Abstract
PURPOSE The purpose of this analysis and commentary was to explore the rationale for an integrated approach, within and outside the office, to help patients pursue healthy behaviors.
METHODS We examined the role of integration, building on (1) patterns observed in a limited qualitative evaluation of 17 Prescription for Health projects, (2) several national policy initiatives, and (3) selected research literature on behavior change.
RESULTS The interventions evaluated in Prescription for Health not only identified unhealthy behaviors and advised change, but also enabled patients to access information at home, use self-help methods, obtain intensive counseling, and receive follow-up. Few practices can replicate such a model with the limited staff and resources available in their offices. Comprehensive assistance can be offered to patients, however, by integrating what is feasible in the office with additional services available through the community and information media.
CONCLUSIONS Blending diverse clinical and community services into a cohesive system requires an infrastructure that fosters integration. Such a system provides the comprehensive model on which the quality of both health promotion and chronic illness care depend. Integrating clinical and community services is only the first step toward the ideal of a citizen-centered approach, in which diverse sectors within the community—health care among them—work together to help citizens sustain healthy behaviors. The integration required to fulfill this ideal faces logistical challenges but may be the best way for a fragmented health care system to fully serve its patients.
Keywords: Integration, coordination, primary care, health promotion, health behavior, chronic disease, self-management, community services
INTRODUCTION
Addressing health behaviors in primary care involves a familiar sequence of steps: (1) identifying the behavior(s) in question, (2) giving brief advice, (3) setting goals, (4) arranging for more intensive assistance, and (5) ensuring follow-up.1 This sequence of tasks is embodied in a variety of models for behavioral counseling, notably the 5 A’s—assess (ask about the behavior status and the factors affecting change), advise (give a clear, personal message of encouragement to change), agree (set goals based on readiness to change), assist (use behavior change techniques, such as self-help, counseling, or both, to promote acquisition of the skills, confidence, and environmental supports for change, supplemented by medical treatments when appropriate), and arrange (schedule follow-up contacts, including referral for more intensive treatment).2
The effectiveness of clinicians in promoting healthy behaviors and the quality of their service to patients are probably maximized when practices have systems in place to support this entire counseling sequence—all of the 5 A’s—rather than simply components of the process.3 Systematic reviews and clinical experience have shown that practices that use multifaceted interventions are more effective in promoting healthy behaviors than those that institute isolated measures.1,4–6
How might such a comprehensive system look in conventional primary care practices? In a perfect world, it would include a redesigned system of office practice that would enable clinicians to offer the full range of services, aided by trained counselors and information technology and adequately reimbursed by payers. Such an idealized office design, as envisioned by the Future of Family Medicine project,7 would be part of an overall restructuring of the health care system that experts now consider vital.8 Until that restructuring occurs, however, strategies to promote health behavior change must be pragmatic. The model must be realistic and compatible with the competing demands of today’s practice environment, minimizing intrusion on the productivity of clinicians and their limited time.
We sought insight into this issue by performing a limited qualitative evaluation of the interventions tested in the first round of the Robert Wood Johnson Foundation’s Prescription for Health program. As described in more detail by Cifuentes et al9 and others in this supplement, this program provided funding to 17 primary care practice-based research networks to test interventions for unhealthy behaviors (smoking, unhealthy diet, physical inactivity, and risky alcohol use) among patients in their practices. In this commentary, we use our analysis of these projects as a point of departure for examining larger lessons about the role of integrated services, both in primary care and in the community at large, in promoting healthy behaviors.
METHODS
We reviewed original proposals and interim reports from each of the 17 Prescription for Health grantees, and classified each intervention within the 5 A’s framework (Table 1 ▶). Each grantee verified that our list included all interventions evaluated in their project, and approved the 5 A’s classification assigned to each intervention. We also examined themes shared by the investigators at grantee meetings convened by the foundation and themes identified in evaluations sponsored by the foundation.4 Finally, using a focused literature review, we examined the concordance between these themes and the attributes of integration that figure prominently in research and national policy initiatives.
Table 1.
