Abstract
Objectives. We examined factors contributing to shifts in primary cesarean rates in the United States between 1991 and 2002.
Methods. US national birth certificate data were used to assess changes in primary cesarean rates stratified according to maternal age, parity, and race/ethnicity. Trends in the occurrence of medical risk factors or complications of labor or delivery listed on birth certificates and the corresponding primary cesarean rates for such conditions were examined.
Results. More than half (53%) of the recent increase in overall cesarean rates resulted from rising primary cesarean rates. There was a steady decrease in the primary cesarean rate from 1991 to 1996, followed by a rapid increase from 1996 to 2002. In 2002, more than one fourth of first-time mothers delivered their infants via cesarean. Changing primary cesarean rates were not related to general shifts in mothers’ medical risk profiles. However, rates for virtually every condition listed on birth certificates shifted in the same pattern as with the overall rates.
Conclusions. Our results showed that shifts in primary cesarean rates during the study period were not related to shifts in maternal risk profiles.
A long-term rise in cesarean rates in the United States began in the mid-1960s and continued to the late 1980s, drawing national attention starting in the late 1970s that focused on reducing the number of cesarean births.1 The American College of Obstetricians and Gynecologists (ACOG) directed particular attention toward increasing the number of vaginal births after cesarean (VBACs) and issued guidelines in 1988 and 1991 that contributed to the heightened use of VBACs,2 after which the overall cesarean birth rate steadily decreased until 1996.3 Notably, the US rate was declining at the same time that national rates in most other industrialized countries were increasing.4 Largely not noted was that whereas VBAC rates rose to an all-time high in 1996, rates of primary cesareans (i.e., cesarean deliveries among women with no previous such deliveries) declined in a comparable, but inverse, pattern.3
As VBAC rates peaked, a debate developed in the clinical literature over the safety of VBACs,5–8 and in the late 1990s rates began a rapid decline, with the most recent figures documenting the lowest rate (10.6%) since cesarean deliveries began to be reported on birth certificates in 1989. By 2004, the overall cesarean rate had risen to 29.1% and the primary cesarean rate to 20.6%, both representing the highest national rates ever reported.9 This latest trend in the overall rate has been noted in government reports,3 provider group studies,10 and the popular press,11 and the majority of attention has been focused on shifting VBAC rates12 and “patient-choice cesareans”13,14 rather than on changes in primary cesarean rates.
We used national birth certificate data to examine changes in primary cesarean rates in the United States between 1991 and 2002. In particular, we assessed demographic and medical risk factors associated with cesarean deliveries in an attempt to determine the degree to which variations in cesarean rates corresponded to changes in the risk profiles of mothers or appeared to be a function of changes in clinical practice.
METHODS
We based our analysis on data drawn from 1991 through 2002 US birth certificate files.15 As mentioned, such data have been available since 1989, and all of the states and the District of Columbia have been reporting information on cesarean deliveries since 1991. We computed cesarean rates for birth records on which information was available for the “method of delivery” item; these data were available for more than 96% of all US births during 1991 through 1993 and more than 99% between 1994 and 2002.
We focused on the rate of primary cesarean deliveries, defined here as the number of primary cesareans per 100 live births among mothers who had not had a previous cesarean. We examined changes in rates among all women as well as among a lower risk group composed of mothers with singleton, full-term (≥ 37 weeks) births involving a vertex presentation. This lower risk subgroup was recommended by ACOG for use in risk adjustment analyses10 and was used as the basis for Healthy People 2010 goals.16 In addition, we stratified outcomes according to age, parity, race, and Hispanic ethnicity. The major outcomes assessed were changes in overall and subgroup primary cesarean rates between 1991 and 2002, with a particular focus on the change in rates between 1996 and 2002.
We also examined changes in the distributions of medical indications that might influence cesarean rates and the shifting rates associated with these indications. In our analysis, we selected from the 31 medical risk factors and labor or delivery complications listed on birth certificates those for which the associated 2002 primary cesarean rate was at least 50% above the national rate, with three exceptions. Too few cases of “seizures during labor” and “anesthetic complications” in the birth certificate data and difficulty in interpreting the meaning of “other excessive bleeding” led to inclusion of all 3 of these indications in the “other complications” category. For comparison, we include rates for those mothers among whom there was no risk factor or complication noted on the birth certificate (this measure has been the subject of a more extensive study elsewhere17).
