Abstract
The potential threat of smallpox as a bioweapon has led to the production and stockpiling of smallpox vaccine in some countries. Human monkeypox, a rare but important viral zoonosis endemic to central and western Africa, has recently emerged in the United States. Thus, even though smallpox has been eradicated, a vaccinia virus vaccine that can induce protective immunity against smallpox and monkeypox is still invaluable. The ability of the highly attenuated vaccinia virus vaccine strain LC16m8, with a mutation in the important immunogenic membrane protein B5R, to induce protective immunity against monkeypox in nonhuman primates was evaluated in comparison with the parental Lister strain. Monkeys were immunized with LC16m8 or Lister and then infected intranasally or subcutaneously with monkeypox virus strain Liberia or Zr-599, respectively. Immunized monkeys showed no symptoms of monkeypox in the intranasal-inoculation model, while nonimmunized controls showed typical symptoms. In the subcutaneous-inoculation model, monkeys immunized with LC16m8 showed no symptoms of monkeypox except for a mild ulcer at the site of monkeypox virus inoculation, and those immunized with Lister showed no symptoms of monkeypox, while nonimmunized controls showed lethal and typical symptoms. These results indicate that LC16m8 prevents lethal monkeypox in monkeys, and they suggest that LC16m8 may induce protective immunity against smallpox.
Three decades have passed since the global eradication of smallpox (variola). This eradication was made possible by the development of effective vaccinia virus vaccines (VVs), such as strains Lister and Dryvax. Unfortunately, we now face the potential threat of bioterrorism with variola virus, the causative agent of variola. This threat has led to the production and stockpiling of vaccinia virus-based vaccines in several countries. Human monkeypox (MPX), infection of humans with monkeypox virus (MPXV), is endemic to central and western Africa (18), and the first human MPX outbreaks outside Africa were reported in the United States in 2004 (6, 9, 30). Most human MPX patients in this outbreak acquired the virus from prairie dogs (Cynomys spp.) that became ill after contact with various exotic rodents shipped from Ghana, Africa (30). Therefore, VVs are still of great importance, although variola has already been eradicated.
LC16m8, a highly attenuated VV strain, was developed in the early 1970s by multiple passages in cell culture through a temperature-sensitive and low-virulence strain, LC16mO, from the original Lister strain (Elstree) (11, 36). LC16m8 forms smaller plaques than Lister in the chicken chorioallantoic membrane. LC16m8 is temperature sensitive, as demonstrated by the fact that LC16m8 does not grow well in primary rabbit kidney (PRK) cells cultured at 41°C, while Lister grows efficiently (36). The fact that LC16m8 grows efficiently in PRK cells but not in African green monkey kidney (Vero) cells, while the parental strain Lister grows well in both cell lines, suggests that LC16m8 has a narrow host cell range, growing in a cell-selective manner (36).
We recently determined the complete genome sequences of LC16m8, the parental LC16mO strain, and the original Lister strain (GenBank accession no. AY678275, AY678277, and AY678276, respectively) (24). It was revealed that there was a single nucleotide deletion of guanosine (G) at the 274th position from the initiation codon in the membrane protein gene B5R (GenBank accession no. M55434 and AY678275) that generated a premature termination codon and truncated the B5R membrane protein of LC16m8 extracellular enveloped virions (EEV) at amino acid position 93. LC16m8 may possess nearly all the open reading frames corresponding to the VV strains Copenhagen and Lister except for the membrane protein B5R. Because Lister had no history of virus cloning, nucleotide polymorphisms were observed at more than 1,000 sites in the whole genome, indicating that it is difficult to make a simple comparison between the nucleotide sequences of LC16m8 and Lister. However, alignments of the EEV-related membrane proteins in LC16m8 and Lister indicated that there were only 1, 1, 1, and 2 amino acid differences in the EEV-related membrane proteins A36R, F13L, A56R, and A33R, respectively, and that the EEV-related membrane protein A34R of LC16m8 was identical to that of Lister. Although the genetic background responsible for the temperature sensitivity has not been elucidated, it has been confirmed that mutation in the membrane protein gene B5R is responsible for small-plaque formation and cell-selective growth of this strain (35).
LC16m8 has very low neurovirulence in animal models (11). More than 100,000 people were vaccinated with LC16m8 in Japan, but no LC16m8-associated adverse events such as serious complications and/or death were reported. The currently available VVs, such as strains Lister and Dryvax, are known to be efficacious. However, severe adverse events, such as encephalitis, encephalopathy, progressive and generalized vaccinia, ocular vaccinia virus infections, and cardiac dysfunction, have been reported for recipients and are of great concern (1, 2, 4, 10, 16, 22, 23, 25, 31, 33, 38). These observations suggest that LC16m8 is safer than the currently used VVs derived from bovine skin (20, 21). Thus, LC16m8 is considered a potentially useful replacement for the currently available VVs.