Interventions Evaluated in Prescription for Health Projects, by Counseling Step
| 4. More Intensive Assistance (Assist) | |||||||
| PBRN | 1. Identify Behaviors and Health Conditions (Assess) | 2. Brief Advice/Training (Advise) | 3. Goal Setting (Agree) | Information | Counseling | Self-Management | 5. Reinforcement, Follow-up (Arrange) |
| ACORN | Web-based behavior survey | Brief Web-based counseling message | Web database of community and behavior change resources | ||||
| APBRN | PDA screening; assess BMI | PDA-guided advice to change behavior | PDA-guided goal setting; action plans | Personalized handouts | Health change facilitator | Telephone follow-up by practice extender | |
| CECH | PDA screening | Action plans | Stage-based counseling | E-mail follow-up by health advisor based on action plan | |||
| CRN | Health behavior survey | Menu for lifestyle change | Action plans | Telephone call 1 wk and 6 mo later | |||
| COOP | Vital sign questions from medical assistants; Web-and paper-based health assessment | Brief advice | Web site information tailored to patient responses | Individual counseling, group visits, and referral to community services | Self-management supported by automatic feedback to patient, feedback to clinician, and Web-based problem-solving module | Telephone/e-mail follow-up by RNs; follow-up visits as indicated by responses to vital sign process or feedback from Web health assessment | |
| GRIN* | Patient questionnaires; nurse screening; BMI and smoking status as vital signs; 5 A’s chart stickers; healthy weight wall chart | Brief advice by physician; brief patient training by clinicians; exercise prescription | Action plans | Stage-tailored and need-specific educational materials, lists of local resources | Referral to community services | Quit kits; community services | Telephone follow-up by nurses or community service |
| HPRN, CaReNet | Intake survey | List of recommended behaviors | Goals documented on prescription pads | Feedback logs | |||
| KAN | “Willingness to change” survey; physician query | Physician prescription/referral | Mailed educational materials | Scheduled longitudinal telephone counseling | Faxed feedback to referring physician | ||
| MAFPRN | Standardized screening for tobacco use, physical activity, diet, risky drinking | Brief motivational enhancement by health coach | Print or online motivational information | Telephone or Web-based motivational counseling | Self-help guidebook; Web site; community resources and programs | Telephone and e-mail follow-up by clinics; follow-up visits | |
| MNCCRN | Assess diet, physical activity, and BMI | Participation in wellness club recommended by advanced practice nurse | Weekly written goals | Written lesson plans for didactic sessions | Support group; nutritionist-led didactic sessions; motivational videos | Food diaries; pedometer counts | Telephone follow-up by educator; health buddies; community activities (see Table 2 ▶) |
| NECF | Screening for tobacco use and risky screening | Brief motivational interviewing by physician, nurse, physician assistant, medical assistant, or health educator | Literature | Follow-up visit | |||
| NOPCRN | Assess BMI, nutrition, and physical activity | PDA-guided goal recommendation | PDA-guided goal setting | Pedometer; activity log | Telephone follow-up by nurse-coordinator; biweekly nurse practice visits for weight and BP checks, pedometer downloads, and activity log assessment | ||
| PitNet | Assess BMI; parent perception survey | Brief motivational interviewing | Handouts and homework | Health educator group sessions | Self-monitoring books | Telephone follow-up | |
| PPRG | Wall chart; nutrition assessment | Brief advice based on nutritional status and menu for lifestyle change | Age- and nutritional status–specific handouts on health behaviors | ||||
| PSARN | Assess BMI | Educational bulletin board; educational materials | Health change facilitator; decision balance exercise; other motivational techniques | Self-help guidebook | Health change facilitator follow-up in person, by telephone, by e-mail | ||
| RAP | Prescription | Web database of community and behavior change resources | |||||
| VaPSRN | Smoking, BMI, vital signs | PDA tool to guide counseling | Patient resources suggested by PDA software | ||||
Note: The contents of this table were reviewed and edited by investigators from each of the 17 Prescription for Health projects.
*Interventions at GRIN practices varied and were determined and implemented individually by practices.
