Abstract
PURPOSE We investigated the prevalence, severity, and course of passive and active suicidal ideation occurring in primary care patients with an uncomplicated depressive disorder.
METHODS We studied suicidal ideation experienced by patients recruited in 60 primary care practices participating in a randomized controlled trial of depression management. Risk levels associated with suicidal ideation and plans were determined by a 2-stage procedure using pertinent items of the Patient Health Questionnaire-9, the Hopkins Symptom Checklist-20, and the Cornell structured assessment interview and management algorithm.
RESULTS Of the 761 patients whom physicians judged in need of treatment for a clinical depression, 405 (53%) were experiencing uncomplicated dysthymia, major depression, or both. Among these depressed patients, about 90% had no risk or a low risk of self-harm based on the presence and nature of suicidal ideation; the rest had an intermediate risk. Almost all patients who were initially classified at the no or low risk levels remained at these levels during the subsequent 6 months. The incidence of suicidal ideation at a risk level requiring the physician’s immediate attention in this no- or low-risk subgroup was 1.1% at 3 months and 2.6% at 6 months.
CONCLUSIONS Almost all patients with uncomplicated dysthymia, major depression, or both acknowledging suicidal ideation of the minimal risk type when initially assessed maintained this minimal risk status during the subsequent 6 months.
Keywords: Depression, suicide, suicidality, suicidal ideation, suicidal risk, risk factors, clinical course
INTRODUCTION
The identifycation and prevention of suicidality in primary care is of concern at the national policy-making and clinical practice levels. Policy reports of the US Surgeon General1 and Institute of Medicine2 assign primary care physicians a key role in assessing and treating patients at risk for self-harming behaviors. Because on average 45% of persons killing themselves contact their physicians in the month preceding the life-ending act,3 physicians are thought to be potentially capable of preventing this outcome. Primary care physicians, themselves, acknowledge responsibility for suicide prevention and participate in educational programs to improve case finding and treatment skills.4 Physicians initially should focus on patients experiencing depression because this disorder is a major risk factor for self-harm.
As 1% to 10% of primary care patients experience life-ending thoughts and intentions,5 suicide risk assessment and management of suicidality are intrinsic to primary care practice. Effective approaches to these clinical tasks are hampered, however, by knowledge gaps6 concerning the severity of suicidal ideation and behaviors and how to assess them in primary care. More precise knowledge about the prevalence of suicidal ideation and the various risk levels for self-harm is needed to manage patients at serious risk of hurting themselves, including the extent to which they burden primary care practices and specialized psychiatric services. In generating risk-stratified suicide rates, valid and efficient assessment strategies should be used. The available approaches7–10 have been perfected in research protocols and mental health settings, but their validity and applicability to primary care practice are unclear.
In a study of depression management in primary care, we investigated rates of suicidal ideation and risk levels (ranging from none to high) generated by a 2-stage assessment procedure, and the course of suicidal ideation and behaviors from baseline through 3- and 6-month follow-ups.
METHODS
We assessed suicidal ideation rates in depressed primary care patients as part of a randomized controlled trial of enhanced depression management.11,12 The randomized trial’s protocol was approved by the Committee for Human Subjects Protection at the participating health care and research organizations.
Sample and Measures
We conducted this study in 3 medical groups and 2 health insurance plans serving patients in 60 geographically diverse primary care practices.12 The participating practices were staffed by 1 to 9 clinicians who offered their clinically depressed patients study enrollment. Those providing written informed consent were referred to Cornell’s research center, whose interviewers administered computer-assisted telephone interviews to participants.
