Abstract
Objectives. We examined associations between trust of health care providers and the government and health service use and outcomes.
Methods. Interviews with a sample of 611 HIV-positive individuals included an attitudinal assessment measuring beliefs concerning the creation of AIDS, information being withheld about the disease, and trust of care providers.
Results. Trust in care providers was associated with increased HIV-related out-patient clinic visits, fewer emergency room visits, increased use of antiretroviral medications, and improved reported physical and mental health. Trusting the government was associated with fewer emergency room visits and better mental and physical health. More than one quarter of the respondents believed that the government created AIDS to kill minorities, and more than half believed that a significant amount of information about AIDS is withheld from the public. Ten percent did not trust their provider to give them the best care possible.
Conclusions. Distrust may be a barrier to service use and therefore to optimal health. Distrust is not isolated in minority communities but also exists among members of nonminority communities and equally interferes with their use of services and health outcomes.
Numerous studies over the past 3 decades have examined access to care among—and the care-seeking behaviors of—individuals with HIV/AIDS.1–3 For example, studies have examined the influence on health service use of patient characteristics, provider characteristics, and factors such as insurance coverage,1–3 and appropriate use of health services has been shown to be related to improved health outcomes.4 In addition, recent studies have identified an association between HIV/AIDS conspiracy beliefs and behaviors engaged in to prevent sexually transmitted infections.5
However, we were unable to find any peer-reviewed studies of associations between patients’ level of trust in systems of care and their care provider and their use of health services. If education and care efforts are to be beneficial, they should take into consideration the target community’s beliefs, particularly as they relate to disease origin and whether providers will provide community members with appropriate care.
Mistrust of the medical community on the part of Black Americans extends back to the era of slavery, when slaves served as subjects in medical experimentation and research without consent or personal benefit.6,7 Blacks believed that White physicians allowed such subjects to die so that they could dissect their bodies.6 Bodies of Black Americans were, in fact, exhumed and sold to science.6 The Tuskegee Syphilis Study further fostered fear and distrust of public health officials and later reinforced the conspiracy theories regarding AIDS.6–9
Studies have shown that a large proportion of Black Americans believe that HIV/AIDS is a man-made weapon of racial warfare and that the government promotes substance abuse as a way of keeping Black Americans poor and in prisons.7 These beliefs have been supported through dissemination by providers, policymakers, and the media of literature promoting such theories.6,10 Other research has found that many people believe that AIDS is a disease created by God as punishment for breaking religious and moral laws, that is, a punishment for their sins or the sins of their parents.11,12
Inequities in access to health care and adequacy of treatment have been well documented4 and may support conspiracy theories. Black Americans are less likely than White Americans to ask their physician questions freely.13 They are more likely to report believing that their physician will expose them to unnecessary risk, prescribe them experimental medications,13 not provide them with the best care available,14 and be motivated by profit.15 Income4 and health insurance coverage13 do not modify the relationship between race and trust. Mistrust in the medical care system has led, in some cases, to an inability to recruit members of minority groups, especially Black Americans, into clinical trials.7 Black Americans have been found to be less likely to perceive any real benefits to such research.
A growing body of literature provides evidence that economic disparities are related to health outcomes and are partially responsible, through varying mechanisms, for discrimination previously believed to be racial or ethnic in nature.4,16 There is a lack of literature related to trust of providers and the government on the part of poor European Americans.
We examined trust in health care providers and the government and its association with health service use and health outcomes among an HIV-positive cohort recruited from 5 states in the “Deep South” (usually considered to include Alabama, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, and all or part of Florida, Virginia, Tennessee, Arkansas, and Texas). We also explored racial differences in levels of trust. If trust influences use of health services, then providers and policymakers attempting to reduce barriers to care, particularly among the poor and disenfranchised, should address this issue.
METHODS
The Coping with HIV/AIDS in the Southeast Study interviewed 611 consecutively sampled HIV-infected individuals who received care at one of 8 infectious disease clinics in 5 states of the Deep South: North Carolina, South Carolina, Georgia, Alabama, and Louisiana. This region was selected as a result of its demographic and economic similarities. Incident AIDS cases increased 29% from 2000 to 2002 in these 5 states, as compared with increases of 9% across the other southern states and less than 1% (0.32%) in the remainder of the country.17,18
This study was funded by the National Institute of Mental Health to examine the characteristics, coping strategies, life histories, and patterns of health care use of individuals receiving HIV-related care outside the 3 major cities within the 5 study states. At the time of recruitment in 2001, the clinics chosen for study inclusion treated 11.9% of the 5 states’ HIV/AIDS patients, and 10.0% of the clinic patients at that time participated in the interviews, which were conducted by Battelle’s Center for Public Health Research and Evaluation in Durham, NC. All sites were carefully monitored to ensure that interviewers were implementing the consecutive sampling strategy.
