Abstract
Interventions that have proven effective in the management of chronic illness have often been difficult to establish in widespread practice. The Chronic Care Model provides a framework for implementing interventions, but it is expensive and difficult to implement.
We developed a decision support system based on this model to improve the care of adults who have diabetes and receive primary care in Vermont or adjacent New York. The Vermont Diabetes Information System uses a network of community laboratories for providing data to produce flowsheets, reminders, action alerts, and population reports that are sent to primary care providers by fax and to patients by mail. Currently, 7295 patients are cared for by 124 primary care providers in 62 practices and are enrolled in a randomized controlled trial to study its effects.
Despite evidence that optimal diabetes care can result in reduced complications and improved economic outcomes, such care is often not achieved. A recent study of outcomes among diabetic patients by the National Health and Nutrition Examination Survey found that 37% had poor glycemic control (hemoglobin A1C > 8%), 40% had blood pressure values greater than 140/90 mm Hg, and more than 50% had cholesterol levels greater than 200 mg/dL.1 Only 7.3% of patients surveyed were on target for all 3 indicators. Similar problems have been found when translating guidelines into practice for a wide variety of other conditions, such as hypertension, congestive heart failure, and cancer screening.
The Chronic Care Model was developed as a framework for approaching the management of chronic illness from a public health perspective.2–4 It emphasizes the importance of bringing together—for an ideal clinical encounter—a prepared, proactive health care team and an informed, activated patient. Chronic disease registries allow for a population-based view of patients and are a central component of this model. However, the model has proved expensive and difficult to fully implement in practice. Because other implementations of the Chronic Care Model require substantial investment by the practice and major changes in the providers’ usual activities, we designed the Vermont Diabetes Information System (VDIS) to require a minimum of effort and no new financial resources on the part of the providers.5
PROGRAM DESCRIPTION
The VDIS is a decision support system designed to help primary care providers and their diabetes patients achieve guideline-based treatment targets. It has 5 defining characteristics: (1) use of the Chronic Care Model as an organizing frame-- work, (2) daily data feeds from otherwise independent laboratories, (3) automatic test interpretation with algorithms on the basis of consensus guidelines, (4) use of fax and mail to report to providers and patients not easily reached by electronic networks, and (5) report formats that are accessible and useful to patients and providers. The primary function of the system is to collect pertinent clinical information and then provide accurate and timely flow sheets, reminders, alerts, and population reports for providers and their diabetes patients. The intended effects of the interventions are shown in Table 1 ▶; an example of a provider flow sheet with trended lab results and decision support is shown in Figure 1 ▶. Providers receive confidential quarterly population reports that display their panel of diabetes patients, who are sorted by degree of hyperglycemia, hyperlipidemia, and proteinuria.
TABLE 1—
Anticipated Effects of Vermont Diabetes Information System Interventions
| Intervention | Anticipated Effect |
| Directed at the practice and primary care provider | |
| Faxed lab flow sheets with recent test results and guideline-based recommendations. | Provide decision support and stimulate appropriate action by provider. |
| Faxed reminders when patients are overdue for recommended lab testing. | Stimulate follow-up of patients who are lost to follow-up or otherwise overdue. |
| Mailed quarterly population reports with report cards of provider performance and lists of patients sorted by degree of control on the basis of lab tests. | Provide the provider a population-based individual view of his or her entire diabetes patient roster for targeted case management. Allow provider to keep roster of patients up to date. Peer comparison may motivate a practice to modify office processes for chronic illness management. |
| Directed at the patient | |
| Mailed alerts when a lab test result is above guideline-based threshold. | Engage and activate patients to know and understand the goals of therapy and to be prepared for interaction with the provider. |
| Mailed reminders when patients are overdue for recommended lab testing. | Remind patient to schedule follow-up testing or an office visit. |
FIGURE 1—
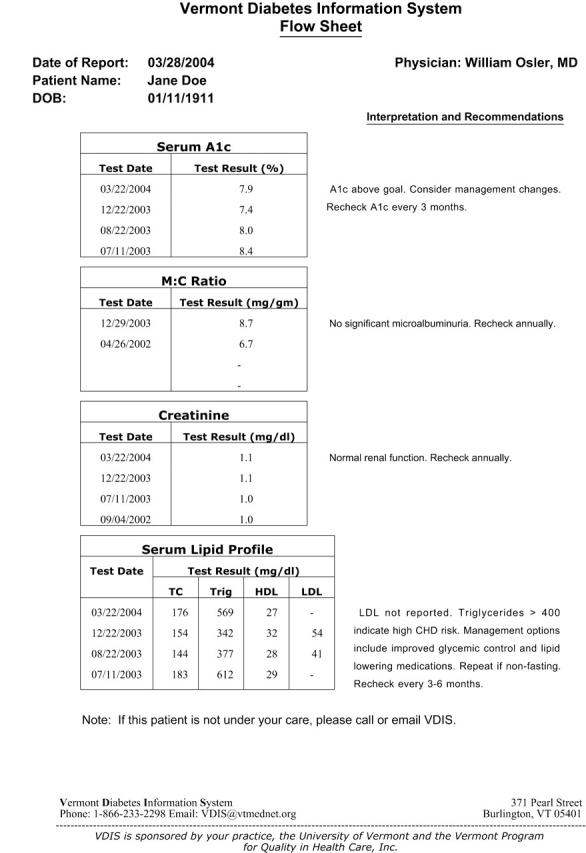
Example of a decision support flow sheet.
