Abstract
Objective: Depression is common among patients with chronic obstructive pulmonary disease (COPD). Patients with COPD may be more likely to have inadequate treatment with antidepressant medications. We tested the hypothesis that depressed patients with COPD have lower odds of adequate duration of antidepressant therapy in the first 3 months of treatment compared to those without COPD.
Method: Using administrative and centralized pharmacy data from 14 northeastern Veterans Affairs Medical Centers, we identified 778 veterans with depression (ICD-9-CM codes 296.2x, 296.3x, and 311.xx) who were in the acute phase of antidepressant treatment from June 1, 1999, through August 31, 1999. Within this group, we identified those patients with COPD (23%). An adequate duration of antidepressant treatment was defined as ≥ 80% of days on an antidepressant. We used multivariable logistic regression models to determine the adjusted odds of adequate acute phase antidepressant treatment duration.
Results: Those patients with COPD had markedly lower odds of adequate acute phase treatment duration (odds ratio = 0.67, 95% CI = 0.47 to 0.96); this was not observed with other medical diagnoses such as coronary heart disease, diabetes mellitus, or osteoarthritis.
Conclusions: The first few months of treatment appears to be a critical period for depressed patients with COPD who are started on antidepressants. The causes for early antidepressant treatment inadequacy among patients with COPD require further investigation. More intensive efforts may be necessary early in the course of treatment to assure high-quality pharmacologic therapy of depressed patients with COPD.
Chronic obstructive pulmonary disease (COPD) and depression are major health concerns. COPD was the fourth leading cause of death in the United States in 2001,1 and it was the fourth most common discharge diagnosis from Veterans Affairs (VA) hospitals.2 Depression is a leading cause of disability worldwide.3 Over a quarter of VA outpatients screened positive for depression in a study conducted in 4 Boston-area VA medical centers.4 Of note, depression is prevalent among patients with COPD.5
The deleterious effect of comorbid illnesses on the care of other disorders is well recognized. Unrelated medical disorders in elderly patients with chronic medical diseases are often undertreated.6 The rate of preventive service delivery to VA patients with chronic medical conditions was lower among those with psychiatric disorders.7 Among diabetic patients, diabetes care is worse among those with mental disorders.8,9 The quality of mental health care is also impacted by comorbid medical illness. Koike and colleagues10 found that depression outcomes were worse among patients who had comorbid medical diseases. A trial examining response to antidepressant treatment revealed that, in the acute phase of treatment, the total burden of comorbid medical disease predicted a worse depression outcome.11 The negative relationship between chronic medical illness and mental disorders may be exacerbated by poor self-care by the patient. For instance, it has been shown that depression is related to worse medication adherence.12 The extent to which COPD and depression influence one another in terms of quality of care is not well understood.
Treating depression in patients with COPD is important for a number of reasons. In general, lack of improvement in depressive symptoms predicted higher mortality rates among elderly veterans with comorbid medical illness.13 For patients with COPD, the high prevalence of depression is a concern, as well as the burdens these diseases confer alone and in combination. Among patients with COPD, depression has been associated with worse health-related quality of life,14 which, in turn, has been independently associated with higher mortality.15 Some research has demonstrated the efficacy of various modalities for treating depression in patients with COPD. For example, psychotherapy improved depression and anxiety symptoms,16 and 1-session cognitive behavioral therapy reduced depressive and anxious symptoms.17 Antidepressants have also been shown to be effective for treating depression in patients with COPD.18,19
Antidepressant prescribing is increasing in primary care,20 and some antidepressant agents may even have effects beyond their primary indication, such as reducing symptoms of dyspnea in patients with COPD.19 However, patients with COPD with depression may be more likely to have poor adherence to antidepressants, and this may be observed early in the course of treatment. A pharmacologic trial for depression in elderly patients with COPD found that 25% of these patients accepted treatment, and only 12% completed the trial.21 Poor antidepressant adherence often results in inadequate treatment, which may translate to worse outcomes such as relapse and recurrence.22 The majority of antidepressant treatment inadequacy is related to duration; in VA patients, 10% did not have an adequate course of treatment due to dose, but 55% did not due to duration.23 We tested the hypotheses that patients with COPD in the acute phase of antidepressant treatment have lower odds of an adequate duration of treatment compared to those without COPD and, secondly, that this effect was associated specifically with COPD by testing the relationship in selected other chronic medical illnesses in which depression is prevalent.
METHOD
We used administrative and centralized pharmacy data from 14 northeastern VA hospitals to create a cohort of veterans with depression who were treated with antidepressants in fiscal years 1998 and 1999 (October 1, 1997, through September 30, 1999). This study was institutional review board–approved, and the dataset contained no identifiers as per Health Insurance Portability and Accountability Act regulations.
Patients with depression were identified by at least 1 ICD-9-CM code of 296.2x (major depressive disorder, single episode) or 296.3x (major depressive disorder, recurrent episode) at a psychiatry, primary care, emergency, or social work visit or at least 1 code of 311.xx (depressive disorder, not elsewhere classified) at a primary care visit, as this was the only code available on the primary care encounter forms for depression. Any patient with major psychiatric comorbidity (schizophrenia and/or bipolar disorder: ICD-9-CM codes 295.00 to 295.95 or 296.00 to 296.89, excluding 296.20 to 296.36) for whom the diagnosis was coded in 2 outpatient visits or 1 inpatient admission was excluded. We then limited our study population to those patients who filled a prescription for any antidepressant from June 1, 1999, through August 31, 1999, which was the profiling period. Antidepressants included the selective serotonin reuptake inhibitors (sertraline, paroxetine, citalopram, fluoxetine, fluvoxamine), the tricyclics (amitriptyline, desipramine, doxepin, imipramine, nortriptyline, protriptyline, trimipramine, clomipramine), and all others (trazodone, bupropion, phenelzine, tranylcypromine, maprotiline, nefazo-done, venlafaxine, mirtazapine, amoxapine).
The acute phase of antidepressant treatment is the first 3 months on the medication after the initial depression diagnosis. To determine that treatment in our cohort was in the acute phase, we used a clean period of 6 months.22,24 Therefore, in order for a patient to be classified as being in the acute phase of treatment, the 6 months prior to the initial visit when depression was coded as a diagnosis had to be free of both depression-coded clinical visits and antidepressant prescriptions. We then limited the cohort to only those patients in the acute phase of treatment, so that the final population for our study were veterans with a depression diagnosis who were receiving acute phase antidepressant treatment within the profiling period.
The course of antidepressant treatment was determined using the pharmacy database during the profiling period, and it was based on a prescription filled for one of the antidepressants listed above and subsequently refilled. We determined the proportion of days in the profiling period on an antidepressant. This proportion was calculated by dividing the number of days to the time of refill by the number of days for which the antidepressant was prescribed, which is specified in all prescriptions done in the VA electronic medical record. We defined an adequate antidepressant treatment duration as 80% of days of the profiling period or more on an antidepressant. An 80% daily adherence rate has been previously used as a standard for adequate antidepressant use.23,24
We identified those with COPD by identifying those veterans who had at least 1 ICD-9-CM code of 490 to 496 in either the inpatient or the outpatient dataset. Other characteristics available from the dataset were age, race, sex, service-connected disability, annual income, marital status, type of clinical care (primary care only, psychiatry only, primary care and psychiatry), medical comorbidity burden, psychiatric comorbidity (anxiety disorder, posttraumatic stress disorder), current tobacco use, alcohol abuse, and substance abuse. Medical comorbidity burden was the unweighted count of up to 30 medical conditions defined from the Veterans Health Study.25
We used t test and χ2 analyses to compare sociodemo-graphic variables, comorbidity, and duration adequacy between those veterans with and without COPD. We used multivariable logistic regression models to determine the adjusted odds of adequate antidepressant treatment duration for those veterans with COPD compared to those without COPD. We included all covariates as described above in the multivariable model.
To test whether antidepressant treatment adequacy was specifically related to COPD, we replaced COPD in the models with 3 other chronic medical illnesses and repeated the analyses as described above for each. We chose coronary heart disease (CHD), diabetes mellitus (DM), and osteoarthritis (OA) for these analyses because of the high rates of depression diagnosis in each.26–28 We identified veterans with CHD by ICD-9-CM codes 410.xx, 411.xx, 412, 413.xx, or 414.0x in either the inpatient or outpatient databases. Likewise, those with DM were identified by ICD-9-CM codes 250.xx, 357.2, 362.0, or 648.0, and an OA diagnosis was ascertained through ICD-9-CM code 715.xx. In addition to the models for which each diagnosis was considered singly, to account for factors related to these other illnesses, we ran the model with COPD, CHD, DM, and OA included simultaneously.
RESULTS
We identified 778 depressed patients who were in the acute phase of antidepressant treatment during the profiling period and had an assessment of the duration of their antidepressant treatment. Of these patients, 23% had COPD.
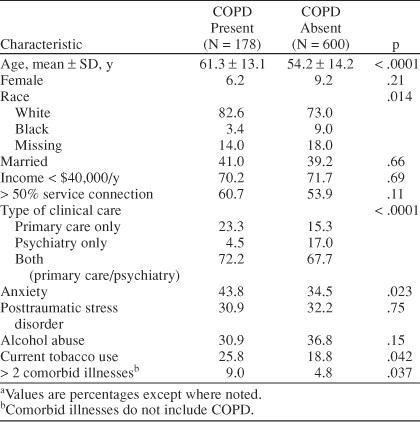
Table 1 compares depressed veterans in the acute phase of antidepressant treatment with and without COPD. Compared to those without COPD, veterans with COPD were significantly older, and they were more commonly white. Of note, 17% of the veterans in our study were missing race information; accordingly, we added “missing” as a category for race rather than excluding these veterans from analysis. Veterans with COPD also had significantly more anxiety and current tobacco use. The burden of comorbid medical illness (in addition to COPD) was greater among those veterans with COPD. Veterans with COPD more commonly received their antidepressants from primary care alone than those without COPD. Sex, marital status, adjusted gross income, service connectedness, prevalence of posttraumatic stress disorder, and prevalence of alcohol abuse did not differ significantly between those patients with and without COPD.
Table 1.
Characteristics of Depressed Veterans Taking Antidepressants With and Without Chronic Obstructive Pulmonary Disease (COPD)a
In the acute phase of antidepressant treatment, the proportion of depressed veterans with an adequate duration of treatment was significantly lower for those with COPD than without (52.8% vs. 63.2%, respectively, p = .01). In the multivariable analysis, the adjusted odds for an adequate course of acute phase antidepressant treatment was 34% lower for those veterans with COPD compared to those without COPD (odds ratio [OR] = 0.67, 95% CI = 0.47 to 0.96).
Other Chronic Diseases
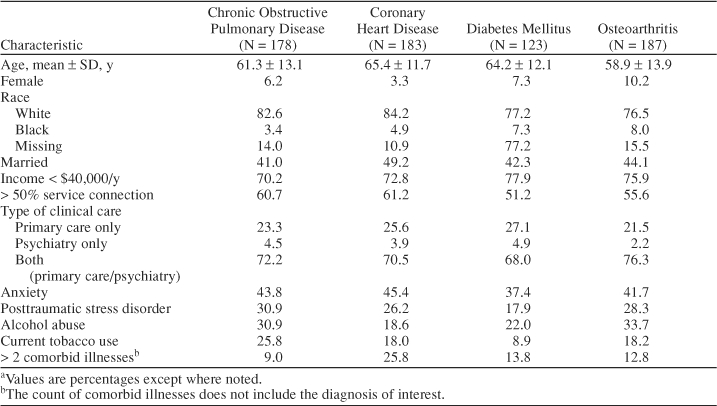
In order to test whether the findings described above were attributable to the diagnosis of COPD, we replaced COPD in the models with CHD, DM, and OA. The prevalence of CHD in our population was 24%; it was 16% for DM and 24% for OA. For perspective, given our findings for COPD, 35% of those veterans with CHD had COPD, 23% of those with DM had COPD, and 27% of those with OA had COPD. Characteristics of patients with each disease are displayed in Table 2; statistical differences were not tested, as many patients had multiple medical comorbidities and therefore were counted within each disease.
Table 2.
Characteristics of Depressed Veterans With Chronic Obstructive Pulmonary Disease, Diabetes Mellitus, Coronary Heart Disease, and Osteoarthritis Taking Antidepressantsa
We compared the frequency of adequate acute phase antidepressant treatment between those who had these 3 other diagnoses (CHD, DM, and OA) and those who did not have these diagnoses. The proportion of veterans with CHD who had adequate acute phase treatment was 65.6% compared to 59.3% among veterans who did not have a diagnosis of CHD (p = .13). Among veterans with DM, 64.2% had an adequate course of acute phase antidepressant treatment, whereas 60.2% of veterans who did not have DM had an adequate course (p = .40). For those with a diagnosis of OA, 61.5% of patients had an adequate course versus 60.6% among veterans who did not have OA (p = .82). When we replaced COPD diagnosis singly in the multivariate model with CHD, DM, and OA, as in the univariate analysis, we found that the presence of CHD was associated with a higher rate of adequate acute phase antidepressant treatment (OR = 1.56, 95% CI = 1.04 to 2.32). We did not find a significant relationship between acute phase antidepressant treatment adequacy and DM (OR = 1.17, 95% CI = 0.76 to 1.79) or OA (OR = 1.04, 95% CI = 0.73 to 1.48).
A model that included all 4 diagnoses (COPD, CHD, DM, OA) in addition to the other covariates had nearly the same result for COPD as when considered singly. The adjusted odds for adequate acute phase treatment was 0.62 (95% CI = 0.44 to 0.87) for veterans with COPD compared to those without COPD. This approach shifted the finding for CHD to nonsignificant by increasing the width of the confidence interval to include unity (OR = 1.39, 95% CI = 0.97 to 1.99). The findings for DM and OA were essentially unchanged (DM: OR = 1.11, 95% CI = 0.73 to 1.67; OA: OR = 1.06, 95% CI = 0.75 to 1.48).
DISCUSSION
We found that those patients with a COPD diagnosis had 34% lower odds of adequate duration of antidepressant use in the acute phase of treatment compared to those without a COPD diagnosis, even when adjusting for potential confounders. Analysis of other common medical illnesses with high rates of depression (e.g., DM, CHD, and OA) did not yield similar results as those for COPD. In addition, our findings with inclusion of all 4 of the diagnoses (COPD, CHD, DM, and OA) suggest that demographic differences across the diagnoses are not enough to substantively change the findings with respect to COPD. Therefore, the lower rate of adequate acute phase antidepressant treatment appears to be related specifically to a COPD diagnosis.
Other researchers have examined the relationship between depression treatment and comorbid medical disease. Iosifescu and coworkers11 found that depressed patients with a greater burden of medical illnesses have worse depression outcomes in the acute phase of treatment. They also examined the continuation phase of treatment and found that the odds of depression relapse increased with greater medical illness burden and with medical illness severity.29 In this study of the continuation phase, the rate of antidepressant continuation was not related to medical comorbidity burden. These studies are important with respect to the study we present here because they directly examined depression outcomes, as opposed to antidepressant treatment adequacy, which is a process outcome that could lead to worse depression outcomes. However, these studies did not examine specific diagnoses as we did, and our work indicates that rates of antidepressant treatment adequacy are not the same for different medical diagnoses. How our findings would translate to depression outcomes is a topic for future research.
Work examining Health Employer Data and Information Set criteria for depression management found that patient nonadherence was a major cause for inadequate treatment in the acute and continuation phases.30 Therefore, the causes for inadequate treatment that we observed in the acute phase of therapy are likely to be similar to those described in Yohannes and colleagues'21 report on a largely unsuccessful pharmacologic intervention for depression in COPD. The reasons patients in that trial gave for refusing antidepressants included frustration with the number of medications, rationalization of the problem, denial, and stigma. Our findings, which were in a real world setting, in combination with Yohannes and coworkers' experimental setting,21 suggest that the first few months of antidepressant treatment are a critical period for depressed COPD patients in terms of treatment adequacy.
Other reasons may underlie the poor acute phase antidepressant adherence in patients with COPD. The stigma of being labeled with a psychiatric diagnosis is a concern with respect to an older patient's decision to discontinue depression treatment.31 It is possible that the stigma related to depression may combine with social stigma among patients with COPD regarding oxygen use,32 which we were not able to explore. Another reason may be side effects of antidepressant medications, although some work has suggested that certain antidepressants may actually help with dyspnea.19 Physician concerns with use of antidepressants in depressed patients with COPD due to medication interactions or other such concerns may play a role, even though the evidence for use of antidepressants in chronic medical illnesses including COPD is favorable.33 Comorbidity with anxiety and posttraumatic stress disorder was common in our study population, and this may also have played a role. A concern that brings the agenda of physician and patient together is that of competing demands.34 Other problems in patients with COPD may compete with depression treatment to the detriment of adequate antidepressant treatment. Of course, the same demands might be expected in DM, CHD, and OA, yet we did not observe the same pattern of antidepressant treatment inadequacy.
Some limitations of the presented work should be acknowledged. Our study was observational, and the source of data is administrative records, both of which have inherent limitations. We did not have a means of assessing severity of depression, which is, in itself, a limitation, but could also lead to a treatment bias. Such a bias would manifest if those patients with COPD had less severe depression and, in turn, may have been subjected to less intensive efforts to continue antidepressant treatment that had been initiated, which would result in our finding that patients with COPD had adequacy rates worse than those without COPD in the acute phase of treatment. Misclassification bias is a possibility, so that those who truly have COPD were not identified as such, but this would bias toward the null. This concern is further mitigated by the high demonstrated accuracy of an outpatient diagnosis of COPD from the VA's computerized databases.35 We assumed that veterans who filled prescriptions were taking at least some of the medications they received and therefore may have included those who never initiated treatment with those who did exceed 80% of days on the medication. Lastly, we do not know the cause for inadequate treatment—it is possible that patients with COPD were a sicker population who may have been more likely to have had a hospitalization interrupt their course of antidepressants. However, those with CHD, DM, and OA might also be prone to such a situation, but our findings for patients with COPD were not similar to these other chronic diseases.
In conclusion, we found that, among veterans with a diagnosis of COPD, the odds of an adequate course of antidepressant therapy were lower in the first few months of treatment. A similar phenomenon was not observed in other chronic medical conditions that are prevalent among veterans and have known elevated rates of depression. Our findings suggest that the critical period in pharmacologic treatment of depressed patients with COPD may be the first few months after the initiation of antidepressant treatment. Our findings are also a “real life” affirmation of the observation that patients with COPD do poorly with respect to antidepressant treatment.21 The causes for early antidepressant treatment inadequacy among patients with COPD are worthy of investigation. Our findings might be applied in both clinic and research settings, wherein more intensive efforts may be necessary to assure good antidepressant treatment of depressed patients with COPD.
Drug names: bupropion (Wellbutrin and others), citalopram (Celexa and others), clomipramine (Anafranil and others), desipramine (Norpramin and others), doxepin (Sinequan, Zonalon, and others), fluoxetine (Prozac and others), imipramine (Tofranil and others), mirtazapine (Remeron and others), nortriptyline (Aventyl, Pamelor, and others), paroxetine (Paxil, Pexeva, and others), phenelzine (Nardil), protriptyline (Vivactil), sertraline (Zoloft), tranylcypromine (Parnate), trazodone (Desyrel and others), trimipramine (Surmontil), venlafaxine (Effexor).
Footnotes
Support for this work was from the Department of Veterans Affairs, Health Services Research & Development Service, Research Career Development Award 04-321 (Dr. Pirraglia) and grant #CPI 99-134 (Drs. Charbonneau, Kader, and Berlowitz).
Earlier versions of this work were presented at the New England Regional Society of General Internal Medicine Meeting, Boston, Mass., March 5, 2004, and the Complexities of Cooccurring Conditions Conference, Washington, D.C., June 24, 2004.
Drs. Pirraglia, Charbonneau, Kader, and Berlowitz report no additional financial or other affliliations relevant to the subject of this article.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
REFERENCES
- Arias E, Anderson R, and Hsiang-Ching K. et al. Deaths: Final Data for 2001. Hyattsville, Md: National Center for Health Statistics. 2003 [PubMed] [Google Scholar]
- Roman J, Perez RL. COPD in VA hospitals. Clin Cornerstone. 2003;5:37–44. doi: 10.1016/s1098-3597(03)90007-x. [DOI] [PubMed] [Google Scholar]
- The World Health Report 2001. Mental Health: New Understanding, New Hope. Geneva, Switzerland: World Health Organization. 2001 [Google Scholar]
- Kazis LE, Miller DR, and Clark J. et al. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998 158:626–632. [DOI] [PubMed] [Google Scholar]
- Kunik ME, Roundy K, and Veazey C. et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005 127:1205–1211. [DOI] [PubMed] [Google Scholar]
- Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. N Engl J Med. 1998;338:1516–1520. doi: 10.1056/NEJM199805213382106. [DOI] [PubMed] [Google Scholar]
- Druss BG, Rosenheck RA, and Desai MM. et al. Quality of preventive medical care for patients with mental disorders. Med Care. 2002 40:129–136. [DOI] [PubMed] [Google Scholar]
- Desai MM, Rosenheck RA, and Druss BG. et al. Mental disorders and quality of diabetes care in the Veterans Health Administration. Am J Psychiatry. 2002 159:1584–1590. [DOI] [PubMed] [Google Scholar]
- Jones LE, Clarke W, Carney CP. Receipt of diabetes services by insured adults with and without claims for mental disorders. Med Care. 2004;42:1167–1175. doi: 10.1097/00005650-200412000-00003. [DOI] [PubMed] [Google Scholar]
- Koike AK, Unutzer J, Wells KB. Improving the care for depression in patients with comorbid medical illness. Am J Psychiatry. 2002;159:1738–1745. doi: 10.1176/appi.ajp.159.10.1738. [DOI] [PubMed] [Google Scholar]
- Iosifescu DV, Nierenberg AA, and Alpert JE. et al. The impact of medical comorbidity on acute treatment in major depressive disorder. Am J Psychiatry. 2003 160:2122–2127. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- Lavretsky H, Bastani R, and Gould R. et al. Predictors of 2-year mortality in a prospective “UPBEAT” study of elderly veterans with comorbid medical and psychiatric symptoms. Am J Geriatr Psychiatry. 2002 10:458–468. [PubMed] [Google Scholar]
- Felker B, Katon W, and Hedrick SC. et al. The association between depressive symptoms and health status in patients with chronic pulmonary disease. Gen Hosp Psychiatry. 2001 23:56–61. [DOI] [PubMed] [Google Scholar]
- Sprenkle MD, Niewoehner DE, and Nelson DB. et al. The Veterans Short Form 36 questionnaire is predictive of mortality and health-care utilization in a population of veterans with a self-reported diagnosis of asthma or COPD. Chest. 2004 126:81–89. [DOI] [PubMed] [Google Scholar]
- de Godoy DV, de Godoy RF. A randomized controlled trial of the effect of psychotherapy on anxiety and depression in chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2003;84:1154–1157. doi: 10.1016/s0003-9993(03)00239-9. [DOI] [PubMed] [Google Scholar]
- Kunik ME, Braun U, and Stanley MA. et al. One session cognitive behavioural therapy for elderly patients with chronic obstructive pulmonary disease. Psychol Med. 2001 31:717–723. [DOI] [PubMed] [Google Scholar]
- Borson S, McDonald G, and Gayle T. et al. Improvement in mood, physical symptoms, and function with nortriptyline for depression in patients with chronic obstructive pulmonary disease. Psychosomatics. 1992 33:190–201. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Pollack MH, and Systrom D. et al. Sertraline effects on dyspnea in patients with obstructive airways disease. Psychosomatics. 1998 39:24–29. [DOI] [PubMed] [Google Scholar]
- Pirraglia PA, Stafford RS, Singer DE. Trends in prescribing of selective serotonin reuptake inhibitors and other newer antidepressant agents in adult primary care. Prim Care Companion J Clin Psychiatry. 2003;5:153–157. doi: 10.4088/pcc.v05n0402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yohannes AM, Connolly MJ, Baldwin RC. A feasibility study of antidepressant drug therapy in depressed elderly patients with chronic obstructive pulmonary disease. Int J Geriatr Psychiatry. 2001;16:451–454. doi: 10.1002/gps.461. [DOI] [PubMed] [Google Scholar]
- Melfi CA, Chawla AJ, and Croghan TW. et al. The effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depression. Arch Gen Psychiatry. 1998 55:1128–1132. [DOI] [PubMed] [Google Scholar]
- Charbonneau A, Rosen AK, and Ash AS. et al. Measuring the quality of depression care in a large integrated health system. Med Care. 2003 41:669–680. [DOI] [PubMed] [Google Scholar]
- Kerr EA, McGlynn EA, and Van Vorst KA. et al. Measuring antidepressant prescribing practice in a health care system using administrative data: implications for quality measurement and improvement. Jt Comm J Qual Improv. 2000 26:203–216. [DOI] [PubMed] [Google Scholar]
- Selim AJ, Fincke G, and Ren XS. et al. Comorbidity assessments based on patient report: results from the Veterans Health Study. J Ambul Care Manage. 2004 27:281–295. [DOI] [PubMed] [Google Scholar]
- Ruo B, Rumsfeld JS, and Hlatky MA. et al. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003 290:215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson RJ, Freedland KE, and Clouse RE. et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001 24:1069–1078. [DOI] [PubMed] [Google Scholar]
- Penninx BW, van Tilburg T, and Deeg DJ. et al. Direct and buffer effects of social support and personal coping resources in individuals with arthritis. Soc Sci Med. 1997 44:393–402. [DOI] [PubMed] [Google Scholar]
- Iosifescu DV, Nierenberg AA, and Alpert JE. et al. Comorbid medical illness and relapse of major depressive disorder in the continuation phase of treatment. Psychosomatics. 2004 45:419–425. [DOI] [PubMed] [Google Scholar]
- Kobak KA, Taylor L, and Katzelnick DJ. et al. Antidepressant medication management and Health Plan Employer Data Information Set (HEDIS) criteria: reasons for nonadherence. J Clin Psychiatry. 2002 63:727–732. [DOI] [PubMed] [Google Scholar]
- Sirey JA, Bruce ML, and Alexopoulos GS. et al. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am J Psychiatry. 2001 158:479–481. [DOI] [PubMed] [Google Scholar]
- Earnest MA. Explaining adherence to supplemental oxygen therapy: the patient's perspective. J General Intern Med. 2002;17:749–755. doi: 10.1046/j.1525-1497.2002.20218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill D, Hatcher S. Antidepressants for depression in medical illness. Cochrane Database Syst Rev. 2000;4:CD001312. doi: 10.1002/14651858.CD001312.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaen CR, Stange KC, Nutting PA. Competing demands of primary care: a model for the delivery of clinical preventive services. J Fam Pract. 1994;38:166–171. [PubMed] [Google Scholar]
- Szeto HC, Coleman RK, and Gholami P. et al. Accuracy of computerized outpatient diagnoses in a Veterans Affairs general medicine clinic. Am J Manag Care. 2002 8:37–43. [PubMed] [Google Scholar]