The demographic characteristics of the study participants were representative of those of the overall populations seen at each of the clinics. Approximately one third of the patients seen at these clinics are female (31% in our study population), and more than 70% are African American (69% in our study population). Also, these percentages reflected the population breakdown of HIV-positive individuals in each of the study states at the time of recruitment (at least 70% African American and approximately 30% female).
Measures
Participants responded to 3 items related to trust in their providers. First, they indicated the extent to which they agreed with the statement “Your doctors want to give you the best care possible.” Second, they were asked “How much do you trust your HIV doctor or clinic to offer you the best medical care they can provide?” and “How much do you trust your HIV doctor or clinic to put your health above everything else?” Each response could range from 1 (no trust) to 5 (complete trust). Respondents were also asked to rate their agreement, on a 5-point Likert scale, with the following 3 statements: “The government is using AIDS as a way of killing off minority groups,” “A lot of information about AIDS is being held back from the general public,” and “AIDS is the punishment of God” (on each statement, the response range was 1 to 5).
Principal components factor analyses conducted on these variables identified 2 underlying factors. The similar factor loadings for the respective component variables suggested that responses could be given equal weights in the creation of summary scales. Respondents’ belief that God created AIDS as punishment had the greatest uniqueness and was used as a separate variable. The questions relating to trust of physicians were combined into a summative scale ranging from 3 to 15 (15 representing the greatest amount of trust), while the 2 remaining items representing trust in the government were combined into a scale ranging from 2 to 10 (10 being the highest). The internal reliabilities of the 2 scales were 0.78 and 0.56, respectively.
Respondents were asked how many times they had gone to an outpatient clinic for HIV-related care over the past 9 months. Approximately one visit every 3 months (3 visits over the 9-month period) was considered optimal care.19 The distribution of clinic visits was skewed, with the majority of respondent visiting a clinic for HIV-related care 3 or fewer times and a large tail to the right with some respondents going to the clinic for HIV care one or more times per week. Because our variables of interest were related to trust, we decided that visiting a clinic at least the optimal number of times was an indication of willingness to receive appropriate care. Therefore, a binary variable was created in which 1 represented 3 or more clinic visits and 0 represented fewer than 3 visits.
Similarly, respondents were asked whether they had been to the emergency room in the past 9 months and, if so, how many times. We did not differentiate between emergency room visits that were related to HIV and those that were not. Emergency room visits are commonly used as an aggregate measure of inappropriate health care use, even among individuals who are HIV positive; however, some visits are unavoidable even at appropriate levels of care seeking.20 Respondents were asked whether or not they were taking antiretroviral medications and to identify their medication on a picture pill chart.
We measured health status using the Medical Outcomes Survey Short Form 36 (SF-36), CD4 counts, and viral load counts. The SF-36 has been used in more than 4000 research studies and has been shown to be predictive of clinical health outcomes.21 The SF-36 measures health outcomes along 8 dimensions: (1) physical functioning, (2) limitations in physical abilities, (3) pain, (4) general perceptions of one’s health, (5) vitality, (6) social functioning, (7) limitations in activities due to emotional health issues, and (8) mental health. The physical component summary scale combines dimensions 1 through 4, and the mental component summary combines dimensions 5 through 8.22–24 The physical and mental health summary scales are the most highly predictive subscales of the SF-36 and can be used in isolation,25 as we did in this study. Items were translated into the recommended rating scale of 0 through 100.24 Viral load and CD4 counts were taken from chart abstraction data. The counts used in this analysis were those that were taken closest to the interview date, and viral loads were logged (base 10).
Whether respondents lived in poverty was calculated from their reported total income from all sources as compared with the federal poverty level. Federal poverty level determinations take into consideration the number of dependents living in a household; therefore, we used number of dependents in the household in our calculations. Because the vast majority of non-White respondents were African American, we created a single variable labeled “minority.”
Statistical Analysis
We conducted t tests to examine differences in variable means between minority and nonminority respondents and between male and female respondents. To further examine interactions between trust and minority status, we created 2 × 2 tables (Minority/Nonminority × Full Trust/Any Distrust) for each outcome variable. We then used t tests to examine differences between these variables.
