Abstract
The US health care system is struggling with a mismatch between the large, simple (low-information) financial flow and the complex (high-information) treatment of individual patients. Efforts to implement cost controls and industrial efficiency that are appropriate for repetitive tasks but not high-complexity tasks lead to poor quality of care.
Multiscale complex systems analysis suggests that an important step toward relieving this structural problem is a separation of responsibility for 2 distinct types of tasks: medical care of individual patients and prevention/population health. These distinct tasks require qualitatively different organizational structures. The current use of care providers and organizations for both purposes leads to compromises in organizational process that adversely affect the ability of health care organizations to provide either individual or prevention/population services.
Thus, the overall system can be dramatically improved by establishing 2 separate but linked systems with distinct organizational forms: (a) a high-efficiency system performing large-scale repetitive tasks such as screening tests, inoculations, and generic health care, and (b) a high-complexity system treating complex medical problems of individual patients.
THE STRUCTURE AND processes of the existing US health care system have been designed around the need to respond to the medical needs of a self-presenting individual. Widespread recognition of the importance of prevention and of population health1–3 has led to efforts to charge the health care system to respond to these needs. There is, however, limited recognition that imposing on the same organization the need to respond to such radically different tasks leads to ineffectiveness and inefficiency. Instead, it should be understood that a distinct system (or subsystem) that is well adapted to the task of prevention and population health services can be much more effective and efficient at those tasks and, by serving these needs, help to solve many of the existing difficulties of the health care system. Thus, the imperatives of public health, which are concerned with prevention and population health, may be better served by developing organizations that serve these needs directly.
This is an organizational approach to the separation of tasks rather than an approach based on questions of public or private financing or delivery. A precise analysis distinguishes tasks that are numerous and repetitive (and thus “large scale”) from those that are numerous and variable (and thus “fine scale” or “highly complex”). Distinct organizational structures are effective at these distinct types of tasks. Separating medical care for individual patients from preventive and population health services provides a first and important line of distinction between highly complex and large-scale health care services.
The concepts of scale and complexity can be used to analyze various aspects of organizational structure. A formal multi-scale analysis implies that for an organization to be effective, there must be a match between the scale and complexity of the functional capabilities of the organization and the scale and complexity of the tasks to be performed. My analysis implies that (1) the serial coupling of large-scale financial flows and complex medical decisionmaking is largely responsible for organizational turbulence and ineffectiveness in the health care system, and (2) Development of separate organizational forms for tasks at different scales is an essential step toward resolving the structural problems of the health care system and will both relieve the financial and organizational turbulence of the health care system and lead to greater effectiveness of complex medical care and large-scale prevention and population health services.
STRUCTURE OF THE HEALTH CARE SYSTEM
Today, it is widely understood that the health care system suffers from low quality and high medical error rates.4,5 Measures of the quality of care as a return on expenses4 and the incidence of medical errors5 depict a severely underperforming system despite the expansion of medical knowledge and the use of increasingly sophisticated technology and training.
Insight into the role of complexity and scale in the health care system can be gained by considering the role of insurance and the financial flows that exercise increasing control over the services provided. The development of health insurance and the trend toward managed care have affected the structure of the health care system in significant ways, separating the flow of money from the interaction between physician and patient. As is well known, the primary financial flow in health care consists of regular payments by employers (or, less often, individuals) to insurance companies, other health plans, or Medicare (or, through a variety of taxes, to Medicaid)—payments that are not directly dependent upon the actual services provided during the same time period. Practically speaking, the payment is often an electronic bank transfer once a month. Part of the money may be deducted from employee salaries, while the other part comes directly from the employer. Either way, the payment amounts are decided upon in advance and are the same from month to month until rate changes take place, typically on a yearly basis. With respect to the nature of the actual care provided, this sum is essentially featureless: large scale and simple, having no information encoded into it about the services it will eventually fund. The insurance company, managed care organization, Medicare, or Medicaid divides this large-scale flow of money into smaller financial flows allocated to medical costs.6
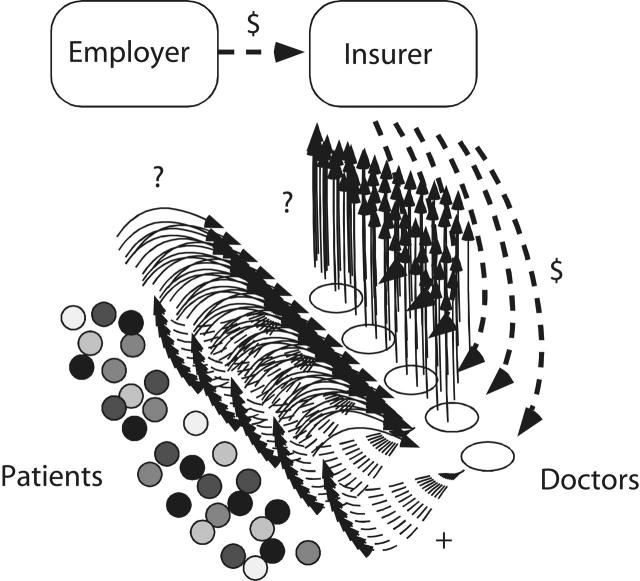
Figure 1 ▶ represents the flow of information, services, and money in the existing health care system. Information and medical care are exchanged in the transactions between physicians and patients, whereas the flow of money is largely from employers to health care insurers and thence to health care provider systems and individual practitioners. The difficulties in imposing efficiency and improving quality of care have their origins in the structure of these flows.
