Abstract
The health inequalities in South Africa are rapidly worsening. Since 1994, the new democratic government has initiated a number of large-scale policies and programs with explicit pro-equity objectives that have improved access to health care and other social resources. However, these policies and programs have been constrained by macroeconomic policies that dictate fiscal restraint and give priority to technical rather than developmental considerations.
We propose an approach to improving health for all that focuses on equity in the allocation of health resources. The implementation of pro-equity policies requires, in addition to technically efficacious interventions, both advocacy initiatives and communication with, and the involvement of, affected communities. The Cape Town Equity Gauge project is presented as one example of a response to the challenge of inequity.
THE VAST INEQUALITIES IN economic and social indicators among middle-income countries, such as South Africa and Brazil, are widely recognized.1 In South Africa, until the late 1980s, apartheid institutionalized such inequalities through labor laws and highly unequal investments in services for different racial groups. South Africa is now a country where the liberation movement that opposed such inequality constitutes the core of government and is under pressure to address this legacy. We present a policy analysis of South Africa’s poor health performance and persisting inequalities and cite reasons for this apparent anomaly by analyzing the nation’s health situation and the appropriateness of the government’s policies for improvement. The dominant global and national policy environment that prioritizes the market and the private sector discourages state spending on “unproductive” social investment. We believe this policy environment encourages efficiency at the expense of equity and accounts largely for the continuing health and welfare inequities, despite constitutionally enshrined rights to health.
WEALTH, HEALTH, AND INEQUALITY IN SOUTH AFRICA
South Africa contributes almost half of the total economic output of Sub-Saharan Africa, and its per capita gross domestic product (> $10000) makes it a middle-income country.2 South Africa’s health system has an international reputation for (1) pioneering the world’s first heart transplant in 1967, (2) contributing scientific understanding to health issues such as severe child malnutrition,3,4 and (3) innovating health systems, e.g., Kark et al.’s model of community-oriented primary care.5
South Africa’s wealth and scientific and technical capacity notwithstanding, its health and other social outcomes are discrepantly poor in comparison to other countries (Table 1 ▶). Furthermore, this situation is deteriorating with the increasing impact of HIV/AIDS. Between 1995 and 2002, life expectancy at birth was estimated to have declined by 16.3%, from 61.4 years to 51.4 years.6 It is estimated that by 2015, average life expectancy could fall by more than 30% compared with 1996.7
TABLE 1—
Selected Health Indicators for South Africa and 5 Other Comparable Countries
| Cuba | Malaysia | Brazil | Thailand | China | South Africa | |
| 2002 GDP per Capita, Purchasing Power Parity, US$ | 5 259 | 9 120 | 7 770 | 7 010 | 4 580 | 10 070 |
| 2002 Public Health Expenditure, % of GDP | 6.2 | 2.1 | 3.2 | 2.1 | 2 | 3.6 |
| Children Fully Immunized Against Measles at Year of Age in 2002, % | 98 | 92 | 93 | 94 | 79 | 78 |
| Physicians per 100 000 Population, 1990–2003 | 596 | 68 | 206 | 30 | 164 | 25 |
| Children Younger Than 5 Years Below Average Height, 1995–2002, % | 5 | … | 11 | 16 | 16 | 25 |
| Life Expectancy at Birth in 2000, Years | 76.7 | 73 | 68.1 | 71 | 71 | 47.7 |
| Infant Mortality Rate per 1000 Live Births, 2002 | 7 | 8 | 30 | 31 | 31 | 52 |
Source. UNDP World Development Indicators.8
Note. GDP = gross domestic product.
The summary indicators shown in Table 1 ▶8 disguise extreme disparities in both wealth and access to services, which are proving to be resistant to change. The infant mortality rate per 1000 live births is still more than 4 times higher among Blacks compared with Whites (47 vs. 11, respectively).9 In 2001, the life expectancy of Blacks was 18 years lower than that of Whites (51 vs. 69 years, respectively).6 Differences in infant mortality across the 9 provinces of South Africa also are large, ranging from a rate of 61 per 1000 live births in the Eastern Cape to a rate of 30 in the Western Cape.9 There also is a great deal of variation within provinces. For example, for the 3 to 4 million people who still live in the former Transkei Homeland area in the Eastern Cape, the infant mortality rate is 99 per 1000 live births compared with a rate of 28 in the largest metropolitan area within the province.10 Any plausible explanation for South Africa’s poor performance in health requires a disaggregation of these inequalities and an interrogation of their underlying causes.
