Abstract
Objectives. We evaluated the World Health Organization’s rapid assessment and response (RAR) method of assessing injection drug use and its associated health problems, focusing on knowledge gain, capacity building, and whether RAR leads to the development of interventions reducing the health effects of injection drug use.
Methods. Data were derived from RAR studies conducted in Beijing, China; Bogotá, Colombia; Greater Rosario, Argentina; Hanoi, Vietnam; Kharkiv, Ukraine; Minsk, Belarus; Nairobi, Kenya; Penang, Malaysia; St. Petersburg, Russia; and Tehran, Iran.
Results. Substantial gains in knowledge and response capacity were reported at all of the study sites. Before RAR initiation, prevention and intervention programs had been absent or inadequate at most of the sites. The RARs resulted in many new or modified interventions; 7 sites reported 24 health-related interventions that were subsequently developed and influenced by the RARs.
Conclusions. RARs, which require relatively little external funding, appear to be effective in linking assessment to development of appropriate interventions. The present results add to the evidence that rapid assessment is an important public health tool.
Rapid assessment is a practical public health tool for use in investigating problems in areas in which policymakers, planners, and practitioners need to make decisions in contexts of limited resources and in which conventional social science and public health assessment methods are inappropriate.1–6 Rapid assessments have been used in fields as diverse as nutrition,5,7 reproductive health, water hygiene,8 environmental disasters,9 and HIV/AIDS.10 Some are undertaken to raise awareness of public health problems, whereas others are oriented toward planning, developing, and implementing public health programs and projects.
The rapid assessment approach is characterized by speed and the use of multiple methods (including analysis of existing data, key informant interviews, focus groups, observations, mapping, and population estimation) and multiple data sources. Rapid assessment promotes an investigative orientation—involving data triangulation and inductive modes of analysis—and multilevel evaluations of the ways in which health problems are influenced at the individual, community, and structural levels.10,11 The method is designed to ensure that responses are strengthened through community involvement.
Rapid assessments are widely used in investigating drug problems.12–16 Rapid assessment guidelines for substance use17 have been issued by the World Health Organization (WHO), the Joint United Nations Programme on HIV/AIDS, the United Nations Children’s Fund, the United Nations International Drug Control Programme,18,19 the US Office of HIV/AIDS Policy, Médecins Sans Frontières of Holland (MSF-H), the United Nations Development Programme, and the International HIV/AIDS Alliance. Most rapid assessment guides and reports remain in the unpublished literature.17
In 1998, the WHO rapid assessment initiatives were relabeled rapid assessment and response (RAR) to highlight the link between the assessment of and the development of health-related interventions. The emphasis is not on knowledge gain per se but on how knowledge is used in improving public health responses. Thus, along with guidance on assessment methods, the WHO RAR guides include information on community participation, capacity building, advocacy, methods of formulating recommendations, and ways to develop and plan interventions. They also include basic information on prevention, harm reduction, and treatment interventions.20–22
RARs on injection drug use (IDU) typically involve profiling the study area and the context of IDU in that area and then assessing the populations and settings at risk, drug use patterns and health risk behaviors, health and social issues linked to IDU, and interventions currently available. These RARs typically result in action plans involving recommendations for new or modified interventions.
A recent review showed that at least 83 rapid assessment studies on substance use, involving 322 different sites in 70 countries, were undertaken in the period 1993 through 2001.23 The largest study—conducted in the Russian Federation—involved the MSF-H program focusing on HIV/AIDS prevention among injection drug users; in this program, 200 health professionals from 61 cities underwent training in rapid assessment and HIV prevention, resulting in 63 rapid assessments.24 Another multisite RAR was the US Rapid Assessment, Rapid Response, and Evaluation (RARE) study, which focused on HIV/AIDS in African American and Hispanic communities.25
The proliferation of rapid assessment work in the substance use field26,27 has not been matched by evaluations of the method,28–30 and there has been considerable debate about evaluation criteria.30–35 In our view, it is necessary to judge the RAR approach in terms of both methodological adequacy and whether the approach leads to relevant public health interventions. We chose to focus on the latter issue, undertaking a prospective evaluation of RAR studies on IDU as part of the WHO Phase II Drug Injection Study.
METHODS
Because, in the case of IDU, one of the issues was whether RAR would be feasible in different settings, staff from the WHO Phase II Drug Injection Study selected sites in low- and middle-income countries to reflect different global regions with emerging or established IDU populations and differing levels of awareness of and readiness to respond to health issues related to IDU. Local principal investigators were contracted to undertake RARs to facilitate the development of projects designed to prevent IDU-related HIV infection and other adverse health consequences.