FIGURE 1—
The structure of the US health care system today.
Note. Information (?) flows from patient to physician. Care and information (+) flow back to the patient. Financial flows ($) proceed from employers (employer) to insurers (insurer; private or public) and thence to care providers (doctors), who provide to insurers information (?) about the care being provided to individual patients (patients). Insurers receive lump sum payments, which are distributed in much smaller amounts to care providers for specific services.
MULTISCALE ANALYSIS
Using recent fundamental advances in complex systems research,7,8 specifically multiscale analysis,9,10 we can identify the functional effectiveness of a system by comparing the set of actions a system can perform at different scales with the same analysis of its designated tasks. Here, scale refers not to size but to the redundancy, coherence, or coordination of a task. Large-scale tasks involve multiple individuals working as a coordinated unit, or multiple individuals performing the same task (e.g., mass immunizations). In contrast, fine-scale tasks involve the attention of a number of individuals each performing a unique task (e.g., one doctor diagnosing and treating an individual patient for a particular condition). To contrast 2 extreme possibilities, a system containing many individuals can be organized to perform a large number of unique (fine-scale) tasks, or a single large-scale task. This illustrates a fundamental trade-off in organizational structure and function.
There are more subtle tradeoffs that can be achieved in the organization of a system and the nature of the tasks that can be performed. These trade-offs can be characterized by the “complexity profile” of a system: the complexity of possible actions as a function of scale. This mathematical construct specifies the number of distinct tasks that can be performed at each scale. It can serve as an analytic tool to provide an understanding of the role of organizational structure in organizational effectiveness.
Multiscale analysis and the complexity profile9,10 decompose the capability of a system according to scale. They are an extension of information theory11,12 designed to capture the relationship between the set of possible behaviors of a system on the one hand and its interdependencies and communication channels on the other. The subject of this analysis is not the same as information asymmetry, incentive analysis, or game theoretic analysis.13–18 Instead, it is a new formalism that can characterize the function and desirability of organizational forms.19–24
In a sense, multiscale analysis is a generalization of statistical analysis that incorporates correlations of multiple variables rather than pairs of variables. Multiscale analysis considers the degree to which k-fold correlations between components of a system are present, where k ranges over the full set of values from 1 to N, the total number of components of the system. Correlations may be equivalently described by mutual information11,12 (when multiple variables are correlated, the same information can be obtained from measurements of any of the variables), and the multiscale analysis quantifies the number of variables of the system from which the same information can be obtained. In effect, this determines how many components of the system are engaged in the same activity (i.e., are coupled in their actions).
As a simple example, consider N components that are coupled to each other in groups of q elements, and each group is tightly coupled so that only one action can be performed by each group so that the scale of action would be q, and the number of distinct actions at a particular time is the number of groups N/q. The complexity (or variety, or information), C(k), as a function of scale, k, is defined as the effective number of actions that can be performed by a particular system at scale k or larger (more formally, it is defined as the logarithm of the number of possible states of the system). In the simple case just described, the number of actions is N/q for all values of k less than q and zero for larger values of k. Mathematical expressions that obtain C(k) for systems with arbitrary probabilities of the set of states of the system can be found in the reference 9.