5 A’s = assess, advise, agree, assist, arrange; ACORN = Virginia Ambulatory Care Outcomes Research Network; APBRN = Alabama Practice Based Research Network; BMI = body mass index; BP = blood pressure; CaReNet = Colorado Research Network; CECH = Center to Enhance Child Health Network; CRN = University of California at San Francisco (UCSF)/Stanford Collaborative Research Network; COOP = Dartmouth-Northern New England COOP Project; GRIN = Great Lakes Research Into Practice Network; HPRN = High Plains Research Network; KAN = Kentucky Ambulatory Network; MAFPRN = Minnesota Academy of Family Physicians Research Network; MNCCRN = Midwest Nursing Centers Consortium Research Network; NECF = New England Clinicians Forum Practice-Based Research Network; NOPCRN = Northwest Ohio Primary Care Research Network; PBRN = practice-based research network; PDA = personal digital assistant; PitNet = Pediatric PitNet; PPRG = Pediatric Practice Research Group; PSARN = Pennsylvania State Ambulatory Research Network; RAP = Research Association of Practices; RN = registered nurse; VaPSRN = Virginia Practice Support and Research Network.
RESULTS
Insights From Prescription for Health: Integration of Services to Achieve Comprehensive Care
Our review of the Prescription for Health projects found that pragmatic features were common among the interventions tested, an outcome reflective of the program’s design. The original call for proposals from the foundation specified that applicants test interventions that could be “easily adopted” and complete their projects within 16 months; project grants could not exceed $125,000. These constraints precluded the testing of complex or protracted interventions, and fostered innovation among grantees to fashion interventions that ordinary practices could implement.
Few Prescription for Health projects were able to evaluate a comprehensive system for promoting behavior change. The interventions instead addressed selected components of the 5 stages of counseling (Table 1 ▶). Some interventions screened for unhealthy behavior, some changed the way advice was given, some focused on goal setting, and some provided more intensive assistance. In only 4 projects did the interventions address all of the 5 A’s.
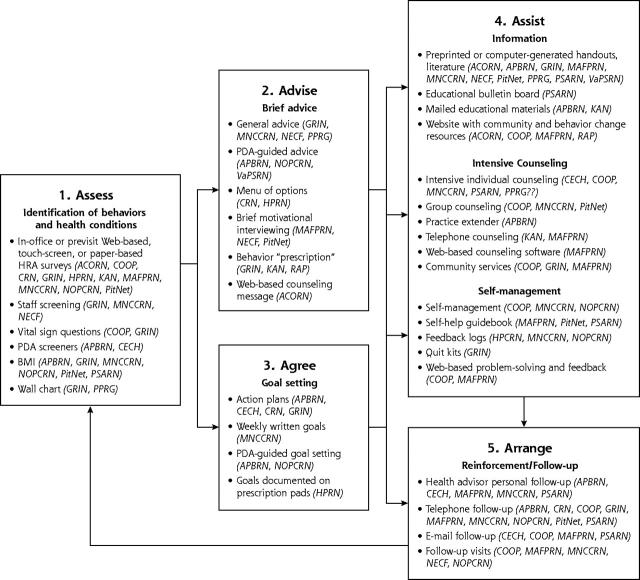
Although no Prescription for Health project was totally comprehensive, when the projects’ interventions are examined as a whole, the design of a complete system to fully support behavior change takes form. A synthesis of the projects (Figure 1 ▶) presents a vision for an integrated, multifaceted system with realistic potential for implementation in primary care settings. Practices that wish to support each of the 5 A’s can choose from the menu of options in the figure, tested by the grantees, to (1) identify unhealthy behaviors (eg, by health risk appraisals), (2) offer brief advice, (3) set collaborative goals and action plans (eg, behavior “prescriptions”), (4) provide more extensive information (eg, handouts, interactive Web sites), counseling (eg, in-office coaches or community health advisors, telephone counseling, group didactic sessions, and support groups, some using motivational interviewing), and self-help tools (eg, guidebooks, pedometers, activity logs, food diaries), and (5) arrange follow-up and reinforcement (eg, health buddies, e-mail or telephone follow-up).
Figure 1.
Integrated model of interventions evaluated by Prescription for Health projects.
