Abstract
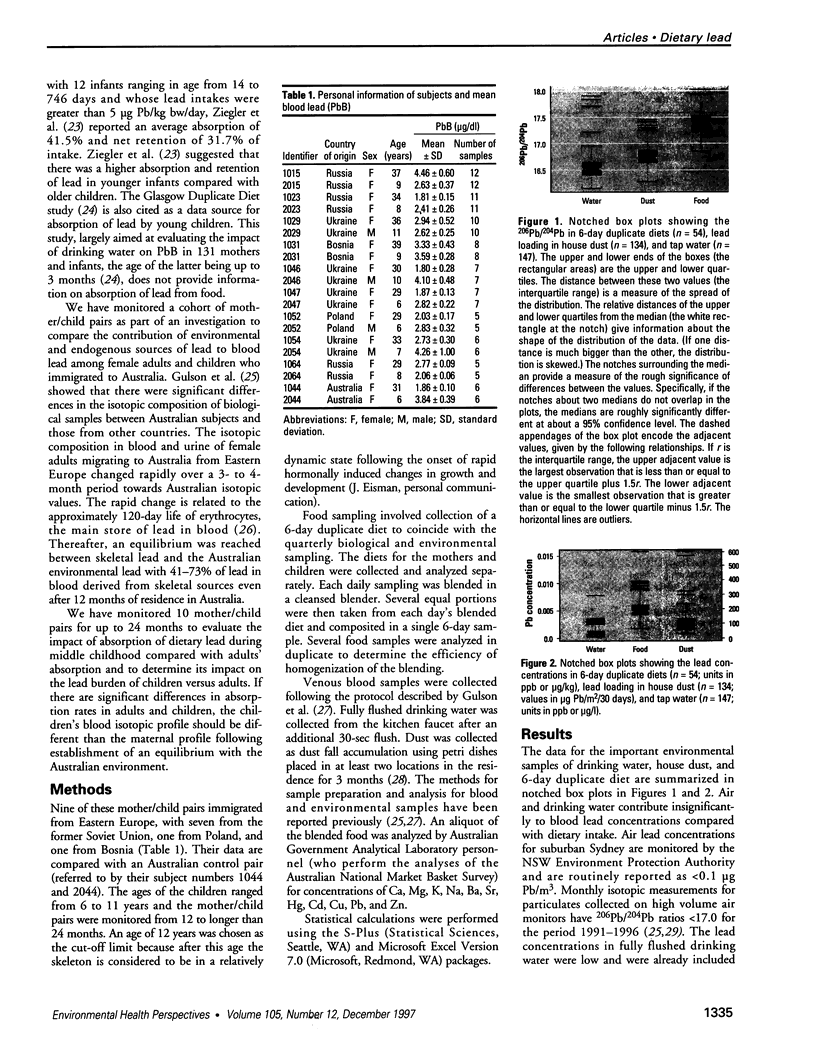
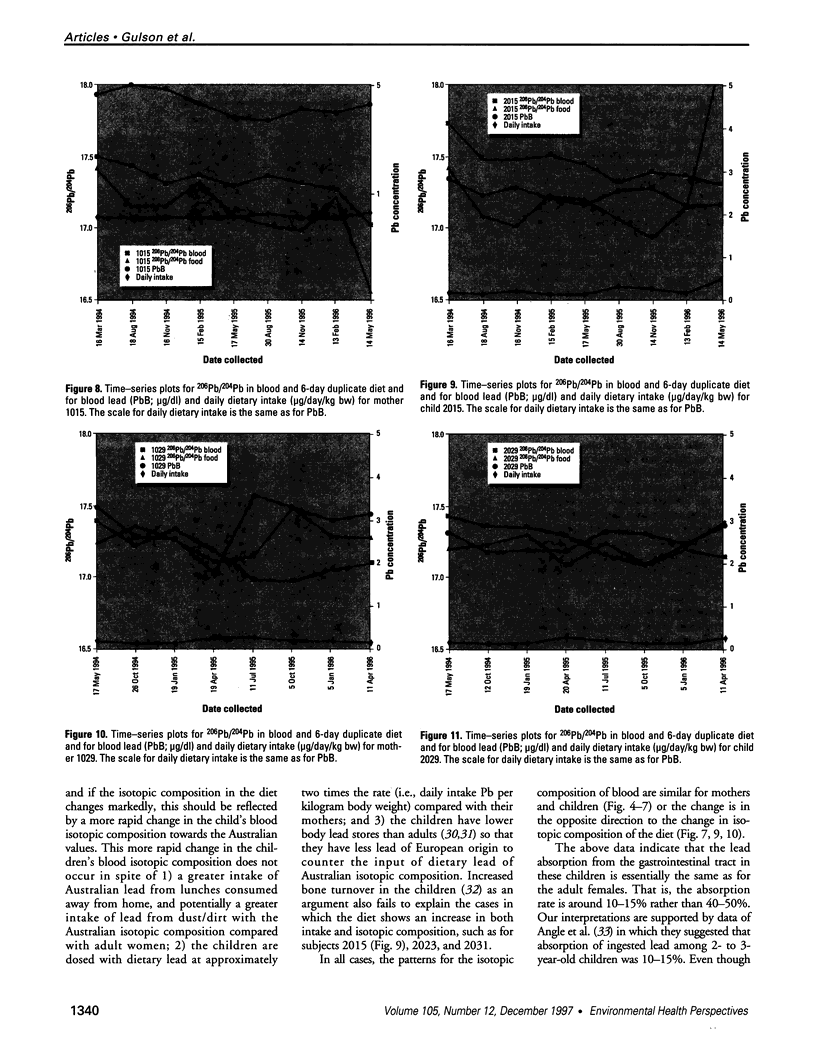
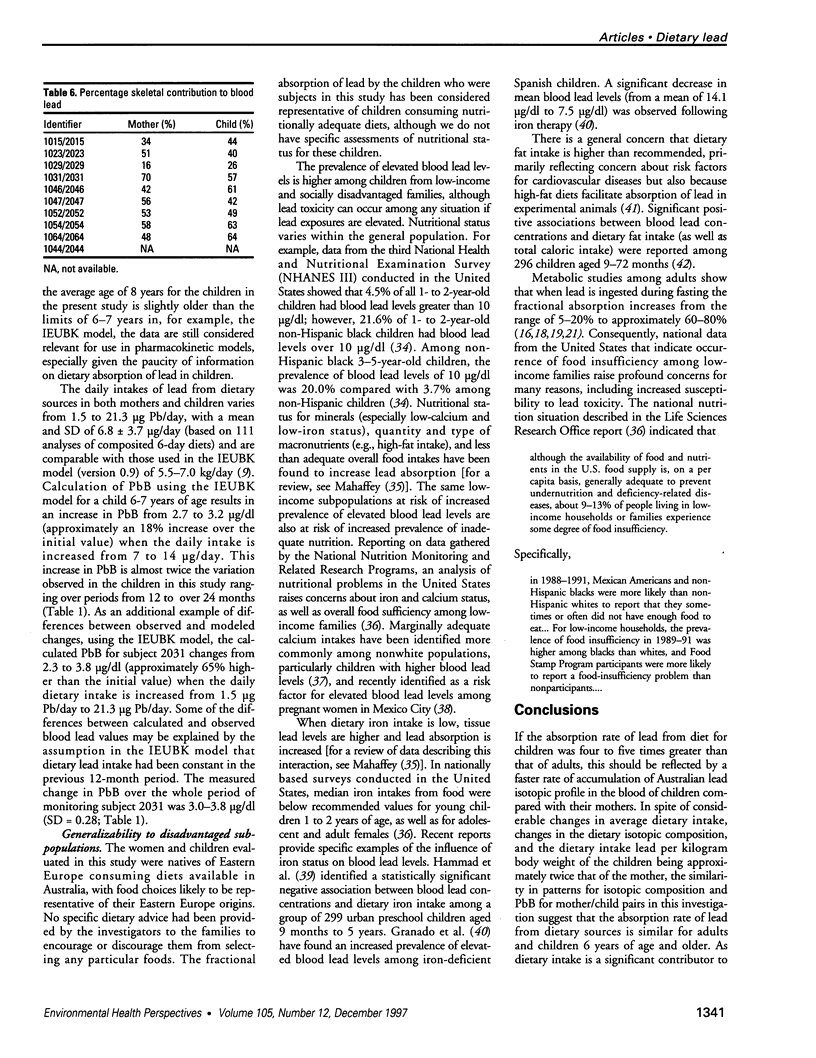
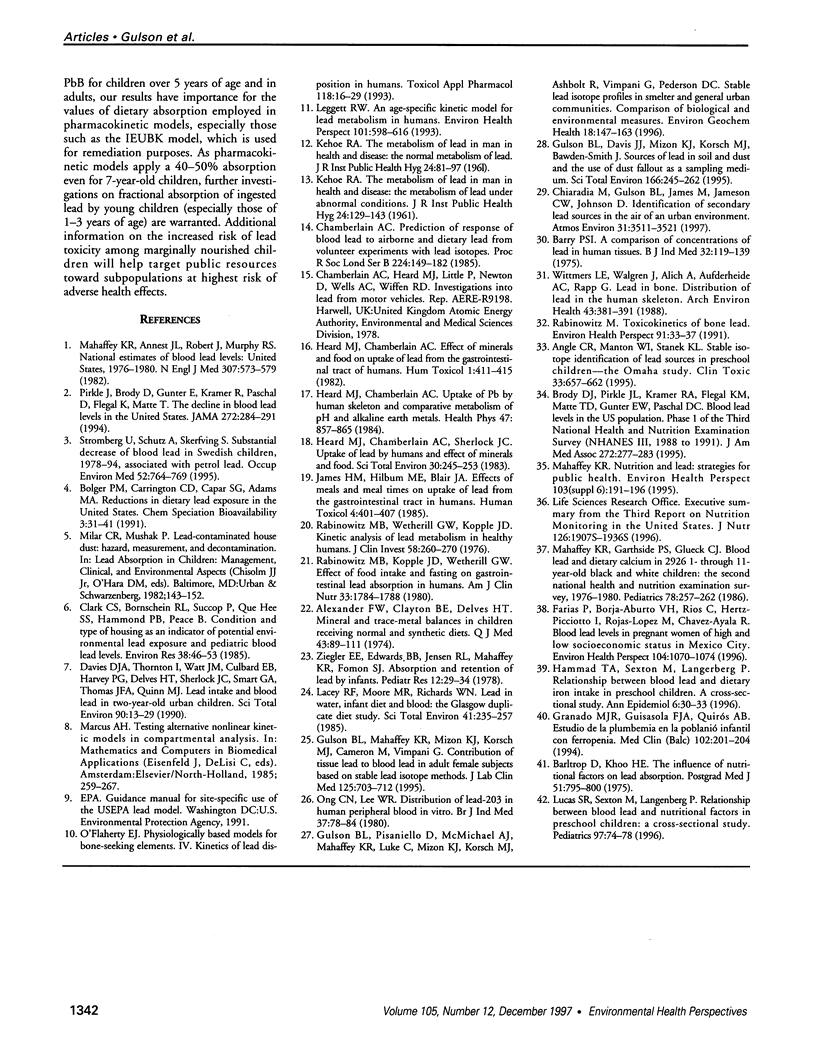
Blood and environmental samples, including a quarterly 6-day duplicate diet, for nine mother/child pairs from Eastern Europe have been monitored for 12 to >24 months with high precision stable lead isotope analysis to evaluate the changes that occur when the subjects moved from one environment (Eastern Europe) to another with different stable lead isotopes (Australia). The children were between 6 and 11 years of age and the mothers were between 29 and 37 years of age. These data were compared with an Australian control mother/child pair, aged 31 and 6 years, respectively. A rationale for undertaking this study of mother/child pairs was to evaluate if there were differences in the patterns and clearance rates of lead from blood in children compared with their mothers. Blood lead concentrations ranged from 2.1 to 3.9 microg/dl in the children and between 1.8 and 4.5 microg/dl in the mothers, but the mean of differences between each mother and her child did not differ significantly from zero. Duplicate diets contained from 2.4 to 31.8 microg Pb/kg diet; the mean+/- standard deviation was 5.5 +/- 2.1 microg Pb/kg and total daily dietary intakes ranged from 1.6 to 21.3 microg/day. Mean daily dietary intakes relative to body weight showed that the intake for children was approximately double that for the mothers (0.218 vs. 0. 113 microg Pb/kg body weight/day). The correlations between blood lead concentration and mean daily dietary intake either relative to body weight or total dietary intake did not reach statistical significance (p>0.05). Estimation of the lead coming from skeletal (endogenous) sources relative to the contribution from environmental (exogenous) sources ranges from 