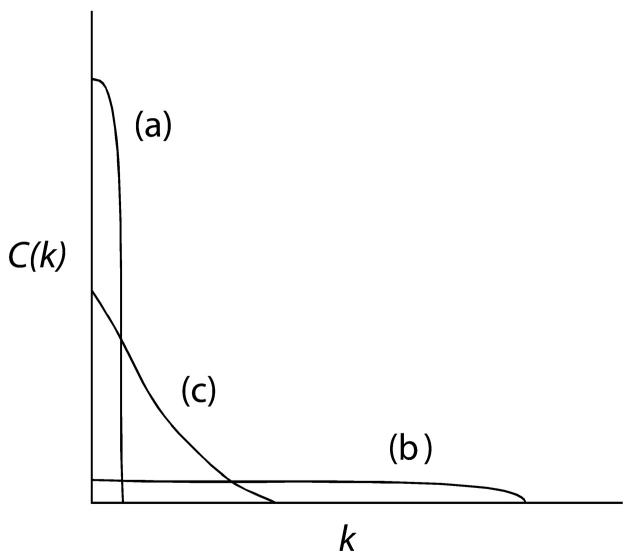
Figure 2 ▶ plots the response capabilities at each scale for the prototypical systems discussed in this section. Larger scales imply that many individuals are performing the same (or directly coupled) tasks, while fine scales imply independently acting individuals. Distinct curves illustrate the relationship between organizational forms and the tasks they can perform. A system in which individuals are independent, responding individually to distinct tasks (curve a), can perform many tasks, each of which draws the attention and efforts of one individual. This is quite different from a system in which all individuals are performing the same or coupled tasks (curve b) and which can only perform a single act in response to an environmental demand, whether the demand is for one or many individuals to perform that act. An organization that has various ways in which individuals coordinate activity into groups of different sizes can act at different scales to differing degrees in a manner that depends on the specific ways individuals are coordinated (curve c). The same analysis that describes the repetition of tasks among multiple individuals also can be used to describe the repetition of tasks over time, compared with its variation when tasks are distinct at different times.
FIGURE 2—
Complexity as a function of scale.
Note. Schematic illustration of complexity C(k) (vertical axis) as a function of scale, k (horizontal axis). A system with the highest possible fine-scale complexity corresponds to a system with independent parts (curve a). When all parts act together, the system has the largest-scale behavior but the same low value of complexity at all scales (curve b). Complex systems have various possible scales of behavior, as illustrated by one example (curve c).
A fundamental result of multi-scale analysis9 is that for a particular set of components, the area under the C(k) curve is independent of organizational structure. This can be readily seen for the simple example earlier in this section, where the area is given by the product of the largest scale of action q—the width of the nonzero part of C(k)—and the number of such actions N/q—the height of the nonzero part of C(k)—which gives the structure-independent value N. The organizational structure therefore selects a trade-off in capability at different scales. This means that, fixing the number of individuals, an organization with the ability to respond at a larger scale is not able to respond at a fine scale, and vice versa.
Thus, different types of industries should be organized in different ways. For example, mass production is a large-scale task and an organization that is designed for mass production should be quite different from an organization that provides individualized care, as is generally understood to be the role of the existing health care system. Different parts of a system can also be analyzed in this way. Of particular relevance is an analysis of the financial flows of the health care system (larger scale) and the system of physicians that are performing the care (higher complexity at a finer scale of action).
TURBULENCE IN THE HEALTH CARE SYSTEM
This multiscale formalism can describe the coupling of a large-scale flow to a fine-scale flow, as is present in the financial flows of the health care system. An analogy to the phenomenon of fluid turbulence helps explain why this coupling, when used for health care, is ineffective. Our conclusions follow from the multiscale framework even without a fine-tuned, quantitative application because, in the language of multiscale formalism, the current situation is far from subtle. This should not be surprising, since the system failures are not subtle either. Turbulence occurs when a simple coherent flow is broken up into many smaller flows. It can be observed in the swirls and eddies in a fast-flowing river, or in the way a column of smoke rises from a camp fire. Although one can identify situations where turbulence will occur, it is very difficult to predict the resulting motions, which are irregular and can change rapidly.
In the health care system, we have an analogous situation. The large-scale financial flows that drive the system eventually have to be allocated as small payments to individual doctors treating individual patients for individual problems. The transition from large to fine scale is turbulent for financial flows just as it is for fluid motion. The idea that turbulence is analogous to what occurs in the health care system will not surprise those who work in it, as they have experienced the turmoil over the past 20 to 30 years. The unpredictable rapid changes have not been in the relationships between doctors and patients, or in the relationships between employers and insurers (although sometimes they feel involved, at least as interested spectators); the main changes have been between insurers and the physicians. The growth of managed care, physician cooperatives, reporting and billing systems, and hospital mergers are all part of the interface between insurers and physicians. These changes in organizational structure, and particularly the consolidation (aggregation) of medical services, are a response to the flows that are disaggregating from large scale to fine scale. Many of the changes at the large scale that have occurred or are being considered to improve the system, including changes in the number of self-insured employers or degree of government involvement, do not significantly change the driving force or the structure of the turbulence.
What does this turbulence look like in human terms? The problem of large flows connected to highly complex flows is abstract, but the reality is quite easy to recognize. Eventually, the issue is related to the problem of controlling the flow, specifically: who is making the decisions that control the flow of money in this system? Increasingly, since the 1970s—or perhaps since the founding of Medicare in 1965—an effort has been made to control the flow at the large-scale end. Both government agencies and private insurers, frequently with the intervention of state and federal government organizations, negotiate the rate of flow of the money. They decide on changes in the rate from one year to the next. Ultimately, the way these rate changes affect the system influences the character of the behavior and organization of the system.
Consider the effects of a simple action like changing the flow at the source, by increasing (or decreasing, although practically speaking the former is more likely) the amount by a certain percentage (e.g., 3%). The amount of increase reflects a decision about how much should be spent on health care. How does the health care industry implement this decision? At the opposite end of this flow, individual doctors treat individual patients with specific highly specialized care based on highly complex choices; their ultimate decisions are based on years of training and experience. The costs of individual treatments range widely—from tens of dollars to millions of dollars.
The consequence of this increase (so much and no more) must manifest itself in the decisions individual doctors make regarding the care of individual patients. They must decide what amount of time and attention to devote to a particular patient, as well as what medical tests and treatments are needed. Ultimately, these decisions must be based on tradeoffs in health and care that compare diverse treatments. Physicians faced with restrictions on expensive procedures and treatments, or incentives to lower their own expenses, have to decide whether the amount of time and effort devoted to a particular appointment or individual, or a particular diagnostic test or therapy, is “worth it”—that is, not only whether a successful outcome is likely but also whether it is cost-effective. Since this kind of judgment includes considerable uncertainties and is largely incompatible with their medical training, different organizations—and individual physicians—make this judgment in different ways, resulting in extremely unstable and variable quality of care overall.
What can those who want to control costs do? It is clearly impossible for those who “manage care” to make decisions about changes in care on an individual-by-individual basis in a way that will altogether correspond to the change in total flow specified from year to year. The only thing they can do is stipulate overall policies that act across the board. These policies typically restrict the set of options that are available for patients or physicians. Patients are restricted to certain physicians, hospitals, or other care providers. Physicians are restricted in what diagnostic tests or medications they can provide. The amount of time spent in hospitals might be limited, or incentives to reduce the amount of time or attention to individual patients could be implemented.
It is not surprising that limiting the options that a patient or physician can choose will have a negative impact on the quality of care that can be provided. Examples of detailed studies illustrating this principle include limitations on postpartum stays correlating with readmissions25 and drug formularies (restrictive lists of prescription drugs) leading to increased costs and decreased quality of care.26,27 The effectiveness of cost control strategies to achieve their objectives has been questioned on the basis of historical experience.6 The more detailed studies challenge the idea that such actions actually save costs even when implemented according to plan, as indirect effects may ultimately lead to increased costs. Multi-scale analysis provides a more general understanding that is based on the functional behaviors of complex systems, and this analysis does not require a specific mechanism in order to arrive at the same conclusion. Fundamentally, it is not a good idea to use across-the-board (large-scale) rules to try to control a highly complex system that is making careful (highly complex) decisions.
This discussion clarifies why recent efforts to increase efficiency have led to organizational turbulence and the current need for and difficulties with quality improvement. As the necessary treatment of individual patients has become progressively more complex and individualized, health maintenance organizations, managed care, Medicare, and Medicaid and other health insurance solutions have been acting in a way that makes the structure of health care more large scale and undifferentiated. Because of the complexity of the resulting allocation problem, unexpected “indirect” effects have resulted from these efficiency methods. According to the analysis presented here, these indirect effects arise from the reduction of fine-scale complexity of the organizations performing the tasks. When an organization becomes less effective overall at many different tasks, it is not necessarily less effective at the particular tasks or measures that management or regulators are focusing on. Indeed, one can expect that for those tasks or measures, the organization will improve, while for others its effectiveness will decline. This explains why problems appear as indirect effects.
Moreover, the more problems arise with quality, the greater are the efforts to regulate the actions of doctors, nurses, and other medical professionals. Uniform regulation, whether for cost containment or for quality, has the same effect on a system performing high-complexity tasks—diminishing overall effectiveness. It may seem that imposing uniform care in some context may be constructive; however, in the context of complex organizations, uniformity is in itself a limitation (exceptions do exist, but they must be understood within the framework of multiscale analysis rather than just assumed to exist). Since the resulting problems show up as indirect effects, it is difficult to discover their origins.
The problem is that the health care system is expected to behave efficiently with respect to financial flows at the large scale, but to exhibit the high complexity of individual patient care at the fine scale. If all patients were in roughly the same condition, requiring roughly the same treatment, an efficiency approach would be adequate, as this approach works well for streamlining low-complexity procedures. However, the medical treatment of patients is an extremely high-complexity fine-scale task. One-size-fits-all does not work in this case. Applying such methods can only result in poor-quality care. Although the current state of the health care system as presented here is grim, a fundamental approach to solving the problem does exist.