Ten sites (Beijing, China; Bogotá, Colombia; Greater Rosario, Argentina; Hanoi, Vietnam; Kharkiv, Ukraine; Minsk, Belarus; Nairobi, Kenya; Penang, Malaysia; St. Petersburg, Russia; and Tehran, Iran) conducted RARs using the WHO IDU-RAR guide.36 Technical support was provided by the Centre for Research on Drugs and Health Behaviour (CRDHB) and WHO. The study was naturalistic and prospective in design: Teams adapted the RAR method as needed, with minimal direction from CRDHB or WHO, and information was collected prospectively. RARs were conducted between November 2000 and September 2002. All sites established community advisory boards and used multiple methods, including analysis of existing data and interviews conducted with key informants. Sites were not allocated a budget for intervention development.
The component of the evaluation study described here focused on detailing the outcomes of the RARs; in a future report, we will describe the methods used by the teams. Outcomes evaluated included generation of relevant local knowledge, capacity building, and whether HIV prevention and other health-related interventions were developed. An intervention was defined as an activity designed to bring about improvements in the health of IDU populations by facilitating changes in individual risk behaviors, changes in community responses and norms, or structural changes (e.g., changes in policies or laws). We included in our assessment new interventions as well as existing ones in which changes had been instituted.
We used 3 data sources in our evaluation. First, we obtained the RAR reports from each site, which were between 35 and 200 pages in length and were written by the principal investigator and the research team. They included descriptions of country and city contexts, methods used, and findings and recommendations.
Our second data source was the questionnaires completed by the principal investigators. Questionnaire 1, completed immediately before the initiation of the RAR, included questions on the principal investigators’ perceptions of the “baseline” situation regarding injection drug users and the health issues associated with IDU. Questionnaire 2, completed when the RAR report was submitted, included questions on principal investigators’ views about the knowledge that had been gained and the interventions that had been developed during the RAR. Questionnaire 3, completed 9 to 12 months after the RAR report had been submitted, requested information on subsequent activities, including capacity building and intervention development.
Third, we obtained data from communications with the principal investigators, including e-mails, telephone conversations, and personal meetings, and from materials related to the interventions such as leaflets and photographs. Data were quantified or subjected to thematic analyses (e.g., extracts from RAR reports). Findings were assessed by the principal investigators to ensure their accuracy. The present study included information received and analyzed up to November 2002.
RESULTS
Knowledge Gain
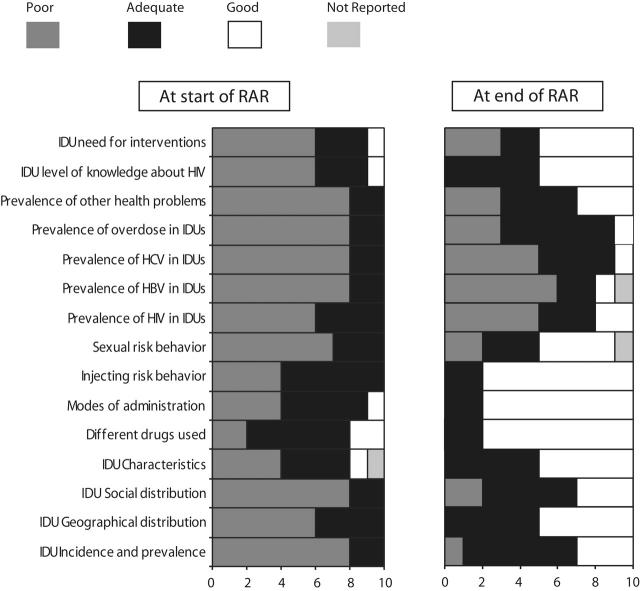
At baseline (as assessed via questionnaire 1), most of the principal investigators rated the information available at their sites on the 15 domains shown in Figure 1 ▶ as poor, with the exception of knowledge of different drugs used and modes of drug administration, characteristics of drug users, and risk behaviors. Figure 1 ▶ shows that principal investigators were reporting substantial gains in knowledge by the end of the RAR (questionnaire 2); at that point, each principal investigator reported that information was adequate or good in all domains, with the exception of prevalence rates of HIV, hepatitis C virus, and hepatitis B virus. (Information on blood-borne viruses was collected in a structured survey conducted after the RAR.)
FIGURE 1—
Principal investigators’ ratings of levels of knowledge about injection drug users (IDUs) at initiation and end of rapid assessment and response (RAR).
Note. HBV = hepatitis B virus. At the Minsk site, data on time 1 characteristics of IDUs and on time 2 sexual risk behaviors were missing; at the Beijing site, data on time 2 prevalence of hepatitis C virus (HCV) infection were missing.
Most principal investigators commented on the significance of the RAR in terms of gaining more detailed information and overcoming anecdotal impressions about drug use. In the words of one principal investigator: “For the first time, we have received a broader spectrum of data on injecting drug use.” Another investigator pointed out that the study represented the first instance in which the actual existence of IDU had been documented in the capital and other major towns and cities.
In questionnaire 2, principal investigators were asked to describe 3 examples of knowledge gain and provide reasons why this information was important (Table 1 ▶). The primary reasons mentioned focused on drug use and risk behaviors, including new trends in drug use, drug-using practices, and risk behaviors; knowledge about injection drug users’ sexual behaviors; injection drug users’ lack of knowledge about risky behaviors, blood-borne viruses, and other health problems (e.g., overdose); and lack of or inadequacy of services for injection drug users.