THE PATTERN OF ILL HEALTH AND ITS DETERMINANTS
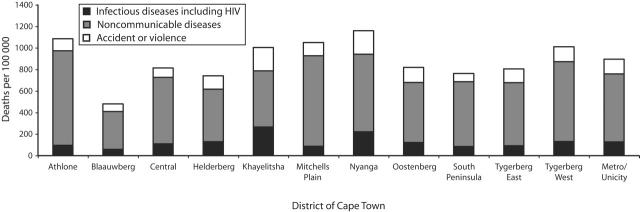
The disease and death profile in South Africa predominantly reflects a society in which the more-affluent sections of the population have completed the epidemiological transition, and economically disadvantaged groups continue to suffer from pretransitional pathologies. According to the profile, infectious diseases—and increasingly, HIV/AIDS—affect the poor, chronic diseases affect both rich and poor and are associated with an urbanized diet and lifestyle, and a large burden of disease, particularly among the poor, is the result of trauma and violence.11 This is starkly illustrated by the pattern of adult mortality across districts in Cape Town (Figure 1 ▶).12
FIGURE 1—
Age-standardized mortality rates across health districts in Cape Town, South Africa, 2001.
Source. Groenewald et al.13
In addition to the high levels of communicable and noncommunicable disease mortality, the poor in Cape Town also have very high rates of mortality due to traffic accidents and violence. The homicide rate in the poorer districts of Cape Town exceeds 100 per 100 000, a level almost unmatched anywhere else in the world.14 Overall, it is estimated that premature adult mortality (measured as the probability of a 15-year-old dying before the age of 60) will reach levels close to 80% within the next 10 years.15
This distribution and pattern of morbidity and mortality are shaped by persisting inequalities in major immediate risk factors, such as the following. Rates of malnutrition show a marked gradient according to socioeconomic status, with stunting rates 6 times higher among those in the poorest quintile (30%) compared with those in the richest quintile (6%).16 Children who reside in the predominantly rural and Black provinces, such as the Eastern Cape, have much higher stunting rates (20%) compared with children who live in the more urbanized and racially mixed provinces (14%), such as the Western Cape,17 and are 9 times more likely not to have had a skilled attendant during birth (18% vs. 2%, respectively).9 Their families also are 2.5 times more likely to lack food security (83% vs 31%),16 4 times less likely to have access to safe sanitation (31% vs 7.5%),18 and 10 times more likely to be using indoor pollutants (e.g., firewood) for cooking and heating (35% vs 3%).19
These inequalities are further aggravated by other growing inequalities, such as employment and income. From 1996 to 2001, the unemployment rate among Blacks increased from 42.5% to more than 50% compared with an increase from 4.6% to 6.3% among Whites. In 2001, 87% of the bottom 40% of South African households had 0 to 1 working family members and relied heavily on pensions or remittances.20 Perhaps contributing to a greater perception of exclusion among the Black majority is that a small minority of Blacks is greatly benefiting from the political transition. The proportion of Blacks in the richest quintile of the South African population increased 5-fold from 1990 to 1995, when the population increased from 2% to 10%. This increase may well have been at the expense of the poor, because the poorest 40% of the population have experienced a drop in their share of income. The level of income disparity (expressed as the Gini coefficient) between Black households increased from 0.3 in 1990 to 0.54 in 1998 (close to the national figure of 0.58).21
KEY GOVERNMENT POLICIES AND PROGRAMS
Since 1994, the first democratic government has put in place policies that address the apartheid health legacy of racial discrimination, fragmentation of management responsibility between different authorities, and centralized control of resources.22 The private health care sector, which serves approximately 15% of the population despite receiving almost 60% of the health care resources (financial and human), remains largely unaffected by these changes in policy and organization.