Our goal was to develop registry capability that requires a minimum of effort by already overburdened office practices. We chose to leverage the laboratory results because (1) they are primary treatment targets highlighted in clinical guidelines, (2) they are available in relatively simple electronic format, and (3) they are an important point of interaction between the provider and the patient.
An Oracle database was developed as a custom software application and is maintained by staff from the information systems department of the academic medical center. We wrote the clinical algorithms on the basis of the American Diabetes Association Clinical Practice Recommendations. The next step involved reaching out to providers and patients. We first recruited clinical laboratories to establish an electronic link between the lab and the VDIS. Practices that use a participating lab were then recruited. The laboratories provided the primary care providers with lists of their patients who had had an A1C test during the previous 2 years. The primary care providers reviewed their lists and deleted patients who were not under their care or were not diabetic. Eligible patients were invited by mail to participate in the study.
Population Served
The VDIS serves diabetes patients who use primary care practices. More than 97% of invited subjects agreed to participate. Eleven labs are currently linked to the system, with flowsheets, alerts, and reminders being generated for 7295 patients who are cared for by 124 physicians, nurse practitioners, or physician assistants in 62 practices.
DISCUSSION
Diabetes is an ideal condition for a registry-based system: the condition is common, complex, and important to patients and providers; the guidelines are well known and respected; and there is considerable room for improvement in clinical care.
Evaluation of the VDIS is being conducted with a randomized controlled trial supported by the National Institutes of Health. Two years of observation were planned and are expected to end in late 2006. Randomization occurred at the practice level, and we have learned several important lessons thus far.
Widely disparate clinical labs can be recruited to contribute data to a central database for quality improvement efforts. One of the motivating factors for labs to participate is that they are able to provide “value-added” lab reports to their customers.
Tools that are designed to help providers must be well integrated into the daily workflow of the practice. Primary care providers are very busy, and interventions that require extra effort by the practice are less likely to be successful. The weakest point of the system is the requirement that primary care providers review their lists of potential subjects.
The median primary care provider panel size of diabetes patients is 83, which is lower than most primary care providers anticipated. This small number allows the primary care provider to use the population report for easy identification of patient outliers who may be eligible for individualized management strategies.
At an average follow-up of 12 months, we have found improvements in test-ordering frequency for A1C, lipids, and urinary microalbumin, although it is too early to evaluate whether there have been improvements in physiological control.
Estimated costs for a long-term, large-scale implementation of the system are approximately $1 per patient per month.
Next Steps
The next steps in the VDIS study are to complete the randomized trial. The primary outcome is the comparison of glycemic control between the control and the intervention groups. Results are expected in 2007. Assuming positive results, the system should be generalizable to other settings and conditions.
KEY FINDINGS
In the absence of a consistent electronic health record, laboratory data can be leveraged to provide decision support for patients who are cared for in a community primary care setting.
This decision support functionality is feasible in any setting where a complete laboratory record can be obtained in a timely manner.
Periodic population reports require only a complete lab record and are less dependant on the timely transfer of data.
Acknowledgments
This study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (grants R01 DK61167 and K24 DK068380). We would like to acknowledge the participation of the clinical laboratories, practice staff, primary care providers, and patients who helped make this project possible.
Human Participant Protection This study was approved by the University of Vermont’s institutional review board.
Peer Reviewed
Contributors All the authors designed the study. C. D. MacLean analyzed the data and was the primary author. B. Littenberg analyzed data and edited the article. M. Gagnon also edited the article.
References
- 1.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291: 335–342. [DOI] [PubMed] [Google Scholar]
- 2.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA. 2002;288:1909–1914. [DOI] [PubMed] [Google Scholar]
- 3.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779. [DOI] [PubMed] [Google Scholar]
- 4.Glasgow RE, Wagner EH, Kaplan RM, Vinicor F, Smith L, Norman J. If diabetes is a public health problem, why not treat it as one? A population-based approach to chronic illness. Ann Behav Med. 1999;21:159–170. [DOI] [PubMed] [Google Scholar]
- 5.MacLean CD, Littenberg B, Gagnon MS, Reardon M, Turner PD, Jordan C. The Vermont Diabetes Information System (VDIS): study design and subject recruitment for a cluster randomized trial of a decision support system in a regional sample of primary care practices. Clin Trials. 2004;1:532–544. [DOI] [PMC free article] [PubMed] [Google Scholar]


