Abstract
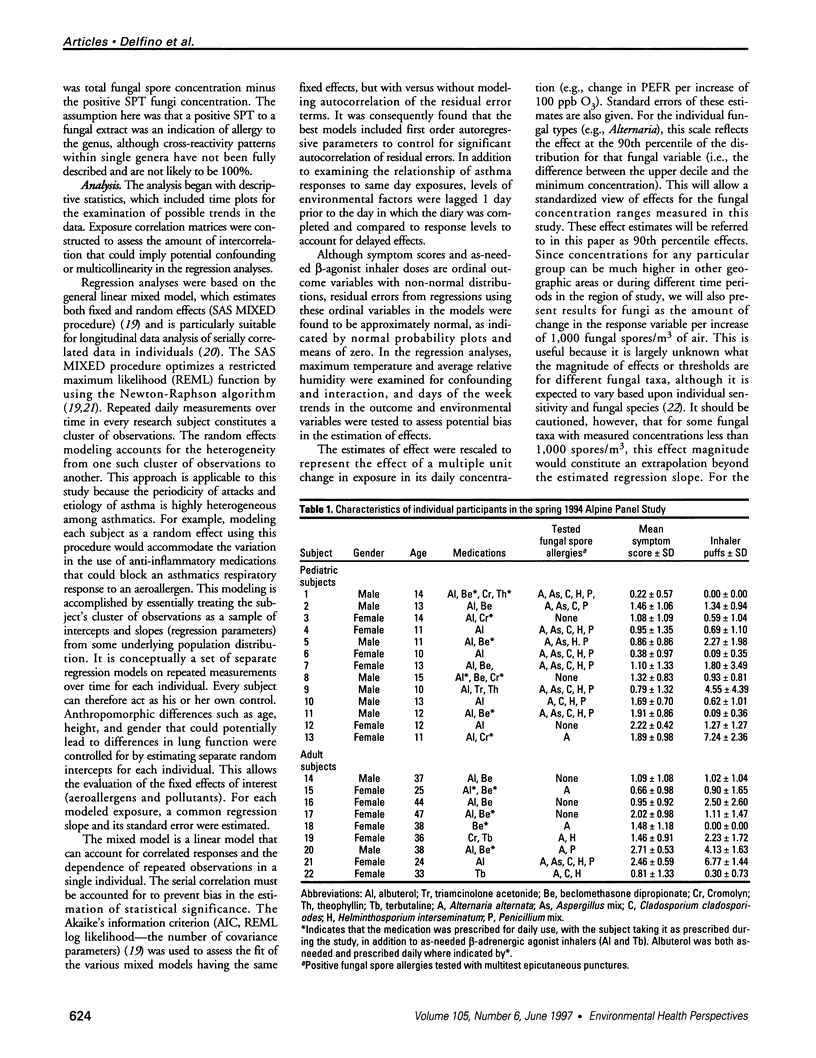
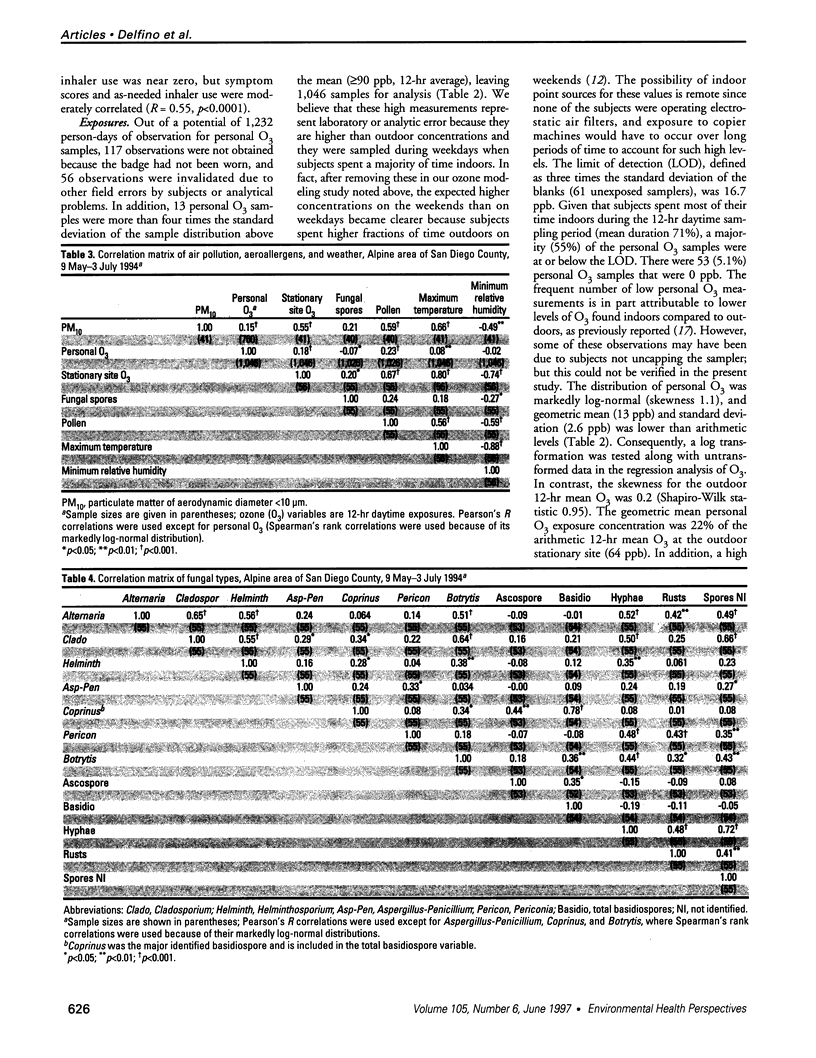
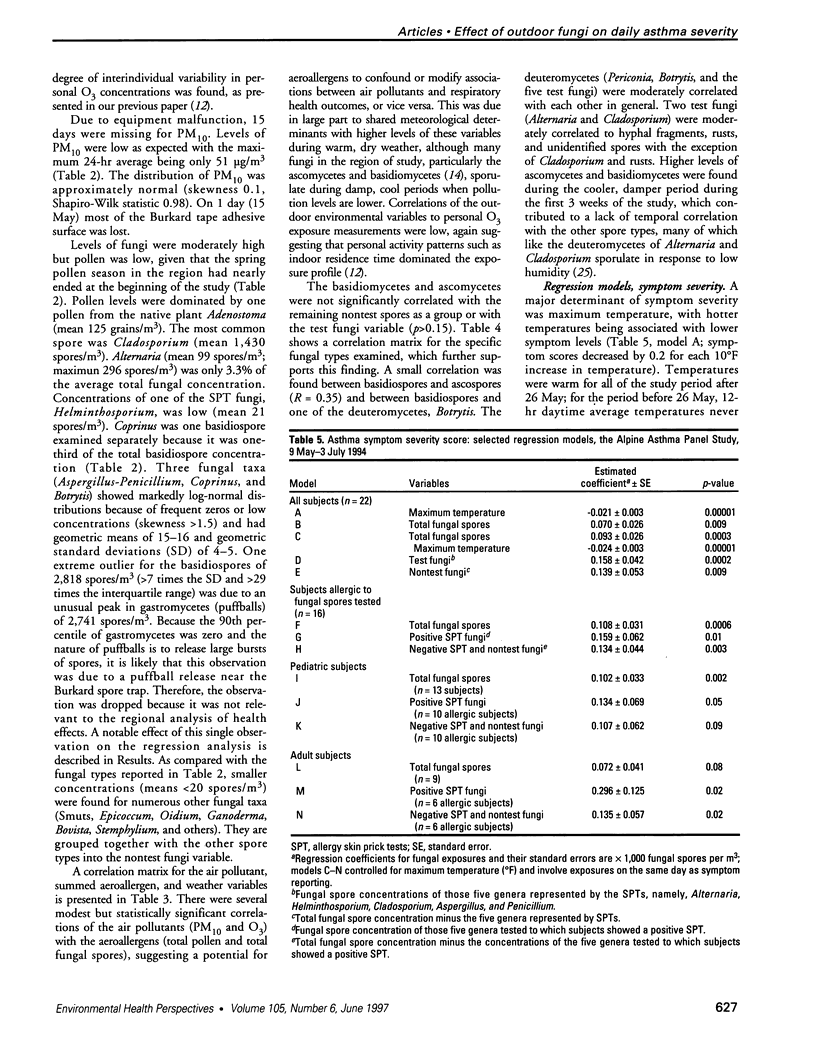
The relationship between day-to-day changes in asthma severity and combined exposures to community air pollutants and aeroallergens remains to be clearly defined. We examined the effects of outdoor air pollutants, fungi, and pollen on asthma. Twenty-two asthmatics ages 9-46 years were followed for 8 weeks (9 May-3 July 1994) in a semirural Southern California community around the air inversion base elevation (1,200 ft). Daily diary responses included asthma symptom severity (6 levels), morning and evening peak expiratory flow rates (PEFR), and as-needed beta-agonist inhaler use. Exposures included 24-hr outdoor concentrations of fungi, pollen, and particulate matter with a diameter < 10 microns (PM10; maximum = 51 micrograms/m3) and 12-hour day-time personal ozone (O3) measurements (90th percentile = 38 ppb). Random effects longitudinal regression models controlled for autocorrelation and weather. Higher temperatures were strongly protective, probably due to air conditioning use and diminished indoor allergens during hot, dry periods. Controlling for weather, total fungal spore concentrations were associated with all outcomes: per minimum to 90th percentile increase of nearly 4,000 spores/m3, asthma symptom scores increased 0.36 (95% CI, 0.16-0.56), inhaler use increased 0.33 puffs (95% CI, -0.02-0.69), and evening PEFR decreased 12.1 l/min (95% CI, -1.8-22.3). These associations were greatly enhanced by examining certain fungal types (e.g., Alternaria, basidiospores, and hyphal fragments) and stratifying on 16 asthmatics allergic to tested deuteromycete fungi. There were no significant associations to low levels of pollen or O3, but inhaler use was associated with PM10 (0.15 inhaler puffs/10 micrograms/m3; p < 0.02). These findings suggest that exposure to fungal spores can adversely effect the daily respiratory status of some asthmatics.
Full text
PDF









Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Balmes J. R. The role of ozone exposure in the epidemiology of asthma. Environ Health Perspect. 1993 Dec;101 (Suppl 4):219–224. doi: 10.1289/ehp.93101s4219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaumont F., Kauffman H. F., Sluiter H. J., De Vries K. Sequential sampling of fungal air spores inside and outside the homes of mould-sensitive, asthmatic patients: a search for a relationship to obstructive reactions. Ann Allergy. 1985 Nov;55(5):740–746. [PubMed] [Google Scholar]
- Brunekreef B., Kinney P. L., Ware J. H., Dockery D., Speizer F. E., Spengler J. D., Ferris B. G., Jr Sensitive subgroups and normal variation in pulmonary function response to air pollution episodes. Environ Health Perspect. 1991 Jan;90:189–193. doi: 10.1289/ehp.90-1519500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdon J. G., Juniper E. F., Killian K. J., Hargreave F. E., Campbell E. J. The perception of breathlessness in asthma. Am Rev Respir Dis. 1982 Nov;126(5):825–828. doi: 10.1164/arrd.1982.126.5.825. [DOI] [PubMed] [Google Scholar]
- Burge H. Bioaerosols: prevalence and health effects in the indoor environment. J Allergy Clin Immunol. 1990 Nov;86(5):687–701. doi: 10.1016/s0091-6749(05)80170-8. [DOI] [PubMed] [Google Scholar]
- Burrows B., Martinez F. D., Halonen M., Barbee R. A., Cline M. G. Association of asthma with serum IgE levels and skin-test reactivity to allergens. N Engl J Med. 1989 Feb 2;320(5):271–277. doi: 10.1056/NEJM198902023200502. [DOI] [PubMed] [Google Scholar]
- Delfino R. J., Coate B. D., Zeiger R. S., Seltzer J. M., Street D. H., Koutrakis P. Daily asthma severity in relation to personal ozone exposure and outdoor fungal spores. Am J Respir Crit Care Med. 1996 Sep;154(3 Pt 1):633–641. doi: 10.1164/ajrccm.154.3.8810598. [DOI] [PubMed] [Google Scholar]
- Dhillon M. Current status of mold immunotherapy. Ann Allergy. 1991 May;66(5):385–392. [PubMed] [Google Scholar]
- Hasnain S. M., Wilson J. D., Newhook F. J. Fungal allergy and respiratory disease. N Z Med J. 1985 May 8;98(778):342–346. [PubMed] [Google Scholar]
