Abstract
Objectives. We examined whether perceived unfair treatment is associated with health conditions, whether social support moderates this association, and whether such relationships differ by location.
Methods. Data were derived from the 1998–1999 Filipino American Community Epidemiological Study, a cross-sectional investigation of 2241 Filipino Americans living in San Francisco and Honolulu. Negative binomial regression was used to examine potential 2-way and 3-way interactions between support, unfair treatment, and city (San Francisco vs Honolulu).
Results. Reports of unfair treatment were associated with increased illness after control for education, employment, acculturation, ethnic identity, negative life events, gender, and age. Furthermore, 2-way interactions were found between instrumental support and city, emotional support and city, and unfair treatment and city, and a 3-way interaction was shown between instrumental support, unfair treatment, and city.
Conclusions. Local contexts may influence the types of treatment encountered by members of ethnic minority groups, as well as their resources. These factors in turn may have implications for health disparities and well-being
Health disparities between population groups may arise when members of minority groups face a greater burden of stressors such as racial discrimination.1,2 Indeed, numerous cross-sectional and longitudinal studies have shown that perceived discrimination may promote illness.3–7
Despite much research, several unresolved questions remain; for example, there is limited knowledge about the factors that may buffer the relationship between discrimination and health and how context may influence experiences of discrimination. We examined the association between perceived discrimination and physical health conditions, assessed social support as a potential moderator of this association, and investigated whether relationships were constant by location.
BACKGROUND
Discrimination may have many effects, including lost economic opportunities, multi-generational trauma, hate crimes, and stress.6,8–12 In this study, we focused on potential stressful aspects, given that unfair treatment may be one of the most endemic and enduring stressors facing minority groups in the United States.13–15 Although everyone encounters slights, some events are socially patterned and happenstance. Among individuals of minority backgrounds, racial group membership may be a key reason for increased encounters with unfair treatment.16,17 Minority group members often report greater experiences of discrimination than Whites.18,19 Furthermore, these reports appear consequential, with numerous studies showing relationships between perceived discrimination and morbidity.5,13,20–23
One major premise of stress theory is that illness occurs when the magnitude of stressors experienced overcomes one’s ability to cope with them.24,25 Recent studies of perceived discrimination and morbidity buttress this proposition. Resources (e.g., racial salience) may moderate the strength of the association between perceived discrimination and well-being.26–30 Interestingly, social support may be an important coping resource, but it has been understudied as a buffer of discrimination stress.31,32
Social support refers to the resources people derive from their network ties. Support networks may provide emotional support (e.g., empathy) to mitigate the effects of discrimination. Discrimination may reflect an “othering” process whereby perpetrators reinforce the social exclusion of recipients.6 Emotional support may blunt this effect by demonstrating inclusion. Instrumental support (e.g., tangible aid) may include the resources to advocate against discrimination, as well as direct aid after discrimination-induced illness has occurred.
We focused on physical health conditions because previous research suggests that markers of physical health are associated with discrimination.3,5,33,34 In accord with observations that chronic stressors are generally stronger predictors of chronic health conditions than are acute life events, we anticipated that markers of routine discrimination would be more predictive of health conditions than measures of acute discrimination.7
Our major hypotheses were as follows: (1) Perceived discrimination will be associated with more adverse health conditions, (2) Measures of acute discrimination will be less predictive than measures of everyday discrimination, (3) Individuals perceiving greater social support will have fewer health conditions, and (4) Social support will moderate the association between discrimination and health conditions.
We tested these hypotheses among Filipino Americans because of their long history of migration to the United States and because, with a population of 2.4 million in the United States, they are the second largest Asian/Pacific Islander group in the country.35 Despite the growing size of this group, little work has been done to examine Filipino American health and well-being.36–41
REGIONAL DIFFERENCES
We also considered whether location makes a difference in the relationship between discrimination, social support, and health. Honolulu and San Francisco represent important destination points for Filipino migrants.35,42 Furthermore, both are areas where ethnic diversity predominates and where Asian Americans/Pacific Islanders represent a large percentage of the population (56% in Honolulu and 31% in San Francisco in 2000). Despite these similarities, there are reasons to suspect regional variations.
For example, racial tensions may vary geographically. Negative attitudes against minorities among Whites have been stronger in southern states than in others.19,43 White supremacist groups remain geographically clustered,44 and hate crime protections vary according to state and locality.6
Discrimination against Filipino Americans has been well documented.9,15,45–50 Although we are unaware of any studies directly comparing differences in discrimination between Filipinos living in the 2 study cities, there are reasons to suspect that differences may exist. The Filipino population is proportionally smaller in San Francisco (5%) than in Honolulu (12%), possibly leading to a greater likelihood of stereotyping and a smaller support base. Filipinos have greater representation in Hawaiian governance, suggesting greater empowerment. Also, more Filipinos in Honolulu (30%) than in San Francisco (13%) report multiple ethnicities, possibly reflecting greater tolerance on the island. These observations suggest that Filipinos living in Honolulu may be less likely to perceive discrimination than those living in San Francisco.
Social networks may also differ between these cities. Liu and colleagues argued that the 1965 Immigration Act (79 Stat 911) resulted in different developmental patterns for Filipinos in Hawaii compared with the continental United States.51 Whereas previous immigration legislation largely prohibited the entry of Asians into the United States, this new legislation allowed Asians and other immigrants to enter the country through 2 major pathways: family reunification and occupational preference. Filipinos have appeared to employ the reunification mechanism in Hawaii, whereas they have tended to use the occupational route on the continent. Consonant with these historical observations, Filipinos in Honolulu today appear to have greater kinship ties than Filipinos in San Francisco. According to our tabulations of the 2000 census, 95% of Filipinos in Honolulu lived in family households in that year, and 13% lived with grandchildren; the corresponding percentages in San Francisco were 86% and 10%.