During the immediate period after political democracy was achieved, several key pro-equity policies were initiated in the public sector. Among the most relevant to health were a vigorous building program for primary health care facilities; the introduction of free maternal and child health care, which was later expanded to free primary care for all who used public sector facilities; a primary school nutrition program; an expansion of basic water provision; and an extension of social welfare grants to previously excluded populations. More recently, antiretroviral treatment for AIDS has been made available to selected public sector health facilities.
Although these bold national policy initiatives improved access to social resources and basic services, their effect on outcomes is less evident. We believe their pro-equity impact has been compromised by factors that are both contextual (policies that facilitate or constrain sustainable approaches) and technical (specific program or intervention processes that successful interventions share).
CONTEXTUAL CONSTRAINTS
Political democracy in South Africa came at a time when the dominant thinking in development policy favored fiscal stringency and liberalizing the markets. These policies had a devastating effect on employment and income levels among the poor; thus, it will be difficult, if not impossible, to successfully surmount health and social inequalities without altering these factors. Additionally, the government’s real per capita investment in economic and welfare infrastructure declined by 14.1% between 1995 and 2002.23 Despite the South African government’s constitutional commitment to equity, the stagnating overall expenditure has made achieving equity extremely difficult.
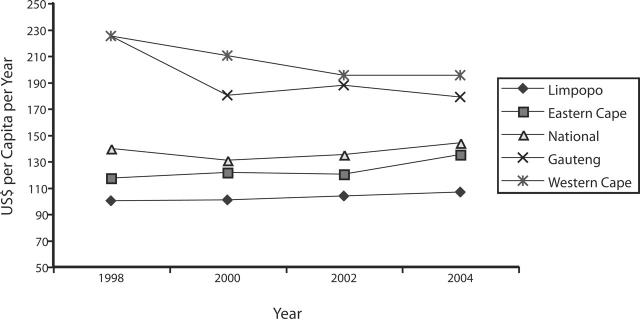
Although there has been some improvement in health spending among previously disadvantaged provinces, average real per capita health expenditure has only increased at an annual rate of 0.3% since 1998 (Figure 2 ▶). After factoring in increases in health workers’ salaries, this annual rate translates into a significant reduction in personnel numbers—at least 19000 jobs have been eliminated during the past 10 years,24 and a high percentage of public sector jobs are becoming vacant for a number of reasons, including the migration of large numbers of health professionals, especially nurses, to the United Kingdom and other countries.25 Unfortunately, many of these jobs have been eliminated or are vacant in the poorest districts, which has resulted in increasing inequalities in the distribution of health personnel. A recent study found that district health expenditures ranged from under $8 per capita per year to $60.26 Furthermore, districts with the greatest health needs, as indicated by the highest levels of deprivation, received the least resources.26
FIGURE 2—
Per capita health expenditures in South Africa, by province.
Source. Doherty et al.28
The greater ability of wealthier districts to absorb new resources for HIV treatment programs is further widening the gap in available public health services.27 Also, the stagnation of government health expenditures in the context of rising morbidity has led to an increasing proportion of total health expenditures coming from out-of-pocket spending, thereby reducing the amount of cross-subsidization possible between the rich and the poor.28
Even when significant resources have been allocated (e.g., the primary school nutrition program and water programs), their developmental potential and sustainability have been undermined by the drive to secure short-term gains through engaging private sector technicians and suppliers and eschewing more developmental approaches that build community capacity and stimulate local entrepreneurship. The current approach is in line with new public management policies that focus on a slimmed down state, reduced levels of public expenditure, increased efficiency in the provision of public services through mechanisms such as contracting and competition, and an extension of the private sector’s role.29 The management of water and sanitation services in South Africa is an example, because the construction, operation, maintenance, and management of water and sanitation are rapidly moving from local governments to private companies.30 There is a concomitant emphasis on cost recovery, and the increasing introduction of prepaid water and electricity meters is the latest manifestation of this. Unfortunately, there is increasing evidence that this is having a serious impact on public health. The recent cholera epidemic in South Africa, which infected more than 200 000 people, has been traced to a community that was forced to use polluted river water after being unable to afford the tariffs for purified tap water.31 Evans conservatively estimated that between 1994 and 2001, 9.8 million households had their water turned off because of nonpayment.32
