Abstract
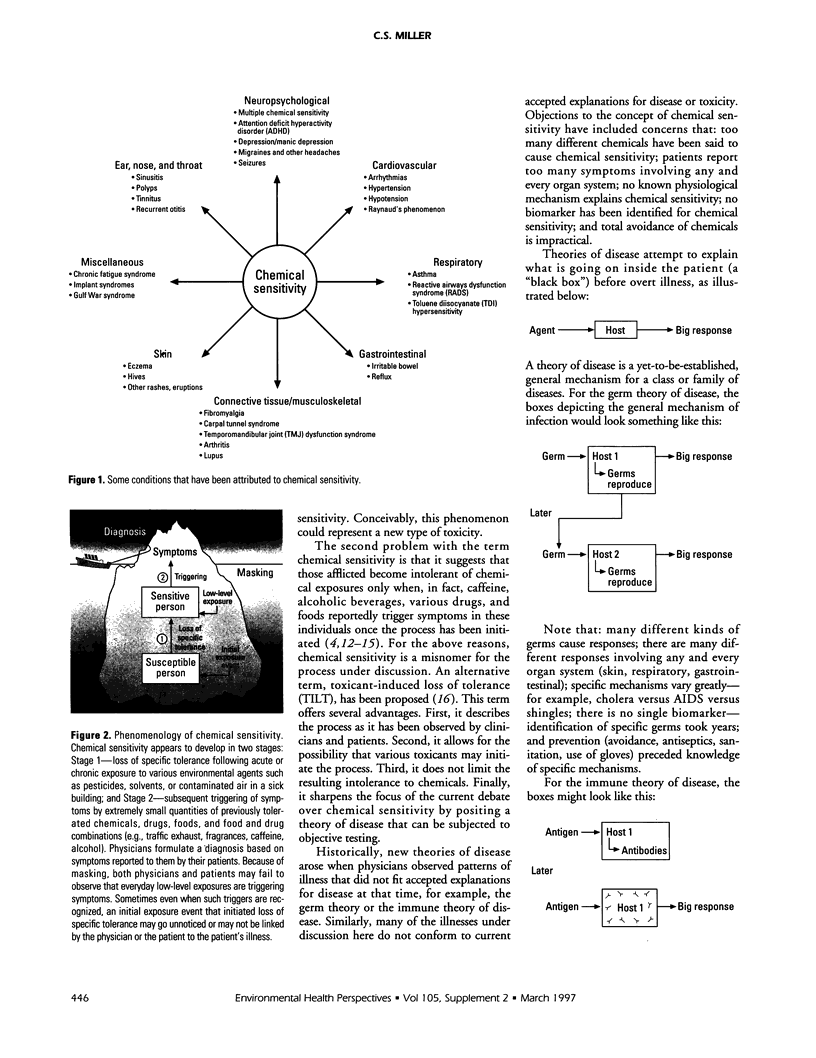
This paper attempts to clarify the nature of chemical sensitivity by proposing a theory of disease that unites the disparate clinical observations associated with the condition. Sensitivity to chemicals appears to be the consequence of a two-step process: loss of tolerance in susceptible persons following exposure to various toxicants, and subsequent triggering of symptoms by extremely small quantities of previously tolerated chemicals, drugs, foods, and food and drug combinations including caffeine and alcohol. Although chemical sensitivity may be the consequence of this process, a term that may more clearly describe the observed process is toxicant-induced loss of tolerance. Features of this yet-to-be-proven mechanism or theory of disease that affect the design of human exposure studies include the stimulatory and withdrawallike nature (resembling addiction) of symptoms reported by patients and masking. Masking, which may blunt or eliminate responses to chemical challenges, appears to have several components: apposition, which is the overlapping of the effects of closely timed exposures, acclimatization or habituation, and addiction. A number of human challenge studies in this area have concluded that there is no physiological basis for chemical sensitivity. However, these studies have failed to address the role of masking. To ensure reliable and reproducible responses to challenges, future studies in which subjects are evaluated in an environmental medical unit, a hospital-based facility in which background chemical exposures are reduced to the lowest levels practicable, may be necessary. A set of postulates is offered to determine whether there is a causal relationship between low-level chemical exposures and symptoms using an environmental medical unit.