8 to 70% for the mothers and 12 to 66% for the children. The difference between mothers and children is not statistically significant (p = 0.28). The children do not appear to achieve the Australian lead isotopic profile at a faster rate than their mothers. These data provide evidence that the absorption or uptake of lead from dietary sources is similar in adult females and children of the age in this study. In spite of lower bone lead and faster bone remodeling and recycling in children compared with adult females, we see no differences between the mothers and their children in overall contribution of tissue lead to blood lead. Results from this study suggest that fractional absorption of ingested lead by children 6-11 years of age is comparable with absorption patterns observed among adult females in the 29-37-year-old age range. Because pharmacokinetic models apply a 40-50% absorption even for 7-year-old children, further investigations on fractional absorption of ingested lead by young children are warranted.Further investigations are especially needed in younger children than those who were subjects in the current study, particularly children in the 1-3-year-old age range. In addition, the effect of nutritional status and patterns of food intake on children's lead absorption require investigation, particularly given the increased prevalence of marginal nutritional status among low-income populations that are at increased risk of elevated blood lead levels.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alexander F. W., Clayton B. E., Delves H. T. Mineral and trace-metal balances in children receiving normal and synthetic diets. Q J Med. 1974 Jan;43(169):89–111. [PubMed] [Google Scholar]
- Angle C. R., Manton W. I., Stanek K. L. Stable isotope identification of lead sources in preschool children--the Omaha Study. J Toxicol Clin Toxicol. 1995;33(6):657–662. doi: 10.3109/15563659509010624. [DOI] [PubMed] [Google Scholar]