Unfortunately, the protective efficacy of LC16m8 against variola has not been evaluated, because variola had already been eradicated at the time of its development. LC16m8 lacks expression of the full-length membrane protein B5R, one of the most immunogenic proteins, because of a frameshift mutation in the membrane protein gene B5R (19, 35). It is expected that LC16m8 does not pass through the EEV stage in the viral life cycle, because the membrane protein B5R is essential in packaging the intracellular mature virion with the trans-Golgi membrane or endosomal cisternae to form intracellular enveloped virions (13, 32, 34) and this protein is also involved in the release of cell-associated enveloped virions from the cell surface to form EEV in cooperation with proteins A36R and A33R (17, 29). Furthermore, the membrane protein B5R induces protective neutralizing antibodies to EEV in vaccinia (8, 14, 15, 34). Recently, it was reported that LC16m8 induced protective immunity to vaccinia virus challenge in mice and rabbits (19, 24). However, the protective efficacy of LC16m8 against variola and human MPX has not been confirmed in humans.
If LC16m8 is as efficacious as Lister and Dryvax, it will be of great benefit to humans, because it is expected to induce much less severe VV-associated adverse events. A nonhuman-primate model for MPXV infections is expected to mimic natural variola virus infection in humans. In the present study, the protective efficacy of LC16m8 against MPX was evaluated in comparison with that of Lister VV in cynomolgus monkeys (Macaca fascicularis). The present study was performed to examine the protective efficacy of LC16m8 against variola in humans.
MATERIALS AND METHODS
Virus, vaccinia virus vaccines, and cells.
MPXV strains Liberia and Zr-599, used in challenge experiments, and MPXV Congo-8, used in the neutralizing antibody assay, had been kept in the National Institute of Infectious Diseases. Strain Liberia was originally isolated from a patient with MPX in Liberia, and strain Zr-599 was from a patient with MPX in the Democratic Republic of Congo (formerly Zaire), suggesting that the former originated from West Africa and the latter from the Congo Basin. It is suggested that MPXV originating from West Africa is less virulent than MPXV originating from the Congo Basin (3). The virus was confirmed to be MPXV by determining the specific nucleotide sequence of the ATI gene of MPXV (28). The infectious dose of the virus was determined by plaque assays on Vero cells, which were purchased from the American Type Cell Collection (Manassas, VA). Vero cells were grown in Eagle's minimum essential medium supplemented with penicillin G and streptomycin and with 5% fetal bovine serum (MEM-5FBS). LC16m8 vaccine was produced by the Chiba Serum Research Institute, Chiba, Japan, and Lister vaccine was produced by the Kitasato Research Institute, Kanagawa, Japan. The titers of the two vaccines were higher than 1 × 108 PFU/ml.
Nonhuman primates and vaccination.
One male and 14 female cynomolgus monkeys (Macaca fascicularis), aged 3 to 4 years and weighing 2,180 to 3,100 g, were used in the experiments (Table 1). These monkeys were born and raised in the Tsukuba Primate Center for Medical Research, National Institute of Infectious Diseases, Tsukuba, Japan. They were assigned to six groups as shown in Table 1: group IN-Naïve, consisting of naïve monkeys challenged intranasally with MPXV (monkeys 4595 and 4596), group IN-Lister, consisting of monkeys immunized with Lister and challenged intranasally with MPXV (monkeys 4597, 4598, and 4599), group IN-LC16m8 (monkeys 4600, 4601, and 4602), group SC-Naïve, consisting of naïve monkeys challenged subcutaneously with MPXV (monkeys 4651 and 4653), group SC-Lister (monkeys 4575 and 4576), and group SC-LC16m8 (monkeys 4577, 4525, and 4526). Monkeys were immunized with each of the vaccines by the multiple-puncture method with standard bifurcated needles in the same way as immunization is performed for humans. Briefly, a bifurcated needle holding a drop of vaccine was pressed more than 15 times into the skin at the vaccination site.
TABLE 1.
Characteristics, MPX-associated symptoms, and viremia in mock-immunized monkeys and those immunized with Lister or LC16m8
| Group | IDa | Vaccination | Sexb (wt [g] | MPXV challenge strain (route,c dose [PFU]) | Virus isolationd (no. of plaques at the indicated day of collection) | MPX-associated symptoms
|
||
|---|---|---|---|---|---|---|---|---|
| Symptom(s) at the site of MPXV inoculation | No. of papulovesicular lesions | Outcome | ||||||
| Expt 1 | ||||||||
| IN-Naïve | 4595 | Mock | F (2,500) | Liberia (IN, 106) | Positive (20 at day 4, 10 at day 6, 10 at day 8) | Rhinorrhea | 10 | Survival |
| 4596 | F (2,320) | Positive (10 at day 6, 10 at day 13) | Rhinorrhea | 16 | Survival | |||
| IN-Lister | 4597 | Lister | F (2,360) | Negative | None | 0 | Survival | |
| 4598 | F (2,580) | Negative | None | 0 | Survival | |||
| 4599 | F (2,700) | Negative | None | 0 | Survival | |||
| IN-LC16m8 | 4600 | LC16m8 | F (2,650) | Negative | None | 0 | Survival | |
| 4601 | F (2,800) | Negative | None | 0 | Survival | |||
| 4602 | F (2,700) | Negative | None | 0 | Survival | |||
| Expt 2 | ||||||||
| SC-Naïve | 4651 | Mock | F (2,560) | Zr-599 (SC, 106) | Positive (4 at day 3, 5 at day 7, 33 at day 9, 30 at day 14) | Erythema, papulovesicles, ulcer | 390 | Death |
| 4653 | M (3,100) | Positive (176 at day 3, 18 at day 7, 3 at day 9, 23 at day 11, 9 at day 14, 3 at day 18) | Erythema, papulovesicles, ulcer | 1,150 | Death | |||
| SC-Lister | 4575 | Lister | F (2,980) | Negative | None | 0 | Survival | |
| 4576 | F (3,100) | Negative | None | 0 | Survival | |||
| SC-LC16m8 | 4577 | LC16m8 | F (2,640) | Positive (1 at day 3) | Erythema | 0 | Survival | |
| 4525 | F (2,180) | Positive (7 at day 3, 1 at day 6) | Erythema, papulovesicles, ulcer | 0 | Survival | |||
| 4526 | F (2,730) | Negative | Erythema, papulovesicles, ulcer | 0 | Survival | |||
ID, monkey identification number.
F, female; M, male.
IN, intranasal inoculation; SC, subcutaneous inoculation.
Positive or negative, MPXV was or was not isolated, respectively, during the observation period from challenge to sacrifice. In experiment 1, the intranasal inoculation model, virus isolation was attempted from aliquots of 106 purified PBMCs collected from monkeys on days 0, 2, 4, 6, 8, 10, 13, 16, and 20 after virus challenge. In experiment 2, the subcutaneous inoculation model, virus isolation was attempted from the buffy coat fractions collected from 4-ml aliquots of total peripheral blood collected on days 0, 3, 7, 9, 11, 14, and 18.
Assays of IgG antibody.
Levels of vaccinia virus-specific antibody were measured by an enzyme-linked immunosorbent assay (ELISA) using the entire vaccinia virus proteins as antigens, as reported previously, except for the secondary antibody conjugated with horseradish peroxidase (24). The secondary antibody was a goat anti-human immunoglobulin G (IgG) antibody conjugated with horseradish peroxidase purchased from Zymed Laboratories (South San Francisco, CA).
Neutralizing antibody assay.
Levels of neutralizing antibody to MPXV Congo-8 in the plasma samples were measured as reported previously with some modifications (12). Briefly, about 30 PFU of MPXV strain Congo-8 in 100 μl of MEM-2FBS was mixed with 100 μl of serially diluted heat-inactivated plasma samples and incubated at 4°C overnight. The mixtures were inoculated into Vero cell monolayers seeded in a 24-well culture plate and were incubated for 2 h for adsorption. The inocula were then removed, and the cells were cultured with MEM-2FBS supplemented with 0.5% methylcellulose. After a 3-day incubation, plaque numbers were counted. The neutralizing antibody titer was defined as the reciprocal of the dilution level at which the plaque number decreased to less than 50% of that in the control.
Cytokine assays.
The concentrations of tumor necrosis factor alpha (TNF-α), gamma interferon (IFN-γ), interleukin-2 (IL-2), IL-4, IL-6, and IL-10 in sera were determined using rhesus monkey TNF-α, monkey IFN-γ, rhesus monkey IL-2, monkey IL-4, human IL-6, and rhesus monkey IL-10 (BioSource International Inc., Camarillo, CA), respectively, according to the manufacturer's instructions.
Virus isolation from PBMCs or buffy coat fraction.
Virus was isolated using Vero cells from peripheral blood mononuclear cells (PBMCs) and buffy coat fractions obtained from monkeys inoculated intranasally and subcutaneously, respectively. PBMCs were isolated from peripheral blood by the Ficoll centrifugation method. Aliquots of 106 PBMCs were cocultivated with Vero cells in MEM-2FBS for 2 weeks, when PBMCs were used. The whole buffy coat fraction collected by centrifugation of 4 ml of peripheral blood was washed twice with a phosphate-buffered saline solution and then cocultivated with Vero cells as described above. When a cytopathic effect was observed in cell culture, the cytopathic effect agent was confirmed to be MPXV by an indirect immunofluorescence assay with an anti-vaccinia virus antibody prepared in our laboratory and by amplification of the ATI gene and sequencing of the amplicon (28). Furthermore, the plaque number was also counted.
Determination of MPXV loads in total peripheral blood by quantitative PCR.
DNAs were isolated from total peripheral blood using a Viral Nucleic Acid purification kit (Roche Diagnostics, Mannheim, Germany) according to the supplier's instructions. The primers and probes were designed based on the specific ATI gene on the MPXV genome. The sequences of primers and probes were as follows: forward primer, 5′-GAGATTAGCAGACTCCAA-3′; fluorescein probe, 5′-GCAGTCGTTCAACTGTATTTCAAGATCTGAGAT-3′-fluorescein; LCRed640 probe, 5′-LCRed640-CTAGATTGTAATCTCTGTAGCATTTCCACGGC-3′-phosphorylation; reverse primers, 5′-TCTCTTTTCCATATCAGC-3′ for amplification of the MPXV Liberia genome and 5′-GATTCAATTTCCAGTTTGTAC-3′ for amplification of the MPXV Zr-599 genome. The internal controls for determination of viral genome copy numbers of MPXV Liberia and MPXV Zr-599 were pGEM-T Easy vectors (Promega Cooperation, Madison, WI) carrying the ATI gene of MPXV strain Liberia or Zr-599, respectively, and were included in each quantitative real-time PCR (qPCR) assay. The reverse primer sequences were designed according the nucleotide sequences of the ATI genes of MPXV Liberia and Zr-599. Amplification conditions were 95°C for 10 min, followed by 40 cycles of 95°C for 10 s, 57°C for 10 s, and 72°C for 6 s, and a melting reaction.
Challenge with MPXV.
All the challenge experiments with MPXV were conducted in a highly contained laboratory at the National Institute of Infectious Diseases, Tokyo, Japan. The monkeys that were mock immunized or immunized with vaccines (Lister and LC16m8) were anesthetized and either inoculated intranasally with 0.5 ml of a virus solution containing 1 × 106 PFU of MPXV strain Liberia by using an atomizer (Keytron Co., Tokyo, Japan) to atomize the virus solution or inoculated subcutaneously with 0.5 ml of a virus solution containing 1 × 106 PFU of MPXV strain Zr-599. Blood samples were collected every week after immunization up to the time of challenge. After the challenge, blood was drawn every 2 to 4 days. Clinical manifestations, such as volume of food and water consumed, the appearance of feces, etc., were observed every day. When monkeys were anesthetized for drawing of blood, the skin surface was observed carefully, and body temperature and weight were measured.
Schedule for immunization and challenge.
In the present study, day zero was defined as the day on which monkeys were challenged with MPXV. All of the monkeys were challenged with MPXV at 5 weeks after immunization. Monkeys were challenged with MPXV (strain Liberia or Zr-599) on day zero and were observed for about 3 weeks.
Histopathological examination.
After sacrifice under deep anesthesia using ketaral, skin, lymph nodes, brain, lungs, heart, liver, spleen, pancreas, kidneys, bladder, gastrointestinal organs, and genitourinary tract structures were excised, fixed in 10% formalin in phosphate-buffered saline, and embedded in paraffin. Macroscopic and histological examinations were performed on the excised tissues and organs. Paraffin sections, 4 μm thick, were stained with hematoxylin and eosin (H&E) and with Luxol-Fast Blue for the brain. Immunohistochemistry (IHC) for the MPXV antigens was performed using paraffin sections according to the method described previously (26, 27). For detection of MPXV antigens, a rabbit anti-vaccinia virus serum was used.
RESULTS
Skin lesions after immunization with LC16m8 or Lister.
Immunization with LC16m8 or Lister induced “vaccine take” (pustules, scabs, and scarring) as shown in Fig. 1. The lesions reached a maximum size at about 2 weeks after immunization. On day 13 postimmunization, the area was 27 ± 11 mm2 with LC16m8, significantly smaller than the area of lesions induced by Lister (115 ± 65 mm2) (Fig. 1B). The lesions induced by Lister were more exudative and granulomatous than those induced by LC16m8. Satellite lesions appeared with Lister but not with LC16m8. Pigmentation of the scars was apparent with Lister, but not with LC16m8, on day 28.
FIG. 1.
Local cutaneous lesions at the site (upper left arm) of vaccination with Lister or LC16m8. (A) Typical vaccine-induced local lesions on the designated days postimmunization. Bars, 10 mm. (B) Sizes (areas) of the vaccine-induced lesions with Lister (n = 5) or LC16m8 (n = 6), measured on day 13 and shown as averages and standard deviations.
Protection of monkeys from intranasal MPXV challenge by immunization with LC16m8.
The challenge experiment included six groups: (i) the IN-Naïve group, comprising two monkeys vaccinated with mock vaccine (negative control) and challenged intranasally with MPXV strain Liberia; (ii) the IN-Lister group, comprising three monkeys vaccinated with Lister and challenged intranasally with MPXV strain Liberia; (iii) the IN-LC16m8 group, comprising three monkeys vaccinated with LC16m8 and challenged intranasally with MPXV strain Liberia; (iv) the SC-Naïve group, comprising two monkeys vaccinated with mock vaccine (negative control) and challenged subcutaneously with MPXV strain Zr-599; (v) the SC-Lister group, comprising two monkeys vaccinated with Lister and challenged subcutaneously with MPXV strain Zr-599; and (vi) the SC-LC16m8 group, comprising three monkeys immunized with LC16m8 and challenged subcutaneously with MPXV Zr-599.
The identification numbers of the monkeys and their sex, weight, and vaccination histories are shown along with summarized results in Table 1. The monkeys were challenged intranasally with MPXV 5 weeks after mock immunization or immunization with VVs (Table 1, experiment 1). Body weight decreased sharply after challenge, by approximately 10%, in group IN-Naïve but not in group IN-Lister or IN-LC16m8 (Fig. 2). In the IN-Naïve group, symptoms including loss of appetite, rhinorrhea and conjunctival discharge, diarrhea, skin rash (papulovesicular and ulcerative lesions, as shown in Fig. 3A), irritability, and decreased activity appeared around day 10 after challenge and continued for approximately 5 days. All the MPX-associated symptoms disappeared by day 20 after challenge except for the skin lesions. All animals in the IN-Lister and IN-LC16m8 groups survived and showed no symptoms associated with MPXV infection.
FIG. 2.
Changes in body weight, MPXV loads in total peripheral blood, and cytokine responses. (A) Body weight expressed as a percentage of that measured at the time of MPXV challenge. (B) Viral loads in total peripheral blood as measured by qPCR. (C) IFN-γ response. (D) IL-6 response. Left and right panels show these indicators for monkeys challenged intranasally with MPXV strain Liberia and subcutaneously with MPXV Zr-599, respectively.
FIG. 3.
Macroscopic and histological lesions observed in naïve monkeys infected with MPXV. (A) Macroscopic and histological lesions in the skin, lungs, and pancreas in the IN-Naïve group. Papulovesicular lesions were observed in the skin (a), and nodular and granulomatous lesions were present in the lungs (b) and pancreas (c). (d) The edges of the cutaneous lesions were characterized by epithelial cell swelling, epidermal hyperplasia, hyperkeratosis, necrosis, and infiltration of inflammatory cells. (e) Nodular and granulomatous lesions in the lungs were characterized by destruction of alveolar structures, necrosis, edema, proliferating fibroblasts, and infiltration of inflammatory cells. (f) Nodular and granulomatous lesions in the pancreas were characterized by extensive necrosis with infiltration of inflammatory cells and proliferating fibroblasts. (g to i) In these lesions, MPXV antigens were demonstrated by IHC analyses, indicating that they were caused by MPXV infection. (B) Macroscopic and histological lesions in the thymus, stomach, and colon in the SC-Naïve group. (a to c) Multiple nodular lesions were present in the thymus, and papilliform and granular lesions with hemorrhaging were seen in the lumens of the stomach and colon. (d) The lesions in the thymus were characterized by granulomatous inflammation and proliferation of fibrous tissue consisting of fibroblastic cells, histiocytes, and microvascular structures. (e) The histology in the stomach consisted of necrotic changes with inflammatory cells including neutrophils. (f) The submucosal area of the colon consisted of fibroblastic tissues with granulomatous inflammation characterized by infiltration of inflammatory cells. The mucosal membranes showed ulceration. (g to i) In these lesions, MPXV antigens were demonstrated by IHC analyses, indicating that they were caused by MPXV infection.
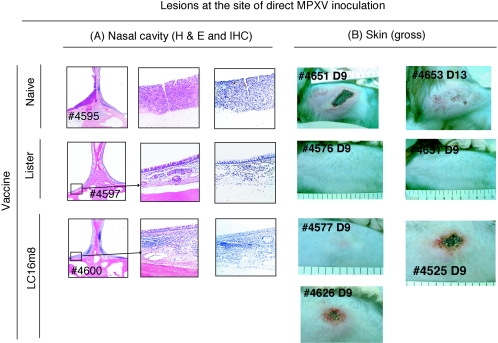
Histopathological examinations of the nasal cavity were carried out at the inoculation site to compare the efficacies of the vaccines in conferring protection against MPXV challenge. In IN-Naïve monkeys, the structures of the mucous membranes were damaged due to necrosis, inflammatory cell accumulation was seen, and MPXV antigens were detected in the lesions. In contrast, the nasal structures of the mucous membranes were maintained, and no MPXV antigens were detected, in the IN-Lister and IN-LC16m8 groups. Inflammation in the mucous membranes was detected in the IN-LC16m8 group but not in the IN-Lister group (Fig. 4).
FIG. 4.
Histology of the nasal cavity caused by intranasal challenge with MPXV strain Liberia (A) and macroscopic lesions at the site of subcutaneous inoculation with MPXV strain Zr-599 (B). The identification numbers of monkeys are given. Analyses by H&E staining (A, low and high magnifications) revealed that the lesions of naïve monkey 4595 were characterized by destruction of mucous membrane structures, disappearance of mucosal epithelial cells resulting in ulcer formation, necrosis, and hyperplasia. MPXV antigens were present in the lesions. In contrast, the mucous membranes of the nasal cavity into which MPXV was inoculated in Lister-immunized monkey 4597 were normal, and MPXV antigens were not detected. Although the mucous membranes of the LC16m8-immunized monkey 4600 showed infiltration of inflammatory cells, the structure was maintained without necrosis. Furthermore, MPXV antigens were not detected. (B) Erythematous, vesicular, and ulcerative lesions appeared in the SC-Naïve group. The maximum diameter of the lesions exceeded 10 cm on day 14 postchallenge. In the SC-LC16m8 group, similar but milder lesions were observed, while no obvious lesions were detected at the site of inoculation in the SC-Lister group.
Protection of monkeys against lethal subcutaneous MPXV challenge by immunization with LC16m8.
The efficacy of LC16m8 in the lethal MPXV infection model was then evaluated (Table 1, experiment 2). Subcutaneous infection with MPXV Zr-599 was fatal to nonimmunized monkeys in the SC-Naïve group (Table 1). Body weight was decreased by approximately 15% after challenge in the SC-Naïve group. However, the monkeys in the SC-Lister and SC-LC16m8 groups maintained their body weight (Fig. 2). Papulovesicular skin lesions appeared on day 7 after challenge in the SC-Naïve group; monkeys 4651 and 4653 showed 390 and 1,150 lesions, respectively. The symptoms of both of the monkeys in the SC-Naïve group were so severe that they were euthanized for ethical reasons. On the other hand, the monkeys in the SC-LC16m8 group did not develop any MPX-associated symptoms, except for local cutaneous lesions at the site of MPXV inoculation (Fig. 4). The lesions consisted of erythema, vesicles, and ulceration and were much milder than those for the SC-Naïve group. The SC-Lister group showed no MPX-associated symptoms, not even cutaneous lesions at the site of MPXV inoculation (Fig. 4).
Histopathological examination.
All the monkeys were sacrificed for virological and histopathological examination 3 weeks after MPXV challenge. After intranasal inoculation, nodular and granulomatous lesions were detected in the lungs in the IN-Naïve group, while no lesions were detected in the lungs of any of the monkeys in the IN-Lister and IN-LC16m8 groups (Fig. 3A). IHC examination with an anti-vaccinia virus antibody revealed the presence of MPXV in the nodular lesions (Fig. 3A). Similar nodular lesions caused by MPXV were also detected in the pancreas of monkey 4595 in the IN-Naïve group (Fig. 3A). Macroscopic and histological examination revealed that the thymus, tonsil, and lymph node structures were affected by MPXV in the IN-Naïve monkeys. In contrast, no MPX-associated lesions were detected in any of the monkeys in the IN-Lister and IN-LC16m8 groups by histopathological examination.
After subcutaneous inoculation with MPXV, MPX-associated lesions were detected in the lymphoid systems (lymph nodes, thymus, and tonsils), respiratory tract structures (lung and trachea), digestive organs (stomach, small intestine, colon, rectum, and liver), urogenital tract (bladder, uterus, and ovary), or skin in the SC-Naïve group (Fig. 3B and 4B). On the other hand, no MPX-associated lesions were detected in any internal organs of any of the monkeys in the SC-Lister and SC-LC16m8 groups, except for skin lesions at the site of MPXV inoculation in the SC-LC16m8 group (Fig. 4B).
Laboratory findings and cytokine responses.
C-reactive protein (CRP) levels were measured as an indicator of inflammation. CRP levels were significantly increased in groups IN-Naïve and SC-Naïve but not in any of the animals immunized with either vaccine (data not shown). Furthermore, lymphocytopenia and thrombocytopenia were also detected in mock-immunized naïve monkeys but were not apparent in any of the animals immunized with either vaccine (data not shown). The levels of IFN-γ, TNF-α, IL-2, IL-4, IL-6, and IL-10 in plasma were examined. IFN-γ and IL-6 levels increased after MPXV challenge in groups IN-Naïve and SC-Naïve (Fig. 2). The levels of IFN-γ and IL-6 were higher in group SC-Naïve than in group IN-Naïve. The monkeys immunized with Lister or LC16m8 showed very low level or no detectable cytokine responses (Fig. 2).
Viremia determined by virus isolation and qPCR.
Virus isolation results are summarized in Table 1. MPXV was isolated from purified PBMCs from group IN-Naïve between days 4 and 13 after challenge but not from PBMCs collected from any of the monkeys in groups IN-Lister and IN-LC16m8. MPXV was also isolated from the buffy coat fractions obtained from 4 ml of peripheral blood collected between days 3 and 14 from monkey 4651 and between days 3 and 18 from monkey 4653 in the SC-Naïve group. MPXV was isolated from the buffy coat fractions of two of the three SC-LC16m8 monkeys, but the plaque number was small and the isolation period was short. MPXV was not isolated from any of the monkeys in the SC-Lister group.
The levels of viremia were assessed by qPCR with LightCycler using in-house primer sets and fluorescent probes. In the intranasal-inoculation model, viremia was demonstrated for group IN-Naïve but not for group IN-Lister or IN-LC16m8 (Fig. 2). In the subcutaneous-inoculation model, viremia was demonstrated for all monkeys in groups SC-Naïve and SC-LC16m8 and for one of the two monkeys in group SC-Lister. The levels and durations of viremia were highest and longest in group SC-Naïve, followed by group SC-LC16m8. These results were consistent with those of virus isolation experiments (Table 1 and Fig. 2).
IgG and neutralizing antibody responses.
VV antigen-specific IgG became detectable by IgG-ELISA in monkeys immunized with Lister or LC16m8 within 2 weeks postimmunization (Fig. 5). The time courses and levels of IgG response determined by ELISA were similar for monkeys immunized with LC16m8 and those immunized with Lister (Fig. 5). IgG reactive to VV antigens became detectable by IgG-ELISA in the IN-Naïve and SC-Naïve groups within 2 weeks after MPXV challenge. The levels of neutralizing antibody to MPXV were tested before and after challenge with MPXV. At the time of challenge with MPXV, neutralizing antibody was detected in the monkeys immunized with LC16m8 or Lister. The titers were not increased after the challenge. Neutralizing antibody was demonstrated in both of the animals in the IN-Naïve group and in one of the two animals in the SC-Naïve group.
FIG. 5.
Vaccinia virus-specific IgG responses determined by IgG ELISA (A) and a neutralizing assay (B) for MPXV. The optical densities at 405 nm (OD405) at serum sample dilutions of 1:100 are shown. (A) Development of specific IgG antibody responses to vaccinia virus antigens in plasma samples collected on different days after vaccination and/or challenge, as measured by IgG ELISA. The day of MPXV challenge was taken as day zero. (B) MPXV-specific neutralizing antibody titers (NT) in plasma samples were determined by plaque reduction assay on different days after vaccination and/or challenge. The neutralizing antibody titers were determined for plasma collected from mice in the SC-Naïve group at the times of MPXV challenge and sacrifice and for plasma collected from mice in the SC-Lister and SC-LC16m8 groups at the times of immunization with Lister or LC16m8, challenge with MPXV, and sacrifice. The day of MPXV challenge was defined as day zero.
DISCUSSION
The protective efficacy of LC16m8 was evaluated in a mild-MPX nonhuman-primate model, in which monkeys were intranasally inoculated with MPXV strain Liberia, and in a lethal-MPX nonhuman-primate model, in which monkeys were subcutaneously inoculated with MPXV strain Zr-599. Monkeys subcutaneously inoculated with MPXV strain Liberia developed relatively milder symptoms of MPX than those subcutaneously inoculated with MPXV strain Zr-599. Monkeys intranasally inoculated with MPXV strain Liberia also developed relatively milder symptoms than those intranasally inoculated with MPXV strain Zr-599. These data suggest that MPXV strain Liberia, one of the West African strains, is less virulent than MPXV Zr-599, one of the Congo Basin strains (unpublished data).
A single vaccination with LC16m8 protected monkeys from MPX, as did a single vaccination with Lister. The results of the present study indicate that LC16m8 confers sufficient protection against MPX in monkeys, even in the lethal-MPX nonhuman-primate model. LC16m8 completely protected nonhuman primates from MPX in the intranasal-inoculation model. The protective efficacy of LC16m8 was confirmed not only with regard to clinical symptoms but also by virological assays, such as determination of the lymphocyte and thrombocyte counts, CRP level, and interleukin levels, viremia level determination by qPCR, virus isolation, and histopathological examinations. Differences between LC16m8 and Lister were observed only with respect to the viremia level and the cutaneous lesions at the site of virus inoculation after subcutaneous MPXV inoculation.
LC16m8 was reported to cause few adverse events when tested in a preliminary trial in which about 30,000 children were immunized in Japan in the 1970s (11). No serious complications were reported. Fever was observed in fewer cases than for Lister- or CV1-78-immunized individuals (11). The results of the present study strongly suggest that LC16m8 is as efficacious as Lister in protecting humans from smallpox or MPX and support the suggestion that LC16m8 may be useful as a replacement for currently available VVs, such as Lister and Dryvax. Especially, the risk of VV-related casualties must be minimized and avoided if VVs are used today, when there are no variola outbreaks. LC16m8 can also be used for the treatment of people in regions in which human MPX is endemic.
It has been reported that some of the characteristics of LC16m8, such as small-pock formation in chicken chorioallantoic membrane and a narrow host range for replication, are due to a mutation in the membrane protein B5R (35). A single-nucleotide deletion in the B5R gene results in a deficiency in expression of full-length and intact B5R membrane protein (24, 35). There was a single-base deletion of G at the 274th position from the initiation codon, resulting in expression of a truncated B5R membrane protein. Although some poxvirus researchers have shown interest in the protective efficacy of LC16m8 (5), LC16m8 was shown to induce protective immunity to MPX in nonhuman primates in the present study. It was reported that the membrane protein B5R is not essential for protection against vaccinia virus infection in mice (19). Lister showed a stronger preventive effect against the local reactions at the site of MPXV inoculation in monkeys and resulted in lower levels of MPXV viremia than LC16m8. These observations suggest a role for the membrane protein B5R in induction of immunity to MPXV in nonhuman primates; however, the presence of the membrane protein B5R is not essential. Although the results of the present study cannot exclude the importance of the membrane protein B5R, LC16m8 induces sufficient protective immunity to MPX and probably induces protective immunity against variola.
Humans are usually infected with MPXV through the skin surface by bites from infected animals (9), while infection with variola occurs through the respiratory tract (7). In the present study, the monkeys were infected with MPXV by either the intranasal or the subcutaneous route in order to design an appropriate nonhuman-primate model not only for MPX but also for variola. The symptoms associated with MPX in naïve monkeys challenged intranasally with MPXV were somewhat milder than those reported in previous studies (15, 37, 39). This may have been due to the differences in MPXV strains, infection routes, or virus doses used for challenge. Subcutaneous infection of naïve monkeys with MPXV was fatal, but a single vaccination with LC16m8 prevented fatal infection. It must be emphasized that LC16m8 sufficiently protects monkeys even from lethal MPX.
In summary, a single vaccination with LC16m8 induced protective immunity against MPX, as did immunization with Lister, in nonhuman primates. These results strongly suggest that LC16m8 is also effective in the induction of high levels of protective immunity against variola.
Acknowledgments
All animal procedures were approved by the Committees on Biosafety and Animal Handling and Ethical Regulations of the National Institute of Infectious Diseases, Japan. We thank A. Harashima, Department of Pathology, National Institute of Infectious Diseases, for technical assistance.
This study was supported financially by a grant-in-aid from the Ministry of Health, Labor, and Welfare of Japan.
REFERENCES
- 1.Cassimatis, D. C., J. E. Atwood, R. M. Engler, P. E. Linz, J. D. Grabenstein, and M. N. Vernalis. 2004. Smallpox vaccination and myopericarditis: a clinical review. J. Am. Coll. Cardiol. 43:1503-1510. [DOI] [PubMed] [Google Scholar]
- 2.CDC. 2004. Update: adverse events following civilian smallpox vaccination—United States, 2003. Morb. Mortal. Wkly. Rep. 53:106-107. [PubMed] [Google Scholar]
- 3.Chen, N., G. Li, M. K. Liszewski, J. P. Atkinson, P. B. Jahrling, Z. Feng, J. Schriewer, C. Buck, C. Wang, E. J. Lefkowitz, J. J. Esposito, T. Harms, I. K. Damon, R. L. Roper, C. Upton, and R. M. Buller. 2005. Virulence differences between monkeypox virus isolates from West Africa and the Congo basin. Virology 340:46-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen, R. T., and J. M. Lane. 2003. Myocarditis: the unexpected return of smallpox vaccine adverse events. Lancet 362:1345-1346. [DOI] [PubMed] [Google Scholar]
- 5.Cohen, J. 2002. Public health. Looking for vaccines that pack a wallop without the side effects. Science 298:2314. [DOI] [PubMed] [Google Scholar]
- 6.Di Giulio, D. B., and P. B. Eckburg. 2004. Human monkeypox: an emerging zoonosis. Lancet Infect. Dis. 4:15-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esposito, J. J., and F. Fenner. 2001. Poxviruses, p. 2887-2921. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 4th ed., vol. 2. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 8.Galmiche, M. C., J. Goenaga, R. Wittek, and L. Rindisbacher. 1999. Neutralizing and protective antibodies directed against vaccinia virus envelope antigens. Virology 254:71-80. [DOI] [PubMed] [Google Scholar]
- 9.Guarner, J., B. J. Johnson, C. D. Paddock, W. J. Shieh, C. S. Goldsmith, M. G. Reynolds, I. K. Damon, R. L. Regnery, and S. R. Zaki. 2004. Monkeypox transmission and pathogenesis in prairie dogs. Emerg. Infect. Dis. 10:426-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Halsell, J. S., J. R. Riddle, J. E. Atwood, P. Gardner, R. Shope, G. A. Poland, G. C. Gray, S. Ostroff, R. E. Eckart, D. R. Hospenthal, R. L. Gibson, J. D. Grabenstein, M. K. Arness, and D. N. Tornberg. 2003. Myopericarditis following smallpox vaccination among vaccinia-naïve US military personnel. JAMA 289:3283-3289. [DOI] [PubMed] [Google Scholar]
- 11.Hashizume, S., H. Yoshizawa, M. Morita, and K. Suzuki. 1985. Properties of attenuated mutant of vaccinia virus, LC16m8, derived from Lister strain, p. 88-99. In G. V. Quinnan (ed.), Vaccinia viruses as vectors for vaccine antigens. Elsevier, Amsterdam, The Netherlands.
- 12.Hatakeyama, S., K. Moriya, M. Saijo, Y. Morisawa, I. Kurane, K. Koike, S. Kimura, and S. Morikawa. 2005. Persisting humoral antiviral immunity within the Japanese population after the discontinuation in 1976 of routine smallpox vaccinations. Clin. Diagn. Lab. Immunol. 12:520-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hollinshead, M., G. Rodger, H. Van Eijl, M. Law, R. Hollinshead, D. J. Vaux, and G. L. Smith. 2001. Vaccinia virus utilizes microtubules for movement to the cell surface. J. Cell Biol. 154:389-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hooper, J. W., D. M. Custer, and E. Thompson. 2003. Four-gene-combination DNA vaccine protects mice against a lethal vaccinia virus challenge and elicits appropriate antibody responses in nonhuman primates. Virology 306:181-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hooper, J. W., E. