Abstract
We examined prevalence and predictors of trauma among HIV-infected persons in the Deep South using data from the Coping with HIV/AIDS in the Southeast (CHASE) study. Over 50% of CHASE participants were abused during their lives, with approximately 30% experiencing abuse before age 13, regardless of gender. Caregiver characteristics were associated with childhood abuse. Abuse is related to increases in high–HIV-risk activities. The findings help explain why people engage in such high-risk activities and can provide guidance in designing improved care and prevention messages.
Childhood sexual and severe physical abuse is associated with the following as adults: posttraumatic stress disorder,1–6 anxiety,1–3 depression,7–11 dissociation,4,7 substance abuse,5,7,12–14 revictimization,6,12–16 high-risk sexual behaviors,7,17–20 and engaging in abuse of others.8 Substance abuse and symptoms of mental illness are associated with reduced medication adherence, lower likelihood of being prescribed therapy, increased morbidity, and poorer quality of life among HIV-infected individuals.21–30 Thus, childhood victimization can be directly linked to behaviors that put a person at risk for infectious diseases and reduced treatment adherence.
Incident AIDS cases increased 29% from 2000 to 2002 in the states of Alabama, Georgia, Louisiana, North Carolina, and South Carolina, and only increased 9% across the other Southern states and less than 0.5% in the rest of the country.31–32 Increases occurred most rapidly outside major metropolitan areas of these 5 states.33–37 This study examines abuse rates and their associations with childhood home environments in a sample of individuals being treated for HIV in the Deep South. We believe that increased knowledge of factors leading to high-risk activities can result in effective prevention and care techniques.
METHODS
Researchers conducting the Coping with HIV/AIDS in the Southeast (CHASE) study interviewed 611 consecutively sampled HIV-infected individuals from 8 infectious diseases clinics outside 3 major metropolitan areas in 5 states in the Deep South.38 The clinics chosen treated 12% of the states’ HIV/AIDS caseload, and 10% of the clinics’ patients participated in the interview. The response rate was 79%.38 Interviewers were trained, certified, and consistently monitored by Battelle Centers for Public Health Research and Evaluation to avoid interviewer bias.
Measures
Sexual abuse included clear force, threat, or harm when (1) touching the victim’s breasts, pubic area, vagina, or anus with hands, mouth, or objects; (2) making the victim touch the perpetrator’s pubic area or anus with hands, mouth, or objects; or (3) making the victim have vaginal or anal intercourse. Even when not stated, the threat of force or harm was implied in children aged younger than 13 when the perpetrator was aged at least 5 years older. Physical abuse was defined as incidents separate from sexual abuse that included threats on one’s life.
Respondents were asked if their primary caretakers were too drunk or high to care for the family; were depressed or mentally ill; went to prison; or were divorced/separated. Respondents stated whether their father, stepfather, or mother’s boyfriend beat, hit, kicked, bit, burned, threatened with, or used, a weapon against their female caretaker. Respondents were asked if, when they were growing up, they had enough to eat and if they were ever placed in foster care, an orphanage, or a reformatory. This list of traumas was adapted from past research.39–40
Statistical Analysis
Logistic regression was used to examine associations with childhood sexual abuse (at age < 13 years); lifetime sexual abuse; childhood sexual and/or physical abuse; and lifetime sexual and/or physical abuse (at age < 13 years). We used a control variable to account for differences in average county income, religiosity, occupation, and education by site.
RESULTS
Approximately 1 in 4 respondents, regardless of gender, were sexually abused before the age of 13 (Figure 1 ▶). Approximately one third of respondents experienced lifetime sexual abuse (30% men and 38% women). More than 50% of respondents experienced sexual or severe physical abuse by the time of the interview.