- Hoek G., Fischer P., Brunekreef B., Lebret E., Hofschreuder P., Mennen M. G. Acute effects of ambient ozone on pulmonary function of children in The Netherlands. Am Rev Respir Dis. 1993 Jan;147(1):111–117. doi: 10.1164/ajrccm/147.1.111. [DOI] [PubMed] [Google Scholar]
- Hyland M. E., Kenyon C. A., Allen R., Howarth P. Diary keeping in asthma: comparison of written and electronic methods. BMJ. 1993 Feb 20;306(6876):487–489. doi: 10.1136/bmj.306.6876.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins P. F., Mullins J. K., Davies B. H., Williams D. A. The possible role of aero-allergens in the epidemic of asthma deaths. Clin Allergy. 1981 Nov;11(6):611–620. doi: 10.1111/j.1365-2222.1981.tb02182.x. [DOI] [PubMed] [Google Scholar]
- Jennrich R. I., Schluchter M. D. Unbalanced repeated-measures models with structured covariance matrices. Biometrics. 1986 Dec;42(4):805–820. [PubMed] [Google Scholar]
- Klabuschnigg A., Götz M., Horak F., Jäger S., Machalek A., Popow C., Haschke F., Skoda-Türk R. Influence of aerobiology and weather on symptoms in children with asthma. Respiration. 1981;42(1):52–60. doi: 10.1159/000194403. [DOI] [PubMed] [Google Scholar]
- Korsgaard J. House-dust mites and absolute indoor humidity. Allergy. 1983 Feb;38(2):85–92. doi: 10.1111/j.1398-9995.1983.tb01591.x. [DOI] [PubMed] [Google Scholar]
- LEINER G. C., ABRAMOWITZ S., SMALL M. J., STENBY V. B., LEWIS W. A. EXPIRATORY PEAK FLOW RATE. STANDARD VALUES FOR NORMAL SUBJECTS. USE AS A CLINICAL TEST OF VENTILATORY FUNCTION. Am Rev Respir Dis. 1963 Nov;88:644–651. doi: 10.1164/arrd.1963.88.5.644. [DOI] [PubMed] [Google Scholar]
- Lehrer S. B., Hughes J. M., Altman L. C., Bousquet J., Davies R. J., Gell L., Li J., Lopez M., Malling H. J., Mathison D. A. Prevalence of basidiomycete allergy in the USA and Europe and its relationship to allergic respiratory symptoms. Allergy. 1994 Jul;49(6):460–465. doi: 10.1111/j.1398-9995.1994.tb00840.x. [DOI] [PubMed] [Google Scholar]