MATCHING SCALES
Multiscale analysis suggests that a key to organizational effectiveness is the matching of the scale of processes to the task. The current structure of the health care system inherently fails to do so. An important aspect of the solution to this problem is the recognition that some health care tasks are repeated many times and are thus large scale. Large-scale tasks can be performed with efficient processes, reducing expenses and improving the overall effectiveness of the system. Once we recognize which of the health care tasks are large scale, we can use them to improve the matching of tasks and financial flows. In this way, the current difficulties of financial control can also be relieved. The approach of identifying which tasks are large scale can be extended to identifying tasks that have intermediate scales. The development of organizations that perform tasks at various intermediate scales as appropriate would result in substantial additional efficiency. This article fouses on the largest-scale aspects of health care that should be addressed at a population level and are often identified with the field of public health.
How can we create a health care organization that is effective at large-scale tasks? The existing approach to health care organizations already has some separation of tasks, particularly in hospitals. Nevertheless, the patient–physician interaction continues to be used as an essential part of most health care tasks. The issue of a trade-off is manifest when we consider whether an individual (e.g., physician) is able to perform rapid repetitive tasks when they are needed and take enough time to perform careful complex tasks when these are needed. Is this possible, or does the speed become compromised in some cases while the need for time becomes compromised in others? Even more critical is the problem of coordination, since when there is a change in protocol of large-scale tasks, all individuals must change behavior. However, individuals must act independently for complex tasks. This creates a need for management structures that control the tasks being performed by the organization when it is necessary, but do not control tasks when it is not advisable. Thus, key demands on individuals and on organizational structures must be met.
We can contrast this to a strategy of separating the large-scale tasks from the fine-scale tasks, creating mostly separate organizations involving different people for doing them. Let’s call the separated organizational structure a heterogeneous organization, and the single organizational structure for all tasks a homogeneous organization. We can think of the task requirements as a complexity profile, C(k), of things to do, and the objective is to cover this area with the complexity profiles of individual people. Stacking individual profiles vertically means having them work independently, and stacking them horizontally means having them work in a coordinated way. In a heterogeneous organization, some individuals stack vertically and others stack horizontally, while in a homogeneous organization all individuals contribute equally to tasks at all scales (so that each individual has the profile C(k)/N ).
The following observations support the choice of a heterogeneous organization: (1) The use of a homogeneous organization is a severe restriction on the types of organization that are possible. Heterogeneity opens many more possible organizational forms. (2) Not all organizations can achieve all forms of coordination. For example, it has been proven that hierarchical organizations cannot achieve high complexity at intermediate scales.9 (3) Organizational structures that are designed for a restricted set of scales are both better known and more transparent than organizational structures requiring various levels of coordination of individuals at multiple scales. Thus, where tasks can be separated, a heterogeneous organization can be more easily understood, planned, and designed than a homogeneous structure. (4) Individuals may be quite different from each other in their individual scale and complexity trade-off. Thus, a person who intrinsically performs simple tasks repetitively is distinct from a person who intrinsically performs careful decisionmaking about high-complexity tasks. A heterogeneous organization allows different individuals to perform individually appropriate roles. (5) Organizational specialization (i.e., the formation of a heterogeneous organization) is a larger version of individual specialization, a well-established concept.
There are many examples of organizations, both biological and social, that separate distinct kinds of tasks and thus provide phenomenological support for these formal conclusions. Human physiology provides several illustrations: legs for walking are designed differently than hands that can manipulate finer-scale entities. The immune system is designed differently from muscles, the former for more complex finer-scale challenges than the latter. Similarly, the military is separated into a variety of forces: tank divisions, infantry, marines, and special forces for different trade-offs in scale and complexity. Even supermarkets have different sections for purchasing cheese—for example, the dairy and the deli, one for larger-scale and the other for more complex products.
These examples illustrate the fundamental principles revealed by the multiscale analysis and the theorem that implies a tradeoff in a system’s effectiveness on the basis of organizational structure. They also show how, by creating distinct parts of the system to address different types of tasks, it is possible to effectively perform these different tasks.
SEPARATING LARGE-SCALE CARE FROM COMPLEX CARE
Intuitively, we can recognize that preventive care and population health services are frequently large-scale tasks. Indeed, we can consider the concept of large scale as defined by the multiscale analysis to provide a possible formal framework for understanding the domain of public health as an organizational imperative. The public health system works through many channels to achieve improved prevention and population health. Moreover, it also frequently serves as a palliative to the failings of the health care system by providing health care services. Still, one of the main channels for action is the health care system. The analysis presented here suggests that a public health system that promotes private organizations or publicly supported organizations (or both) that are effective at large-scale prevention and population care will be more effective in the long term.