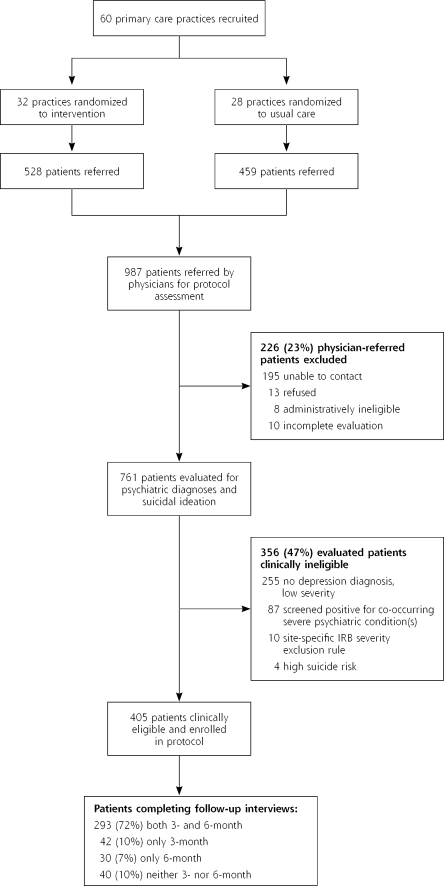
Intervention and usual care practice clinicians referred 987 patients, of whom 226 were excluded for reasons presented in Figure 1 ▶. A total of 761 patients (77% of those referred) were administered a 5- to 10-minute interview that included the Patient Health Questionnaire-9 (PHQ-9)13 to determine whether the patient was experiencing a major depressive disorder or dysthymia as well as his/her degree of suicidal ideation; modified Structured Clinical Interview for Axis I DSM-IV Disorders (SCID)14 scales to identify patients screening positive for bipolar disorder, posttraumatic stress disorder (PTSD), substance abuse, and schizophrenia, diagnoses that excluded patients from the study; and the Cut-down, Annoyed, Guilt, Eye-opener (CAGE) questionnaire15 to identify alcohol abuse, another diagnosis that excluded patients.
Figure 1.
Flow chart of participation in the trial.
IRB = institutional review board.
Figure 1 ▶ indicates that 356 of the 761 screened patients were ineligible for the study for various reasons. Most of these ineligible patients lacked a depression diagnosis, had depression of minimal severity (a score >0.49 on the 20 depression items of the Hopkins Symptom Checklist-90 [HSCL-20]16), or both. Some screened positive for 1 or more of the following diagnoses co-occurring with depression: schizophrenia, bipolar disorder, PTSD, and alcohol or substance abuse. One study site excluded 10 patients because its Committee for the Protection of Human Subjects considered patients acknowledging even fleeting thoughts of self-harm or passive ideation to be at serious risk for initiating life-ending behaviors. Four patients, 1 of whom was also assigned the diagnosis of PTSD, were judged to be at high suicidal risk and were thus protocol ineligible given the specificity of their life-ending plans. Thus, 405 (53%) of 761 evaluated patients met the study’s depression diagnoses and severity criteria. They completed a 20- to 25-minute test battery including the following: the HSCL-2016 to measure depressive severity; modified Primary Care Evaluation of Mental Disorders (PRIME-MD)17 scales to identify co-occurring symptoms of generalized anxiety and panic; the World Health Organization Disability Assessment Schedule II (WHODAS)18 to measure functional abilities in performing life activities and social participation; and the 1-item self-report pain scale of the Medical Outcomes Study 36-item Short-Form Health Survey19 to determine extent of physical distress.
Protocol for Assessing Suicide Risk
The first-stage screener for determining whether the patient was experiencing suicidal ideation consisted of the PHQ-913 question inquiring about thoughts during the past 2 weeks of being “better off dead or hurting yourself in some way.” This assessment required less than 1 minute. Patients denying these ideations were judged to be at no risk for suicidality. Because the PHQ-9 item inquires about both passive and active death wishes, we then clarified whether a patient was specifically endorsing “… thoughts of harming yourself in some way?” Patients denying this active ideation were classified as low risk because they had previously acknowledged passive death wishes.
Patients endorsing active ideation were administered stage 2 of the suicidality risk assessment, consisting of a structured clinical interview and algorithm developed to assess suicide risk in depressed home care patients.20 The second-stage assessment investigates severity of the patient’s active ideation including the nature and frequency of thoughts of inflicting self-harm; attempts at self-harm in the past month or previously; specificity of current plans and capacity to implement them; strength of death wishes; intensity of hopelessness; and impulse control and the availability of preventive deterrents. Patients acknowledging active thoughts of self-harm but lacking an articulated plan for doing so were classified at the intermediate risk level; those presenting a defined self-harm plan or lacking needed impulse control were judged to be at the high risk level.
The stage-2 clinical interview requires 5 to 20 minutes, depending on the extent of a patient’s self-harm impulses and thoughts. The assessment questionnaire and the detailed algorithm used to classify suicidal risk are posted on the MacArthur Depression Initiative Web site (http://www.depression-primarycare.org).