- Licorish K., Novey H. S., Kozak P., Fairshter R. D., Wilson A. F. Role of Alternaria and Penicillium spores in the pathogenesis of asthma. J Allergy Clin Immunol. 1985 Dec;76(6):819–825. doi: 10.1016/0091-6749(85)90755-9. [DOI] [PubMed] [Google Scholar]
- Liu L. J., Delfino R., Koutrakis P. Ozone exposure assessment in a southern California community. Environ Health Perspect. 1997 Jan;105(1):58–65. doi: 10.1289/ehp.9710558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L. J., Koutrakis P., Suh H. H., Mulik J. D., Burton R. M. Use of personal measurements for ozone exposure assessment: a pilot study. Environ Health Perspect. 1993 Sep;101(4):318–324. doi: 10.1289/ehp.93101318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez M., Voigtlander J. R., Lehrer S. B., Salvaggio J. E. Bronchoprovocation studies in basidiospore-sensitive allergic subjects with asthma. J Allergy Clin Immunol. 1989 Aug;84(2):242–246. doi: 10.1016/0091-6749(89)90331-x. [DOI] [PubMed] [Google Scholar]
- Louis T. A., Lavori P. W., Bailar J. C., 3rd, Polansky M. Crossover and self-controlled designs in clinical research. N Engl J Med. 1984 Jan 5;310(1):24–31. doi: 10.1056/NEJM198401053100106. [DOI] [PubMed] [Google Scholar]
- Metzger W. J., Richerson H. B., Worden K., Monick M., Hunninghake G. W. Bronchoalveolar lavage of allergic asthmatic patients following allergen bronchoprovocation. Chest. 1986 Apr;89(4):477–483. doi: 10.1378/chest.89.4.477. [DOI] [PubMed] [Google Scholar]
- Molfino N. A., Slutsky A. S., Zamel N. The effects of air pollution on allergic bronchial responsiveness. Clin Exp Allergy. 1992 Jul;22(7):667–672. doi: 10.1111/j.1365-2222.1992.tb00189.x. [DOI] [PubMed] [Google Scholar]
- Neas L. M., Dockery D. W., Koutrakis P., Tollerud D. J., Speizer F. E. The association of ambient air pollution with twice daily peak expiratory flow rate measurements in children. Am J Epidemiol. 1995 Jan 15;141(2):111–122. doi: 10.1093/oxfordjournals.aje.a117399. [DOI] [PubMed] [Google Scholar]
- O'Hollaren M. T., Yunginger J. W., Offord K. P., Somers M. J., O'Connell E. J., Ballard D. J., Sachs M. I. Exposure to an aeroallergen as a possible precipitating factor in respiratory arrest in young patients with asthma. N Engl J Med. 1991 Feb 7;324(6):359–363. doi: 10.1056/NEJM199102073240602. [DOI] [PubMed] [Google Scholar]
