| Lacerations | 17 | 0.99 | 0.30 | 0.96 | 0.40 | 0.93 | 0.59 |
| Depression, anxiety, neuroses | 16 | 1.32 | 0.12 | 1.28 | 0.14 | 1.26 | 0.18 |
| Headaches | 16 | 0.89 | 0.46 | 0.92 | 0.50 | 0.94 | 0.64 |
| Cervical pain syndromes | 16 | 1.02 | 0.47 | 0.98 | 0.77 | 1.06 | 1.06 |
| Constipation | 14 | 0.81 | 0.34 | 0.78 | 0.45 | 0.72 | 0.59 |
| Fluid/electrolyte disturbances | 13 | 1.09 | 0.21 | 1.07 | 0.29 | 1.09 | 0.37 |
| Dementia and delirium | 13 | 1.06 | 0.52 | 1.10 | 0.58 | 1.00 | 0.65 |
| Thrombophlebitis | 10 | 1.94 | 0.55 | 1.66 | 0.59 | 1.45 | 0.70 |
Note: A primary care focus implies that the diagnoses are made more often for patients in primary care than in specialty care. Differences are significant at the .005 level (unless indicated by ns) using paired t tests with Hochberg multiple test family-wise error rate adjustment. Not all 66 diagnoses shown.
COPD = chronic obstructive pulmonary disease.
The number of primary care visits exceeded the number of specialty visits in the lowest and intermediate (but not the highest) morbidity burden groups for patients with an additional 9 diagnoses. Included in this category are musculoskeletal signs and symptoms and low back pain.
For patients with 87 diagnoses, visits to specialists exceeded visits to primary care physicians in all morbidity burden groups (Table 2 ▶ displays examples). These diagnoses may be considered to be specialty focused, as they are recorded more by specialists than by primary care physicians. Some of these conditions are quite common (prevalences, Table 2 ▶).
Table 2.
Number of Patient Visits to Primary Care and Specialist Physicians for Diagnoses With a Specialty Care Focus, by Overall Morbidity Burden
| Overall Morbidity Burden | |||||||
| Lowest | Intermediate | Highest | |||||
| Diagnosis | Prevalence per 1,000 | Visits to Primary Care | Visits to Specialists | Visits to Primary Care | Visits to Specialists | Visits to Primary Care | Visits to Specialists |
| Cataract, aphakia | 187 | 0.03 | 1.31 | 0.04 | 1.40 | 0.04 | 1.47 |
| Ischemic heart disease | 152 | 0.90 | 1.17 | 1.01 | 1.35 | 1.08 | 1.60 |
| Benign and unspecified neoplasm | 108 | 0.23 | 1.16 | 0.22 | 1.28 | 0.24 | 1.43 |
| Skin keratoses | 108 | 0.14 | 1.31 | 0.13 | 1.41 | 0.12 | 1.52 |
| Cardiac arrhythmia | 102 | 1.29 | 1.49 | 1.35 | 1.65 | 1.31 | 1.78 |
| Glaucoma | 87 | 0.01 | 2.28 | 0.01 | 2.29 | 0.01 | 2.29 |
| Low-impact malignant neoplasms | 82 | 0.38 | 2.79 | 0.50 | 3.31 | 0.62 | 4.03 |
| Retinal disorders (excluding diabetic retinopathy) | 65 | 0.01 | 1.56 | 0.02 | 1.68 | 0.02 | 1.75 |
| Cerebrovascular disease | 54 | 0.80 | 0.85 | 0.81 | 0.95 | 0.85 | 1.05 |
| Urinary symptoms | 53 | 0.50 | 0.94 | 0.44 | 1.15 | 0.41 | 1.34 |
| Prostatic hypertrophy | 52 | 0.41 | 0.97 | 0.35 | 1.15 | 0.28 | 1.34 |
| Cardiovascular signs and symptoms | 51 | 0.59 | 0.62 | 0.58 | 0.71 | 0.56 | 0.80 |
| Dermatitis and eczema | 49 | 0.51 | 0.88 | 0.43 | 1.02 | 0.38 | 1.17 |
| Bursitis, synovitis, tenosynovitis | 48 | 0.67 | 0.82 | 0.59 | 1.04 | 0.55 | 1.34 |
| Malignant neoplasms of the skin | 48 | 0.13 | 1.75 | 0.12 | 1.86 | 0.11 | 1.96 |
| Surgical aftercare | 48 | 0.16 | 1.44 | 0.23 | 1.61 | 0.25 | 1.71 |
| Cardiac valve disorders | 41 | 0.42 | 1.06 | 0.41 | 1.08 | 0.39 | 1.17 |
| Allergic rhinitis | 37 | 1.12 | 1.93 | 1.20 | 2.27 | 1.14 | 2.69 |
| Gastrointestinal signs and symptoms | 34 | 0.59 | 0.61 | 0.52 | 0.78 | 0.49 | 0.89 |
| Peripheral neuropathy, neuritis | 29 | 0.64 | 1.04 | 0.57 | 1.24 | 0.53 | 1.40 |
| Conjunctivitis, keratitis | 26 | 0.27 | 1.01 | 0.21 | 1.19 | 0.18 | 1.33 |
| Disorders of the eyelid and lacrimal duct | 26 | 0.02 | 1.26 | 0.02 | 1.38 | 0.02 | 1.50 |
| Fractures (excluding digits) | 26 | 0.45 | 1.62 | 0.45 | 1.60 | 0.48 | 1.51 |
| Autoimmune and connective tissue disease | 24 | 1.12 | 1.93 | 1.30 | 2.16 | 1.34 | 2.34 |
| Deafness, hearing loss | 24 | 0.17 | 0.98 | 0.14 | 1.07 | 0.09 | 1.16 |
| Menopausal symptoms | 22 | 0.45 | 0.76 | 0.39 | 0.83 | 0.39 | 0.90 |
| Peripheral vascular disease | 22 | 0.62 | 0.88 | 0.61 | 1.04 | 0.55 | 1.27 |
| Vaginitis, vulvitis, cervicitis | 21 | 0.41 | 0.70 | 0.35 | 0.80 | 0.33 | 0.91 |
| Other skin disorders | 19 | 0.49 | 0.68 | 0.44 | 0.74 | 0.37 | 0.84 |
| Ophthalmic signs and symptoms | 16 | 0.06 | 1.04 | 0.08 | 1.06 | 0.10 | 1.09 |
| High-impact malignant neoplasms | 16 | 0.62 | 3.51 | 0.93 | 4.36 | 0.98 | 4.89 |
| Refractive errors | 15 | 0.00 | 1.02 | 0.00 | 1.04 | 0.00 | 1.05 |
| Uterovaginal prolapse | 15 | 0.23 | 1.51 | 0.18 | 1.69 | 0.16 | 1.84 |
| Infections of eyelid | 14 | 0.08 | 1.16 | 0.07 | 1.23 | 0.05 | 1.29 |
| Sebaceous cyst | 14 | 0.44 | 0.87 | 0.34 | 0.96 | 0.26 | 1.04 |
| Joint disorders, trauma related | 13 | 0.35 | 1.22 | 0.34 | 1.41 | 0.33 | 1.48 |
Note: A specialist focus implies the diagnosis is made more often for patients in specialty care than in primary care. Differences are significant at the .005 level (unless indicated by ns) using paired t tests with Hochberg multiple test family-wise error rate adjustment. Not all 87 diagnoses shown.
The number of specialist visits exceeded the number of primary care visits in the intermediate and highest (but not the lowest) morbidity burden groups for an additional 17 diagnoses. Included in this category are degenerative joint disease and respiratory tract signs and symptoms.
A slightly greater percentage of visits to specialists (42%) than to primary care physicians (35%) were associated with a diagnosis that had a frequency of less than 20 per 1,000; conversely, a slightly lower percentage of diagnoses to specialists (20%) than to primary care physicians (25%) had a prevalence of greater than 100 per 1,000. Even so, there were many common conditions for which there were more visits to specialists than generalists and many uncommon conditions for which there were more visits to primary care physicians than there were to specialists (prevalences, Tables 1 ▶ and 2 ▶).