We determined the longitudinal course of suicidal ideation and plans at both 3 and 6 months by again assessing 293 (72%) of the 405 patients experiencing uncomplicated dysthymia, major depression, or both (Figure 1 ▶). At these time points, the HSCL-20 rather than PHQ-9 suicide inquiry served as the first-stage screener. Patients endorsing thoughts of “ending” their lives during the past week were administered the same second-stage risk assessment questionnaire used during the baseline interview.
Data Analysis
Patient characteristics were described using means and standard deviations for continuous variables and percentages for categorical variables. Comparisons of patient characteristics across risk levels were performed using analysis of variance (ANOVA) for continuous variables. We examined the effect of baseline social, demographic, and clinical characteristics on missing follow-up suicidal ideation data by comparing completers with patients who missed any follow-up appointment. These comparisons were performed with t tests and χ2 tests for continuous and categorical baseline characteristics, respectively. We used SAS software (SAS Institute, Inc, Cary, NC) for all statistical analyses.
RESULTS
We compared the 528 intervention and the 459 usual care patients referred by physicians with the randomized clinical trial population and found no differences in the groups’ rates of protocol eligibility and recruitment; in their baseline social, demographic, and clinical characteristics; or in their rate of participation in the follow-up assessments. The 2 treatment groups are combined, therefore, in the following analyses of the prevalence and course of suicidal ideation in the subgroup of 405 primary care patients with uncomplicated dysthymia, major depression, or both (Figure 1 ▶).
This cohort consisted of middle-aged patients, the majority of whom were female, white, employed, earning an income exceeding the poverty level, married, and living with others (Table 1 ▶). Depressive symptoms of the 405 protocol-eligible patients as measured by the HSCL-2016 were moderate to severe; primary care physicians already had prescribed an antidepressant medication for 90% of them. A substantial minority of patients screened positive for symptoms of generalized anxiety, panic, or both. On the WHODAS18 subscales, patients acknowledged only mild limitations in self-care but moderate to severe limitations in performing life activities and societal participation.
Table 1.
Baseline Characteristics of Patients With Major Depression, Dysthymia, or Both, Stratified by Risk Level of Suicidal Ideation
| Risk Level* | |||||
| Characteristic | Total (N = 405) | None (n = 259) | Low (n = 105) | Intermediate (n = 41) | P Value |
| Social and demographic | |||||
| Female, % | 80.25 | 82.63 | 78.10 | 70.73 | .168 |
| Age, mean (SD), y | 41.94 (14.62) | 42.50 (14.25) | 43.57 (16.07) | 34.17 (10.35) | .001 |
| Education, mean (SD), y | 13.24 (2.32) | 13.32 (2.34) | 13.15 (2.10) | 12.98 (2.72) | .610 |
| Ethnic minority,† % | 16.87 | 18.68 | 14.29 | 12.20 | .420 |
| Married, % | 55.31 | 54.83 | 54.29 | 60.98 | .740 |
| Living with others , % | 87.65 | 86.10 | 86.67 | 100.00 | .040 |
| Income level above poverty,‡ % | 78.76 | 81.45 | 77.78 | 64.10 | .464 |
| Paid employment, % | 61.48 | 65.25 | 60.95 | 39.02 | .006 |
| Clinical§ | |||||
| HSCL-20 depression severity score, mean (SD) | 2.01 (0.65) | 1.86 (0.61) | 2.23 (0.63) | 2.39 (0.60) | .001 |
| Depressive disorder | |||||
| MDD only, % | 78.52 | 77.22 | 82.86 | 75.61 | |
| MDD and dysthymia, % | 19.26 | 19.31 | 17.14 | 24.39 | .183 |
| Dysthymia only, % | 2.22 | 3.47 | 0.00 | 0.00 | |
| Symptoms of panic, % | 20.54 | 20.08 | 19.23 | 26.83 | .566 |
| Symptoms of GAD, % | 40.94 | 42.02 | 36.19 | 46.34 | .449 |
| CAGE score, mean (SD) | 0.11 (0.39) | 0.12 (0.41) | 0.06 (0.27) | 0.17 (0.54) | .236 |
| SF-36 pain score, mean (SD) | 1.43 (1.37) | 1.26 (1.33) | 1.68 (1.33) | 1.85 (1.57) | .003 |
| WHODAS disability scores, mean (SD) | |||||
| Understand and communicate | 0.32 (0.19) | 0.30 (0.18) | 0.35 (0.20) | 0.40 (0.21) | .001 |