- Barltrop D., Khoo H. E. The influence of nutritional factors on lead absorption. Postgrad Med J. 1975 Nov;51(601):795–800. doi: 10.1136/pgmj.51.601.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry P. S. A comparison of concentrations of lead in human tissues. Br J Ind Med. 1975 May;32(2):119–139. doi: 10.1136/oem.32.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody D. J., Pirkle J. L., Kramer R. A., Flegal K. M., Matte T. D., Gunter E. W., Paschal D. C. Blood lead levels in the US population. Phase 1 of the Third National Health and Nutrition Examination Survey (NHANES III, 1988 to 1991) JAMA. 1994 Jul 27;272(4):277–283. doi: 10.1001/jama.272.4.277. [DOI] [PubMed] [Google Scholar]
- Chamberlain A. C. Prediction of response of blood lead to airborne and dietary lead from volunteer experiments with lead isotopes. Proc R Soc Lond B Biol Sci. 1985 Apr 22;224(1235):149–182. doi: 10.1098/rspb.1985.0027. [DOI] [PubMed] [Google Scholar]
- Clark C. S., Bornschein R. L., Succop P., Que Hee S. S., Hammond P. B., Peace B. Condition and type of housing as an indicator of potential environmental lead exposure and pediatric blood lead levels. Environ Res. 1985 Oct;38(1):46–53. doi: 10.1016/0013-9351(85)90071-4. [DOI] [PubMed] [Google Scholar]
- Davies D. J., Thornton I., Watt J. M., Culbard E. B., Harvey P. G., Delves H. T., Sherlock J. C., Smart G. A., Thomas J. F., Quinn M. J. Lead intake and blood lead in two-year-old U.K. urban children. Sci Total Environ. 1990 Jan;90:13–29. doi: 10.1016/0048-9697(90)90182-t. [DOI] [PubMed] [Google Scholar]