DISCUSSION
The study found that first, an increasingly high morbidity burden is associated with increasingly larger number of visits to specialists, particularly for comorbid conditions. Second, about one third of diagnoses are made mainly in primary care, regardless of the degree of overall morbidity burden. Third, the number of visits for comorbid conditions far exceeds the number of visits for any individual diagnosis in individual patients. Fourth, specialist visits dominate regardless of the extent of overall morbidity burden, even for conditions that are generally in the purview of primary care (ie, conditions of high prevalence). Finally, prevalence was not associated with the number of visits to specialists or generalists, in contrast to visit-based analyses in general populations.3
Limitations
There are several potential limitations of this study. We could not determine the main diagnosis in individual patients. Coding rules do not provide criteria for ranking different conditions in medical records as to their clinical priority; consequently, there is no way to distinguish principal diagnoses from other diagnoses. Because 87% of all visits had only 1 diagnosis, and fewer than 2% had 3 or more, the multiplicity of diagnoses in individual patients comes from the multiplicity of visits and not from the listing of comorbid diagnoses in different visits. Statistical issues in studies in which the unit of analysis is patients with diagnoses rather than patients or visits have not been well thought-out, and there are few, if any, previous studies that have come to grips with the challenges of comorbidity.
Our data set may not reflect all conditions experienced by patients; that is, prevalence rates are really treated prevalence rates. Thus, the analyses underestimate the extent of morbidity burden as well as degree of comorbidity, but the impact on primary care vs specialty visits is unknown.
Although primary care and specialist physicians may use different names to designate the same problem, the system used to categorize diagnoses in this study (the EDCs) was specifically designed to deal with this issue by giving the same code to similar diagnoses. A related concern is that billing practices of generalists and specialists may vary systematically, thus giving different numbers and types of diagnoses. It seems unlikely that billing practice would make a difference with regard to number of diagnoses (as most visits had only 1), but it might make a difference as to the diagnoses recorded.
In addition, we cannot determine, for individual patients, whether large numbers of visits to specialists represent many visits to a few specialists or visits to many different specialists. The variety of types of diagnoses made in specialist visits suggests that large numbers of visits to specialists are likely to be a result of visits to a variety of types of specialists.
Furthermore, it is possible that specialists would record fewer diagnoses because of their specialty interest, which, if so, would have the effect of underestimating the number of visits to specialists for specific conditions.
Implications
The findings of this study indicate the high salience of comorbidity in the care of elderly patients. In the absence of any system to assign a main diagnosis to patients for a period of time, a more appropriate designation would be multimorbidity,5,6 which is characteristic of elderly patients. Little is known about the relative roles of primary care physicians and specialists in the long term, particularly in the presence of multimorbidity.
The importance of a primary care physician in the care of all conditions, except those that are highly complex or rare, is increasingly recognized, at least from data on visits. For example, data from the National Ambulatory Medical Care Survey for all ages show that most physician visits for common, serious conditions occur in primary care practice: 85% for chronic obstructive pulmonary disease, 82% for hypertension, 68% for diabetes, 58% for stroke, 57% for coronary artery disease, and 56% for asthma.7 Others have also indicated that primary care physicians provide about 80% of the visits for such conditions as diabetes and hypertension.8 Our study, which used the patient (over time) as the unit of analysis, qualified these findings in a major way: for Medicare beneficiaries in the United States, specialists played a major role in the care of many common conditions, particularly when the level of morbidity burden was high.