| Getting around | 0.24 (0.24) | 0.20 (0.21) | 0.30 (0.26) | 0.31 (0.26) | .001 |
| Self-care | 0.16 (0.17) | 0.14 (0.16) | 0.18 (0.18) | 0.26 (0.19) | .001 |
| Getting along with people | 0.30 (0.23) | 0.26 (0.21) | 0.36 (0.24) | 0.38 (0.24) | .001 |
| Life activities | 0.41 (0.24) | 0.37 (0.23) | 0.47 (0.25) | 0.47 (0.25) | <.001 |
| Societal participation | 0.41 (0.18) | 0.37 (0.17) | 0.46 (0.19) | 0.52 (0.18) | .001 |
HSCL-20 = 20 depression items from the Hopkins Symptom Checklist-90; MDD = major depressive disorder; GAD = generalized anxiety disorder; CAGE = Cut-down, Annoyed, Guilt, Eye-opener; SF-36 = Medical Outcomes Study 36-item Short-Form Health Survey; WHODAS = World Health Organization Disability Assessment Schedule II.
* None comprised 64% of total; low, 26% of total; and intermediate, 10% of total.
† Race or ethnicity other than non-Hispanic white.
‡ Poverty status was defined according to guidelines of the US Department of Health and Human Services, based on total annual household income (see The 2001 HHS Poverty Guidelines at http://aspe.hhs.gov/poverty/01poverty.htm).
§ HSCL-20 score range was 0 to 4; CAGE score range was 0 to 4; WHODAS scores were standardized to range from 0 (no impairment in last 30 days) to 1.0 (complete inability to perform throughout full 30 days).
The relationship of patient characteristics with suicidal ideation and risk level is presented in Table 1 ▶. Demographically, patients reporting ideation of the intermediate risk level compared with those reporting ideation of the no or low risk levels were significantly younger, more frequently lived with others, and were less likely to have paid employment. Clinically, the former group was significantly more depressed, experienced more pain, and was more functionally disabled than the groups with no- or low-risk suicidal ideation.
Clinical Course of Suicidal Ideation and Risk Status
Suicidal ideation and risk levels were assessed 3 and 6 months after baseline. The 293 patients who did and the 112 who did not participate in both follow-ups differed significantly only with regard to age and living arrangements. Those with complete follow-up were older (43.7 vs 37.3 years of age) and were less likely to live with others (85.7% vs 92.9%). Participants and nonparticipants did not differ, however, on other factors that could potentially bias outcome patterns, such as baseline suicidal ideation risk levels and depression severity.
The HSCL-20 item inquiring about life-ending thoughts was administered as the screener at these time points. Because this item does not precisely distinguish ideation of the no and low suicide risk types, these 2 types are combined in the following analyses. At 3 months, the great majority of followed-up patients remained clinically stable or had a reduction of their suicide risk status (Table 2 ▶). Only 3 (1.1%) of the 268 patients initially judged as having no or only a low risk level reported suicidal thoughts that elevated them to the intermediate risk status when again interviewed. Conversely, 19 (76%) of the 25 patients initially classified at this intermediate risk level given their baseline ideation about self-harm were clinically improved and considered to have no or only low suicidal ideation 3 months later.
Table 2.
Longitudinal Course of Suicidal Ideation and Risk Status in Patients Completing 3- and 6-Month Assessments
| At 3 Months | At 6 Months | ||||
| Risk Level at Baseline | No. of Patients | None or Low No. (%) | Intermediate No. (%) | None or Low No. (%) | Intermediate No. (%) |
| None or low | 268 | 265 (98.9) | 3 (1.1) | 261 (97.4) | 7 (2.6) |
| Intermediate | 25 | 19 (76.0) | 6 (24.0) | 20 (80.0) | 5 (20.0) |
| Total | 293 | 284 (96.9) | 9 (3.1) | 281 (95.9) | 12 (4.1) |
Continuing clinical improvement was again evident at the 6-month follow-up. At this time point, only 12 (4.1%) of 293 patients displayed suicidal thoughts or behavior warranting the intermediate risk classification, compared with the 25 (8.5%) patients so classified at baseline. None of the patients interviewed at 3 and 6 months reported ideation placing them at high risk of harming themselves.