Other strategies not tested under Prescription for Health offer additional options for supporting behavior change. Examples include computer-generated physician and patient reminders and e-mails, chart reminder stickers and flow sheets, examination and waiting room posters, teamwork interventions, patient-held health diaries, and interactive technologies (eg, Web-based resources, clinic-based CD-ROMs, interactive voice-response telephone calls).10,11
Integration Between the Practice and the Community: Reaching Out Beyond the Clinic
Intensive counseling can enhance behavior change but is often beyond the capacity of ordinary primary care practices, which lack the time and resources for such follow-up. As Cohen et al4 describe in this supplement, Prescription for Health grantees discovered that delivering high-quality counseling often taxed the capabilities of practices and their staff. Some interventions required clinicians to undergo extensive training or to depend on practice extenders and external support from research teams. The long-term sustainability of such self-contained interventions is unclear4,12; furthermore, their generalizability to practices across the country is uncertain.
Real-world practices that lack the resources to replicate intensive approaches within their offices can still ensure that patients receive high-quality counseling by reaching out beyond the office—establishing integrated linkages with information and community resources. The few minutes that clinicians and staff have with patients can then be used for what clinicians do best: identifying the behaviors and conveying to patients the importance of change.13,14 As Stange et al15 have advocated, these first steps can be leveraged into more effective interventions if they connect patients with professionals and programs—within or outside the office—that can provide more extensive follow-up. As with any consulting relationship, these resources should work in concert with primary care professionals in a team approach, reporting to and consulting with clinicians as counseling progresses, and integrating follow-up into ongoing health care.16
Certain smoking cessation models provide an example of the use and integration of resources beyond the office. In some states and health systems, clinicians can identify smokers (assess) and offer brief advice (advise) in the office and then refer patients to telephone quit line programs that can offer more intensive counseling (assist, arrange).17 The best models, as in Massachusetts’ quit line program,18 have a feedback component that enables counselors to share progress reports with the primary care clinician as part of a longitudinal team relationship. A research network in Virginia that was a grantee under Prescription for Health is now conducting a randomized trial, funded by the Agency for Healthcare Research and Quality, to test whether this integrated counseling model increases the quality of the assistance that smokers receive.19
A number of Prescription for Health projects pursued this approach, testing interventions that reached beyond the office to enable patients to access information at home (eg, through interactive Web sites), to use self-help methods (eg, guidebooks), to access intensive counseling after leaving the clinic (eg, intensive in-person or telephone sessions with trained counselors in the practice or through community health alliances),20 and to obtain follow-up and reinforcement over time (eg, health buddies, telephone or e-mail follow-up).4 Almost every project provided patients with resources that they could use at home to act on the advice they received in the office (Table 2 ▶). That so many grantees turned to this approach reflects not only the logic of leveraging, but also a recognition of the impracticality of the alternative: expecting practices to rely on their own staff and resources to deliver intensive counseling and follow-up, often with limited or no reimbursement.
Table 2.
Resources and Assistance Used in Prescription for Health Projects to Reach Out Beyond the Office
| PBRN | Resources and Assistance |
| ACORN | Patient access to Web-based information and linkage with community and practice resources |
| APBRN | Telephone contact by practice extender; personalized materials and referral to local resources |
| CECH | Copy of action plan; e-mail contact from health advisor based on action plan |
| CRN | Telephone follow-up |
| COOP | Web site interaction at home before or after visit; self-management; referral to community resources at schools, home/social services, lay volunteer programs; establish community health alliances |
| GRIN | Consultation assistance by nurse-consultants from health systems for self-selected systematic change in practice; many practices developed packets of educational materials tailored to targeted behaviors or stage of readiness, some including lists of local resources |
| HPRN, CaReNet | Goal “prescription”; feedback logs |
| KAN | Mailed educational material; telephone counseling |
| MAFPRN | Print or online motivational information, self-help guidebook; telephone or Web-based motivational counseling, referrals to community resources and programs, telephone and e-mail follow-up from clinics, follow-up visits |
| MNCCRN | Telephone reminders and follow-up; “health buddy,” food diaries, pedometers; organized visits to safe walking routes, fast food restaurants, super-markets, community exercise facilities, and food preparation classes |
| NECF | Patient education literature; referrals to community resources |
| NOPCRN | Pedometer; activity log; nurse surveillance visits; telephone follow-up |
| PitNet | Self-monitoring book; handouts; telephone follow-up |
| PPRG | Age- and nutritional status–specific handouts on health behaviors |
| PSARN | Educational materials; self-help guidebook; telephone or e-mail contact from nurse-educator; referral to community resources |
| RAP | Patient access to Web-based information and linkage with community and practice resources |
| VaPSRN | Patient resources suggested by PDA software |
Note: The contents of this table were reviewed and edited by investigators from each of the 17 Prescription for Health projects.