FIGURE 1—
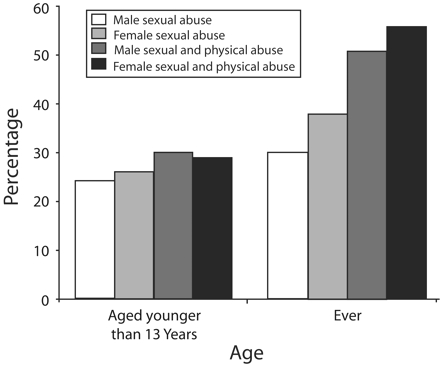
Prevalence of abuse before and after the age of 13, by gender.
Having parents too high or drunk to care for the family was associated with more than twice the risk of childhood sexual and/or physical abuse, as was being removed from the family (Table 1 ▶). A male guardian physically harming or threatening the respondent’s mother or stepmother was associated with childhood sexual abuse, and having a reportedly depressed parent was associated with both forms of abuse.
TABLE 1—
Odds Ratios and 95% Confidence Intervals for Sexual and Physical Abuse, by Childhood Environment Variables and Demographic: CHASE Study, 2001–2003
| Childhood Sexual Abusea | Lifetime Sexual Abuse | Childhood Sexual and/or Physical Abusea | Lifetime Sexual and/or Physical Abuse | |
| Childhood | ||||
| Depressed parent (20.9%) | 1.51 (0.91, 2.53) | 1.57 (0.97, 2.54) | 2.00 (1.23, 3.24)** | 1.78 (1.08, 2.91)** |
| Impaired parent (11.4%) | 2.24 (1.18, 4.29)** | 1.73 (0.90, 3.33) | 2.46 (1.28, 4.73)** | 1.64 (0.80, 3.36)** |
| Spousal abuse (22.4%) | 1.70 (1.03, 2.78)** | 1.49 (0.92, 2.42) | 1.60 (1.00, 2.60) | 1.94 (1.19, 3.16) |
| Hungry (19.8%) | 0.96 (0.54, 1.69) | 1.26 (0.75, 2.16) | 1.06 (0.62, 1.82) | 0.74 (0.45, 1.21) |
| Parent died (11.5%) | 0.76 (0.38, 1.53) | 0.86 (0.45, 1.62) | 0.85 (0.44, 1.65) | 1.04 (0.57, 1.91) |
| Parent in prison (7.5%) | 1.42 (0.70, 3.00) | 1.16 (0.55, 2.46) | 1.62 (0.77, 3.41) | 0.88 (0.41, 1.88) |
| Foster care (8.6%) | 2.14 (1.02, 4.52)** | 1.70 (0.82, 3.53) | 2.50 (1.21, 5.19)** | 2.07 (0.95, 4.48) |
| Parents divorced (39.4%) | 1.83 (1.18, 2.83)** | 1.66 (1.10, 2.50)** | 2.10 (1.39, 3.18)** | 2.10 (1.42, 3.10)** |
| Demographics | ||||
| Male (69%) | 0.38 (0.20, 0.70)** | 0.17 (0.09, 0.34)*** | 0.56 (0.32, 0.99)*** | 0.44 (0.27, 0.73)** |
| Not heterosexual (44.5%) | 3.99 (2.18, 7.31)*** | 6.88 (3.51, 13.48)*** | 3.21 (1.86, 5.55)*** | 2.35 (1.44, 3.85)** |
| Minority (69%) | 1.33 (0.81, 2.18) | 1.14 (0.72, 1.79) | 1.12 (0.70, 1.78) | 0.85 (0.55, 1.31) |
| Study site (50%) | 0.82 (0.53, 1.26) | 0.74 (0.49, 1.10) | 0.97 (0.65, 1.47) | 0.86 (0.59, 1.26) |
| Self in jail (2.5%) | 5.17 (2.26, 11.81)*** | 3.66 (0.65, 1.47)** | ||
aOccuring when respondent was aged younger than 13 years.
*P = .10; **P = .05; ***P < .0001.
Gender was significant only when controlling for sexual orientation. Women and non-heterosexual men were more than twice as likely to have experienced both forms of abuse. Alternative specifications with interaction effects yielded the same results.
DISCUSSION
The high rates of reported trauma in this sample from the Deep South may help to explain why the HIV epidemic continues unabated as a largely rural and heterosexual disease in this region. The finding that there were no differences in sexual abuse between male and female respondents is important given that studies usually report higher rates of sexual abuse among women of all ages. Even among heterosexual male respondents, the rates of sexual abuse were higher than for previously studied clinical populations. The rates of respondents that grew up under difficult living situations is higher than the general population, and may also help to explain the ineffectiveness of previous HIV prevention messages. The lack of difference by race is in line with other research in the Deep South,41 suggesting that other factors, such as childhood poverty and social structure, may be more important in identifying at-risk groups.
This study was retrospective; all accounts of parental characteristics are on the basis of study participants’ perceptions of their past, which may be biased. Additionally, this sample represents only those who seek care. We are reassured by the similarity in demographic characteristics between our sample and those in the clinical populations. This study posed sexual abuse questions that are correlated with many poor-health indicators.39,42,43 Therefore, our higher prevalence findings may be due, in part, to detailed and accurate questioning.
Sexual and physical trauma is associated with increased risk-taking behavior (such as injection drug use or high-risk sexual behavior), putting people at increased risk for contracting HIV, transmitting HIV,7,17–20 and not engaging fully in treatment protocols. Teaching persons who have been sexually abused how to use a condom and the importance of its use may be insufficient to ensure its use by persons who disengage from their bodies during sexual activities. Childhood abuse leads to higher rates of disassociation during physical contact,4,7 possibly extending to clinic visits, which could prevent full engagement and learning during the visit. As researchers continue to search for ways to stop the spread of HIV, it is important to provide health care providers and policymakers with knowledge of high rates of previous trauma to develop targeted services and policies that can address the root causes of HIV-related transmission behaviors and lack of treatment adherence.
Acknowledgments
This study was supported in part by the National Institute of Mental Health, the National Institute of Drug Abuse, and the National Institute of Nursing Research, National Institutes of Health (grant 5R01MH061687-05). Surveys were conducted by Battelle Centers for Public Health Research and Evaluation, North Carolina.
We thank Charles Knott, Dawn Dampier, all of the interviewers, principle investigators, and respondents at each of the research sites who made this work possible.
Human Participant Protection Institutional review board approval was received by each participating site, including sites at Duke University and Battelle Centers for Public Health Research and Evaluation.
Peer Reviewed
Contributors K. Whetten originated this study and lead the analyses; J. Lesserman, D. Stangl, M. Swartz, and N. Thielman were the lead investigators on the CHASE study and assisted in the interpretation of data and presentation of results. K. Lowe was a lead author on the manuscript and conducted literature reviews. L. Hanisch assisted in the data interpretation. L. Van Scoyoc acted as programmer and also assisted in data interpretation. All authors were actively involved in the editing process.
References
- 1.Epstein JN, Saunders BE, Kilpatrick DG. Predicting PTSD in women with a history of childhood rape. J Trauma Stress. 1997;10:573–587. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez NR, Ryan SW, Vande Kemp H, Foy DW. Posttraumatic stress disorder in adult female survivors of child sexual abuse: a comparison study. J Consult Clin Psychol. 1997;65:53–39. [DOI] [PubMed] [Google Scholar]
- 3.Roth S, Newman E, Pelcovitz D, van der Kolk B, Mandel FS. Complex PTSD in victims exposed to sexual and physical abuse: results from the DSM-IV Field Trial for Posttraumatic Stress Disorder. J Trauma Stress. 1997;10:539–555. [DOI] [PubMed] [Google Scholar]
- 4.Zlotnick C. Posttraumatic stress disorder (PTSD), PTSD comorbidity, and childhood abuse among incarcerated women. J Nerv Ment Dis. 1997;185:761–763. [DOI] [PubMed] [Google Scholar]
- 5.Epstein JN, Saunders BE, Kilpatrick DG, Resnick HS. PTSD as a mediator between childhood rape and alcohol use in adult women. Child Abuse Negl. 1998;22: 223–234. [DOI] [PubMed] [Google Scholar]
- 6.Widom CS. Posttraumatic stress disorder in abused and neglected children grown up. Am J Psychiatry. 1999;156:1223–1229. [DOI] [PubMed] [Google Scholar]
- 7.McCauley J, Kern DE, Kolodner K, et al. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA. 1997;277: 1362–1368. [PubMed] [Google Scholar]
- 8.DePaul J, Domenech L. Childhood history of abuse and child abuse potential in adolescent mothers: a longitudinal study. Child Abuse Negl. 2000;24: 701–713. [DOI] [PubMed] [Google Scholar]
- 9.Styron T, Janoff-Bulman R. Childhood attachment and abuse: long-term effects on adult attachment, depression, and conflict resolution. Child Abuse Negl. 1997;21:1015–1023. [DOI] [PubMed] [Google Scholar]
- 10.Allers CT, Benjack KJ. Connection between childhood abuse and HIV Infection. J Couns Dev. 1991;70: 309–313. [Google Scholar]
- 11.Wenninger K, Ehlers A. Dysfunctional cognitions and adult psychological functioning in child sexual abuse survivors. J Trauma Stress. 1998;11:281–300. [DOI] [PubMed] [Google Scholar]
- 12.Kunitz SJ, Levy JE, McCloskey J, Gabriel KR. Alcohol dependence and domestic violence as sequelae of abuse and conduct disorder in childhood. Child Abuse Negl. 1998;22:1079–1091. [DOI] [PubMed] [Google Scholar]
- 13.Fleming J, Mullen PE, Sibthorpe B, Bammer G. The long-term impact of childhood sexual abuse in Australian women. Child Abuse Negl. 1999;23: 145–159. [DOI] [PubMed] [Google Scholar]
- 14.Merrill LL, Newell CE, Thomsen CJ, et al. Childhood abuse and sexual revictimization in a female navy recruit sample. J Trauma Stress. 1999;12: 211–225. [DOI] [PubMed] [Google Scholar]
- 15.Schaaf KK, McCanne TR. Relationship of childhood sexual, physical, and combined sexual and physical abuse to adult victimization and posttraumatic stress disorder. Child Abuse Negl. 1998;22:1119–1133. [DOI] [PubMed] [Google Scholar]
- 16.Nishith P, Mechanic MB, Resnick PA. Prior interpersonal trauma: the contribution to current PTSD symptoms in female rape victims. J Abnorm Psychol. 2000;109:20–25. [PMC free article] [PubMed] [Google Scholar]
- 17.Springs FE, Friedrich WN. Health risk behaviors and medical sequelae of childhood sexual abuse. Mayo Clin Proc. 1992;67:527–532. [DOI] [PubMed] [Google Scholar]
- 18.Bensley LS, Van Eenwyk J, Simmons KW. Self-reported childhood sexual and physical abuse and adult HIV-risk behaviors and heavy drinking. Am J Prev Med. 2000;18:151–158. [DOI] [PubMed] [Google Scholar]
- 19.Parillo KM, Freeman RC, Collier K, Young P. Association between early sexual abuse and adult HIV-risky sexual behaviors among community-recruited women. Child Abuse Negl. 2001;25:335–346. [DOI] [PubMed] [Google Scholar]
- 20.Paolucci EO, Genuis ML, Violato C. A meta-analysis of the published research on the effects of child sexual abuse. J Psychol. 2001;135:17–36. [DOI] [PubMed] [Google Scholar]
- 21.Kilpatrick DG, Acierno R. Mental health needs of crime victims: epidemiology and outcomes. J Trauma Stress. 2003;16:119–132. [DOI] [PubMed] [Google Scholar]
- 22.Sherbourne CD, Hays RD, Fleishman JA, et al. Impact of psychiatric conditions on health-related quality of life in persons with HIV infection. Am J Psychiatry. 2000;157:248–254. [DOI] [PubMed] [Google Scholar]
- 23.Spire B, Duran S, Souville M, et al. Adherence to highly active antiretroviral therapies (HAART) in HIV-infected patients: from a predictive to a dynamic approach. Soc Sci Med. 2002;54:1481–1496. [DOI] [PubMed] [Google Scholar]
- 24.Singh N, Squier C, Sivek C, Wagener M, Nguyen MH, Yu VL. Determinants of compliance with antiretroviral therapy in patients with human immunodeficiency virus: prospective assessment with implications for enhancing compliance. AIDS Care. 1996;8: 261–269. [DOI] [PubMed] [Google Scholar]
- 25.Bartlett JA. Addressing the challenges of adherence. J Acquir Immune Defic Syndr. 2002;29(suppl 1): S2–S10. [DOI] [PubMed] [Google Scholar]
- 26.Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol. 2000;19: 124–133. [PubMed] [Google Scholar]
- 27.Arnsten JH, Demas PA, Grant RW, et al. Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. J Gen Intern Med. 2000;17:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2002;133: 21–30. [DOI] [PubMed] [Google Scholar]
- 29.Turner BJ, Fleishman JA, Wenger N, et al. Effects of drug abuse and mental disorders on use and type of antiretroviral therapy in HIV-infected persons. J Gen Intern Med. 2001;16:625–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fairfield KM, Libman J, Davis RB, Eisenberg DM. Delays in protease inhibitor use in clinical practice. J Gen Intern Med. 1999;14:395–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. HIV AIDS Surveill Rep. 2002;14(2)(2): Table 2.
- 32.Centers for Disease Control and Prevention. HIV AIDS Surveill Rep. 2001;13(2): Table 2.
- 33.Centers for Disease Control and Prevention. Year-end edition. HIV AIDS Surveill Rep. 2000;12(2).
- 34.Centers for Disease Control and Prevention. Year-end edition. HIV AIDS Surveill Rep. 1999;11(2).
- 35.Centers for Disease Control and Prevention. Year-end edition. HIV AIDS Surveill Rep. 1998;10(2).
- 36.Centers for Disease Control and Prevention. Year-end edition. HIV AIDS Surveill Rep. 1997;9(2).
- 37.Centers for Disease Control and Prevention. Year-end edition. HIV AIDS Surveill Rep. 1996;8(2).
- 38.Leserman J, Whetten K, Lowe K, Stangl D, Swartz M, Thielman NM. How trauma, recent stressful events and PTSD impact functional health status and health utilization in HIV-infected patients in the South. Psychosom Med. 2005;67:500–507. [DOI] [PubMed] [Google Scholar]
- 39.Kilpatrick DG, Resnick HS. A description of the posttraumatic stress disorder field trial. In: Davidson JRT, Foa EB, eds. Posttraumatic Stress Disorder: DSM-IV and Beyond. Washington, DC: American Psychiatric Press; 1993:113–143.
- 40.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. [DOI] [PubMed] [Google Scholar]
- 41.Whetten-Goldstein K, Nguyen TQ. You’re the First One I’ve Told: New Faces of HIV in the South. New Brunswick, NJ: Rutgers University Press; 2002.
- 42.Koss MP, Gidycz CA. Sexual experiences survey: reliability and validity. J Consult Clin Psychol. 1985;53: 422–423. [DOI] [PubMed] [Google Scholar]
- 43.Leserman J, Drossman DA, Li Z, Toomey TC, Nachman G, Glogau L. Sexual and physical abuse history in gastroenterology practice: how types of abuse impact health status. Psychosom Med. 1996;58:4–15. [DOI] [PubMed] [Google Scholar]