- Farias P., Borja-Aburto V. H., Rios C., Hertz-Picciotto I., Rojas-Lopez M., Chavez-Ayala R. Blood lead levels in pregnant women of high and low socioeconomic status in Mexico City. Environ Health Perspect. 1996 Oct;104(10):1070–1074. doi: 10.1289/ehp.961041070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulson B. L., Mahaffey K. R., Mizon K. J., Korsch M. J., Cameron M. A., Vimpani G. Contribution of tissue lead to blood lead in adult female subjects based on stable lead isotope methods. J Lab Clin Med. 1995 Jun;125(6):703–712. [PubMed] [Google Scholar]
- Hammad T. A., Sexton M., Langenberg P. Relationship between blood lead and dietary iron intake in preschool children. A cross-sectional study. Ann Epidemiol. 1996 Jan;6(1):30–33. doi: 10.1016/1047-2797(95)00097-6. [DOI] [PubMed] [Google Scholar]
- Heard M. J., Chamberlain A. C. Effect of minerals and food on uptake of lead from the gastrointestinal tract in humans. Hum Toxicol. 1982 Oct;1(4):411–415. doi: 10.1177/096032718200100407. [DOI] [PubMed] [Google Scholar]
- Heard M. J., Chamberlain A. C., Sherlock J. C. Uptake of lead by humans and effect of minerals and food. Sci Total Environ. 1983 Sep;30:245–253. doi: 10.1016/0048-9697(83)90016-5. [DOI] [PubMed] [Google Scholar]
- Heard M. J., Chamberlain A. C. Uptake of Pb by human skeleton and comparative metabolism of Pb and alkaline earth elements. Health Phys. 1984 Dec;47(6):857–865. doi: 10.1097/00004032-198412000-00006. [DOI] [PubMed] [Google Scholar]
- James H. M., Hilburn M. E., Blair J. A. Effects of meals and meal times on uptake of lead from the gastrointestinal tract in humans. Hum Toxicol. 1985 Jul;4(4):401–407. doi: 10.1177/096032718500400406. [DOI] [PubMed] [Google Scholar]
- KEHOE R. A. The metabolism of lead in man in health and disease. 2(2). The metabolism of lead under abnormal conditions. J R Inst Public Health. 1961 Jun;24:129–143. [PubMed] [Google Scholar]
- KEHOE R. A. The metabolism of lead in man in health and disease. I. The normal metabolism of lead. J R Inst Public Health. 1961 Apr;24:81–97. [PubMed] [Google Scholar]
- Lacey R. F., Moore M. R., Richards W. N. Lead in water, infant diet and blood: the Glasgow Duplicate Diet Study. Sci Total Environ. 1985 Mar 1;41(3):235–257. doi: 10.1016/0048-9697(85)90144-5. [DOI] [PubMed] [Google Scholar]
- Leggett R. W. An age-specific kinetic model of lead metabolism in humans. Environ Health Perspect. 1993 Dec;101(7):598–616. doi: 10.1289/ehp.93101598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas S. R., Sexton M., Langenberg P. Relationship between blood lead and nutritional factors in preschool children: a cross-sectional study. Pediatrics. 1996 Jan;97(1):74–78. [PubMed] [Google Scholar]
- Mahaffey K. R., Annest J. L., Roberts J., Murphy R. S. National estimates of blood lead levels: United States, 1976-1980: association with selected demographic and socioeconomic factors. N Engl J Med. 1982 Sep 2;307(10):573–579. doi: 10.1056/NEJM198209023071001. [DOI] [PubMed] [Google Scholar]
- Mahaffey K. R., Gartside P. S., Glueck C. J. Blood lead levels and dietary calcium intake in 1- to 11-year-old children: the Second National Health and Nutrition Examination Survey, 1976 to 1980. Pediatrics. 1986 Aug;78(2):257–262. [PubMed] [Google Scholar]
- Mahaffey K. R. Nutrition and lead: strategies for public health. Environ Health Perspect. 1995 Sep;103 (Suppl 6):191–196. doi: 10.1289/ehp.95103s6191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Flaherty E. J. Physiologically based models for bone-seeking elements. IV. Kinetics of lead disposition in humans. Toxicol Appl Pharmacol. 1993 Jan;118(1):16–29. doi: 10.1006/taap.1993.1004. [DOI] [PubMed] [Google Scholar]
- Ong C. N., Lee W. R. Distribution of lead-203 in human peripheral blood in vitro. Br J Ind Med. 1980 Feb;37(1):78–84. doi: 10.1136/oem.37.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkle J. L., Brody D. J., Gunter E. W., Kramer R. A., Paschal D. C., Flegal K. M., Matte T. D. The decline in blood lead levels in the United States. The National Health and Nutrition Examination Surveys (NHANES) JAMA. 1994 Jul 27;272(4):284–291. [PubMed] [Google Scholar]