The role of such organizations should include performance of a variety of tasks that are intrinsically large scale. In health care, these include wellness services (such as nutrition programs), the management of some widespread chronic problems, prenatal care, the treatment of common minor health issues (allergies, stress, the common cold), and preventive procedures (such as immunizations and screening through diagnostic tests). Many of these services can be made highly efficient when performed on populations, as they do not require decision-making on an individual basis. They can be separated from those aspects of health care that require decisionmaking on an individual basis. While the general principle is clear, the specific services to be separated should be determined by a more detailed quantitative analysis of complexity and scale as well as pilot programs that are properly focused on the issue of efficiency and effectiveness as articulated by the analysis. The degree of separation may also be explored. Some solutions might place prevention and population services as divisions or units within health care organizations, and others might have them associated with other types of organizations, such as pharmacies and supermarkets, that have more experience with efficient services. While the separation could also be done through government delivery, this is not necessary even if government oversight is desirable.
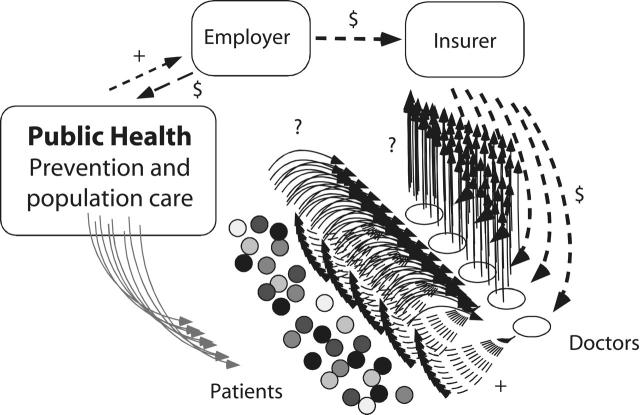
The high-efficiency prevention and population care system pictured in Figure 3 ▶ would function in some ways analogously to a traditional mass production factory model, or a mass market service organization like a fast food provider. There are ample precedents for such activities in health care in the United States and internationally, from historical and current public vaccination programs28,29 to modern supermarket delivery30,31 and mass screening programs.32 Such programs administer vaccinations and diagnostic tests on groups rather than through individual appointment. The purpose is to ensure a high level of health in the population and to identify those who will need individual medical attention. Exceptions are referred to the medical system. The objective is large-scale efficiency, but once a problem is identified, individual attention can be personal and effective.
FIGURE 3—
A proposed structure for a new health care system.
Note. The proposed new public health component (left box) provides efficient population-based care (+) to its customers, including employers (as shown by the upper left arrows), private insurers, government agencies, or individuals (similar to high-efficiency fast food and other mass market products or services); arrows are not shown for the latter cases. Moreover, it refers (gray arrows) those who need individualized care to the other part of the healthcare system (with interactions and symbols as in Figure 1 ▶) that is focused on individualized care.
Separating large-scale tasks from complex tasks enables efficient and effective organizations to be formed around these distinct tasks. A system for population health can be made efficient on a large scale. A system designed for the complexities of individual medical care must be error free in individual tasks. Separating large-scale “prevention and population care” from complex “individualized care” relieves physicians of tasks that can be addressed with a much higher efficiency, enabling them to focus their attention on the complex tasks for which they are uniquely trained. Overall, this enables the system to be more efficient as well as more effective.
The idea of separate systems reasonably evokes concerns about reciprocal communication. Moreover, the need for communication often suggests the adoption of centralized databases, which raises concerns over privacy. Without engaging in a full discussion, I can suggest at least one potential solution: having individuals carry personal health information with them in portable storage media such as memory cards, which are a simple and relatively inexpensive technology.
The development of an efficient system for prevention and population health also would help to fundamentally address many of the other problems with the health care system. Highly efficient services would make such care much more widely available, with the potential of radically reducing disparities. Perhaps even more important, the fundamental role of prevention and population health in reducing the need for medical care (which is what prevention is about) could be realized. The benefits of the “virtuous cycle” of prevention—which reduces the costs of health care and frees resources for more careful medical care where it is needed, as well as for more preventive and population care—is the converse of the current “vicious cycle” of reduced prevention—which leads to the need for more medical care and the availability of fewer resources for each individual that requires care. This virtuous cycle—along with the intrinsic value of improved health—is recognized as the reason prevention is needed, but it can only be realized when prevention is performed efficiently and effectively.