TABLE 1—
New Information About Injection Drug Users Produced by RARs and How or Why It Was Useful: WHO Phase II Drug Injection Study, 2000–2002
| Site | Information Type/Description | How or Why Information Was Useful |
| Beijing | New information on initiation of drug use | Important for health education and prevention messages |
| Lack of support structures for non–drug-using partners of heroin users | Non–drug-using partners leave the relationship or start to use drugs themselves | |
| Fear of becoming infected with HIV has led police and doctors to turn away HIV-positive drug users from detoxification and voluntary treatment centers without HIV counseling | Implications for HIV surveillance in Beijing and possibly in other provinces where similar practices may be occurring | |
| Bogotá | IDU is an expanding type of drug use and is fashionable in some social settings | Need to develop policies and actions to prevent transition to IDU and address the risks involved in IDU |
| Inexperience and lack of tradition of injection, lack of information about safe injection practices and risks of indirect sharing of paraphernalia | Need to develop educational and preventive strategies addressing specific problems and gaps in information levels and risk perceptions of injection drug users | |
| The complete lack of specific actions to prevent health problems in drug-using and drug-injecting populations | Need to develop programs and actions in the middle term to reduce the adverse health consequences of IDU | |
| Greater Rosario | Existence of shooting galleries that had never before been reported | Important contact living in a shooting house collaborated in planning interventions |
| Drugs and poverty, especially use of free base cocaine and glue in marginal populations and diffusion of free base made in domestic kitchens | Materials developed in collaboration with community advisory board to access shantytown population; problems with the law and police indicated need to produce information about drug users’ rights | |
| Lack of interventions addressing IDU | Development of “Let’s Reduce Risks—Condoms and Syringes” campaign, funded by Regional AIDS Program and implemented by National University of Rosario in collaboration with community advisory board | |
| Hanoi | Mapping of drug use | Helped reach injection drug users and locate interventions |
| Sexual risk behaviors of injection drug users and their sexual partners | More known about IDU sexual networks and drug use among female sex workers; helped explain the dynamics of HIV transmission from injection drug users to female sex workers and other populations | |
| Information on available services and interventions for drug users | Showed policymakers that current interventions were insufficient to reduce/stop IDU and HIV transmission and other health consequences; more intensive harm reduction activities needed | |
| Kharkiv | Information about prevalence and spread of IDU and users’ enrollment in treatment programs | . . . a |
| Information about incidence and details of overdoses occurring among injection drug users | ||
| New information about equipment and medicines used to prepare narcotics at home | ||
| Minsk | Users often inject in places with no free access to running water (e.g., in a car, on a staircase) | . . . a |
| Risky injecting behaviors are less common among clients of syringe exchange outlets | ||
| Injection drug users are reluctant to call an ambulance in fear of possible legal consequences | ||
| Nairobi | Widespread and well-established injecting | IDU may have a role in heterosexual spread of HIV perinatally and to individuals who are not injection drug users; need for further investigations to determine contribution of injection drug users to prevalence of HIV and viral hepatitis |
| Multiperson use of needles and syringes and unprotected sexual intercourse with multiple partners | ||
| Heroin is easily available in the streets of Nairobi. Kenyan international airports and seaports serve as trans-shipment points for heroin and other drugs destined for markets in the West | RAR revealed that despite the existence of antinarcotics unit, drugs spill over into the local market | |
| Penang | How addicts add or mix substances together with heroin to inject | . . . a |
| Addicts had almost no knowledge about hepatitis B and C infections | ||
| Addicts perceive that only sharing needles is risky. They continue to share other injecting paraphernalia | ||
| St. Petersburg | Behavioral risk among injection drug users is more dangerous than we anticipated | Important to prepare prevention programs |
| Injection drug users obtain narcological services from hospital of infectious diseases | Important to consider need for adequate services | |
| An outbreak of overdose; injection drug users obtain emergency treatment at city hospitals, but death rates are high; treatment duration is only 1 day | Important to develop standards for services when overdose occurs | |
| Tehran | Factors negatively influencing injection drug users’ access to sterile needles | Introduction of pilot intervention in districts with high prevalences of needle sharing |
| Existing training, supportive, and treatment facilities | Facilities available for injection drug users much lower than expected; lobbying of appropriate authorities in response | |
| High prevalence of drug overdose and feeble management by health services; death because of insufficient management not uncommon | Issue not adequately dealt with in past; secondary data from intoxication and forensic medicine centers unreliable; health centers and facilities inadequately equipped; determination being made of how to push for improvements in services |
Note. RAR = rapid assessment and response; IDU = injection drug use. Data were derived from principal investigators’ reports.
a No response.
Capacity Building
Capacity building was defined as increases in a site’s ability to respond stemming from new links, new knowledge, and new skills obtained from carrying out RARs. In questionnaire 3, all principal investigators reported that they had established new links at the city level with individuals, agencies, or institutions; 8 reported that they had developed new national and international links (in addition to those formed as part of the study collaboration); and 4 had developed new regional links. These linkages reportedly led to better collaboration and to initiation of new types of responses to IDU and HIV.
For example, a harm reduction program to provide outreach, needles and syringes, information on safe disposal of drug supplies, and access to health care services to residents of shantytowns was developed in marginal areas of the Greater Rosario belt. This project was developed in collaboration with the Ministry of Health (which provided syringes and salaries) and the Regional AIDS Programme (which provided condoms); the RAR group provided training, and the national harm reduction network coordinated this training. The data in Table 2 ▶ show that principal investigators assigned a mean rating of 4.0 (out of a possible 5) to the importance of contacts made during the RAR to the development of interventions.
TABLE 2—
Development of Responses and Interventions Linked to RARs: WHO Phase II Drug Injection Study, 2000–2002
| Site | Intervention Type | Intervention Description | Funder/Other Input | Principal Investigator Data Ratinga | Principal Investigator Contact Ratingb |
| Beijing | None | ||||
| Bogotá | Education and prevention | Information about risks for injection drug users | WHO; Canadian government | 5 | 1 |
| Policy and strategy | Inclusion of injection drug users in national drug plan | US Embassy | 2 | 1 | |
| Training | Training of professionals in the area of injection drug use | Programa Presidencial para Afrontar el Consumo de Drogas; British Council | 3 | 1 | |
| Greater Rosario | Harm reduction | Education campaign: syringes and condoms | Ministry of Health; National University of Rosario; Argentinean Harm Reduction Association | 5 | 5 |
| Harm reduction | Harm reduction program in shantytowns | Ministry of Health; Regional AIDS Programme; Argentinean Harm Reduction Association | 4 | 5 | |
| Hanoi | Training | Training in peer intervention harm reduction (needles, condoms) | German–Vietnam Technical Cooperation | 3 | 3 |
| Kharkiv | Research | Intervention coverage | UNICEF | 5 | 5 |
| Counseling | Establishment of network of counseling centers | UNICEF; State Centre for Youth Social Services; local budgets | 5 | 5 | |
| Advocacy | Development of network to provide support to HIV/AIDS agencies | British Council; European Commission | 5 | 5 | |
| Minsk | Counseling | Assistance to HIV-positive individuals | . . . c | 4 | 5 |
| Rehabilitation | Rehabilitation centers for injection drug users | . . . c | 4 | 4 | |
| Treatment | Pilot substitution project | . . . c | 5 | 5 | |
| Harm reduction | Establishment of a network of outreach workers and volunteers | . . . c | 5 | 5 | |
| Harm reduction | Expansion of the network of syringe exchange outlets | . . . c | 5 | 5 | |
| Nairobi | None | ||||
| Penang | None | ||||
| St. Petersburg | Research | Referrals/treatment links between outpatient and inpatient facilities | Switzerland | 5 | 5 |
| Treatment | Treatment for drug problems | Switzerland | 5 | 5 | |
| Health care | Integration of drug users into existing state health care services | Family Health International | 5 | 5 | |
| Training | Training of psychologists in counseling in infectious disease units | Norwegian Church Aid | 5 | 5 | |
| Tehran | Policy and strategy | Establishment of “National Committee on Harm Reduction” at Ministry of Health; preparation of “National Harm Reduction Action Plan” | 3 | 3 | |
| Treatment | Methadone programs in outpatient clinics | . . . c | 2 | 3 | |
| Research | Drug use RAR in prisons | . . . c | 4 | 3 | |
| Harm reduction | Harm reduction programs in prisons | . . . c | 2 | 2 | |
| Harm reduction | Guidelines on pharmacy sales of syringes | . . . c | 5 | 5 | |
| Training | Harm reduction training for health workers and pharmacists | . . . c | 3 | 3 |
Note. RAR = rapid assessment and response. The data presented here were reported during the 9–12-month period after the RAR. The total number of interventions was 24.
aPrincipal investigator’s rating (on a 1–5 scale) of the extent to which RAR data assisted in response development (mean rating: 4.1).
bPrincipal investigator’s rating (on a 1–5 scale) of the extent to which contacts made during the RAR assisted in response development (mean rating: 4.0).
cNot reported.
Each of the principal investigators reported that conducting the rapid assessment led to an increase in the capacity for research and assessment on the part of the RAR team, the community advisory board, and others (government, nongovernmental organizations, and community-based organizations), including a greater ability to contact and interview “hard-to-reach” populations such as injection drug users about whom little information was available. The teams also reported increases in the areas of knowledge of and capacity for using different research methods, dissemination of findings and recommendations, community participation (especially through linking with populations of drug users and with other organizations), use of data for advocacy with local and national governments and funding agencies, and development of interventions.
Recommendations for Interventions
All teams formulated specific and grounded recommendations in their RAR reports for interventions designed to reduce IDU-related health risks. Common recommendations were as follows: institution of policy changes enabling interventions to be introduced, initiation of information and education projects, improvements in primary prevention and health promotion, establishment of additional professional training and research opportunities, and initiation of specific harm reduction interventions and treatment and rehabilitation for injection drug users.
All RAR reports identified target groups such as injection drug users and drug users in treatment and in the community, drug users who had been tested for HIV, partners of drug users, female drug users, drug dealers, homeless drug users, prisoners, parents of drug users, young people, teachers, doctors and health care professionals, journalists, staff members of nongovernmental organizations, law enforcement personnel, social workers, and religious organizations. Each study team made recommendations that addressed drug and HIV problems at a number of levels, for example, promoting outreach to injection drug users and advocating for policy changes that would enable such outreach to take place.
Reports varied in terms of evidence of strategic thinking. Some indicated that recommendations were unlikely to be implemented unless obstacles were removed. Constraints identified included legislation (e.g., restrictions on the establishment or operations of nongovernmental organizations or on provision of methadone), lack of financial or human resources, and the failure of authorities to recognize the nature and seriousness of the IDU problem. One report recommended the introduction of methadone treatment but noted that legal changes would be required to do so and thus rated the plan’s acceptability and feasibility as “low.” Another team noted that although outreach and information programs were theoretically feasible, “avoiding barriers and guaranteeing the continuity of actions is not easy given the scarcity of resources and the crisis within the health sector.”
Interventions Developed and Implemented
The ultimate test was whether the sites could develop the interventions recommended. Nine to 12 months after completion of the RARs, principal investigators from 7 sites reported on a total of 24 interventions that had been implemented or modified and that had been informed by the RAR. Table 2 ▶ shows the types of interventions developed. The majority of projects were funded externally. Overall, principal investigators assigned a mean rating of 4.1 (out of a possible 5) to the extent that RAR data contributed to the development of each intervention.
Some of the projects focused on the training of generic and specialist staff members. In St. Petersburg, for example, a project was implemented to develop a psychological services center in the city’s infectious diseases hospital. The goal of this project was to train psychologists from other hospitals in HIV pretest and posttest voluntary counseling. New services implemented for injection drug users included substitution treatment; for example, the ministries of health care and internal affairs in Belarus approved a substitution treatment pilot project for opioid-dependent injection drug users in Minsk, and several methadone programs were initiated in outpatient drug treatment clinics in Tehran. Many sites developed harm reduction initiatives by providing syringes and condoms and engaging in outreach activities; in Greater Rosario, for instance, the discovery of shooting galleries led to a peer-based intervention in collaboration with a key informant living in a house where there was such a gallery.
Some interventions focused on education and prevention among injection drug users and those at risk of injecting through targeted interventions in high-risk locations, delivered through peer intervention and outreach programs involving outreach workers and volunteers. Other projects focused on policy and strategy. For example, in Colombia there had been little interest in IDU, and therefore in Bogotá the RAR helped to ensure that this issue was addressed in national policies, strategies, and actions of the national drug program.
Some of the projects were new; others were modified after the RAR. In Hanoi, for instance, the RAR helped strengthen peer education and harm reduction projects for injection drug users, adding 7 peer education groups in “hot districts” of the city, increasing the overall number of groups to 19.
RAR teams also helped develop advocacy and networking projects designed to promote IDU issues in health care agencies, provide interagency support, and help increase access to care in existing health services. For example, the Kharkiv team developed an advocacy project to help change the attitudes of local authorities toward IDU, develop cooperation between organizations and agencies, and support projects focusing on HIV and drug use prevention.
At 2 sites, the RAR contributed to the development of further research. In St. Petersburg, an additional research project sought to improve the quality of health care provided to drug users in existing state health services. In Kharkiv, new research was conducted to estimate the numbers of injection drug users in 2 other cities, identify organizations involved in HIV prevention among injection drug users, analyze possibilities for extending HIV prevention, and reach a politically acceptable decision to continue prevention activities at the local level.
DISCUSSION
Limitations in the design of our study warrant some caution. This study was conceived as an “uncontrolled” investigation relying on reports from program participants. However, the principal investigators offered candid and critical comments about difficulties in conducting RARs and the limitations of their work.
Data sources were limited, and the evaluation itself—in the spirit of RAR—was conducted at low cost, with a total budget of approximately $60 000. Bias was possible on the part of the evaluation team because the evaluators had also been responsible for developing RAR guides. Finally, the RARs assessed in this study may not be typical of others. They were not always rapid, and some teams were overambitious. Most were led by principal investigators with experience (to a greater or lesser extent) in social science research but rarely in multimethod research. Most teams had previous knowledge of and experience with drug and HIV issues.
Knowledge Gain, Capacity Building, and Intervention Planning
What we now know is that, in practice, undertaking an RAR is itself part of the intervention process. RARs led to substantial reported gains in knowledge about local conditions, and in their reports the teams were enthusiastic about their new knowledge: There was a sense of discovery in the way evidence was reported. This was especially the case in instances in which the research staff, health and welfare personnel, and government personnel were unknowledgeable about and unaccustomed to direct contact with injection drug users. RARs helped to de-mystify and reduce fear of injection drug users and demonstrated that they could be contacted in the community—itself a precursor to outreach for HIV prevention and health promotion. RARs also demonstrated to the target populations that someone was interested in their health and welfare. Thus, as well as being an investigative method, RARs pave the way for interventions.
RARs also enhance response capacity. Undertaking RARs helps develop knowledge and skills and provides new links to individuals and agencies, in turn facilitating intervention development. This process appears to take place because RARs emphasize community and organizational involvement and because the practical need to collect information from a wide range of sources quickly brings the team into contact with many organizations and individuals, again indicating how RARs are part of the intervention process.
A third way in which RARs can be considered a component of the intervention process is that they encourage teams to consider what needs to be done to reduce harm and improve health. In undertaking RARs, principal investigators and teams learn how to analyze problems from a public health perspective.
All teams used the knowledge gained to recommend a range of activities designed to reduce IDU-related harms. The recommendations were not “formulaic” but were relevant to local contexts. In the words of 1 of the principal investigators, RARs allowed the creation of prevention materials on the basis of “local realities and language.” Thus, recommendations were grounded in both the data and the analysis.
Interventions Implemented
The final test is whether RARs lead to practical changes that aid the target population; in other words, are they a vehicle for implementing public health responses? Projects develop through complex stages from the initial idea to formulation of proposals, acquisition of funding, and establishment of the intervention itself. A major challenge in the present case was that WHO funding did not include intervention development, and thus, part of the “test” was whether teams could convince funders of the merits of the case for helping injection drug users. Seven sites reported on a total of 24 interventions that had been developed and were informed by the RARs within 9 to 12 months after their completion. These interventions represented a good return on the WHO RAR investment of approximately $10 000 per site. Thus, the results of the present study add to evidence from elsewhere suggesting that rapid assessments indeed aid development of interventions.
For example, the MSF-H Russian project led to 34 HIV prevention programs, including needle exchange programs, outreach and group education, health promotion materials, treatment referral systems, and provision of medical services.24 The RARE program produced new knowledge that was highly relevant to local intervention development aimed at preventing HIV infection.25 Our review of 83 rapid assessment reports revealed that half were followed by interventions relevant to the target group, such as workshops, training, policy changes, involvement of the community in intervention development, network building, and specific medical and nonmedical interventions.23
It would be unwise to assume that the RARs were solely responsible for the interventions developed. Undoubtedly, interventions had already been under consideration at many sites (as in Greater Rosario), some sites were at the stage of response readiness, and other sites used the RARs to help them modify existing projects (as in Hanoi). However, principal investigators believed that the RAR data gathered and contacts made during the rapid assessment were significant in the development of projects. All reported that existing projects were enlarged or new ones initiated after the completion of the RAR. Finally, many of the projects involved collaboration between agencies, confirming the views of the principal investigators about the importance of the links that had been established during the RARs.
At 3 sites, interventions had not been implemented by 9 to 12 months after the RAR. In 1 case, the problems were a lack of government awareness and readiness to respond and competing health and economic difficulties. It may therefore be unfair to judge an RAR only according to whether interventions are developed, that is, without considering the relationship of the RAR to national and local response readiness. The site that reported no interventions did in fact have an impact on the national drug policy, and thus, the RAR played a role in the first stage of policy change. At another site, the reason for the lack of intervention development might have been that most of the study team members were from a research institute involved in large-scale, long-term interventions. Two of the sites where interventions had not yet occurred had pipeline projects.
RARs do not operate in a vacuum, and there are many factors beyond the control of research teams that affect the likelihood of recommendations being adopted and translated into interventions and influence the long-term sustainability of interventions. Not the least of these issues are a country’s economic and social conditions and the fact that, in many nongovernmental organizations and funding agencies, drug prevention may be more of a priority than harm reduction. In some countries, public opinion is antipathetic toward injection drug users, and government policies do not address the needs of this population to any significant degree. It is unrealistic to expect RARs to always be successful given that their scale is relatively small in the face of considerable obstacles. What is apparent, however, is that in many cases rather small amounts of money can lead to implementation of innovative and much-needed interventions. Our findings add to the growing evidence on the role of rapid assessment as a practical public health intervention.