Previous research in a younger, commercially insured and managed care population used the same methods as in this study but reached somewhat different conclusions.9 That study showed much lower relative frequency of use of specialists (with much less of a difference in use of primary care physicians) and a predominance of primary care visits in all but the highest morbidity burden category. The Medicare program may engender much greater use of specialists because there is generally free choice of physician and no requirement for referrals from primary care, as would be encouraged or even required in some commercial managed care organizations. An alternative explanation is that greater specialist use among the elderly is a result of greater morbidity burden; even though use was assessed after stratifying for overall morbidity burden, the elderly may have greater morbidity burden within each category. When we categorized the Medicare population into the same morbidity burden groupings as was done in the earlier study, most of the Medicare beneficiaries fell into the highest morbidity category. The small proportion that were in the lowest morbidity categories, however, had the same predominance of primary care visits as the managed care population, suggesting that the differences between the younger and older populations are in part due to a greater propensity of the elderly with comorbid conditions to visit specialists and not solely due to increasing morbidity in the older population.
Although it is intuitively obvious that patients with more morbidity (such as the elderly) use more services, it is not obvious that patients with a high morbidity burden should be receiving so much care from specialists rather than from primary care physicians. Most comorbid conditions receiving care from specialists are extremely common, and there may be legitimate questions about the need for specialist care. Because specialists are more likely than generalists to suspect serious abnormalities, they are more likely to do extensive and unnecessary procedures.10–11 As a result, primary care physicians are better overall diagnosticians than are specialists, and specialist performance is better in patients referred by primary care physicians.12 A related issue concerns evaluations of the quality of care. Although specialists generally achieve better quality of care (but only in their own area of competence), generalists do better when the measures are generic (ie, not disease specific).13 Inappropriate use of specialists could contribute to explaining why costs are higher in areas with a greater numbers of specialists, even though there is no improvement in outcomes among the elderly.14–16
Dealing with the challenges of comorbidity (including appropriateness of disease-oriented guidelines in the presence of other morbidity) might be approached by assigning patients with complex needs to case managers for coordination of care rather than to disease managers17 who focus primarily on particular conditions. Prioritizing needs to address those aspects of comorbidity that are most urgent, concerted attention to management of complex medication effects, and management by a nursing team skilled in various specialties would be appropriate foci for management and thus would approximate the functions of patient-focused primary care rather than focus on particular conditions (the hallmark of conventional specialty care).18 Alternatively, primary care physicians could be helped to be better coordinators of care19 through improved division of responsibility with specialists and collaboration with other health professionals working in teams.
Existing data from national research networks indicate that at least one half of referrals to specialists from family physicians and pediatricians are for short-term needs, such as advice with diagnosis or therapy or short-term specific tests or procedures19,20; only referrals to allergists, ophthalmologists, and psychiatrists are likely to be for long-term management in more than 30% of instances.2 Moreover, primary care physicians generally express an interest in sharing care (with specialists) rather than passing responsibility to specialists.19,20
Consultations with specialists directly (rather than through the patient) may be more efficient overall and more convenient for the patient. Trials of teleconsultations or specialist outreach sessions (in general practitioner offices) as alternatives to referrals show promise.21 Similarly, a simple intervention consisting of giving primary care physicians cameras and direct access to specialists resulted in a 25% reduction in dermatologist visits by patients.22 Various attempts to reduce unnecessary specialist visits through better mechanisms of information transfer (such as integrated electronic medical records23) have had modest success, and there have been trials (particularly involving patients with specific diseases, such as diabetes) in which consultants do not see the patient but provide education, support, and strategic planning to the primary care physicians.24
Policy strategies might profitably be undertaken to provide incentives to professional organizations to reevaluate the roles of specialists. For many conditions, specialists might better serve as consultants to the primary care physician rather than undertake management strategies directly with individual patients, at least for specific types of clinical interventions and patient needs. The staggering extent of morbidity burden within the population9 makes it necessary to find alternatives to unnecessary specialty care in the search for effectiveness, efficiency, and equity in health services delivery.
Conflicts of interest: none reported
Funding support: This work was supported in part by Grant No. 6 U30 CS 00189-05 S1 R1 of the Bureau of Primary Health Care, Health Resources and Services Administration, Department of Health and Human Services, to the Primary Care Policy Center for the Underserved at Johns Hopkins University, and by the Partnership for Solutions, a national program of the Robert Wood Johnson Foundation.
Footnotes
The Johns Hopkins University has copyrighted software based on the ACG case-mix system applied in this study. Royalties are paid to the university when this software is used by insurance plans and commercial organizations.