The policy context in South Africa influences not only the approach to the financing and management of projects but also their technical features. For example, there has been a technocratic approach to water and sanitation provision, where the often inappropriate focus has been on hardware—a large plant versus the protection of small water sources—at the expense of software—the crucial social processes needed to implement and sustain development projects.33 The laborious but indispensable processes of engaging communities in the various options for water and sanitation, and developing their capacity to assist in the construction and maintenance of facilities, for the most part have been eschewed in South Africa.34 Field reports suggest that many new water installations are failing because of lack of maintenance and cost recovery.35,36
Another example is the primary school nutrition program, which has contracted commercial suppliers—who often provide relatively expensive and nonnutritious products—rather than engage local, unemployed women to cook meals with locally produced foods.37 Furthermore, the foods supplied are often specially devised products that are not generally available through normal retail outlets or cultivatable by those who still engage in subsistence farming, which undermines the potential long-term contribution to household food security.38
These factors—technical and contextual— also have constrained the success of HIV programs. President Mbeki’s reluctance to take a central role in the fight against HIV/AIDS is well known, but this should not overshadow the fact that South Africa developed a comprehensive AIDS plan more than 10 years ago and has committed considerable resources to HIV programs. The failure to contain the epidemic can be traced to the contextual changes of rapid urbanization, the continued operation of the migrant labor system, and the persistent poverty. However, continual restructuring of state structures, declining budgets, and limited managerial capacity—among other reasons—have seriously curtailed the state’s ability to mount a response beyond condom distribution and health education.39 These weaknesses also have limited the effectiveness of other public health programs, both those that are not so dependent on a consistent and functional health system (e.g., the Expanded Program on Immunization) (Table 1 ▶) and more complex programs, such as the prevention of mother-to-child transmission of HIV40 and tuberculosis41 and the prevention and management of severe malnutrition.42
ALTERNATIVE RESPONSES
Bridging the continuing gap between health policy and reality requires more explicit targeting of resources through measurement of key disparities in health needs and a social process and application of effective technologies to address these needs.43 Successful large-scale health and nutrition programs are often based on cost-effective health facility interventions associated with broader intersectoral interventions that include active community involvement.44 Fundamentally, this involves some sort of relationship between local community-based structures and personnel and state agents who have key technical skills.45 Advocacy and community mobilization are the keys to securing the accountability and the “political will” that are necessary for influencing more equitable resource allocation, because local initiatives contribute important insights for a pro-equity approach to public health programming.
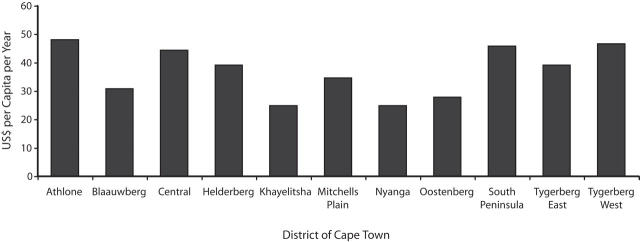
The Cape Town Equity Gauge (CTEG), which is 1 of 11 local initiatives around the world,46 is a partnership among the City of Cape Town, the Provincial Health and Welfare Departments, academic institutions, nongovernmental organizations, and community-based organizations. The CTEG’s goals are to measure and monitor inequities in health and health care to foster community mobilization and to generate advocacy action for policy change. The first CTEG project included measuring health resource allocation, such as the recurrent expenditure on, and the distribution of, personnel in primary care facilities across the different districts of Cape Town. This distribution has then been compared with a composite needs index, which includes data on disease burden and other indicators of deprivation (e.g., income levels, provision of water and sanitation, etc.) and has been calculated for each of the districts. The findings showed a very stark manifestation of the inverse care law47; the districts with the highest burden of disease, such as Nyanga and Khayelitsha, received far fewer health care resources than wealthier districts (Figure 3 ▶).
FIGURE 3—
Primary health care expenditures per dependent population across health districts in Cape Town, South Africa.