RESULTS
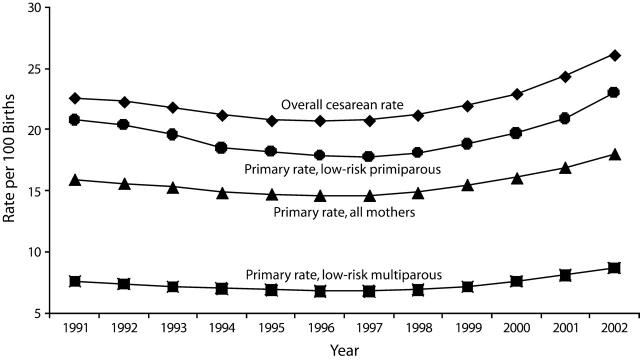
In 2002, there were 634 426 primary cesarean and 1 043 846 overall cesarean births in the United States, the latter representing an increase of 246 727 over the number of such births in 1996. More than half (53.0%) of that growth was a result of the increase of 130 702 primary cesareans between 1996 and 2002. Figure 1 ▶ illustrates trends over time for the following categories of cesarean births: all cesareans, primary cesareans among all mothers, and primary cesareans among nulliparous and multiparous women in the lower risk subgroup described earlier (full-term singleton, vertex presentation). Trends in overall cesareans, which have also been reported elsewhere,3 indicate a slow but steady decline from 1991 to 1996 followed by a rapid increase, reaching a point in 2002 at which rates were higher than a decade earlier.
FIGURE 1—
Overall and primary cesarean rates and primary cesarean rates among low-risk primiparous and multiparous women: United States, 1991–2002.
Note. Rates are per 100 births. Low-risk mothers were defined as those with singleton, full-term (≥ 37 weeks) births involving vertex presentations.
The trends over time for all primary cesareans and lower risk primary cesareans were comparable. Likewise, although the rate of primary cesareans among nulliparous women was consistently about 2.5 times higher than that among multiparous women, these women exhibited the same pattern over time. The substantial rise followed by a decline in the national VBAC rate (data not shown) has been described as reflecting clinical practice changes in response to concerns about uterine rupture,18 but the primary cesarean rate, far less remarked on, had an almost perfect negative correlation with the annual VBAC rate between 1991 and 2002 (Pearson r= −0.99).
Primiparous Mothers
Despite the decline in the early 1990s, the primary cesarean rate in 2002 in the United States (18.0%) was higher than the 1991 rate (15.9%), and there were substantial variations in subgroup-specific patterns of change. Given that past research3,19 had indicated that mother’s age, parity, and race/ethnicity are related to the likelihood of a cesarean delivery, we assessed primary cesarean rates after taking these factors into account (Table 1 ▶). Among primiparous mothers of all races, the primary cesarean rate generally decreased markedly (11%) from 1991 to 1996; however, it rose even more substantially, to 25.8%, from 1996 to 2002 (21%). In other words, more than one fourth of first-time mothers delivered their infants via cesarean in 2002.
TABLE 1—
Trends in Primary Cesarean Deliveries, by Various Characteristics of Mothers: United States, 1991, 1996, and 2002
| First Child | Second Child or After | |||||||||||
| Primary Cesareans, % | Primary Cesareans, % | |||||||||||
| Race/Ethnicity and Age Group | 1991 | 1996 | 2002 | No. of Primary Cesareans, 2002 | Change Between 1991 and 1996, % | Change Between 1996 and 2002, % | 1991 | 1996 | 2002 | No. of Primary Cesareans, 2002 | Change Between 1991 and 1996, % | Change Between 1996 and 2002, % |
| All racial/ethnic groupsa | ||||||||||||