The principle of separation of tasks at different scales can be applied also to many other aspects of health care. For example, some surgical procedures may be performed as efficient mass production processes if there are many individuals with similar conditions requiring similar procedures. This may be true even if the decision to perform the surgery is highly complex. Other forms of surgery are clearly highly complex. Such examples abound within the health care system. Understanding the concepts of scale and complexity and how to apply them to specific tasks may be helpful in determining the details of organizational structures. A more detailed discussion is beyond the scope of this article.
Finally, high-efficiency processes, when widely applied, increase dramatically the availability of data that can improve knowledge of how to use this information.
CONCLUSIONS
A multiscale analysis of information flow in the health care system demonstrates that efforts to lower costs through managed care must lead to ineffectiveness, as is manifest in medical errors and low quality of care. Moreover, while there has been significant debate about whether the payer system should be public or private, this dichotomy does not address the essential failings of the system, and either choice (public or private) can be well or poorly executed.
A public health system should recognize key distinctions between individual and population care, and develop systems that are well designed for delivering distinct types of services. The need for increased investment in prevention and population-based services must be married to a recognition of the organizational needs for such tasks. Among the changes in the health care system that can contribute to improvement is a separation of complex tasks from large-scale tasks. The current health care system is an individualized system, and even when it provides care relevant to populations it typically provides them through a one-to-one physician–patient model. Individualized care should be entrusted to a fine-scale, individual-care medical system, while a distinct system should be created for large-scale and efficient prevention and population health programs.
With such a separation, we will no longer expect one organizational structure to provide both financially efficient population and preventative care that can be performed in a repetitive way and complex medical care that requires careful decisionmaking in each case. Attempts by the same organization to perform both will create conflict between the short-term response to immediate needs of individual patients and the long-term benefits of prevention and population care. Just as having physicians doing the laundry at hospitals would be ineffective and inefficient, such a dual-purpose system can only be expected to provide mediocre response to both tasks. An efficient prevention and population-based care delivery system will improve this aspect of care and health care as a whole by helping to relieve the stresses on care provided to individuals.
A system that delivers effective population-based care can demonstrate clearly the importance of prevention and population care in the overall health care system. In this context, the traditional expectations of the benefit of prevention can be realized. The well-understood cost-effectiveness of prevention in the long term implies that even a small proportion of the overall costs, though not small in absolute terms, devoted to public health can enable the larger proportion, which is devoted to individual medical care, to be allocated to needed individual services that are not provided by the current overburdened system. The result is a relief of financial pressure, a better balance between prevention/population care and individualized medical care, and systems that are separately effective at both, leading ultimately to a healthier population.
A full discussion of specific practical transitional steps to achieve such a system is beyond the scope of this article. However, it should be understood that the benefit of a multiscale understanding of the health care system is the recognition that changes in organization can be of widespread benefit, and this understanding should promote the adoption of change. Specifically, a wide range of players should recognize that changes that promote adoption of a prevention- and population-based care system will serve their goals and interests.
A more complete solution for the problems of the health care system would also require other concepts essential to the development of highly complex organizational structures. These concepts, which can be obtained from multiscale analysis, include (1) recognition of the limitations of centralized control in the management of complex medical care; (2) recognition of both the possible constructive role and the limitations of automation in improving health care; (3) analysis of structures of information flow associated with medical errors, which may suggest structures that eliminate medical errors; and (4) the understanding of how to induce organizational change and improvement in highly complex organizations for high-complexity medical tasks, including the role of competition and cooperation in systems that may or may not be market driven. Such issues are relevant to the role of payment and reward systems. A discussion of these ideas can be found elsewhere.10
Acknowledgments
This work was supported in part by the Centers for Medicare and Medicaid Services and the Centers for Disease Control and Prevention.
Transcription and editing of early versions of the manuscript were performed by Chitra Ramalingam and Laurie Burlingame. Acknowledgments are due to my students and colleagues who read and commented on previous versions. In particular, I thank Michael Ganz for comments on the manuscript and the referees for helpful remarks.
Human Participant Protection No protocol approval was needed for this study.
Peer Reviewed
References
- 1.Institute of Medicine. The Future of Public Health. Washington, DC: National Academies Press; 1989.
- 2.Institute of Medicine. Future of the Public’s Health in the 21st Century. Washington, DC: National Academies Press; 2003.
- 3.Declaration of Alma-Ata. International Conference on Primary Health Care, Alma-Ata, USSR. Geneva, Switzerland: World Health Organization;1978.
- 4.World Health Report 2000. Geneva, Switzerland: World Health Organization; 2001.
- 5.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the Twenty-First Century. Washington, DC: National Academy Press; 2001.