REFERENCES
- 1.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–2276. [DOI] [PubMed] [Google Scholar]
- 2.Starfield B, Forrest CB, Nutting PA, von Schrader S. Variability in physician referral decisions. J Am Board Fam Pract. 2002;15:473–480. [PubMed] [Google Scholar]
- 3.Forrest CB, Reid RJ. Passing the baton: HMOs’ influence on referrals to specialty care. Health Aff (Millwood). 1997;16:157–162. [DOI] [PubMed] [Google Scholar]
- 4.Hochberg Y. A sharper Bonferoni procedure for multiple tests of significance. Biometrika. 1988:800–802.
- 5.van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol. 1998;51:367–375. [DOI] [PubMed] [Google Scholar]
- 6.van den Akker M, Buntinx F, Roos S, Knottnerus JA. Problems in determining occurrence rates of multimorbidity. J Clin Epidemiol. 2001;54:675–679. [DOI] [PubMed] [Google Scholar]
- 7.Green LA. Is primary care worthy of physicians? In: Showstack J, Rothman AA, Hassmiller SB, eds. The Future of Primary Care. San Francisco, Calif: Jossey-Bass; 2004:143–160.
- 8.Grumbach K, Bodenheimer T. A primary care home for Americans: putting the house in order. JAMA. 2002;288:889–893. [DOI] [PubMed] [Google Scholar]
- 9.Starfield B, Lemke KW, Bernhardt T, et al. Comorbidity: implications for the importance of primary care in ‘case’ management. Ann Fam Med. 2003;1:8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sox HC. Decision-making: a comparison of referral practice and primary care. J Fam Pract. 1996;42:155–160. [PubMed] [Google Scholar]
- 11.Sackett DL, Haynes RB. The architecture of diagnostic research. BMJ. 2002;324:539–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hashem A, Chi MT, Friedman CP. Medical errors as a result of specialization. J Biomed Inform. 2003;36:61–69. [DOI] [PubMed] [Google Scholar]
- 13.Starfield B. Deconstructing primary care. In: Showstack J, Rothman AA, Hassmiller SB, eds. The Future of Primary Care. San Francisco, Calif: Jossey-Bass; 2004.
- 14.Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–287. [DOI] [PubMed] [Google Scholar]
- 15.Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138:288–298. [DOI] [PubMed] [Google Scholar]
- 16.Baicker K, Chandra A. The productivity of physician specialization: evidence from the Medicare program. Am Econ Rev. 2004;94:357–361. [DOI] [PubMed] [Google Scholar]
- 17.Johnson A. Measuring DM’s net effect is harder than you might think. Manag Care. 2003;12:28–32. [PubMed] [Google Scholar]
- 18.Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, eds. Primary Care: America’s Health in a New Era. Washington, DC: National Academy Press; 1996. [PubMed]
- 19.Forrest CB, Glade GB, Baker AE, et al. The pediatric primary-specialty care interface: how pediatricians refer children and adolescents to specialty care. Arch Pediatr Adolesc Med. 1999;153:705–714. [DOI] [PubMed] [Google Scholar]
- 20.Forrest CB, Nutting PA, Starfield B, von Schrader S. Family physicians’ referral decisions: results from the ASPN referral study. J Fam Pract. 2002;51:215–222. [PubMed] [Google Scholar]
- 21.Wallace P, Haines A, Harrison R, et al. Joint teleconsultations (virtual outreach) versus standard outpatient appointments for patients referred by their general practitioner for a specialist opinion: a randomised trial. Lancet. 2002;359:1961–1968. [DOI] [PubMed] [Google Scholar]
- 22.Leggett P, Gilliland AE, Cupples ME, et al. A randomized controlled trial using instant photography to diagnose and manage dermatology referrals. Fam Pract. 2004;21:54–56. [DOI] [PubMed] [Google Scholar]
- 23.Burton LC, Anderson GF, Kues IW. Using electronic health records to help coordinate care. Milbank Q. 2004;82:457–481, table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. New York, NY: Oxford University Press; 1998.