- Rabinowitz M. B., Kopple J. D., Wetherill G. W. Effect of food intake and fasting on gastrointestinal lead absorption in humans. Am J Clin Nutr. 1980 Aug;33(8):1784–1788. doi: 10.1093/ajcn/33.8.1784. [DOI] [PubMed] [Google Scholar]
- Rabinowitz M. B. Toxicokinetics of bone lead. Environ Health Perspect. 1991 Feb;91:33–37. doi: 10.1289/ehp.919133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabinowitz M. B., Wetherill G. W., Kopple J. D. Kinetic analysis of lead metabolism in healthy humans. J Clin Invest. 1976 Aug;58(2):260–270. doi: 10.1172/JCI108467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redondo Granado M. J., Alvarez Guisasola F. J., Blanco Quirós A. Estudio de la plumbemia en la población infantil con ferropenia. Med Clin (Barc) 1994 Feb 19;102(6):201–204. [PubMed] [Google Scholar]
- Shattock S. G. Rhabdomyoma of the Urinary Bladder. Proc R Soc Med. 1910;3(PATHOL):31–41. [PMC free article] [PubMed] [Google Scholar]
- Strömberg U., Schütz A., Skerfving S. Substantial decrease of blood lead in Swedish children, 1978-94, associated with petrol lead. Occup Environ Med. 1995 Nov;52(11):764–769. doi: 10.1136/oem.52.11.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittmers L. E., Jr, Aufderheide A. C., Wallgren J., Rapp G., Jr, Alich A. Lead in bone. IV. Distribution of lead in the human skeleton. Arch Environ Health. 1988 Nov-Dec;43(6):381–391. doi: 10.1080/00039896.1988.9935855. [DOI] [PubMed] [Google Scholar]
- Ziegler E. E., Edwards B. B., Jensen R. L., Mahaffey K. R., Fomon S. J. Absorption and retention of lead by infants. Pediatr Res. 1978 Jan;12(1):29–34. doi: 10.1203/00006450-197801000-00008. [DOI] [PubMed] [Google Scholar]