Full text
PDF




Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bell I. R., Miller C. S., Schwartz G. E. An olfactory-limbic model of multiple chemical sensitivity syndrome: possible relationships to kindling and affective spectrum disorders. Biol Psychiatry. 1992 Aug 1;32(3):218–242. doi: 10.1016/0006-3223(92)90105-9. [DOI] [PubMed] [Google Scholar]
- Buchwald D., Garrity D. Comparison of patients with chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivities. Arch Intern Med. 1994 Sep 26;154(18):2049–2053. [PubMed] [Google Scholar]
- Carter K. C. Ignaz Semmelweis, Carl Mayrhofer, and the rise of germ theory. Med Hist. 1985 Jan;29(1):33–53. doi: 10.1017/s0025727300043738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cone J. E., Sult T. A. Acquired intolerance to solvents following pesticide/solvent exposure in a building: a new group of workers at risk for multiple chemical sensitivities? Toxicol Ind Health. 1992 Jul-Aug;8(4):29–39. [PubMed] [Google Scholar]
- Cullen M. R. The worker with multiple chemical sensitivities: an overview. Occup Med. 1987 Oct-Dec;2(4):655–661. [PubMed] [Google Scholar]
- Fiedler N., Kipen H. M., DeLuca J., Kelly-McNeil K., Natelson B. A controlled comparison of multiple chemical sensitivities and chronic fatigue syndrome. Psychosom Med. 1996 Jan-Feb;58(1):38–49. doi: 10.1097/00006842-199601000-00007. [DOI] [PubMed] [Google Scholar]
- Griffiths R. R., Woodson P. P. Caffeine physical dependence: a review of human and laboratory animal studies. Psychopharmacology (Berl) 1988;94(4):437–451. doi: 10.1007/BF00212836. [DOI] [PubMed] [Google Scholar]
- HILL A. B. THE ENVIRONMENT AND DISEASE: ASSOCIATION OR CAUSATION? Proc R Soc Med. 1965 May;58:295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackney J. D., Linn W. S., Mohler J. G., Pedersen E. E., Breisacher P., Russo A. Experimental studies on human health effects of air pollutants. II. Four-hour exposure to ozone alone and in combination with other pollutant gases. Arch Environ Health. 1975 Aug;30(8):379–384. doi: 10.1080/00039896.1975.10666729. [DOI] [PubMed] [Google Scholar]
- Miller C. S. Chemical sensitivity: symptom, syndrome or mechanism for disease? Toxicology. 1996 Jul 17;111(1-3):69–86. doi: 10.1016/0300-483x(96)03393-8. [DOI] [PubMed] [Google Scholar]
- Miller C. S., Mitzel H. C. Chemical sensitivity attributed to pesticide exposure versus remodeling. Arch Environ Health. 1995 Mar-Apr;50(2):119–129. doi: 10.1080/00039896.1995.9940889. [DOI] [PubMed] [Google Scholar]
- Miller C. S. Possible models for multiple chemical sensitivity: conceptual issues and role of the limbic system. Toxicol Ind Health. 1992 Jul-Aug;8(4):181–202. [PubMed] [Google Scholar]
- Miller C. S. Possible models for multiple chemical sensitivity: conceptual issues and role of the limbic system. Toxicol Ind Health. 1992 Jul-Aug;8(4):181–202. [PubMed] [Google Scholar]
- Miller C. S. White paper: Chemical sensitivity: history and phenomenology. Toxicol Ind Health. 1994 Jul-Oct;10(4-5):253–276. [PubMed] [Google Scholar]
- Riihimäki V., Savolainen K. Human exposure to m-xylene. Kinetics and acute effects on the central nervous system. Ann Occup Hyg. 1980;23(4):411–422. doi: 10.1093/annhyg/23.4.411. [DOI] [PubMed] [Google Scholar]
- Rosenthal N. E., Cameron C. L. Exaggerated sensitivity to an organophosphate pesticide. Am J Psychiatry. 1991 Feb;148(2):270–270. [PubMed] [Google Scholar]
- Silverman K., Evans S. M., Strain E. C., Griffiths R. R. Withdrawal syndrome after the double-blind cessation of caffeine consumption. N Engl J Med. 1992 Oct 15;327(16):1109–1114. doi: 10.1056/NEJM199210153271601. [DOI] [PubMed] [Google Scholar]
- Staudenmayer H., Selner J. C., Buhr M. P. Double-blind provocation chamber challenges in 20 patients presenting with "multiple chemical sensitivity". Regul Toxicol Pharmacol. 1993 Aug;18(1):44–53. doi: 10.1006/rtph.1993.1043. [DOI] [PubMed] [Google Scholar]
- Waddell W. J. The science of toxicology and its relevance to MCS. Regul Toxicol Pharmacol. 1993 Aug;18(1):13–22. doi: 10.1006/rtph.1993.1040. [DOI] [PubMed] [Google Scholar]
- Warner M. Hunting the yellow fever germ: the principle and practice of etiological proof in late nineteenth-century America. Bull Hist Med. 1985 Fall;59(3):361–382. [PubMed] [Google Scholar]