ACORN = Virginia Ambulatory Care Outcomes Research Network; APBRN = Alabama Practice Based Research Network; CaReNet = Colorado Research Network; CECH = Center to Enhance Child Health Network; CRN = University of California at San Francisco (UCSF)/Stanford Collaborative Research Network; COOP = Dartmouth-Northern New England COOP Project; GRIN = Great Lakes Research Into Practice Network; HPRN = High Plains Research Network; KAN = Kentucky Ambulatory Network; MAFPRN = Minnesota Academy of Family Physicians Research Network; MNCCRN = Midwest Nursing Centers Consortium Research Network; NECF = New England Clinicians Forum Practice-Based Research Network; NOPCRN = Northwest Ohio Primary Care Research Network; PBRN = practice-based research network; PDA = personal digital assistant; PitNet = Pediatric PitNet; PPRG = Pediatric Practice Research Group; PSARN = Pennsylvania State Ambulatory Research Network; RAP = Research Association of Practices; VaPSRN = Virginia Practice Support and Research Network.
Aside from its pragmatic value to practices, this outreach is potentially more useful to patients because the work of lifestyle change occurs outside the clinic. An approach to health promotion that is restricted to the clinical encounter ignores the basic principles of the socioecological model21 and compromises the effectiveness of health behavior counseling. Clinicians’ time with patients represents a tiny fraction of patients’ daily lives, and clinicians’ efforts have limited impact on patients’ health behaviors if conditions at home, at work, at school, and in the community are not supportive.4,22 Clinicians’ influence on the lifestyle is possible through integrated and stable partnerships and linkages if an infrastructure is in place for these relationships to flourish.
Parallels in Chronic Disease Management
The same philosophy of integrated and comprehensive care is embedded in current thinking about how best to manage chronic disease. Good outcomes in chronic diseases cannot be expected without providing patients with the knowledge, tools, and support to incorporate self-care into their daily lives.23 Systems of care are investing resources to expand the infrastructure required for coordination.24 More than 500 health care organizations have participated in the Breakthrough Series, sponsored by the Institute for Healthcare Improvement, to pursue comprehensive systems change to improve chronic illness care.25 They are establishing teams that streamline and integrate the work of health professionals and community services.26 They are installing reminder systems for clinicians and patients, and adapting information technologies to better link clinicians and consumers with each other and with relevant knowledge information.27,28
Similar support is needed to help patients achieve and sustain behavior change, suggesting the need to think more broadly about the aims of redesigning systems. Designing and investing in bridging systems that connect practices with implementation strategies outside the office can reap benefits simultaneously in the domains of disease prevention and chronic illness care.29 To focus on only one domain is a lost opportunity to maximize public health impact and efficiency. The distinction is also alien to primary care, which provides both disease prevention and chronic illness care, often to the same patient and sometimes in the same visit. System changes made by practices for health promotion or chronic illness care accrue to the benefit of all patients: for example, the reminder system that prompts the clinician to perform a foot examination in a diabetic patient can also prompt questions about smoking status, and the telephone counseling program that supports physical activity can, with augmentation, support self-management in patients with heart failure.
The Bigger Picture: A Citizen-Centered Approach
The integration of primary care with the community and with information resources, as occurred in Prescription for Health projects, is a first step in fulfilling a much larger need—faced by communities—to provide a web of integrated services to help citizens sustain healthy behaviors. Ideally, a person who chooses to become physically active should find a community working together to support the effort. The individual’s physician might recommend exercise, but local media and advertising can reinforce the message,30,31 employers can offer incentives,32 and the built environment (eg, neighborhood walkways) can be redesigned to foster outdoor activity.33
A diverse collaboration is required to give citizens a seamless support system for healthy diet, physical activity, smoking cessation, and moderation in alcohol consumption. It includes not only local health systems but also school boards, park authorities, workplaces, churches, bars, restaurants, theaters, sports centers, grocers and other retail outlets, volunteer organizations, senior centers, news media, advertisers, urban planners, and the leaders who set direction for these sectors.
Community-level integration of this type is beginning to emerge in many communities, often through concerted efforts such as the Steps to a Healthier US Cooperative Agreement program.34 In 2004, this US Department of Health and Human Services program issued $36 million in grants to 40 communities to develop integrated community action plans to reduce the burden of diabetes, overweight, obesity, and asthma, and to address risk factors such as physical inactivity, poor nutrition, and tobacco use.35
One Steps grantee (Seattle and King County, Wash), for example, has undertaken a comprehensive approach that involves media, policy makers, schools, workplaces, health care, and the community in a 100-member consortium that includes clinicians, hospitals, health plans, universities, community organizations, faith groups, government agencies, and school districts.36 Their work with clinicians establishes integration between patient care and the community by using chronic disease and wellness coordinators to facilitate systems change, linking patients with community resources, and using case management. Their citizen-centered approach takes integration to a much broader community level. Examples of their comprehensive efforts include promoting community and housing policies that support physical activity, discouraging sales of nonnutritious foods at schools, and working with faith communities to train lay educators in health promotion.
The Challenges of Integrating Clinical and Community Services
Integration makes sense but is hardly straightforward. Systems to help practices reach out beyond the office encounter logistical challenges, as Prescription for Health grantees discovered. Projects in Minnesota and Pennsylvania developed self-help materials but found that patients preferred telephone or face-to-face interpersonal contact. A Kentucky project found that only 500 of 15,000 patients who received postcard invitations to obtain telephone counseling called the program to arrange services. Projects in Virginia, Ohio, and Minnesota developed Web sites to facilitate behavior change but encountered technical challenges and low use rates.4 A New Hampshire project found that receiving e-mail messages was unpopular with adolescent patients. Projects using practice extenders required resources for training and efforts to maintain coordination with primary clinicians and to ensure privacy of data.4
Substantial resources are required to build an infrastructure within health care that integrates primary care practices and communities. The sources of funding to establish this infrastructure and their long-term sustainability are unclear. Tobacco quit lines, for example, have struggled as state budgets, a primary funding source, have tightened.37 For integration to be truly viable, these and other counseling resources to which clinicians might refer patients require stable funding; in addition, clinicians and health systems will expect reimbursement for the added work entailed in establishing and maintaining ties with diverse community services.38 Finally, the very definition of integration and the performance measures that evaluators would use to know when it exists require development.
CONCLUSIONS
The formidable challenges to integration must be overcome to make it a key feature of the future transformation of health care. Integration, the natural answer to the current fragmentation of health care, was highlighted by the Institute of Medicine as a national priority.39 The importance of integrating clinical and community services was evident in the Prescription for Health experience, but a similar lesson has been echoed in other quality improvement projects of the Robert Wood Johnson Foundation. Integration is a recurring theme in the foundation’s work with other agencies (eg, the Institute for Healthcare Improvement, the MacColl Institute for Healthcare Innovation) and figures prominently in programs that bridge clinical practice and the community (eg, Pursuing Perfection,40 Improving Chronic Illness Care,41 Innovative Care for Chronic Conditions42) and that build partnerships between the community and public health agencies (eg, Turning Point43).
The prominence of integration and primary care in so many of these quality improvement programs underscores their vital role in drawing together the services that patients require to address their health needs. Over time, the premier quality improvement initiatives and accompanying research, including the second round of Prescription for Health, will clarify whether integration of services improves the health and satisfaction of the population. These insights might suggest solutions to the logistical barriers to implementing integration. Morbidity, mortality, and health care costs can be substantially reduced by even modest reductions in unhealthy behaviors. If the hard work of building a comprehensive system to support healthy lifestyles can make a difference, it is a cause well worth pursuing.
Acknowledgments
We thank investigators from the 17 Prescription for Health projects for reviewing the tables and figure in this manuscript, and we appreciate comments on the body of the text provided by Thomas Bodenheimer, MD; Myra A. Crawford, PhD, MPH; Cecelia A. Gaffney, MEd; Larry A. Green, MD; Anton J. Kuzel, MD, MS; Alfred F. Tallia, MD, MPH; John H. Wasson, MD; and Diane B. Wilson, EdD, MS, RD. The comments of the anonymous reviewers were especially helpful.
Conflicts of interest: none reported
Funding support: This work was supported by Prescription for Health (grant No. 049060), a national program of The Robert Wood Johnson Foundation with support from the Agency for Healthcare Research and Quality.
REFERENCES
- 1.Goldstein MG, Whitlock EP, DePue J. Multiple behavioral risk factor interventions in primary care: summary of research evidence. Am J Prev Med. 2004;27:61–79. [DOI] [PubMed] [Google Scholar]
- 2.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 2002;22:267–284. [DOI] [PubMed] [Google Scholar]
- 3.Glasgow RE, Goldstein MG, Ockene JK, Pronk NP. Translating what we have learned into practice: principles and hypotheses for interventions addressing multiple behaviors in primary care. Am J Prev Med. 2004;27:88–101. [DOI] [PubMed] [Google Scholar]
- 4.Cohen DJ, Tallia AF, Crabtree BF, Young DM. Implementing health behavior change in primary care: lessons from Prescription for Health. Ann Fam Med. 2005;3(Suppl):S12–S19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mullen PD, Simons-Morton DG, Ramirez G, et al. A meta-analysis of trials evaluating patient education and counseling for three groups of preventive health behaviors. Patient Educ Couns. 1997;32:157–173. [DOI] [PubMed] [Google Scholar]
- 6.Solberg LI, Brekke ML, Fazio CJ, et al. Lessons from experienced guideline implementers: attend to many factors and use multiple strategies. Jt Comm J Qual Improv. 2000;26:171–188. [DOI] [PubMed] [Google Scholar]
- 7.The future of family medicine: a collaborative project of the family medicine community. Ann Fam Med. 2004;2(Suppl 1):S3–S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed]
- 9.Cifuentes M, Fernald DH, Green LA, Niebauer LJ, Crabtree BF, Hassmiller SB. Prescription for Health: changing primary care practice to foster healthy behaviors. Ann Fam Med. 2005;3(Suppl):S4–S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dickey LL, Gemson DH, Carney P. Office system interventions supporting primary care-based health behavior change counseling. Am J Prev Med. 1999;17:299–308. [DOI] [PubMed] [Google Scholar]
- 11.Glasgow RE, Bull SS, Piette JD, Steiner JF. Interactive behavior change technology: a partial solution to the competing demands of primary care. Am J Prev Med. 2004;27:80–87. [DOI] [PubMed] [Google Scholar]
- 12.Bodenheimer T, Young DM, MacGregor K, Holtrop JS. Practice-based research in primary care: facilitator of or barrier to practice improvement? Ann Fam Med. 2005;3:p-p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000;9:426–433. [DOI] [PubMed] [Google Scholar]
- 14.Wasson JH, Godfrey MM, Nelson EC, Mohr JJ, Batalden PB. Microsystems in health care: Part 4. Planning patient-centered care. Jt Comm J Qual Saf. 2003;29:227–237. [DOI] [PubMed] [Google Scholar]
- 15.Stange KC, Woolf SH, Gjeltema K. One minute for prevention: the power of leveraging to fulfill the promise of health behavior counseling. Am J Prev Med. 2002;22:320–323. [DOI] [PubMed] [Google Scholar]
- 16.Peek CJ, Sanner B, Goldstein MG. Addressing Multiple Behavioral Risk Factors in Primary Care. West Haven, Conn: Bayer Institute for Health Care Communication; 2004.
- 17.Centers for Disease Control and Prevention. Telephone Quitlines: A Resource for Development, Implementation, and Evaluation. Atlanta, Ga: Office on Smoking and Health, Centers for Disease Control and Prevention; 2004.
- 18.Quitworks Web site. Available at: http://www.quitworks.org. Accessed December 31, 2004.
- 19.CRISP abstract, grant 1R21HS014854-01. Available at: http://crisp.cit.nih.gov/crisp/CRISP_LIB.getdoc?textkey=6887120&p_grant_num=1R21HS014854-01&p_query=&ticket=12302004&p_audit_session_id=58184385&p_keywords=. Accessed December 28, 2004.
- 20.Luce P, Phillips J, Benjamin R, Wasson JH. Technology for community health alliances. J Ambul Care Manage. 2004;27:366–374. [DOI] [PubMed] [Google Scholar]
- 21.Cohen DA, Scribner RA, Farley TA. A structural model of health behavior: a pragmatic approach to explain and influence health behaviors at the population level. Prev Med. 2000;30:146–154. [DOI] [PubMed] [Google Scholar]
- 22.Chin NP, Monroe A, Fiscella K. Social determinants of (un)healthy behaviors. Educ Health (Abingdon). 2000;13:317–328. [DOI] [PubMed] [Google Scholar]
- 23.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779. [DOI] [PubMed] [Google Scholar]
- 24.Kaplan A. Curing the System: Stories of Change in Chronic Illness Care. Washington, DC: National Coalition on Health Care; 2002.
- 25.Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20:64–78. [DOI] [PubMed] [Google Scholar]
- 26.Wagner EH. The role of patient care teams in chronic disease management. BMJ. 2000;320:569–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cherry JC, Dryden K, Kobb R, Hilsen P, Nedd N. Opening a window of opportunity through technology and coordination: a multisite case study. Telemed J E Health. 2003;9:265–271. [DOI] [PubMed] [Google Scholar]
- 28.Glasgow RE, Nutting PA, King DK, et al. A practical randomized trial to improve diabetes care. J Gen Intern Med. 2004;19:1167–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Glasgow RE, Orleans CT, Wagner EH. Does the Chronic Care Model serve also as a template for improving prevention? Milbank Q. 2001;79:579–612, iv-v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finlay SJ, Faulkner G. Physical activity promotion through the mass media: inception, production, transmission and consumption. Prev Med. 2005;40:121–130. [DOI] [PubMed] [Google Scholar]
- 31.Welcome to VERB. Web site. Available at: http://www.cdc.gov/youth-campaign/index.htm. Accessed December 31, 2004.
- 32.Promoting Physical Activity in Communities: Forward-Looking Options From an Executive Roundtable. Washington, DC: Partnership for Prevention; 2002.
- 33.Jackson RJ. The impact of the built environment on health: an emerging field. Am J Public Health. 2003;93:1382–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.US Department of Health and Human Services. Steps to a HealthierUS Cooperative Agreement Program. Available at: http://www.healthierus.gov/steps/grantees/StepsCoopAgrmnt_021804.pdf. Accessed December 31, 2004.
- 35.US Department of Health and Human Services. HHS awards $35.7 million to support community programs that promote better health and prevent disease [press release]. September 28, 2004. Available at: http://www.hhs.gov/news/press/2004pres/20040928.html. Accessed December 31, 2004.
- 36.US Department of Health and Human Services. Steps to a HealthierUS: Seattle & King County. 2004. Available at: http://www.healthierus.gov/steps/grantees/Seattle.pdf. Accessed December 31, 2004.
- 37.Schroeder SA. Tobacco control in the wake of the 1998 master settlement agreement. N Engl J Med. 2004;350:293–301. [DOI] [PubMed] [Google Scholar]
- 38.Bodenheimer T, Wang MC, Rundall TG, et al. What are the facilitators and barriers in physician organizations’ use of care management processes? Jt Comm J Qual Saf. 2004;30:505–514. [DOI] [PubMed] [Google Scholar]
- 39.Adams K, Corrigan JM, eds. Priority Areas for National Action: Transforming Health Care Quality. Washington, DC: National Academies Press; 2003. [PubMed]
- 40.Pursuing Perfection: Raising the Bar for Health Care Performance. Web site. Available at: http://www.ihi.org/IHI/Programs/PursuingPerfection. Accessed December 31, 2004.
- 41.About ICIC. Available at: http://www.improvingchroniccare.org/about/index1.html. Accessed December 31, 2004.
- 42.Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the quality of health care for chronic conditions. Qual Saf Health Care. 2004;13:299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Turning Point Performance Management National Excellence Collaborative. From Silos to Systems: Using Performance Management to Improve the Public’s Health. Seattle, Wash: University of Washington; 2003.