During the 6-month observation period, no patient committed suicide, and 1 attempted to take her life by ingesting unknown doses of hydrocodone bitartrate and clonazepam. The baseline suicide assessment had classified this 41-year-old woman at the intermediate risk level given her self-harm ideation, and her primary care physician already was treating her with paroxetine. After the overdose, the patient’s primary care physician changed her pharmacotherapy to venlafaxine and referred her to a psychologist for psychotherapy as well.
DISCUSSION
Our study addresses information gaps identified by the US Preventive Services Task Force regarding procedures for determining suicidal risk in depressed primary care patients.6 We used a 2-stage assessment strategy consisting of a rapid screen and a structured interview to establish the patient’s risk level of suicidal thoughts or plans. Of the 405 patients experiencing uncomplicated dysthymia, major depression, or both, 64% endorsed no suicidal ideation, 26% acknowledged passive death wishes, and only 10% reported active suicidal ideation (Table 1 ▶).
The rate of suicidal ideation and the risk levels we observed among patients with uncomplicated depression require replication in other primary care populations. Future studies should include patients who have both depression and other psychopathology to determine whether our findings are generalizable to depressed patients experiencing comorbid disorders that increase their risk for self-harm.2 Also of interest is whether suicidal ideation and risk rates differ among depressed patients treated pharmacologically and nonpharmacologically, given the US Food and Drug Administration’s Public Health Advisory21 regarding a possible relationship between the use of antidepressants and suicidality.
We consider a 2-stage assessment strategy useful for judging suicidality in depressed primary care patients. The first stage (item 9 of the PHQ) screens for any thoughts of death or self-harm and can be administered in less than 1 minute. The need for this screen is supported by findings that in only a minority of encounters do medical patients explicitly inform their physicians about thoughts and plans for self-harm.22–24 Indirect techniques for recognizing potential suicidality, for example, the patient’s office visit pattern, are not reliable.25,26
Six-month follow-up of patients experiencing uncomplicated dysthymia, major depression, or both showed decreasing suicidal ideation and risk levels. Almost all patients initially classified at the no or low risk levels continued at these levels (Table 2 ▶). Among patients whose ideation initially placed them at the intermediate risk level, only 24% and 20% maintained this risk level at 3 and 6 months, respectively. To the best of our knowledge based on regular interactions with the study sites, only a single suicide attempt and no completed suicides occurred during the 6-month follow-up period among patients who did and did not complete the research assessments. This finding is consistent with earlier reports that completed suicide is quite rare among primary care patients.27,28
Study limitations include the protocol’s exclusion of patients experiencing comorbid psychiatric disorders, such as alcohol abuse, PTSD, bipolar disorder, and psychosis, which potentially can increase a depressed person’s risk for self-harm.2 Our findings may therefore not be generalizable to these depressed primary care patients who are candidates for referral to mental health specialists. Second, we assessed suicidality at 3 and 6 months by administering the HSCL-20 inquiry about thoughts of “ending your life” rather than the baseline PHQ inquiry about thoughts of “being better off dead or hurting yourself.” Only patients acknowledging the potentially less sensitive HSCL screener at follow-up were administered the more comprehensive interview to determine whether their ideation at 3 and 6 months met criteria for intermediate risk of self-harm. Some patients at intermediate risk thus may not have been found at follow-up. Finally, it is unclear whether suicidal ideation patterns of patients consenting to the protocol’s requirements also pertain to a primary care sample followed naturalistically.
Conflicts of interest: none reported
Funding support: This research was supported by the John D. and Catherine T. MacArthur Foundation, Chicago, Ill.
REFERENCES
- 1.The Surgeon General’s Call To Action To Prevent Suicide. Rockville, Md: US Department of Health and Human Services; 1999.