| Overall | 23.8 | 21.3 | 25.8 | 338 324 | −11 | 21 | 11.3 | 10.7 | 13.3 | 294 097 | −5 | 24 |
| < 20 | 16.8 | 14.7 | 17.8 | 55 302 | −13 | 21 | 9.6 | 9.4 | 11.3 | 12 271 | −2 | 20 |
| 20–24 | 22.0 | 19.2 | 22.5 | 88 277 | −13 | 17 | 9.6 | 8.7 | 10.4 | 56 236 | −9 | 20 |
| 25–29 | 26.9 | 23.3 | 27.6 | 84 980 | −13 | 18 | 10.8 | 10.0 | 12.0 | 74 412 | −7 | 20 |
| 30–34 | 31.6 | 28.4 | 33.7 | 71 647 | −10 | 19 | 12.1 | 11.3 | 14.3 | 84 004 | −7 | 27 |
| 35–39 | 38.6 | 35.0 | 42.4 | 30 786 | −9 | 21 | 14.8 | 13.8 | 17.6 | 51 409 | −7 | 28 |
| 40–49b | 46.4 | 42.6 | 52.4 | 7 332 | −8 | 23 | 19.0 | 18.3 | 23.8 | 15 765 | −4 | 30 |
| White, non-Hispanicc | ||||||||||||
| Overall | 24.4 | 21.5 | 26.4 | 200 132 | −12 | 23 | 11.5 | 10.7 | 13.4 | 169 222 | −7 | 25 |
| <20 | 17.1 | 14.4 | 17.8 | 24 058 | −16 | 24 | 10.9 | 10.1 | 12.3 | 5 049 | −7 | 22 |
| 20–24 | 22.2 | 19.0 | 22.0 | 47 080 | −14 | 16 | 10.3 | 9.0 | 10.7 | 28 148 | −13 | 19 |
| 25–29 | 26.4 | 22.7 | 26.8 | 53 620 | −14 | 18 | 10.9 | 10.0 | 12.0 | 41 687 | −8 | 20 |
| 30–34 | 30.9 | 27.4 | 32.9 | 49 236 | −11 | 20 | 11.6 | 10.9 | 14.0 | 52 692 | −6 | 28 |
| 35–39 | 37.7 | 33.5 | 41.3 | 21 125 | −11 | 23 | 14.2 | 13.0 | 16.8 | 31 905 | −8 | 29 |
| 40–49b | 45.2 | 40.6 | 51.1 | 5 013 | −10 | 26 | 18.3 | 17.6 | 22.9 | 9 741 | −4 | 30 |
| Black, non-Hispanicc | ||||||||||||
| Overall | 23.2 | 22.4 | 27.2 | 46 363 | −3 | 21 | 11.8 | 12.2 | 15.5 | 51 494 | 3 | 27 |
| < 20 | 17.1 | 16.6 | 20.0 | 14 134 | −3 | 20 | 8.9 | 9.7 | 12.7 | 3 783 | 9 | 31 |
| 20–24 | 23.7 | 22.3 | 26.8 | 15 091 | −6 | 20 | 9.6 | 9.7 | 12.3 | 13 939 | 1 | 27 |
| 25–29 | 31.9 | 30.0 | 34.8 | 7 964 | −6 | 16 | 12.0 | 12.0 | 14.6 | 13 051 | 0 | 22 |
| 30–34 | 37.9 | 36.3 | 41.1 | 5 642 | −4 | 13 | 15.0 | 14.7 | 18.7 | 11 431 | −2 | 27 |
| 35–39 | 42.4 | 44.0 | 49.7 | 2 812 | 4 | 13 | 18.4 | 18.1 | 23.0 | 7 087 | −2 | 27 |
| 40–49b | 51.1 | 52.8 | 58.0 | 720 | 3 | 10 | 22.9 | 22.6 | 28.0 | 2 203 | −1 | 24 |
| Hispanicc,d | ||||||||||||
| Overall | 22.5 | 19.8 | 23.8 | 66 432 | −12 | 20 | 10.3 | 9.5 | 11.6 | 55 870 | −8 | 22 |
| < 20 | 16.2 | 14.0 | 16.6 | 15 425 | −14 | 19 | 8.2 | 8.1 | 9.3 | 3 039 | −1 | 15 |
| 20–24 | 21.5 | 19.0 | 22.0 | 21 977 | −12 | 16 | 8.0 | 7.4 | 8.6 | 12 095 | −8 | 16 |
| 25–29 | 29.4 | 25.4 | 29.4 | 15 393 | −14 | 16 | 9.8 | 8.7 | 10.6 | 15 679 | −11 | 22 |
| 30–34 | 35.2 | 31.8 | 37.3 | 9 178 | −10 | 17 | 12.3 | 11.2 | 13.7 | 14 082 | −9 | 22 |
| 35–39 | 43.5 | 38.8 | 45.2 | 3 647 | −11 | 16 | 15.6 | 14.7 | 17.9 | 8 473 | −6 | 22 |
| 40–49b | 47.6 | 46.2 | 54.9 | 812 | −3 | 19 | 20.1 | 19.2 | 23.9 | 2 502 | −4 | 24 |
Note. The primary cesarean rate was defined as the number of primary cesareans per 100 live births among women who had not had a previous cesarean.
a Includes races other than White and Black as well as Hispanic origin not stated.
b Beginning in 1997, data were for women aged 40 to 54 years.
c In 1991, New Hampshire did not report data on Hispanic origin. Thus, for 1991, all infants in this state were assumed to be delivered by non-Hispanic women (in 1993, the first year that data were available, 99% of births in New Hampshire were to non-Hispanic women).
d Includes all women of Hispanic origin of any race.
Patterns among White, non-Hispanic and Hispanic women were similar. However, among Black, non-Hispanic primiparous mothers, the decrease from 1991 to 1996 was minimal (3%), whereas the increase from 1996 to 2002 (21%) was similar to that seen among the other groups. Thus, whereas the primary cesarean rate among Black, non-Hispanic primiparous mothers was more than a full percentage point lower than that among primiparous White, non-Hispanic mothers in the early 1990s, the rate was almost a full percentage point higher in 2002.
In all cases, primary cesarean rates increased with advancing maternal age, with more than half (52.4%) of primiparous mothers older than 40 years delivering via cesarean in 2002. Notably, the overall primary cesarean rate among primiparous White, non-Hispanic mothers in 2002 was more than 2.6 percentage points higher than the rate among primiparous Hispanic mothers. However, in every age group with the exception of teenagers, the primary cesarean rate among Hispanic mothers was equal to or higher than that among White non-Hispanic mothers (Table 1 ▶). The lower overall rate among primiparous Hispanic mothers in 2002 was the result of the much larger concentration of births among mothers younger than 25 years (45% of births among Hispanic women compared with 30% among White, non-Hispanic women).
Likewise, the largest concentration of births among mothers younger than 25 years (51%) was in the Black, non-Hispanic group. Thus, despite their much higher age-specific primary cesarean delivery rates in every age group in 2002, the overall primary cesarean rate among Black, non-Hispanic primiparous mothers was less than 1 percentage point higher (27.2%) than that among White, non-Hispanic mothers (26.4%).
Multiparous Mothers
Despite the fact that this group was composed of mothers who had given birth to their previous children vaginally, more than 1 in 8 (13.3%) had a primary cesarean in 2002. The pattern of change in cesarean delivery rates among these mothers was different from that among primiparous women (Table 1 ▶). In terms of trends, the overall 1991 to 1996 decrease was half that observed among primiparous mothers, whereas the 1996 to 2002 increase was slightly greater. This pattern was generally consistent across all of the groups we examined; Black, non-Hispanic multiparous mothers once again exhibited the largest overall increase (11.8% to 15.5%) between 1991 and 2002, with the result that the rate among these women was one third higher than that among Hispanic multiparous mothers (11.6%).
Rates also increased with advancing maternal age among multiparous women, with older Black, non-Hispanic women exhibiting the highest rates. Almost one fourth (24%) of Black, non-Hispanic mothers older than 35 years who had delivered their children vaginally in the past had a primary cesarean in 2002.
Risk Profile: Cesarean Births
There are 3 potential explanations for the changes observed in rates of primary cesarean births during the study period. First, the demographic and medical risk profiles of US mothers may have changed. It can be seen from Table 1 ▶ that, in terms of demographic characteristics, changes in primary cesarean rates have occurred among women of all ages, parity groups, and racial/ethnic groups. We conducted a direct standardization analysis20 assessing the effects of differences in mothers’ age distributions between 1996 and 2002 on primary cesarean rates. This analysis revealed virtually no such effects (data not shown), suggesting that the increase in primary cesarean rates between 1996 and 2002 cannot be attributed to changes in the age composition of women having primary cesareans. An example of a change in mothers’ medical risk profiles would be an increase in the number of macrosomic (birthweight above 4000 g) babies, which in turn would lead to an increase in the overall number of cesareans even if the rate of cesareans performed as a result of macrosomia remained unchanged (Table 2 ▶).
TABLE 2—
Rates of Selected Birth Events, by Parity: United States, 1991–1996 and 1996–2002
| Year | |||||
| Parity Status, Presentation, and Outcome | 1991 | 1996 | 2002 | Change Between 1991 and 1996, % | Change Between 1996 and 2002, % |
| Primiparous women | |||||
| Breech/malpresentation: singleton | 39.7 | 38.1 | 37.5 | −4 | −2 |
| Premature (< 37 wk gestation): singleton | 97.6 | 98.3 | 102.9 | 1 | 5 |
| Birthweight > 4000 g: singleton | 87.6 | 81.8 | 75.8 | −7 | −7 |
| Multiple births | 11.4 | 13.6 | 17.2 | 19 | 26 |
| Multiparous women | |||||
| Breech/malpresentation: singleton | 29.6 | 29.3 | 28.4 | −1 | −3 |
| Premature (< 37 wk gestation): singleton | 98.6 | 96.6 | 105.1 | −2 | 9 |
| Birthweight > 4000 g: singleton | 119.4 | 117.5 | 104.1 | −2 | −11 |
| Multiple births | 30.0 | 34.3 | 40.6 | 14 | 18 |
Note. Rates are per 1000 live births.
Second, medical risk profiles may not have changed but, regardless, the behavior of clinicians changed21 (e.g., the number of macrosomia cases was the same, but there was a greater frequency of cesareans associated with that diagnosis) (Table 3 ▶). The third possibility is that both demographic characteristics and risk factor profiles could have played a role.
TABLE 3—
Percentages of Live Births Delivered via Cesarean to Low-Risk Primiparous Mothers, by Selected Medical Risk Factors and Complications of Labor or Delivery: United States, 1991, 1996, and 2002
| Cesarean Rate | ||||||
| 1991 | 1996 | 2002 | Change Between 1991 and 1996, % | Change Between 1996 and 2002, % | Change Between 1991 and 2002, % | |
| Medical risk factor | ||||||
| Diabetes | 36.9 | 33.1 | 39.3 | −10 | 19 | 7 |
| Eclampsia | 45.4 | 37.3 | 42.5 | −18 | 14 | −6 |
| Genital herpesa | 45.3 | 35.3 | 34.7 | −22 | −2 | −23 |
| Hydramnios/oligohydramnios | 41.2 | 31.4 | 34.1 | −24 | 9 | −17 |
| Pregnancy-associated hypertension | 36.9 | 30.6 | 34.8 | −17 | 14 | −6 |
| Chronic hypertension | 39.0 | 34.8 | 41.6 | −11 | 20 | 7 |
| Incompetent cervix | 30.8 | 31.0 | 35.9 | 1 | 16 | 17 |
| Uterine bleeding a | 24.8 | 21.5 | 24.6 | −13 | 14 | −1 |
| Other b | 35.5 | 31.9 | 34.9 | −10 | 9 | −2 |
| Complication of labor or delivery | ||||||
| Placenta abruptio | 60.3 | 57.9 | 63.5 | −4 | 10 | 5 |
| Cephalopelvic disproportion | 98.1 | 97.0 | 97.3 | −1 | 0 | −1 |
| Cord prolapse | 59.7 | 59.9 | 62.4 | 0 | 4 | 5 |
| Dysfunctional labor | 72.1 | 68.2 | 76.6 | −5 | 12 | 6 |
| Febrile | 36.3 | 30.5 | 32.5 | −16 | 7 | −10 |
| Fetal distressa | 64.3 | 56.4 | 64.8 | −12 | 15 | 1 |
| Placenta previa | 72.8 | 70.2 | 70.5 | −4 | 0 | −3 |
| Premature rupture of membranes | 29.7 | 23.6 | 26.1 | −21 | 11 | −12 |
| Prolonged labor | 41.8 | 37.6 | 40.3 | −10 | 7 | −4 |
| Birthweight > 4000 g | 38.9 | 34.6 | 40.9 | −11 | 18 | 5 |
| Other c | 37.6 | 33.8 | 38.0 | −10 | 12 | 1 |
| No risk factor noted | 5.6 | 6.1 | 10.0 | 9 | 64 | 79 |
Note. Low-risk mothers were defined as those with singleton, full-term (≥ 37 weeks) births involving vertex presentations. Between 1991 and 2001, some of the reporting areas did not include all of the risk factors and complications listed here on birth certificates.
a Texas does not report this item.
b Includes anemia, acute or chronic lung disease, cardiac disease, hemoglobinopathy, previous preterm or small-for-gestational-age infant, previous infant with a birthweight of 4000 g or above, renal disease, and Rh sensitization.
c Includes other excessive bleeding, moderate/heavy meconium, seizures during labor, precipitous labor, and anesthetic complications.
Initially we assessed, after control for parity, patterns of change in the 3 factors—gestation, presentation, and plurality—recommended by ACOG10 and Healthy People 201016 for use in cesarean rate risk adjustments; in addition, we analyzed an indicator that has been widely examined as a possible influence on cesarean rates, macrosomia.19,22 The data presented in Table 2 ▶ offer little support for a “change in risk profile” hypothesis. It can be seen that there was only one category—singleton premature births among multiparous women—in which the pattern corresponded to the early 1990s decrease and the late 1990s increase in primary cesarean rates (and the magnitude of change was much lower than the overall average). Regardless of parity group, proportions of breech and macrosomic births actually decreased from 1991 to 2002, whereas proportions of multiple births rose rapidly.
An additional analysis of the prevalence of all medical risk factors and complications of labor and delivery listed on birth certificates (data not shown) revealed that the general pattern of change (a decrease between 1991 and 1996 and an increase from 1996 to 2002) applied to only one of the 31 risk factors or complications examined (dysfunctional labor). Reported rates of the medical risk factors assessed generally rose during both time periods studied, and, with the minor exception of dysfunctional labor, reported rates of labor and delivery complications dropped during both periods. Overall, for all women, there was no clear correspondence between the pattern of recorded risks and changes in primary cesarean rates.
Risk Factors for Primary Cesareans
Table 3 ▶ presents primary cesarean rates for lower risk (full-term, vertex, singleton births) primiparous mothers associated with 18 of the medical risk factors and complications recorded on birth certificates as well as 2 summary measures comprising the remaining indications. Because of its importance in past research, we also included a variable reflecting birthweights above 4000 g. In virtually every instance, regardless of indication, primary cesarean rates decreased between 1991 and 1996 and increased from 1996 to 2002. Rates for those mothers with no reported risk factors17 are shown in the bottom row of Table 3 ▶, and here the pattern was one of a small increase between 1991 and 1996 followed by a rapid increase between 1996 and 2002, resulting in a 79% overall increase.
DISCUSSION
It appears from our results that, in concert with population changes (e.g., more older women delivering a first infant and increased rates of multiple births),15 changes in obstetrical practices were the major influence on the shifting pattern of primary cesarean rates in the 1990s and the early 2000s. Although age, race/ethnicity, and parity distributions of mothers changed in the 1990s, an examination of cesarean births among lower risk mothers showed that rates of primary cesareans in virtually all of the subgroups analyzed shifted in the same pattern: a decrease between 1991 and 1996 followed by a larger increase between 1996 and 2002. Rates increased over time among older mothers, a significant consideration given the growing number of births in this group.
Likewise, although an examination of the prevalence of medical risk factors and labor or delivery complications revealed changes in the occurrence of such conditions, these alterations did not correspond to the pattern of shifts observed in primary cesarean rates. However, primary cesarean rates associated with virtually every possible medical risk factor and complication did correspond closely to the pattern of a 1991 to 1996 decrease and a 1996 to 2002 increase.
Examination of the lower risk group of mothers with singleton, full-term births involving a vertex presentation showed that the cesarean rate in 2002 for primiparous mothers was 22.4%, far higher than the recommended Healthy People 2010 guideline of 15% for first-time mothers in this risk profile subgroup.16 Among those cases in which there was no reported medical indication whatsoever,17 there was a sharp rise in rates of primary cesareans, with an increase of 79% between 1991 and 2002.
Despite the great deal of attention focused on increasing VBACs—and then questioning of this practice—changes in primary cesarean rates had the greater impact on overall cesarean rates in the United States in the 1990s and early 2000s. In the case of individual mothers, primary and repeat cesareans are now powerfully linked because the growing restrictions on VBACs23 mean that mothers having primary cesareans will typically deliver subsequent infants via cesarean. Increasing rates of primary cesareans, particularly among younger, primiparous mothers, will therefore profoundly influence overall cesarean rates in the future by creating a large cohort of women for whom repeat cesareans will be the norm. For example, in 2002 alone, 228559 women younger than 30 years who were delivering their first infant had a primary cesarean, and, given current practice, they are highly likely to have a repeat cesarean in any future birth.
Notwithstanding the recent focus on VBACs, several studies have explored potential influences on primary cesarean rates. Gregory et al., using national hospital discharge data, compared information from 1985 and 1994 and found that, in the latter year, a small but increased proportion of primary cesareans were associated with breech presentations.24 However, as a percentage of overall births, breech presentations remain relatively rare. Parrish and colleagues, analyzing data from Washington State, found that primary cesarean rates were affected by maternal age, parity, and birthweight,19 although Taffel et al.,25 using a similar model and national data, reanalyzed these results and suggested that age and parity accounted for most of the variation. Gregory et al.,26,27 in 2 analyses of California hospital discharge data, found that maternal age was a major factor, as was hospital type (data on this latter variable are not available on birth certificates).
Recent studies have also suggested that prepregnancy obesity (a measure not available in the present data) is related to higher primary cesarean rates.28,29 However, rates of obesity among US women in all age groups continued to increase during the entire period of our study,30 and these trends did not coincide with the trends in cesareans observed. Overall comparisons between the studies just described and the present research are limited as a result of the reliance on different data sets, time periods, and questions asked; however, we examined the variables identified as important in these studies whenever possible.
There are legitimate concerns associated with reliance on certain birth certificate items,31 but, for several reasons, this was probably not as significant a problem in the present study as in others. First, the key variables assessed in our analysis—primary cesarean rate, age, and parity—are among the more reliably measured items on birth certificates.32 Second, although the completeness and quality of the medical risk factor and complication data included on birth certificates are of concern (issues related to under-reporting of individual items have been summarized elsewhere31), our findings are consistent across all categories of risk factors and complications. Finally, and most important, because we examined changes over time, there is no inherent reason to expect bias that would have led to shifts in the measurement of these variables at different time points.
The recent change in the primary cesarean rate in the United States has involved a notable decrease followed by a substantial increase in just over a decade. The present results suggest the need for further studies focusing on nonclinical reasons for shifts in cesarean delivery rates. It has been suggested that some of the growth in primary cesareans has resulted from “patient choice” cesareans,13 although evidence of such a trend is not based on systematic surveys of mothers. A current debate in the obstetrical literature, with more published editorials calling for elective cesareans,33 indicates that there may be a shift in obstetricians’ attitudes,34 but again the data are anecdotal.
In addition, there have been suggestions that “defensive” medicine associated with fear of malpractice awards might cause shifts in clinicians’ behavior.35 More research is needed on the causes of such trends, given that the increase in primary cesareans combined with growing restrictions on VBACs will lead to a continuation—and, in all likelihood, acceleration—of the current growth in overall cesarean rates in the United States.
Peer Reviewed
Contributors E. Declercq originated the project, planned the study, and wrote the first draft of the article. All of the authors analyzed the data and contributed to subsequent drafts.
Human Participant Protection No protocol approval was needed for this study.
References
- 1.National Institutes of Health. Cesarean Childbirth. Washington, DC: US Dept of Health and Human Services; 1981. NIH publication 82–2067.
- 2.Guidelines for Vaginal Delivery After Previous Cesarean Birth. Washington, DC: American College of Obstetricians and Gynecologists; 1988.
- 3.Hamilton BE, Martin JA, Ventura SJ, Sutton PD, Menacker F. Births: preliminary data for 2004. Nat Vital Stat Rep. 2005;54(8):1–17. [PubMed] [Google Scholar]
- 4.The National Sentinel Caesarean Section Audit Report. London, England: Royal College of Obstetricians and Gynaecologists, Clinical Effectiveness Support Unit; 2001.
- 5.Sachs BP, Kobelin C, Castro MA, Frigoletto F. The risks of lowering the cesarean-delivery rate. N Engl J Med. 1999;340:54–57. [DOI] [PubMed] [Google Scholar]
- 6.Greene M. Vaginal delivery after cesarean section—is the risk acceptable? N Engl J Med. 2001;345:55–56. [DOI] [PubMed] [Google Scholar]
- 7.Lydon-Rochelle M, Holt V, Easterling T, Martin D. Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med. 2001; 345:3–8. [DOI] [PubMed] [Google Scholar]
- 8.Smith GC, Pell JP, Cameron AD, Dobbie R. Risk of perinatal death associated with labor after previous cesarean delivery in uncomplicated term pregnancies. JAMA. 2002;287:2684–2690. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton BE, Martin JA, Sutton PD. Births: preliminary data for 2003. Natl Vital Stat Rep. November 23, 2004;53(9). [PubMed]
- 10.Evaluation of Cesarean Delivery. Washington, DC: American College of Obstetricians and Gynecologists Task Force on Cesarean Delivery; 2000.
- 11.Springen K. The right to choose. Newsweek. December 4, 2000:73–74. [PubMed]
- 12.Zinberg S. Vaginal delivery after previous cesarean delivery: a continuing controversy. Clin Obstet Gynecol. 2001;44:561–570. [DOI] [PubMed] [Google Scholar]
- 13.Harer WB. Patient choice cesarean. ACOG Clin Rev. 2000;5:13–16. [Google Scholar]
- 14.Minkoff H, Chernevak FA. Elective primary cesarean delivery. N Engl J Med. 2003;348:946–950. [DOI] [PubMed] [Google Scholar]
- 15.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2002. Natl Vital Stat Rep. December 17, 2003;52(10). [PubMed]
- 16.Healthy People 2010. 2nd ed. Washington, DC: US Dept of Health and Human Services; 2000.
- 17.Declercq E, Menacker F, MacDorman M. Rise in “no indicated risk” primary caesareans in the United States, 1991–2001. BMJ. 2005;330:71–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Landon MB, Hauth JC, Leveno KJ, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;351:2581–2589. [DOI] [PubMed] [Google Scholar]
- 19.Parrish KM, Holt VL, Easterling TR, Connell FA, LoGerfo JP. Effect of changes in maternal age, parity, and birth weight distribution on primary cesarean delivery rates. JAMA. 1994;271:443–447. [PubMed] [Google Scholar]
- 20.Shryock HS, Siegel JS, Stockwell EG, et al. The Methods and Materials of Demography. New York, NY: Academic Press Inc; 1976.
- 21.Leitch CR, Walker JJ. The rise in caesarean section rate: the same indications but a lower threshold. Br J Obstet Gynaecol. 1998;105:621–626. [DOI] [PubMed] [Google Scholar]
- 22.Rhodes JC, Schoendorf KC, Parker JD. Contribution of excess weight gain during pregnancy and macrosomia to the cesarean delivery rate. Pediatrics. 2003;111:1181–1185. [PubMed] [Google Scholar]
- 23.Vaginal Delivery After Previous Cesarean Birth. Washington, DC: American College of Obstetricians and Gynecologists; 2004.
- 24.Gregory KD, Curtin SC, Taffel SM, Notzon FC. Changes in indications for cesarean delivery: United States, 1985 and 1994. Am J Public Health. 1998;88:1384–1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taffel SM, Clarke SC, Placek PJ. Factors influencing primary cesarean rates. JAMA. 1994;271:1829–1830. [PubMed] [Google Scholar]
- 26.Gregory KD, Korst LM, Gornbein JA, Platt LD. Using administrative data to identify indications for elective primary cesarean delivery. Health Serv Res. 2002;37:1387–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gregory KD, Korst LM, Platt LD. Variation in elective primary cesarean delivery by patient and hospital factors. Am J Obstet Gynecol. 2001;184:1521–1534. [DOI] [PubMed] [Google Scholar]
- 28.Guilhrad P, Blondel B. Trends in risk factors for caesarean sections in France between 1981 and 1995: lessons for reducing the rates in the future. Br J Obstet Gynaecol. 2001;108:48–55. [DOI] [PubMed] [Google Scholar]
- 29.Kaiser PS, Kirby RS. Obesity as a risk factor for cesarean in a low risk population. Obstet Gynecol. 2001; 97:39–43. [DOI] [PubMed] [Google Scholar]
- 30.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. [DOI] [PubMed] [Google Scholar]
- 31.Parrish KM, Holt VL, Connell FA, Williams B, LoGerfo JP. Variations in the accuracy of obstetric procedures and diagnoses on birth records in Washington State, 1989. Am J Epidemiol. 1993;138:119–127. [DOI] [PubMed] [Google Scholar]
- 32.Green DC, Moore JM, Adams MM, Berg CJ, Wilcox LS, McCarthy BJ. Are we underestimating rates of vaginal birth after previous cesarean birth? The validity of delivery methods from birth certificates. Am J Epidemiol. 1998;147:581–586. [DOI] [PubMed] [Google Scholar]
- 33.O’Boyle AL, Davis GD, Calhoun BC. Informed consent and birth: protecting the pelvic floor and ourselves. Am J Obstet Gynecol. 2002;187:981–983. [DOI] [PubMed] [Google Scholar]
- 34.Scott JR. Putting elective cesareans into perspective. Obstet Gynecol. 2002;99:967–968. [DOI] [PubMed] [Google Scholar]
- 35.Dubay L, Kaestner R, Waidmann T. The impact of malpractice fears on cesarean section rates. J Health Economics. 1999;18:491–522. [DOI] [PubMed] [Google Scholar]