- 6.Altman D, Levitt L. The sad story of health care cost containment as told in one chart. Health Aff. January 23, 2003. Available at: http://content.healthaffairs.org/cgi/content/full/hlthaff.w2.83v1/DC1. Accessed January 25, 2006. [DOI] [PubMed]
- 7.Bar-Yam Y. Dynamics of Complex Systems. Cambridge, Mass: Perseus Press; 1997.
- 8.Bar-Yam Y. General features of complex systems. In: Keil LD, ed. Knowledge Management, Organizational Intelligence and Learning, and Complexity. Encyclopedia of Life Support Systems [online publication]. Oxford, England: UNESCO EOLSS Publishers; 2002. Available at: http://www.eolss.net. Accessed January 26, 2006.
- 9.Bar-Yam Y. Multiscale variety in complex systems. Complexity. 2004;9: 37–45. [Google Scholar]
- 10.Bar-Yam Y. Making Things Work: Solving Complex Problems in a Complex World. Cambridge, Mass: NECSI Knowledge Press; 2005.
- 11.Shannon CE. A mathematical theory of communication. In: Shannon CE, Weaver W. The Mathematical Theory of Communication. Urbana: University of Illinois Press; 1963:29–125.
- 12.Cover TM, Thomas JA. Elements of Information Theory. New York, NY: Wiley; 1991.
- 13.Arrow KJ. Uncertainty and the welfare economics of medical care. Am Econ Rev. 1963;53:941–969. [Google Scholar]
- 14.Rothschild M, Stiglitz J. Equilibrium in competitive insurance markets: an essay on the economics of imperfect information. Q J Econ. 1976;90:629–650. [Google Scholar]
- 15.Akerlof G. The market for lemons: qualitative uncertainty and the market mechanism. Q J Econ. 1970;84:488–500. [Google Scholar]
- 16.Ma CA. Health care payment systems: cost and quality incentives. J Econ Manage Strategy. 1994;3:93–112. [Google Scholar]
- 17.Ellis RP. Creaming, skimping, and dumping: provider competition on the intensive and extensive margins. J Health Econ. 1998;17:537–555. [DOI] [PubMed] [Google Scholar]
- 18.Glazer J, McGuire TG. Optimal risk adjustment in markets with adverse selection: an application to managed care. Am Econ Rev. 2000;90:1055–1071. [Google Scholar]
- 19.March JG, Simon HA. Organizations. 2nd ed. New York, NY: John Wiley & Sons; 1958.
- 20.Galbraith J. Designing Complex Organizations. Reading, Mass: Addison-Wesley; 1973.
- 21.Mintzberg H. The Structuring of Organizations. Englewood Cliffs, NJ: Prentice-Hall; 1979.
- 22.Weick K. The Social Psychology of Organizing. 2nd ed. New York, NY: McGraw-Hill; 1979.
- 23.Robbins SP. Organization Theory. 3rd ed. Englewood Cliffs, NJ: Prentice-Hall; 1990.
- 24.Daft RL. Organization Theory and Design. 8th ed. Cincinnati, Ohio: SouthWestern; 2004.
- 25.Malkin JD, Broder MS, Keeler E. Do longer postpartum stays reduce newborn readmissions? Analysis using instrumental variables. Health Serv Res. 2000;35:1071–1091. [PMC free article] [PubMed] [Google Scholar]
- 26.Horn SD, Sharkey PD, Tracy DM, Horn CE, James B, Goodwin F. Intended and unintended consequences of HMO cost-containment strategies: results from the Managed Care Outcomes Project. Am J Manag Care. 1996;2: 253–264. [Google Scholar]
- 27.Horn SD, Sharkey PD, Phillips-Harris C. Formulary limitations and the elderly: results from the Managed Care Outcomes Project. Am J Manag Care. 1998;4:1104–1113. [PubMed] [Google Scholar]
- 28.Plotkin SA, Orenstein WO, eds. Vaccines. 3rd ed. Philadelphia, Pa: WB Saunders; 1999:112.
- 29.Bland J, Clements J. Protecting the world’s children: the story of WHO’s immunization programme. World Health Forum. 1998;19:162–173. [PubMed] [Google Scholar]
- 30.Weitzel KW, Goode JV. Implementation of a pharmacy-based immunization program in a supermarket chain. J Am Pharm Assoc (Wash). 2000;40: 252–256. [DOI] [PubMed] [Google Scholar]
- 31.Glezen WP, Mostow SR, Schaffner W. The revolution in influenza care. Patient Care. 2000;34:22–24. [Google Scholar]
- 32.Sone S, Takashima S, Li F, et al. Mass screening for lung cancer with mobile spiral computed tomography scanner. Lancet. 1998;351:1242–1245. [DOI] [PubMed] [Google Scholar]