Source. Reagon et al.48
The involvement of local government policymakers and officials in the CTEG has required a prolonged process of negotiation and readjustment, because they raised concerns about the types of indicators to be measured and the weighting of those measures. These objections only had a minimal effect on the results, which were eventually accepted, because the inequities are so large. However, local government policymakers and officials have found it extremely difficult to shift resources away from the wealthier districts. One reason includes a concern about loss of efficiency, because many of the management and health systems in the poorer districts are not functioning well. While measurement of this health equity gap has included managers and policymakers, it is clear that without sustained advocacy and organized community demand, significant change in resource allocation is unlikely to be affected.
The CTEG’s measurement component has provided detailed empirical information about health inequities across the districts; however, a more textured insight into both the health management processes and the intersectoral involvement has been gained through a focus on a few priority health problems—HIV/AIDS and TB, diarrheal disease and intestinal worms, and violence and trauma. The dual objective of this more in-depth work has been both to facilitate improved quality of care and to engage affected communities and relevant state sectors in a process of analysis and action, the latter involving both community mobilization and advocacy. One example is provided in the next paragraph.
Local research showed high rates of intestinal worm infestation among primary schoolchildren in the Cape Town township of Khayelitsha, which sparked concern among local health workers, teachers, and community groups. A school-based de-worming, education, and improved sanitation program was successfully initiated, but reinfection rates were high.49 The CTEG team became involved at this stage and facilitated feedback sessions during school meetings, where teachers and parents learned about the main transmission routes (fecal contamination). Parents were provided with low-cost cameras to photograph community conditions that they thought might be contributing to the problem. These photos showed that the problem was a lack of proper sanitation, a problem compounded by the high water table and the sandy soil in Khayelitsha that prevented use of deep-pit toilets. Teachers developed new curricular materials about hygiene, and school administrators committed themselves to improving water and sanitation facilities within the schools. At the community level, a program was established to test and evaluate “dry sanitation” (urinary diversion) toilets as an option for the informal settlements. These proved to be highly popular, because each family owned a toilet that was close to their shacks.50 Access to sufficient potable water and obtaining space/resources for more dry toilets are problems for the community members, health workers, and researchers; however, the National Department of Water Affairs and Forestry recently provided resources to the Cape Town local authority for wider dissemination of this initiative. The focus of this pilot program has been active community participation in collaboration with the local government and the Department of Water Affairs and Forestry at all levels—from choosing the toilets and who tested them to training and education to participation in program management.
CONCLUSION
Post-apartheid South Africa is an instructive case study of the difficulties associated with redressing social and health inequities. Despite constitutionally enshrined social and economic rights and universal and apparent pro-equity policies, deep (and deepening) inequalities persist. This situation requires a different approach—one that focuses on the development of programs and initiatives that can provide models for larger-scale implementation. More importantly, these initiatives must include the measurement of inequities in resource allocation and quality of caring processes, advocacy efforts, and community member involvement to enhance their capacity to make demands for health equity.
Peer Reviewed
Contributors Both authors originated the study and wrote this article.
Human Participant Protection No protocol approval was needed for this study.
References
- 1.Sen AK. Inequality Re-examined. Cambridge, Mass: Harvard University Press; 1992.
- 2.World Bank. African Development Indicators. Washington, DC: World Bank Publications; 2004.
- 3.Brock JF, Autret M. Kwashiorkor in Africa. Bull World Health Org. 1952; 5:1–71. [PMC free article] [PubMed] [Google Scholar]
- 4.Hansen JD, Brock JF. Potassium deficiency in the pathogenesis of nutritional oedema in infants. Lancet. 1954; 267:477. [DOI] [PubMed] [Google Scholar]
- 5.Tollman SM. The Pholela Health Centre—the origins of community-oriented primary health care (COPC). An appreciation of the work of Sidney and Emily Kark. S Afr Med J. 1994;84:653–658. [PubMed] [Google Scholar]
- 6.Statistics South Africa. Causes of Death. 2002. Pretoria, South Africa: Statistics South Africa; 2003.
- 7.Dorrington RE, Bradshaw D, Budlender D. HIV/AIDS Profile of the Provinces of South Africa—Indicators for 2002. Cape Town, South Africa: Centre for Actuarial Research, Medical Research Council and the Actuarial Society of South Africa, University of Cape Town; 2002.
- 8.United Nations Development Programme. World Development Indicators 2004. Available at: http://hdr.undp.org/statistics/default.cfm. Accessed August 3, 2004.
- 9.Bradshaw D, Masiteng K, Nannan N. Health status and determinants. In: Ntuli A, Crisp N, Clark E, Barron P, eds. South African Health Review 2000. Durban, South Africa; Health Systems Trust; 2004:45–57.
- 10.National Department of Health. South African Demographic Health Survey 1998. Pretoria, South Africa: National Department of Health; 2001.
- 11.Bradshaw D. Health for all—monitoring equity. In: Ntuli A, Day C, eds. South African Health Review 1998. Durban, South Africa: Health Systems Trust; 1998:59–72.
- 12.Bradshaw D, Nannan N. Health status. In: Ijumba P, Day C, Ntuli A, eds. South African Health Review 2004. Durban, South Africa: Health Systems Trust; 2004:45–57.
- 13.Groenewald P, Bradshaw D, Nojilana B, et al. Cape Town Mortality, 2001, Part I, Cause of death and premature mortality. South African Medical Research Council, Cape Town, South Africa.
- 14.Prinsloo M, Matzopoulos R, Sukhai A. The magnitude of firearm homicide in Cape Town, 2001. Afr Safety Promotion: J Inj Violence Prev. 2003;1:19–25. [Google Scholar]
- 15.Dorrington R, Bourne D, Bradshaw D, Laubscher R, Timaeus IM. The Impact of HIV/AIDS on Adult Mortality in South Africa. Technical Report. Burden of Disease Research Unit. Cape Town, South Africa: Medical Research Council; 2001.
- 16.Project for Statistics on Living Standards and Development. South Af-rican Rich and Poor: Baseline Household Statistics. Rondebosch, South Africa: South African Labour and Development Research Unit; 1996.
- 17.Labadarios D, ed. The National Food Consumption Survey (NFCS): Children Aged 1—9 years, South Africa. Pre-toria, South Africa: National Department of Health; 2003. [PubMed]
- 18.Statistics South Africa. The People of South Africa Population Census, 2001. Census in Brief. Available at: http://www.statssa.gov.za/census2001/census2001.htm. Accessed August 20, 2004.
- 19.Statistics South Africa. October Household Survey 1999. Available at: http://www.statssa.gov.za/Statistical_releases/Statistical_releases.htm. Accessed July 20, 2004.
- 20.Statistics South Africa. Achieving a Better Life for All: Progress Between Census ’96 and Census 2001. Available at: http://www.statssa.gov.za/census2001/census2001.htm. Accessed August 20, 2004.
- 21.United Nations Development Programme. South Africa: Human Development Report 2000. Available at: http:// www.undp.org.za/sahdr2000/hdr.con-tents.pdf. Accessed March 25, 2004.
- 22.Van Rensburg HCJ, ed. Health and Health care in South Africa. Pretoria, South Africa: Van Schaik Publishers; 2004.
- 23.United Nations Development Programme. South Africa: Human Development Report 2003. Available at: http:// www.undp.org.za/NHDR2003.htm. Accessed March 25, 2004.
- 24.Blecher M, Thomas S. Health care financing. In: Ijumba P, Day C, Ntuli A, eds. South African Health Review. Dur-ban, South Africa: Health Systems Trust; 2004.
- 25.Padarath A, Ntuli A, Berthiaume L. Human resources. In: Ijumba P, Day C, Ntuli A, eds. South African Health Review. Durban, South Africa: Health Systems Trust; 2004.
- 26.Thomas S, Mbatsha S, Muirhead D, Okorafor O. Primary Health Care Financing and Need Across Health Districts in South Africa. Durban, South Africa: Local Government and Health Project Consortium, Health Systems Trust; 2004.
- 27.Scott V, Chopra M, Conrad E, Ntuli A. How equitable is the scaling up of HIV service provision in South Africa? S Afr Med J. 2005;95:109–113. [PubMed] [Google Scholar]
- 28.Doherty J, Thomas S, Muirhead D. Health Care Financing and Expenditure in Post-Apartheid South Africa, 1996/ 97–1998/99. Pretoria, South Africa: Department of Health; 2003.
- 29.Mills A. Reforming health sectors: fashion, passions and common sense. Paper presented at: Eighth Annual Public Health Forum, April 21–24, 1998; London, UK.