- Reid M. J., Moss R. B., Hsu Y. P., Kwasnicki J. M., Commerford T. M., Nelson B. L. Seasonal asthma in northern California: allergic causes and efficacy of immunotherapy. J Allergy Clin Immunol. 1986 Oct;78(4 Pt 1):590–600. doi: 10.1016/0091-6749(86)90076-x. [DOI] [PubMed] [Google Scholar]
- Sakaguchi M., Inouye S., Sasaki R., Hashimoto M., Kobayashi C., Yasueda H. Measurement of airborne mite allergen exposure in individual subjects. J Allergy Clin Immunol. 1996 May;97(5):1040–1044. doi: 10.1016/s0091-6749(96)70255-5. [DOI] [PubMed] [Google Scholar]
- Salvaggio J., Seabury J., Schoenhardt F. A. New Orleans asthma. V. Relationship between Charity Hospital asthma admission rates, semiquantitative pollen and fungal spore counts, and total particulate aerometric sampling data. J Allergy Clin Immunol. 1971 Aug;48(2):96–114. doi: 10.1016/0091-6749(71)90091-1. [DOI] [PubMed] [Google Scholar]
- Solomon W. R., Burge H. A., Boise J. R. Exclusion of particulate allergens by window air conditioners. J Allergy Clin Immunol. 1980 Apr;65(4):305–308. doi: 10.1016/0091-6749(80)90160-8. [DOI] [PubMed] [Google Scholar]
- Targonski P. V., Persky V. W., Ramekrishnan V. Effect of environmental molds on risk of death from asthma during the pollen season. J Allergy Clin Immunol. 1995 May;95(5 Pt 1):955–961. doi: 10.1016/s0091-6749(95)70095-1. [DOI] [PubMed] [Google Scholar]
- Weiss S. T., Ware J. H. Overview of issues in the longitudinal analysis of respiratory data. Am J Respir Crit Care Med. 1996 Dec;154(6 Pt 2):S208–S211. doi: 10.1164/ajrccm/154.6_Pt_2.S208. [DOI] [PubMed] [Google Scholar]
- Wickman M., Gravesen S., Nordvall S. L., Pershagen G., Sundell J. Indoor viable dust-bound microfungi in relation to residential characteristics, living habits, and symptoms in atopic and control children. J Allergy Clin Immunol. 1992 Mar;89(3):752–759. doi: 10.1016/0091-6749(92)90384-e. [DOI] [PubMed] [Google Scholar]