We used logistic regression in analyses of HIV-related outpatient visits and in analyses of whether respondents reported being on or off antiretroviral medications. We used a negative binomial model to examine emergency room visits, the reason being that such models explicitly deal with count data and can account for large proportions of zeros in use measures and skewed distributions of positive values. In addition, unlike the more commonly used Poisson model, the negative binomial model allows for overdispersion, or variance greater than the mean. In the case of emergency room visits, the mean was 0.87, with a variance of 4. We used ordinary least squares regression in analyses of health status because each of the outcome variables was continuous and normally distributed.
We used F tests to determine whether site variables were jointly statistically significant in any of the regression models. Statistical significance would have indicated significant variation in the outcome variables according to study site, and this variation, if correlated with trust, would have biased our estimates if omitted. We found that site differences were significant in several of the models, and thus we included site-fixed effects in each of the regressions.
To analyze the sensitivity of the findings to the model specification, we ran alternative specifications for each regression model. The regression models focusing on health care use (e.g., clinic and emergency room visits) were run with and without physical health and mental health as independent variables, and viral load was examined in both the presence and absence of antiretroviral use. We present the regression results without the antiretroviral use variable because this variable was associated with trust. All of the models were also run with and without interaction terms for minority and the variables for trust in providers and trust in government.
RESULTS
Descriptive Statistics
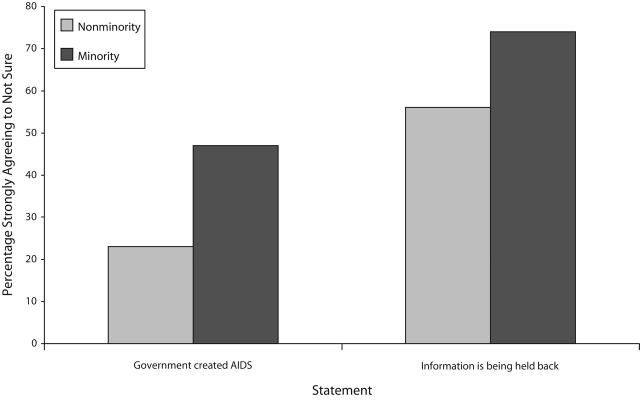
Nearly one quarter of all minority respondents (23%) and 11% of nonminority respondents strongly or somewhat believed that the government created AIDS to kill minorities (Figure 1 ▶). These percentages increased to 47% and 23%, respectively, when uncertainty as to whether the government created the disease was included.
FIGURE 1—
Findings reflecting mistrust of the government.
More than half of the minority respondents and one third of the nonminority respondents strongly or somewhat believed that a significant amount of information about AIDS was being held back from the public. When uncertainty as to whether information was being withheld was included, the percentages increased to nearly three quarters of minority respondents and more than half of nonminority respondents. Overall, half of the respondents believed that information regarding HIV was being withheld from them.
Differences in trust according to minority status were statistically significant (P < .001). Ten percent of respondents did not trust their doctor or clinic to provide them with the best care possible, and 1 in 7 did not believe that their provider placed their health care above all other considerations.
Respondents’ mean rating of trust in their doctors was 13.5 on the earlier-mentioned 3 to 15 scale, and their mean rating of trust in the government was 6.5 on the 2 to 10 scale described earlier (Table 1 ▶). Their mean rating in terms of believing that AIDS is not a punishment from God was 4.5 on a scale ranging from 1 to 5, with 5 representing strong agreement. An examination of levels of trust according to minority racial status revealed significant differences (Table 1 ▶). Minority respondents were more likely to believe that the government created AIDS and that information about it is being withheld (both Ps < .001). Minority respondents also were more likely to believe that AIDS is a punishment from God (P < .001).
TABLE 1—
Means and Percentages for Dependent and Independent Variables
| Total Sample (n = 611) | Minority Respondents (n = 422) | Nonminority Respondents (n = 189) | |
| Trust doctor,a mean rating (SD) | 13.5 (2.4) | 13.46 (2.06) | 13.69 (1.92) |
| Trust government,b mean rating (SD) | 6.5 (1.1) | 6.10 (2.32) | 7.45 (2.24)* |
| AIDS is a punishment from God,c mean rating (SD) | 4.5 (2.0) | 4.36 (1.14) | 4.67 (0.91)* |
| Age, mean (SD) | 40.2 (8.7) | 40.3 (8.5) | 40.2 (8.7) |
| Younger than 40 y, % | … | … | … |
| Male, % | 68.7 | 62.7 | 82.0* |
| Minority, % | 69.0 | … | … |
| High school graduate, % | 79.7 | 75.6 | 88.9 |
| Living in poverty, % | 70.5 | 70.1 | 71.4 |
| SF-36 physical composite score, mean (SD) | 67.5 (23.7) | 67.5 (23.5) | 67.6 (24.1) |
| SF-36 mental health composite score, mean (SD) | 59.1 (21.5) | 60.3 (21.2) | 56.7 (22.0) |
| Taking antiretrovirals, % | 77.6 | 75.8 | 81.5 |
Note. SF-36 = Medical Outcomes Survey Short Form 36.
aOn a scale of 3–15, with 15 being highest.
bOn a scale of 2–10, with 10 being highest.
cOn a scale of 1–5, with 1 being punishment.
*P < .001.
The average age of the study population was 40 years. The proportions of the respondents who were male and members of minority groups were reflective of the HIV-positive populations residing in the study states. More than two thirds of the respondents were living in poverty. Nonminority respondents were more likely to be male and had higher CD4 counts (P < .001). No other race-specific differences were observed.
Student t tests indicated that minority respondents who distrusted their provider were less likely to visit their provider 3 or more times (P < .05), but this relationship did not hold for nonminority respondents. However, examination of differences between trust means related to reported physical health and mental health scores showed that both minority and nonminority respondents scored significantly lower if they distrusted their provider. Trends were similar, but not significant, for trust in government.
Regression Analyses
Trust in one’s care providers was significantly associated with 5 of the 6 outcome variables (Tables 2 ▶ and 3 ▶): 3 or more HIV-related clinic visits (P<.05), fewer emergency room visits (P<.05), greater likelihood of taking antiretrovirals (P<.01), better mental health (P<.001), and better physical health (P<.01). Trusting the government was associated with 3 of the 6 outcome variables: fewer emergency room visits (P<.05), better mental health (P< .001), and better physical health (P<.001). The statistical significance levels of the associations between trust in care providers and number of outpatient care visits, number of emergency room visits, and use of antiretrovirals did not change when we controlled for physical health status (data not shown).
TABLE 2—
Relationships Between Trust and Service Use
| 3 or More Clinic Visitsa: Odds Ratio (95% Confidence Interval) | Emergency Room Visitsb: Coefficient (SE) | Use of Antiretroviralsc Odds Ratio: (95% Confidence Interval) | |
| Trust care providers | 1.13* (1.02, 1.25) | −0.0768* (0.0365) | 1.15** (1.04, 1.28) |
| Trust government | 1.06 (0.97, 1.17) | −0.0689* (0.0340) | 1.06 (0.96, 1.16) |
| God did not create AIDS | 1.06 (0.87, 1.29) | 0.0392 (0.0672) | 0.97 (0.80, 1.19) |
| Minority | 1.00 (0.59, 1.68) | 0.124 (0.179) | 1.10 (0.66, 1.85) |
| Male | 1.03 (0.65, 1.64) | −0.595*** (0.159) | 1.57* (1.00, 2.47) |
| Younger than 40 y | 0.90 (0.58, 1.40) | −0.009 (0.154) | 0.74 (0.48, 1.14) |
| Living in poverty | 1.15 (0.71, 1.86) | −0.111 (0.169) | 1.56 (0.97, 2.51) |
| High school graduate | 1.32 (0.79, 2.23) | 0.119 (0.190) | 1.29 (0.77, 2.14) |
Note. Clinic differences were controlled via fixed effects.
an = 575.
bn = 594.
cn = 595.
*P < .05; **P < .01; ***P < .001.
TABLE 3—
Relationships Between Trust and Health
| Coefficient (SE) | |||
| Mental Health Scorea | Physical Health Scorea | Viral Load (Log 10)b | |
| Trust care providers | 1.573*** (0.454) | 1.433** (0.498) | −0.0170 (0.0389) |
| Trust government | 1.448*** (0.385) | 1.778*** (0.422) | 0.0067 (0.0295) |
| God did not create AIDS | 0.608 (0.805) | 0.154 (0.882) | −0.0064 (0.0640) |
| Minority | 5.996** (2.055) | 3.039 (2.250) | 0.382* (0.160) |
| Male | 3.263 (1.898) | 3.139 (2.078) | −0.085 (0.145) |
| Younger than 40 y | 2.455 (1.751) | 10.049*** (1.918) | 0.051 (0.134) |
| Living in poverty | 2.966 (1.936) | 0.297 (2.120) | −0.232 (0.149) |
| High school graduate | 5.436 (2.219) | 5.114 (2.430) | −0.358* (0.167) |
Note. Clinic differences were controlled via fixed effects.
an = 595.
bn = 379.
*P < .05; **P < .01; ***P < .001.
Believing that God did not create AIDS as punishment for sins was not related to any of the outcome variables. Minority status was associated with a higher viral load (P<.05), whereas being a high school graduate was associated with a lower viral load (P<.05). Minority status was associated with better mental health (P<.01). Male gender was associated with more emergency room visits (P<.001); being younger than 40 years was associated with better physical health (P<.001). The trust variables were not significantly related to either the CD4 (data not shown) or viral load regression models (Table 3 ▶).
When interaction effects for provider trust and minority status and for government trust and minority status were included in the models, they were not significant either individually or together. Poisson regression provided the same statistical significance for the independent variables as the negative binomial. The significance level for trust in providers was higher (P < .001) when number of clinic visits was run as a negative binomial with the outcome variable being squared deviation from 3 visits. Antiretroviral use was significantly associated with viral load (P < .001) and did not change the results for any other variable.
DISCUSSION
Trust was associated with more appropriate numbers of clinic visits, use of antiretroviral medications, fewer emergency room visits, and better health outcomes. Although a number of studies have found associations between distrust and attitudinal barriers to care, this study illustrates that trust is significantly associated with use of services and medication as well as health outcomes. Our estimates of prevalence of distrust in an HIV-positive population were similar to those reported in a recent telephone survey of 500 randomly selected African Americans aged 15 to 44 years; in that study, 16% of respondents agreed that AIDS was created by the government to control the Black population, and 59% believed that a significant amount of information about AIDS was being held back from the public.5
The finding that members of nonminority groups are distrustful of providers and the government is new to the trust and health literature. Distrust was associated with poor reported health among both minorities and non-minorities. When we controlled for poverty, education, age, and gender, the interaction terms for minority and distrust were not significant, indicating that, regardless of race, individuals with similar sociodemographic characteristics who do not trust their providers or the government are less likely to visit clinics, more likely to use the emergency room, less likely to use antiretrovirals, and more likely to report poor physical and mental health.
These findings suggest the need for further causal research, including studies ascertaining level of trust before treatment initiation and following patients longitudinally to determine whether trust precedes patterns of use. Our cross-sectional data cannot illuminate, for example, whether lower levels of trust result in people being less likely to seek mental health services or accept antiretroviral medications or whether, in contrast, receipt of less care leads to a lack of trust. Furthermore, people who are sicker may feel and express greater distrust.
Another limitation of our study is that consecutive sampling biased the sample recruited toward those who frequented care facilities more often. Also, bias could have been introduced by seasonal variation in the types of patients receiving care. If one were to hypothesize the direction of the resulting bias, it would be toward greater trust in the system of care being used, and thus our results would be conservative.
HIV is spreading at a relatively rapid pace in the Deep South, and this study indicates that more than half of those undergoing care believe that information about AIDS is being held back from the public, and one quarter believe that the government created AIDS as a way to kill minorities. One in 10 of our respondents reported not trusting their doctor or clinic to provide them the best care possible, and 1 in 7 reported not believing that their provider placed their health care above all other considerations. Furthermore, minority respondents exhibited greater distrust, but nonminority respondents were also distrustful. Our results indicate that distrust is a major issue in these 5 states of the Deep South, one that may need to be addressed in both prevention and care services.
Acknowledgments
This study was supported in part by the National Institute of Mental Health (NIMH), the National Institute of Drug Abuse (NIDA) and the National Institute of Nursing Research (NINR) (grant 5R01MH061687–05).
We thank the principal investigators, project coordinators, and interviewers at each of the study sites for their incredible work in ensuring a truly consecutive sampling procedure, their participation in training, certification, and ongoing monitoring and their work with their institutional review boards. This study would not be possible without them. We would also like to thank Dawn Dampier and Charles Knott of Battelle Research Inc. for their professionalism and excellent work.
Human Participant Protection This study was approved by the institutional review boards of Duke University and each of the separate study sites. All of the participants provided informed consent.
Peer Reviewed
Contributors K. Whetten was responsible for inclusion of the trust-related survey questions and the conceptualization of the analysis and was the primary author of the article. R. Whetten was responsible for conceptualization and editing of the article. J. Ostermann was responsible for conceptualization and statistical analyses. N. Thielman, M. Swartz, D. Stangl, and J. Leserman contributed to conceptualization and editing of the article.
References
- 1.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9: 208–220. [PMC free article] [PubMed] [Google Scholar]
- 2.Aday LA, Begley CE, Lairson DR, Slater CH. Evaluating the Medical Care System: Effectiveness, Efficiency, and Equity. Ann Arbor, Mich: Health Administration Press; 1993.
- 3.Goicoechea-Balbona AM. Culturally specific health care model for ensuring health care use by rural, ethnically diverse families affected by HIV/AIDS. Health Soc Work. 1997;22:172–180. [DOI] [PubMed] [Google Scholar]
- 4.Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. [PubMed]
- 5.Bogart LM, Thorburn S. Are HIV/AIDS conspiracy beliefs a barrier to HIV prevention among African Americans? J Acquir Immune Defic Syndr. 2005;38: 213–218. [DOI] [PubMed] [Google Scholar]
- 6.Dula A. African American suspicion of the health-care system is justified: what do we do about it? Camb Q Healthc Ethics. 1994;3:347–357. [DOI] [PubMed] [Google Scholar]
- 7.El-Sadr W, Capps L. The challenge of minority recruitment in clinical trials for AIDS. JAMA. 1992; 267:954–957. [PubMed] [Google Scholar]
- 8.Thomas SB, Quinn SC. The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the black community. Am J Public Health. 1991;81:1498–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kirp DL. Blood, sweat, and tears: the Tuskegee experiment and the era of AIDS. Tikkun. 1995;10:50. [PubMed] [Google Scholar]
- 10.Smith C. African Americans and the medical establishment. Mt Sinai J Med. 1999;66:280–281. [PubMed] [Google Scholar]
- 11.Bryan CS. Is there divine justice in AIDS? Why now, and not before? South Med J. 1990;83:199–202. [DOI] [PubMed] [Google Scholar]
- 12.Flaskerud JH. AIDS and traditional health beliefs and practices of black women. Nurs Res. 1989;38: 210–215. [PubMed] [Google Scholar]
- 13.Corbie-Smith G, Thomas SB, St. George MM. Distrust, race, and research. Arch Intern Med. 2002; 162:2458–2463. [DOI] [PubMed] [Google Scholar]
- 14.Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. J Gen Intern Med. 1999;14:537–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller ST, Seib HM, Dennie SP. African American perspectives on health care: the voice of the community. J Ambulatory Care Manage. 2001;24:37–44. [DOI] [PubMed] [Google Scholar]
- 16.Weisfeld A, Perlman RL. Disparities and discrimination in health care: an introduction. Perspect Biol Med. 2005;48(suppl 1):S1–S9. [PubMed] [Google Scholar]
- 17.HIV/AIDS Surveillance Report. Vol. 14. Atlanta, Ga: Centers for Disease Control and Prevention; 2002:Table 14.
- 18.HIV/AIDS Surveillance Report. Vol. 13. Atlanta, Ga: Centers for Disease Control and Prevention; 2001; 13:Table 2.
- 19.McNeil J, Sheffield JVL, Bartlett JG. Core elements of HIV primary care. In: A Guide to Primary Care for People With HIV/AIDS, 2004 Edition. Washington, DC: Health Resources and Services Administration; 2004:51–75.
- 20.Parry MF, Stewart J, Wright P, McLeod GX. Collaborative management of HIV infection in the community: an effort to improve the quality of HIV care. AIDS Care. 2004;16:690–699. [DOI] [PubMed] [Google Scholar]
- 21.McHorney CA, Ware JEJ, Lu JF, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994; 32:40–66. [DOI] [PubMed] [Google Scholar]
- 22.Wu AW, Hays RD, Kelly S, Malitz F, Bozzette SA. Applications of the Medical Outcomes Study: health related quality of life measures in HIV/AIDS. Qual Life Res. 1997;6:531–554. [DOI] [PubMed] [Google Scholar]
- 23.Wu AW, Revicki DA, Jacobson D, Malitz FE. Evidence for reliability, validity and usefulness of the Medical Outcomes Study HIV Health Survey (MOS-HIV). Qual Life Res. 1997;6:479–491. [DOI] [PubMed] [Google Scholar]
- 24.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Boston, Mass: New England Medical Center; 1993.
- 25.Ware JE, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Boston, Mass: New England Medical Center; 1994.