These observations led us to inquire whether the relationship between discrimination and health may be stronger in San Francisco than Hawaii because Filipinos living in San Francisco may encounter a greater burden of discrimination. We also investigated whether the moderating effect of social support differs between the areas. Social support may be a more potent buffer in Honolulu because a richer social network there may provide greater protective resources for individuals experiencing discrimination. Alternatively, social support may have a greater moderating effect in San Francisco because there may be more discriminatory stress to buffer.
METHODS
We used data from the 1998–1999 Filipino American Community Epidemiological Study. The sampling scheme has been described in detail elsewhere28,52; it is summarized briefly here. One eligible person was randomly selected within households meeting the inclusion criteria (Filipino heritage, age 18–65 years, residence in either San Francisco or Honolulu). Surveys were administered in English, Tagalog, or Ilocano. A total of 2285 interviews were completed; the response rate was 78%. Data were weighted to adjust for demographic variables and differential probabilities of selection within a household. Forty-four respondents were excluded owing to missing data, resulting in a final sample of 2241.
Measures
Our dependent variable was current health conditions, a composite formed from a checklist that comprised hypertension, high blood pressure, stroke, health failure, congestive heart conditions, angina, coronary artery disease, high blood sugar, diabetes, and other heart disease. This subset of items was derived from the Medical Outcomes Study.53–55 We excluded health conditions (e.g., trouble seeing) not previously associated with perceived unfair treatment. Results of supplemental analyses including the full checklist of Medical Outcomes Study items were consistent with those presented here.
We distinguished everyday discrimination from discriminatory events in an attempt to better understand the difference between perceptions of routine unfair treatment and more episodic occurrences. Everyday discrimination was a 9-item measure, adapted from the Detroit Area Study23,56 and based on the qualitative work of Essed57 and Feagin,16 of routine experiences of unfair treatment taking place during the preceding month. Although validity studies have not been completed, the measure has been found to be correlated with global self-reported health among African Americans, but not Whites, after control for sociodemographic factors and other stressors.56
Items included on this Likert scale (1 = never, 5 = very often) were as follows: perceptions of “prejudice and discrimination from others”; being treated with less “courtesy” and less “respect”; “receiving poorer service at restaurants or stores”; people acting as if they are “afraid of you,” as if “they think you are dishonest,” or as if they are “better than you are”; being “called names or insulted”; and being “threatened or harassed.” Respondents were free to attribute these experiences to racial, ethnic, or other characteristics. Higher values indicate greater frequency of unfair treatment. In this study, the scale’s Cronbach alpha coefficient was 0.88.
Discriminatory events was a count of endorsements to being “treated unfairly or badly” during the preceding 12 months because of the respondent’s race or ethnicity, speaking a different language, or speaking with an accent. This measure of acute experiences of discrimination has been shown to be correlated with mental health and health service use among Chinese Americans after control for sociodemographic and general stress variables.58
City was a dichotomous variable, 1 indicating San Francisco and 0 indicating Honolulu. Social support was measured with 2 indicators adapted from previous work.25,59 Emotional support from family members, relatives, and friends was a 12-item scale scored from 1 (least) to 4 (most). Respondents were asked the extent to which their network members “really care about you”; “understand the way you feel about things”; “appreciate you”; “help you out in a crisis, even though they would have to go out of their way”; and “talk about your worries.”
Instrumental support was measured with a 12-item scale scored from 1 (least) to 5 (most). Respondents were asked how likely members of their support networks would be to do things such as loan them $100, look after their home or apartment, help with repairs, or drive them somewhere. Cronbach alpha coefficients were 0.92 and 0.94 for the emotional and instrumental support scales, respectively.
Several control variables were included as well. Negative life events accounted for the possibility that perceptions of discrimination tapped into more general life stressors as opposed to unfair treatment. Events were measured with a composite of 35 items that included death of a spouse, being fired, and moving to a worse neighborhood. Higher values indicated more negative events over the past 12 months. Similar measures have been used in studies of stress and coping60 and have been shown to correlate with health and mental health outcomes after control for sociodemographic variables and measures of discrimination.56,58
Ethnic identity was included because it may moderate the relationship between perceived discrimination and mental health among Filipinos.28 Ethnic identity was measured with a 9-item scale derived from the Multigroup Ethnic Identity Measure.61 Representative items included “I have a strong sense of belonging to the Filipino community” and “I participate in Filipino cultural practices, such as special food, music, or customs.” This 4-point Likert scale (1 = strongly disagree, 4 = strongly agree) had good interitem reliability (Cronbach alpha = 0.74). Higher scores indicate greater ethnic identity. The instrument has been reported to have good psychometric properties and concurrent validity and a good factor structure.61–64 In supplemental analyses (data not shown), we found that ethnic identity did not moderate the association between discrimination and health conditions and that this result did not vary by city.
Acculturation was measured with 2 indicators: (1) length of time in the United States measured number of years of residence in the country, and (2) daily language captured the language used by the respondent in daily conversation (“Filipino [Tagalog or Ilocano] only,” “Filipino and English,” or “English only”). Other control variables included age, gender (0 = male, 1 = female), education (in years), marital status (0 = not married, 1 = married), and employment status (0 = not employed/other, 1 = currently employed).
Exploratory analyses guided the specification of variables. We centered predictor variables as appropriate to facilitate interpretation of the intercept and to reduce multicollinearity.65 Because diagnostic analyses indicated overdispersion, we used negative binomial regression rather than Poisson regression in all of the multivariate analyses.66 Models became successively more complex, beginning with control variables and building to the 2-way and then 3-way interactions between support, perceived discrimination, and city. When an interaction was detected, conditional simple slopes were calculated and tested against the null hypothesis that the slopes were 0 and against the hypothesis that the slopes differed from each other.65
RESULTS
There were no geographic differences in health conditions, length of time in the United States, gender, or marital status (Table 1 ▶). However, in comparison with respondents in Honolulu (n = 1281), those in San Francisco (n = 960) reported more everyday discrimination, discriminatory events, instrumental support, use of English, and negative life events. In addition, they were younger overall and reported more years of education, higher levels of employment, less emotional support, and scored lower on ethnic identity.