- 2.Goldsmith S, Pellman T, Kleinman A, Bunney W, eds. Reducing Suicide: A National Imperative. Washington, DC: National Academies Press; 2002. [PubMed]
- 3.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Milton J, Ferguson B, Mills T. Risk assessment and suicide prevention in primary care. Crisis. 1999;20:171–177. [DOI] [PubMed] [Google Scholar]
- 5.Schulberg HC, Bruce ML, Lee PW, Williams JW Jr, Dietrich AJ. Preventing suicide in primary care patients: the primary care physician’s role. Gen Hosp Psychiatry. 2004;26:337–345. [DOI] [PubMed] [Google Scholar]
- 6.Gaynes BN, West SL, Ford CA, et al. Screening for suicide risk in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140:822–835. [DOI] [PubMed] [Google Scholar]
- 7.Stoppe G, Sandholzer H, Huppertz C, Duwe H, Staedt J. Family physicians and the risk of suicide in the depressed elderly. J Affect Disord. 1999;54:193–198. [DOI] [PubMed] [Google Scholar]
- 8.Adamek ME, Kaplan MS. Caring for depressed and suicidal older patients: a survey of physicians and nurse practitioners. Int J Psychiatry Med. 2000;30:111–125. [DOI] [PubMed] [Google Scholar]
- 9.Olfson M, Weissman MM, Leon AC, Sheehan DV, Farber L. Suicidal ideation in primary care. J Gen Intern Med. 1996;11:447–453. [DOI] [PubMed] [Google Scholar]
- 10.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–352. [DOI] [PubMed] [Google Scholar]
- 11.Dietrich AJ, Oxman TE, Williams JW Jr, et al. Going to scale: re-engineering systems for primary care treatment of depression. Ann Fam Med. 2004;2:301–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dietrich AJ, Oxman TE, Williams JW Jr, et al. Re-engineering systems for the treatment of depression in primary care: cluster randomised controlled trial. BMJ. 2004;329:602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spitzer RL, Gibbon M, Williams JB, eds. Structured Clinical Interview for Axis I DSM-IV Disorders (SCID). Washington, DC: American Psychiatric Association Press; 1995.
- 15.Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121–1123. [DOI] [PubMed] [Google Scholar]
- 16.Lipman RS, Covi L, Shapiro AK. The Hopkins Symptom Checklist (HSCL)—factors derived from the HSCL-90. J Affect Disord. 1979;1:9–24. [DOI] [PubMed] [Google Scholar]
- 17.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 18.Chwastiak LA, Von Korff M. Disability in depression and back pain: evaluation of the World Health Organization Disability Assessment Schedule (WHO DAS II) in a primary care setting. J Clin Epidemiol. 2003;56:507–514. [DOI] [PubMed] [Google Scholar]
- 19.Ware JE Jr, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 20.Bruce ML, McAvay GJ, Raue PJ, et al. Major depression in elderly home health care patients. Am J Psychiatry. 2002;159:1367–1374. [DOI] [PubMed] [Google Scholar]
- 21.Public Health Advisory. Worsening depression and suicidality in patients being treated with antidepressant medications. Washington, DC: US Food and Drug Administration; March 22, 2004.
- 22.Stenager EN, Jensen K. Attempted suicide and contact with the primary health authorities. Acta Psychiatr Scand. 1994;90:109–113. [DOI] [PubMed] [Google Scholar]
- 23.Coombs DW, Miller HL, Alarcon R, et al. Presuicide attempt communications between parasuicides and consulted caregivers. Suicide Life Threat Behav. 1992;22:289–302. [PubMed] [Google Scholar]
- 24.Isometsa ET, Aro HM, Henriksson MM, Heikkinen ME, Lonnqvist JK. Suicide in major depression in different treatment settings. J Clin Psychiatry. 1994;55:523–527. [PubMed] [Google Scholar]
- 25.Bartels SJ, Coakley E, Oxman TE, et al. Suicidal and death ideation in older primary care patients with depression, anxiety, and at-risk alcohol use. Am J Geriatr Psychiatry. 2002;10:417–427. [PubMed] [Google Scholar]
- 26.Vassilas CA, Morgan HG. General practitioners’ contact with victims of suicide. BMJ. 1993;307:300–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Diekstra RF, van Egmond M. Suicide and attempted suicide in general practice, 1979–1986. Acta Psychiatr Scand. 1989;79:268–275. [DOI] [PubMed] [Google Scholar]
- 28.Simon GE, VonKorff M. Suicide mortality among patients treated for depression in an insured population. Am J Epidemiol. 1998;147:155–160. [DOI] [PubMed] [Google Scholar]