- 30.McDonald DA, Ruiters G. The Age of Commodity: Water Privatisation in Southern Africa. London, UK: Earthscan; 2004.
- 31.Deedat H, Cottle E. Cost recovery and prepaid water meters and the cholera outbreak in KwaZulu-Natal. In: Mc-Donald DA, Pape J, eds. Cost Recovery and the Crisis of Service Delivery. Lon-don, UK: Zed Books; 2002.
- 32.McDonald D. We are water wise. Mail and Guardian. December 2004: 17–23.
- 33.Evans P. Government action, development and social capital: reviewing the evidence for synergy. World Dev. 1996; 24:1119–1129. [Google Scholar]
- 34.McDonald DA. No Money, No service: South Africa’s poorest citizens lose out under attempts to recover service costs for water and power. Alternatives. 2002;28:21–43. [Google Scholar]
- 35.McDonald DA, Pape J, eds. Cost Recovery and the Crisis of Service Delivery in South Africa. London, UK: Zed Books; 2002.
- 36.Breslin ED. Lessons from the field: rethinking community management for sustainability. Paper presented at: Rural and Peri-Urban Water Supply and Sanitation in South Africa—Appropriate Practices Conference; March 14–19, 1999; East London, South Africa.
- 37.McCoy D, Saitowitz R, Saasa M, et al. An Evaluation of South Africa’s Primary School Nutrition Programme. Dur-ban, South Africa: Health Systems Trust; 1998.
- 38.Swart R, Sanders D. Evaluating the Primary School Nutrition Programme as a Vehicle for Nutrition Education in South Africa. Western Cape, South Africa: University of the Western Cape; 1998.
- 39.Schneider H, Stein J. Implementing AIDS policy in post-apartheid South Africa. Soc Sci Med. 2001;52:723–731. [DOI] [PubMed] [Google Scholar]
- 40.McCoy D, Besser M, Visser R, Do-herty T. Interim Findings on the National PMTCT Pilot Sites. Durban, South Africa: Health Systems Trust; 2002.
- 41.Zwarenstein M, Schoeman JH, Vundule C, Lombard CJ, Tatley M. Randomised controlled trial of self-supervised and directly observed treatment of tuberculosis. Lancet. 1998;352: 1340–1343. [DOI] [PubMed] [Google Scholar]
- 42.Ashworth A, Chopra M, McCoy D, et al. WHO guidelines for management of severe malnutrition in rural South Af-rican hospitals: effect on case fatality and the influence of operational factors. Lancet. 2004;4;363:1110–1115. [DOI] [PubMed] [Google Scholar]
- 43.Victora CG, Wagstaff A, Schellen-berg JA, Claesen M, Habicht JP. Applying an equity lens to child health and mortality: more of the same is not enough. Lancet. 2003;362:233–241. [DOI] [PubMed] [Google Scholar]
- 44.Gillespie S, Mason J, Martorell R. How Nutrition Improves. Geneva, Switz-erland: United Nations Administrative Committee on Coordination/SubCommittee on Nutrition; 1996
- 45.Sanders D, Chopra M. Integrated comprehensive health care in developing countries Int J Integrated Care. 2001; 3:258–268. [Google Scholar]
- 46.McCoy D, Bambas L, Acurio D, et al. Global Equity Gauge Alliance: reflections on early experiences. J Health Popul Nutr. 2003;21:273–287. [PubMed] [Google Scholar]
- 47.Reagon G, Scott V, Tyler P. Primary health care expenditures across Cape Town. Cape Town, South Africa: University of the Western Cape.
- 48.Tudor Hart J. Commentary: three decades of the inverse care law. BMJ. 2000;320:18–19. [PubMed] [Google Scholar]
- 49.Johnson B, Chopra M. Evaluation of a Primary Education Programme to Combat Worm Infestation in Khayelitsha, Cape Town. Cape Town, South Africa: Medical Research Council; 2002.
- 50.Stern R, Mokgatle MJ. The Acceptability of Dry Sanitation: A Preliminary Study in Two Informal Settlements in Khayelitsha, Cape Town. Cape Town, South Africa; University of Western Cape, Cape Town Equity Gauge; 2004.