TABLE 1—
Sample Descriptive Statistics, by City: Filipino American Community Epiemiological Study, 1998–1999
| Measure | San Francisco (n = 960) | Honolulu (n = 1281) | Total Sample (n = 2241) |
| Health conditions composite score, mean (SD) (range: 0–6) | 0.36 (0.71) | 0.31 (0.69) | 0.33 (0.70) |
| Demographic characteristics | |||
| Age, y, mean (SD) | 40.47** (13.35) | 42.39 (13.15) | 41.57 (13.30) |
| Female, % | 51.91 | 49.80 | 50.70 |
| Marital status, % | |||
| Single | 27.35 | 24.47 | 25.70 |
| Widowed/separated/divorced | 15.64 | 15.23 | 15.41 |
| Married | 57.01 | 60.29 | 58.89 |
| Acculturation | |||
| Years in US (range: 0–65), mean (SD) | 19.08 (11.25) | 19.78 (15.2) | 19.48 (13.67) |
| Language spoken in household, % | |||
| Filipino | 17.88** | 40.12 | 30.62 |
| Filipino and English | 58.90** | 41.59 | 48.98 |
| English | 23.22* | 18.29 | 20.39 |
| Socioeconomic position | |||
| Years of education, mean (SD) | 14.38** (2.32) | 9.35 (5.6) | 11.5 (5.21) |
| Currently employed, % | 80.69** | 70.52 | 74.86 |
| Number of negative life events, mean (SD) (range: 0–16) | 1.7** (1.96) | 1.08 (1.62) | 1.34 (1.80) |
| Ethnic identity score, mean (SD) (range: 1–4) | 3.48** (0.47) | 3.61 (0.47) | 3.55 (0.47) |
| Social support score, mean (SD) | |||
| Emotional support (range: 1–4) | 3.42** (0.56) | 3.64 (0.45) | 3.55 (0.51) |
| Instrumental support (range: 1–5) | 4.12** (0.82) | 3.93 (0.71) | 4.01 (0.76) |
| Everyday discrimination score, mean (SD) (range: 1–4.8) | 1.63** (0.65) | 1.19 (0.41) | 1.38 (0.56) |
| Number of discriminatory events, mean (SD) (range: 0–3) | 0.17** (0.74) | 0.09 (0.46) | 0.17 (0.60) |
Note. Significance levels refer to differences between San Francisco and Honolulu.
* P < .01; **P < .001.
Table 2 ▶ displays the results of the multivariate analyses. Model 1 included age, gender, length of time in the United States, language, education, employment, negative life events, ethnic identity, and emotional and instrumental social support. Age and negative life events predicted more physical health conditions, whereas emotional support, employment, and use of the Filipino language (compared with English) were associated with fewer health conditions. Model 2 added the 2 perceived unfair treatment measures. Everyday discrimination was associated with health conditions, whereas discriminatory events were not. Model 3 added city, for which there was no significant main effect. (In the discussion of subsequent models, “discrimination” refers to everyday discrimination only.)
TABLE 2—
Results of Negative Binomial Regression Analysis of Health Conditions: Filipino American Community Epidemiological Study, 1998–1999
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | Model 9 | Model 10 | |
| Age | 0.059*** (0.004) | 0.060*** (0.004) | 0.060*** (0.004) | 0.059*** (0.004) | 0.060*** (0.004) | 0.060*** (0.004) | 0.059*** (0.004) | 0.034*** (0.003) | 0.033*** (0.003) | 0.058*** (0.004) |
| Female gender | −0.083 (0.091) | −0.065 (0.092) | −0.073 (0.092) | −0.097 (0.092) | −0.075 (0.092) | −0.077 (0.092) | −0.100 (0.092) | 0.234*** (0.064) | 0.234*** (0.064) | −0.101 (0.093) |
| Years in US | 0.002 (0.003) | 0.002 (0.003) | 0.003 (0.003) | 0.004 (0.003) | 0.003 (0.003) | 0.003 (0.003) | 0.003 (0.003) | 0.001 (0.003) | 0.002 (0.003) | 0.004 (0.003) |
| Filipino language | −0.487** (0.169) | −0.517** (0.168) | −0.499** (0.169) | −0.479** (0.169) | −0.482** (0.169) | −0.498** (0.169) | −0.466** (0.169) | −0.341** (0.111) | −0.306** (0.110) | −0.447** (0.169) |
| Both languages | −0.128 (0.140) | −0.163 (0.139) | −1.68 (0.139) | −1.63 (0.139) | −1.80 (0.139) | −0.180 (0.139) | −0.165 (0.139) | −0.145 (0.091) | −0.137 (0.090) | −0.161 (0.138) |
| Education | 0.014 (0.010) | 0.012 0.010) | 0.004 (0.011) | 0.006 (0.011) | 0.005 (0.011) | 0.001 (0.011) | 0.003 (0.011) | −0.006 (0.007) | 0.000 (0.007) | 0.009 (0.011) |
| Employment | −0.376*** (0.098) | −0.392*** (0.099) | −0.403*** (0.099) | −0.395*** (0.099) | −0.397*** (0.098) | −0.401*** (0.098) | −0.389*** (0.098) | −0.393*** (0.069) | −0.379*** (0.068) | −0.393*** (0.098) |
| Negative life events | 0.100*** (0.023) | 0.085*** (0.023) | 0.083*** (0.023) | 0.075*** (0.022) | 0.080*** (0.023) | 0.080*** (0.024) | 0.073*** (0.022) | 0.070*** (0.016) | 0.074*** (0.016) | 0.075*** (0.022) |