Acknowledgments
This article was based on the participation by the authors in the WHO Phase II Drug Injection Study, coordinated and sponsored by WHO with financial support from the Joint United Nations Programme on HIV/AIDS. The study was implemented by the WHO Phase II Drug Injection Collaborative Study Group, which includes Moruf Adelekan, Queen’s Park Hospital, Blackburn, England; Francisco Inacio Bastos, Oswaldo Cruz Foundation, Rio de Janeiro, Brazil; Kachit Choopanya and Suphak Vanichseni, Bangkok Metropolitan Administration and Bangkok AIDS Vaccine Evaluation Groups, Bangkok, Thailand; Don Des Jarlais and Theresa Perlis, National Development and Research Institutes Inc, New York, NY; Nguyen Tran Hien and Dao Thi Minh An, Hanoi Medical University, Hanoi, Vietnam; Sylvia Inchaurraga, Universidad Nacional de Rosario, Rosario, Argentina; Rahim Lawal, University of Ilorin Teaching Hospital, Ilorin, Kwara State, Nigeria; Maristela Monteiro, World Health Organization, Geneva, Switzerland; Visum Navaratnam and Vicknasingam B. Kasinather, University of Sains Malaysia, Penang, Malaysia; Augusto Perez Gomez and Ines Elvira Mejia, Programa Presidencial para Afrontar el Consumo de Drogas, Bogotá, Colombia; Fabio Mesquita, Faculdade de Medicina da Universidad de Sao Paulo, Santos, Brazil; Sergey Molochko, Minsk City Narcological Dispensary, and Yauhenia Kechyna, Belarussian State University, Minsk, Belarus; Maurice Odek-Ogunde, United States International University, Nairobi, Kenya; Dimitry Ostrovsky, Foundation “Vozvrastcheniye,” St. Petersburg, Russia; Vladimir Poznyak, World Health Organization, Geneva, Switzerland; Emran Razzaghi, Tehran University of Medical Sciences, and Afarin Rahimi, National Research Centre for Medical Sciences, Tehran, Iran; Gerry Stimson and Chris Fitch, Imperial College London, London, England; Olga Balakireva and Marina Varban, Ukrainian Institute for Social Research, Kiev, Ukraine; and Zunyou Wu and Lorraine Yap, Chinese Academy of Preventive Medicine, Beijing, China. Site reports are available from WHO.
Thanks to Katherine Keetley for editorial assistance.
Note. The authors are responsible for the views expressed in this article, which do not necessarily represent the views of the other investigators participating in the WHO Phase II Drug Injection Study or the views or policies of the World Health Organization.
Human Participant Protection Each site was responsible for the ethical review of its RAR and provided the best fit between human participant protection and national standards and concerns.
Peer Reviewed
Contributors G. V. Stimson, D. Des Jarlais, V. Poznyak, T. Perlis, and the WHO Phase II Drug Injection Collaborative Study Group originated the WHO Phase II Drug Injection Study. Overall coordination was provided by V. Poznyak; G. V. Stimson and C. Fitch coordinated the RAR component and provided technical support to study sites. G. V. Stimson designed the evaluation with the assistance of C. Fitch. C. Fitch was responsible for data collection and day-to-day liaison with RAR principal investigators. G. V. Stimson undertook the analysis of the data with the assistance of E. Oppenheimer. G. V. Stimson and E. Oppenheimer wrote the first draft with later input from all other authors. G. V. Stimson wrote the final draft with input from all other authors. T. Rhodes assisted with development of the RAR method.
References
- 1.Manderson L. Population and Reproductive Health Programmes: Applying Rapid Anthropological Assessment Procedures. New York, NY: United Nations Population Fund; 1996.
- 2.Rhoades E. The coming revolution in methods for rural development research. In: Scrimshaw NS, Gleason GR, eds. Rapid Assessment Procedures: Qualitative Methodologies for Planning and Evaluation of Health Related Programmes. Boston, Mass: International Nutrition Foundation for Developing Countries; 1992:60–78.
- 3.Chambers R. Rapid Rural Appraisal: Rationale and Repertoire. Sussex, England: Institute for Development Studies; 1980. Discussion paper 155.
- 4.Unwin N, Aspray TJ. Quick decision? Fast track data for health policy. Available at: http://www.id21.org/insights/insights-h01/index.html. Accessed November 17, 2003.
- 5.Field Guide on Rapid Nutritional Assessment in Emergencies. Geneva, Switzerland: World Health Organization; 1995.
- 6.Larson A, Manderson L. Contextual Assessment Procedures for STDs and HIV/AIDS Prevention Programmes: A Manual. Brisbane, Queensland, Australia: Australian Centre for International and Tropical Health and Nutrition; 1997.
- 7.Scrimshaw SCM, Hurtado E. Rapid Assessment Procedures for Nutrition and Primary Health Care. Tokyo, Japan: United Nations University; 1987.
- 8.Almedon AM, Blumenthal U, Manderson L. Hygiene Evaluation Procedures. Boston, Mass: International Nutrition Foundation for Developing Countries; 1997.
- 9.Glass RI, Noji EK. Epidemiologic surveillance following disasters. In: Halperin WE, Baker EL, Monson RR, eds. Public Health Surveillance. New York, NY: Van Nostrand Reinhold; 1992:195–205.
- 10.Fitch C, Rhodes T, Stimson GV. Origins of an epidemic: the methodological and political emergence of rapid assessment. Int J Drug Policy. 2000;11(1–2): 63–82. [DOI] [PubMed] [Google Scholar]
- 11.Stimson GV, Fitch C, Rhodes T, Ball A. Rapid assessment and response: methods for developing public health responses to drug problems. Drug Alcohol Rev. 1999;18:317–325. [Google Scholar]
- 12.Rhodes T, Stimson GV, Fitch C, Ball A, Renton A. Rapid assessment, injecting drug use, and public health. Lancet. 1999;354:65–68. [DOI] [PubMed] [Google Scholar]
- 13.Dorabjee J, Samson L. A multi-centre rapid assessment of injecting drug use in India. Int J Drug Policy. 2000;11(1–2):99–112. [DOI] [PubMed] [Google Scholar]
- 14.De Jong W, Tsagarelli T, Schouten E. Rapid assessment of injection drug use and HIV in the Republic of Georgia. J Drug Issues. 1999;29:843–860. [Google Scholar]
- 15.Kumar MS, Mudaliar S, Thyagarajan SP, Kumar S, Selvanayagam A, Daniels D. Rapid assessment and response to injecting drug use in Madras, South India. Int J Drug Policy. 2000;11(1–2):83–98. [DOI] [PubMed] [Google Scholar]
- 16.Mwenesi HA. Rapid assessment of drug abuse in Kenya. Bull Narc. 1996;48:65–78. [PubMed] [Google Scholar]
- 17.Fitch C, Stimson GV. RAR Review: An International Mapping and Retrospective Evaluation Study of Rapid Assessments Conducted on Drug Use. Geneva, Switzerland: World Health Organization; 2003.
- 18.Guidelines for Conducting a Rapid Assessment Study. Geneva, Switzerland: United Nations International Drug Control Programme; 1993.
- 19.Guidelines for the Development and Implementation of Drug Abuse Rapid Situation Assessments. Vienna, Austria: United Nations International Drug Control Programme; 1998.
- 20.Rhodes T, Fitch C, Stimson GV. The Rapid Assessment and Response Guide on Psychoactive Substance Use and Sexual Risk Behaviour. Geneva, Switzerland: World Health Organization; 2002.
- 21.Stimson GV, Fitch C, Rhodes T. The Rapid Assessment and Response Guide on Psychoactive Substance Use and Prevention. Geneva, Switzerland: World Health Organization; 1998.
- 22.Howard J, Rhodes T, Fitch C, Stimson GV. Rapid Assessment and Response Guide on Psychoactive Substance Use and Especially Vulnerable Young People (EVYP-RAR). Geneva, Switzerland: World Health Organization; 1998.
- 23.Fitch C, Stimson GV, Rhodes T, Vladimir Poznyak V. Rapid assessment: an international review of diffusion, practice and outcomes in the substance use field. Soc Sci Med. 2004;59:1819–1830. [DOI] [PubMed] [Google Scholar]
- 24.Burrows D, Trautmann F, Bijl M, Sarankov Y. Training in the Russian Federation on rapid assessment and response to HIV/AIDS among injecting drug users. J Drug Issues. 1999;29:811–842. [Google Scholar]
- 25.Needle RH, Trotter RT, Singer M, et al. Rapid assessment of the HIV/AIDS crisis in racial and ethnic minority communities: an approach for timely community interventions. Am J Public Health. 2003;93:970–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rhodes T, Fitch C, Stimson GV, Kumar S. Rapid assessment in the drugs field. Int J Drug Policy. 2000; 11(2):1–11. [DOI] [PubMed] [Google Scholar]
- 27.Fitch C, Rhodes T, Hope V, Stimson GV, Renton A. The role of rapid assessment methods in drug use epidemiology. Bull Narc. 2003;54:1–2. [Google Scholar]
- 28.McKeganey N. Rapid assessment: really useful knowledge or an argument for bad science? Int J Drug Policy. 2000;11(2):13–18. [Google Scholar]
- 29.Harris KJ, Jerome NW, Fawcett SB. Rapid assessment procedures: a review and critique. Hum Organ. 1997;56:375–377. [Google Scholar]
- 30.Friedman SR. What hath RAR wrought? Int J Drug Policy. 2000;11(2):37–39. [Google Scholar]
- 31.Ong BN. Assessing rapid assessment and response by the appropriate standards. Int J Drug Policy. 2000; 11(2):49–50. [Google Scholar]
- 32.Archibald CP, Sisushansian J, Jayaraman G, Sutherland D. RAR hath wrought . . . Hobson’s choice? Int J Drug Policy. 2000;11(2):41–44. [Google Scholar]
- 33.Manderson L. People before contestability. Int J Drug Policy. 2000;11(2):45–47. [Google Scholar]
- 34.Sarkar S. Rapid assessment and response: some lessons learnt in the South Asian context. Int J Drug Policy. 2000;11(2):51–54. [Google Scholar]
- 35.de Jong WM. The politics of rapid assessment and response. Int J Drug Policy. 2000;11(2):55–58. [Google Scholar]
- 36.Stimson GV, Fitch C, Rhodes T. The Rapid Assessment and Response Guide on Injecting Drug Use (IDU-RAR). Geneva, Switzerland: World Health Organization; 1998.