| Ethnic identity | 0.195 (0.105) | 0.217* (0.105) | 0.230* (0.106) | 0.261* (0.106) | 0.230* (0.106) | 0.241* (0.107) | 0.262* (0.107) | 0.057 (0.065) | 0.036 (0.065) | 0.235* (0.105) |
| Emotional support | −0.318*** (0.094) | −0.284** (0.098) | −0.266** (0.099) | −0.273** (0.098) | −0.264** (0.100) | −0.465*** (0.144) | −0.400** (0.144) | −0.387*** (0.065) | −0.323*** (0.067) | −0.222* (0.103) |
| Instrumental support | 0.102 (0.069) | 0.092 (0.069) | 0.080 (0.069) | 0.075 (0.068) | 0.069 (0.069) | 0.050 (0.070) | 0.045 (0.069) | 0.163*** (0.050) | 0.368*** (0.066) | 0.186* (0.094) |
| Everyday discrimination | 0.197* (0.083) | 0.171* (0.085) | 0.430*** (0.117) | 0.218* (0.086) | 0.186* (0.086) | 0.407*** (0.117) | 0.213*** (0.058) | 0.215*** (0.057) | 0.432*** (0.118) | |
| 12-month discrimination | 0.031 (0.074) | 0.024 (0.075) | 0.030 (0.075) | 0.010 (0.074) | 0.017 (0.075) | 0.014 (0.075) | 0.050 (0.048) | 0.048 (0.047) | 0.037 (0.074) | |
| San Francisco | 0.168 (0.116) | 0.169 (0.112) | 0.170 (0.115) | 0.208 (0.116) | 0.200 (0.112) | 0.282*** (0.081) | 0.262*** (0.080) | 0.155 (0.110) | ||
| D _ SF | −0.423** (0.147) | −0.351* (0.158) | −0.412** (0.150) | |||||||
| D _ ES | 0.247 (0.145) | 0.315 (0.267) | ||||||||
| SF _ ES | 0.365* (0.183) | 0.269 (0.180) | ||||||||
| D _ SF _ ES | −0.249 (0.311) | |||||||||
| D _ IS | −0.088 (0.061) | −0.277 (0.164) | ||||||||
| SF _ IS | −0.375*** (0.084) | −0.231 (0.122) | ||||||||
| D _ SF _ IS | 0.393* (0.197) | |||||||||
| Intercept | −1.281*** (0.091) | −1.213*** (0.090) | −1.280*** (0.105) | −1.275*** (0.103) | −1.275*** (0.104) | −1.286*** (0.104) | −1.259*** (0.101) | 0.002 (0.067) | 0.006 (0.066) | −1.236*** (0.102) |
Note. ES = emotional support; IS = instrumental support; D = everyday discrimination; SF = San Francisco. Coefficients shown are with standard errors in parentheses. An underscore indicates an interaction term.
* P < .05; **P < .01; ***P < .001.
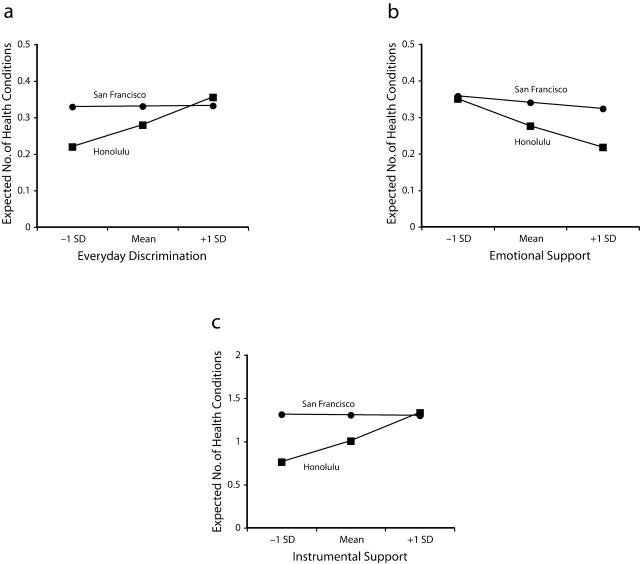
Model 4 added the interaction between discrimination and city. The significant interaction indicates that discrimination was associated with an increased number of health conditions in Honolulu but not in San Francisco (Figure 1a ▶). Models 5, 6, and 7, respectively, examined the 2-way interaction between discrimination and emotional support, the 2-way interaction between city and emotional support, and the 3-way interaction between discrimination, emotional support, and city. The only significant interaction was that between city and emotional support (model 6, Figure 1b ▶). Increased emotional support was associated with fewer health conditions in Honolulu, but there was no relationship between emotional support and health conditions in San Francisco.
FIGURE 1—
Relationships between health conditions and everyday discrimination (a), emotional support (b), instrumental support (c), by city.
Note. Shown are 2-way interactions with all covariates controlled. All of the slopes for Honolulu are statistically different from 0; none of the slopes for San Francisco are statistically significant.
Models 8, 9, and 10 examined the 2-way interaction between discrimination and instrumental support, the 2-way interaction between city and instrumental support, and the 3-way interaction between discrimination, city, and instrumental support. The interaction between discrimination and instrumental support was not significant. However, the interaction between instrumental support and city was significant (model 9, Figure 1c ▶): increased instrumental support was associated with more health conditions in Honolulu but not in San Francisco.
The significant 3-way interaction between discrimination, city, and instrumental support (model 10) is shown in Figure 2 ▶. “High” discrimination and “low” discrimination refer to 1 standard deviation above and below the mean, respectively.65 In San Francisco, reports of discrimination were not significantly associated with health conditions, regardless of level of instrumental support. Furthermore, instrumental support did not predict health conditions, regardless of level of discrimination.
FIGURE 2—
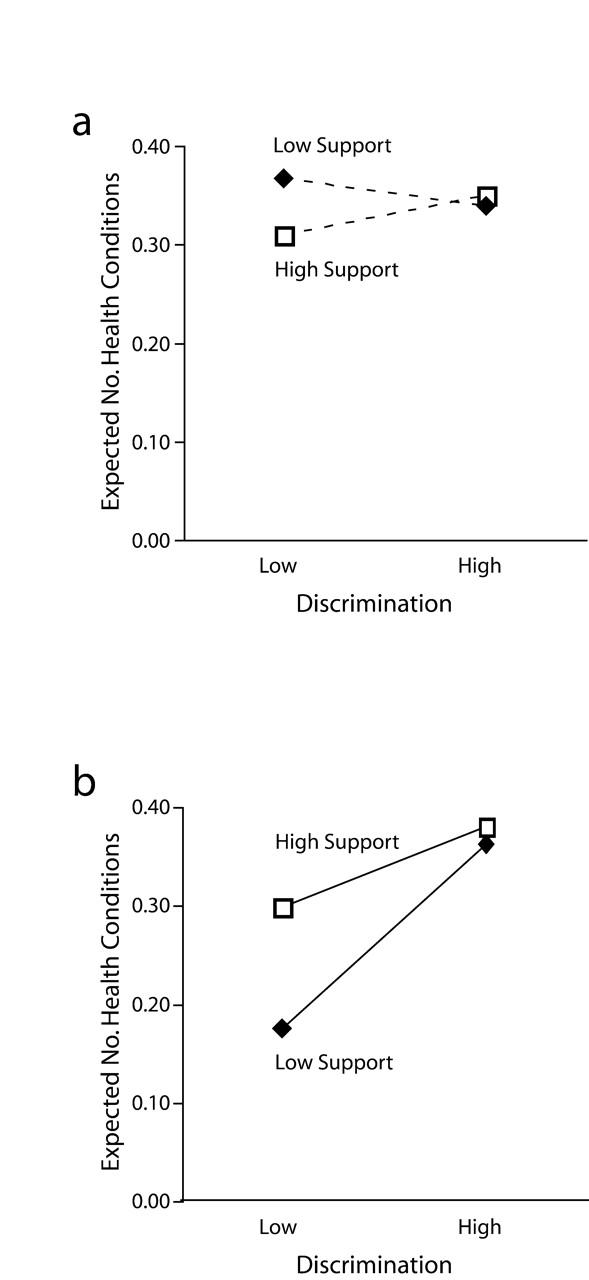
Relationships between everyday discrimination, instrumental support, and health conditions in San Francisco (a) and Honolulu (b).
Note. Shown are 3-way interactions with all covariates controlled. The slopes of solid lines are statistically different from 0; the slopes of dashed lines are not. “Low” refers to 1 standard deviation below the mean; “high” refers to 1 standard deviation above the mean.
In Honolulu, however, high levels of discrimination were associated with more health conditions than were low levels of discrimination. Also, individuals perceiving higher levels of instrumental support reported more health conditions than those with less support. Moreover, instrumental support moderated the association between discrimination and health. The conditional simple slope for discrimination was steeper for those with low levels of support (0.65; P >.001) than for those with higher levels of support (0.22; P >.001). At levels of discrimination 1 standard deviation below the mean, the expected number of conditions is about 2-fold higher among those with high support than among those with low support; conversely, at levels of discrimination 1 standard deviation above the mean, the difference in health conditions between those at high and low levels of instrumental support converges.
DISCUSSION
Consistent with our first hypothesis, discrimination showed a main effect on health, such that individuals perceiving discrimination reported more health conditions. Consonant with our second hypothesis, measures of everyday experiences involving unfair treatment were predictive of health, whereas measures of discriminatory events over the preceding year were not (conditional on each other and covariates). This is in accord with the observation that chronic stressors are more predictive of chronic illness than acute life events; it further suggests that health disparities may arise from differential exposures to stressors over the life course.2,7,67,68
Our third hypothesis received partial support. Considering main effects, increased emotional support was significantly associated with fewer health conditions, whereas instrumental support was not associated with health conditions. Other studies have also found emotional support to be a more consistent predictor of health than instrumental support.31,69 It may be that emotional support promotes health in a relatively global fashion, whereas instrumental support is influential under a more restricted set of conditions.59
Our fourth hypothesis, that social support moderates the association between discrimination and health conditions, was not supported by the 2-way interaction models. There were no significant interactions between instrumental support and everyday discrimination or between emotional support and everyday discrimination. Others have reported similarly inconsistent evidence regarding the buffering effects of social support on stressors.59
Context also may influence individual risk factors and the associations between risk factors and health. Filipinos living in San Francisco and Honolulu reported similar levels of health but differed in terms of several risk factors. Most pertinent for this study, Filipinos in San Francisco perceived greater discrimination and more instrumental support but less emotional support.
Considering first the 2-way interactions, we found that city significantly moderated everyday discrimination, instrumental support, and emotional support. Discrimination, instrumental support, and emotional support were not significant predictors of health conditions among Filipinos in San Francisco. In Honolulu, however, Filipinos reporting high levels of everyday discrimination and instrumental support had significantly more health conditions, and those reporting high levels of emotional support had fewer health conditions.
The 3-way interaction between city, instrumental support, and everyday discrimination adds further information. As with the 2-way interactions, discrimination and instrumental support did not predict health conditions in San Francisco. Also, we found no effect modification of instrumental support with discrimination in San Francisco.
However, a different picture emerged in Honolulu. Filipinos reporting higher levels of instrumental support had more health conditions than those reporting lower levels of support. In addition, those reporting more discrimination were at greater risk of illness than those reporting less discrimination. Furthermore, the association between discrimination and illness was stronger among those with less instrumental support than those with more support.
Altogether, the results of our study suggest that discrimination, emotional support, and instrumental support predict health conditions among Filipinos living in Honolulu but not in San Francisco. In Honolulu, reports of discrimination were associated with increased reports of health conditions, supporting the notion that routine experiences of unfair treatment may be a risk factor for illness.
The effects of social support in Honolulu paralleled the complexity of findings noted in several reviews.31,70 Receipt of emotional support was associated with a decreased risk of illness, whereas receipt of instrumental support was associated with an increased risk. The reason might be that emotional support provides ubiquitous protection in terms of health, whereas instrumental support may reflect the receipt of aid among those who have become ill. Furthermore, receipt of instrumental support may lead to feelings of guilt and distress among members of less wealthy networks.36
Consistent with the buffering hypothesis, the strength of association between discrimination and health conditions was weaker among individuals reporting high levels of instrumental support than among those reporting low levels. Studies of mental health outcomes have tested the buffering hypothesis directly (i.e., using interaction terms) and have generally found that coping resources moderate the effects of perceived discrimination.26,27,29,30,71 However, studies focusing on physical health have tested only the main effects of coping with discrimination.5,34 Thus, the present study contributes to the literature through its direct test of the buffering hypothesis with physical health conditions.
However, the data also indicate another possible interpretation. Individuals at lower levels of instrumental support and discrimination had fewer conditions than respondents at other levels of these factors, suggesting that instrumental support might be viewed as a marker of health risk (people who are sick need and receive more support) rather than as a buffering resource. From this perspective, the effect modification may reflect not the buffering hypothesis but, rather, the synergy associated with being at low risk. This explanation, although unclear, might reflect the accumulation of other contextual or lifestyle advantages. We were limited in our ability to examine this interpretation in that our cross-sectional data did not allow us to temporally establish whether illness leads to use of support and reports of discrimination (as implied by such an interpretation).70,72,73
Post hoc analyses suggested that the null findings in San Francisco might be explained by socioeconomic position, given that employment was one of the most robust predictors. Thus, in San Francisco, socioeconomic position may be more relevant than discrimination or social support in terms of health conditions. Because the socioeconomic position of Filipinos is complicated by remittance (i.e., they send a portion of their wages overseas),36 full exploration of socioeconomic position remains for a future study.
A few additional caveats should be mentioned. For example, our self-reported data did not capture “objective” experiences of discrimination, social support, or health conditions. Respondents may have overestimated or underestimated their actual experiences. Future researchers may wish to examine clinical outcomes and other health measures. Individual perceptions of discrimination also leave unexamined institutionalized and other forms of oppression.10,20 Although language and length of stay in the United States are commonly used measures of acculturation, they do not fully capture the acculturation process.
In addition, the context for our study was 2 metropolitan areas, leaving unanswered several questions about the relationship between city of residence and health mechanisms. More refined spatial units (e.g., census tracts) would permit a broader array of questions and methodological approaches (e.g., hierarchical linear models).74–76 Also, our findings may have been the product of sampling differences between the 2 cities. Replicating these analyses in other samples would help evaluate this possibility. Furthermore, the extent to which these findings are generalizable to Filipinos elsewhere or to other ethnic groups is unclear.
Granted these caveats, our study contributes to the knowledge base. First, we have added to the evidence showing that physical health conditions are associated with perceived discrimination.3,5,56 Second, we have demonstrated that everyday discrimination is a more likely predictor of health conditions than are acute discriminatory events. Third, we found evidence that social support may moderate the association between discrimination and health. Fourth, we have highlighted the importance of considering geographic context in understanding health risk factors.74,77–79 Finally, we examined an understudied population, Filipino Americans.
Social support and city of residence may moderate the association between perceived discrimination and physical health. Although we focused on individual-level stress processes, individual factors may be shaped by institutionalized forces.67,80–82 Examining context is one modest way of exploring these processes, but much work remains to determine how social forces contribute to individual experiences and health disparities.
Acknowledgments
This study was supported by the National Institute on Alcohol Abuse and Alcoholism (grant 098633 to David Takeuchi).
We thank Wendy Lin, Dawn Misra, and several anonymous reviewers for their helpful comments on previous versions of the article.
Human Participant Protection This study was approved by the institutional review board of the University of Washington. Participants provided informed consent.
Peer Reviewed
Contributors G. C. Gee originated the study and led the writing. J. Chen and D. Tran prepared the data and conducted the analyses. M. S. Spencer and D. Takeuchi helped with the writing of the article and provided technical guidance on the analyses. S. See and O. A. Kuester provided important insights about Filipino culture and history and assisted with the writing and revisions.
References
- 1.Clark R, Anderson A, Clark VR, Williams DR. Racism as a stressor for African Americans. Am Psychol. 1999;54:805–816. [DOI] [PubMed] [Google Scholar]
- 2.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis. 1992;2:207–221. [PubMed] [Google Scholar]
- 3.Harrell JP, Hall S, Taliaferro J. Physiological responses to racism and discrimination: an assessment of the evidence. Am J Public Health. 2003;93:243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caughy MO, O’Campo PJ, Muntaner C. Experiences of racism among African American parents and the mental health of their preschool-aged children. Am J Public Health. 2004;94:2118–2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. Am J Public Health. 1996;86:1370–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv. 1999;29: 295–352. [DOI] [PubMed] [Google Scholar]
- 7.Williams DR, Neighbors H, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93:200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Research Council, Panel on Methods for Assessing Discrimination. Measuring Racial Discrimination. Washington, DC: National Academy Press; 2004.
- 9.Feagin JR. Racist America: Roots, Current Realities, and Future Reparations. New York, NY: Routledge; 2000.
- 10.Meyer IH. Prejudice as stress: conceptual and measurement problems. Am J Public Health. 2003;93: 262–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Geronimus AT. To mitigate, resist, or undo: addressing structural influences on the health of urban populations. Am J Public Health. 2000;90:867–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;27:146–161. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Michelson KD, Williams DR. The prevalence, distribution and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–230. [PubMed] [Google Scholar]
- 14.Ong PM. The Asian American challenge to race relations. In: Ong PM, ed. The State of Asian Pacific America: Transforming Race Relations. Los Angeles, Calif: Leadership for Asian Pacifics Inc; 2005:13–39.
- 15.Okihiro G. The Columbia Guide to Asian America History: A Resource Guide to Asian American Literature. New York, NY: Columbia University Press; 2001.
- 16.Feagin JR. The continuing significance of race: antiblack discrimination in public places. Am Sociol Rev. 1991;56:101–116. [Google Scholar]
- 17.Jones CP. Levels of racism: a theoretical framework and gardener’s tale. Am J Public Health. 2000;90: 1212–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.LaVeist TA, Rolley NC, Daila C. Prevalence and patterns of discrimination among US health care consumers. Int J Health Serv. 2003;33:331–344. [DOI] [PubMed] [Google Scholar]
- 19.Schuman H, Steeh C, Bobo L. Racial Attitudes in America: Trends and Interpretations. Cambridge, Mass: Harvard University Press; 1985.
- 20.Gee GC. A multilevel analysis of the relationship between institutional racial discrimination and health status. Am J Public Health. 2002;92:615–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson JS, Brown TN, Williams DR, Torres M, Sellers SL, Brown K. Racism and the physical and mental health status of African Americans: a thirteen year national panel study. Ethn Dis. 1996;6:132–147. [PubMed] [Google Scholar]
- 22.Pavalko E, Mossakowski KN, Hamilton V. Does perceived discrimination affect health? Longitudinal relationships between work discrimination and women’s physical and emotional health. J Health Soc Behav. 2003;44:18–34. [PubMed] [Google Scholar]
- 23.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socioeconomic status, stress, and discrimination. J Health Psychol. 1997;2:335–351. [DOI] [PubMed] [Google Scholar]
- 24.Lazarus RS, Folkman S. Stress, Appraisal and Coping. New York, NY: Springer; 1984.
- 25.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- 26.Noh S, Beiser M, Kaspar V, Hou F, Rummens J. Perceived racial discrimination, depression, and coping: a study of Southeast Asian refugees in Canada. J Health Soc Behav. 1999;40:193–207. [PubMed] [Google Scholar]
- 27.Noh S, Kaspar V. Perceived discrimination and depression: moderating effects of coping, acculturation and ethnic support. Am J Public Health. 2003;93: 232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mossakowski KN. Coping with perceived discrimination: does ethnic identity protect mental health? J Health Soc Behav. 2003;44:318–331. [PubMed] [Google Scholar]
- 29.Sellers R, Shelton JN. The role of racial identity in perceived racial discrimination. J Pers Soc Psychol. 2003;84:1079–1092. [DOI] [PubMed] [Google Scholar]
- 30.Sellers RM, Caldwell CH, Schmeelk-Cone KH, Zimmerman MA. Racial identity, racial discrimination, perceived stress, and psychological distress among African American young adults. J Health Soc Behav. 2003;44:302–317. [PubMed] [Google Scholar]
- 31.Berkman LF, Glass T. Social integration, social networks, social support, and health. In: Berkman LF, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press Inc; 2000:137–173.
- 32.Berkman LF, Clark C. Neighborhoods and networks: the construction of safe places and bridges. In: Kawachi I, Berkman LF, eds. Neighborhoods and Health. New York, NY: Oxford University Press Inc; 2003: 288–302.
- 33.Armstead CA, Lawler KA, Gordon G, Cross J, Gibbons J. Relationship of racial stressors to blood pressure responses and anger expression in Black college students. Health Psychol. 1989;8:541–556. [DOI] [PubMed] [Google Scholar]
- 34.Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990;30: 1273–1281. [DOI] [PubMed] [Google Scholar]
- 35.Lai E, Arguelles D, eds. The New Face of Asian Pacific America: Numbers, Diversity and Change in the 21st Century. San Francisco, Calif: AsianWeek; 2004.
- 36.Agbayani-Siewert P, Revila L. Filipino Americans. Newbury Park, Calif: Sage Publications; 1995.
- 37.Chen MS Jr, Hawks BL. A debunking of the myth of healthy Asian Americans and Pacific Islanders. Am J Health Promotion. 1995;9:261–268. [DOI] [PubMed] [Google Scholar]
- 38.Ghosh C. Healthy People 2010 and Asian Americans/Pacific Islanders: defining a baseline of information. Am J Public Health. 2003;93:2093–2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ro M. Moving forward: addressing the health of Asian American and Pacific Islander women. Am J Public Health. 2002;92:516–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Srinivasan S, Guillermo T. Toward improved health: disaggregating Asian American and Native Hawaiian/Pacific Islander data. Am J Public Health. 2000; 90:1731–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yu ESH, Liu WT. US national health data on Asian Americans and Pacific Islanders: a research agenda for the 1990s. Am J Public Health. 1992;82: 1645–1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chan S. Asian Americans: An Interpretive History. Boston, Mass: Twayne Publishers; 1991.
- 43.Firebaugh G, Davis KE. Trends in antiblack prejudice, 1972–1984: region and cohort effects. Am J Sociol. 1988;94:251–272. [Google Scholar]
- 44.Flint C. Introduction. In: Flint C, ed. Spaces of Hate: Geographies of Discrimination and Intolerance in the USA. New York, NY: Routledge; 2004:1–20.
- 45.Abel EK. “Only the best class of immigration”: public health policy toward Mexicans and Filipinos in Los Angeles, 1910–1940. Am J Public Health. 2003; 93:932–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zia H. Asian American Dreams: The Emergence of an American People. New York, NY: Farrar Straus & Giroux; 2000.
- 47.Enriquez V. From Colonial to Liberation Psychology: The Philippine Experience. Manila, the Philippines: DeLaSalle University Press; 1994.
- 48.Jung MK. Interracialism: the ideological transformation of Hawaii’s working class. Am Sociol Rev. 2003; 94:373–400. [Google Scholar]
- 49.San Juan E Jr. Configuring the Filipino diaspora in the United States. Diaspora. 1994;2:117–133. [Google Scholar]
- 50.Ngai MM, Lee J, Lim I, Matsukawa Y. From colonial subject to undesirable alien: Filipino migration, exclusion, and repatriation, 1920–1940. In: Lee J, Lim I, Matsukawa Y, eds. Re/Collecting Early Asian America. Philadelphia, Pa: Temple University Press; 2002: 111–126.
- 51.Liu JM, Ong PM, Rosenstein C. Dual chain migration: post-1965 Filipino immigration to the United States. Int Migration Rev. 1991;25:487–513. [PubMed] [Google Scholar]
- 52.Gong F, Gage S-J, Tacata LA. Helpseeking behavior among Filipino Americans: a cultural analysis of face and language. J Community Psychol. 2003;31: 469–488. [Google Scholar]
- 53.Alonso J, Ferrer M, Bandek B, et al. Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004;13:283–289. [DOI] [PubMed] [Google Scholar]
- 54.Stewart AL, Greenfield S, Hays RD, et al. Functional status and well-being of patients with chronic conditions: results from the Medical Outcomes Study. JAMA. 1989;262:907–913. [PubMed] [Google Scholar]
- 55.Ware JE. The status of health assessment. Annu Rev Public Health. 1994;16:327–354. [DOI] [PubMed] [Google Scholar]
- 56.Williams DR, Spencer MC, Jackson JS. Race, stress and physical health: the role of group identity. In: Contrada RJ, Ashmore RD, eds. Self, Social Identity, and Physical Health. New York, NY: Oxford University Press Inc; 1999:71–100.
- 57.Essed P. Understanding Everyday Racism. Newbury Park, Calif: Sage Publications; 1992.
- 58.Spencer MS, Chen J. Discrimination and mental health service use among Chinese Americans. Am J Public Health. 2004;94:809–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Israel BA, Farquhar S, James SA, Schulz AM, Parker EA. The relationship between social support, stress, and health among women on Detroit’s East Side. Health Educ Behav. 2002;29:342–360. [DOI] [PubMed] [Google Scholar]
- 60.Kessler RC. The effects of stressful life events on depression. Annu Rev Psychol. 1997;48:191–214. [DOI] [PubMed] [Google Scholar]
- 61.Phinney J. The Multigroup Ethnic Identity Measure: a new scale for use with adolescents and young adults from diverse groups. J Adolesc Res. 2004;7: 156–176. [Google Scholar]
- 62.Phinney JS, Alipuria LL. At the interface of cultures: multiethnic/multiracial high school and college students. J Soc Psychol. 1996;136:139–158. [DOI] [PubMed] [Google Scholar]
- 63.Spencer MC, Icard L, Harachi T, Catalano R, Oxford M. Ethnic identity among monoracial and multiracial early adolescents. J Early Adolescence. 2000;20: 365–387. [Google Scholar]
- 64.Robers RE, Phinney JS, Masse LC, Chen YR, Roberts CR, Romero A. The structure of ethnic identity of young adolescents from diverse ethnocultural groups. J Early Adolescence. 1999;19:301–332. [Google Scholar]
- 65.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, Calif: Sage Publications; 1991.
- 66.Long JS. Regression Models for Categorical and Limited Dependent Variables. Thousand Oaks, Calif: Sage Publications; 1997.
- 67.James SA. John Henryism and the health of African Americans. Cult Med Psychiatry. 1994;18: 163–182. [DOI] [PubMed] [Google Scholar]
- 68.Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42:589–597. [DOI] [PubMed] [Google Scholar]
- 69.House J, Kahn R. Measures and concepts of social support. In: Cohen S, Syme SL, eds. Social Support and Health. Orlando, Fla: Academic Press Inc; 1985: 83–108.
- 70.Antonucci TC. Social relations: an examination of social networks, social support, and sense of control. In: Birren JE, Schaie KW, eds. Handbook of Psychology of Aging. New York, NY: Academic Press Inc; 2001: 427–445.
- 71.Moskowitz JM, Lin Z, Hudes ES. The impact of workplace smoking ordinances in California on smoking cessation. Am J Public Health. 2000;90:757–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Link BG, Phelen JC, Bresnahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am J Public Health. 1999;89:1328–1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gallant MP. The influence of social support on chronic illness self-management: a review and directions for research. Health Educ Behav. 2003;32:170–195. [DOI] [PubMed] [Google Scholar]
- 74.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21:171–192. [DOI] [PubMed] [Google Scholar]
- 75.Gee GC, Takeuchi DT. Traffic stress, vehicular burden and well-being: a multilevel analysis. Soc Sci Med. 2004;59:405–414. [DOI] [PubMed] [Google Scholar]
- 76.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Thousand Oaks, Calif: Sage Publications; 2002.
- 77.Ross CE, Jang SJ. Neighborhood disorder, fear, and mistrust: the buffering role of social ties with neighbors. Am J Community Psychol. 2000;28: 401–420. [DOI] [PubMed] [Google Scholar]
- 78.Gee GC, Payne-Sturges DC. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2004; 112:1645–1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and injury mortality: individual and neighborhood determinants. J Epidemiol Community Health. 2000;54:517–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.James SA, Keenan NL, Strogatz DS, Browning SR, Garrett JM. Socioeconomic status, John Henryism, and blood pressure in black adults: the Pitt County Study. Am J Epidemiol. 1992;135:59–67. [DOI] [PubMed] [Google Scholar]
- 81.James SA, Strogatz DS, Wing SB, Ramsey DL. Socioeconomic status, John Henryism, and hypertension in blacks and whites. Am J Epidemiol. 2004;126: 664–673. [DOI] [PubMed] [Google Scholar]
- 82.Pearlin LI. The sociological study of stress. J Health Soc Behav. 1989;30:241–256. [PubMed] [Google Scholar]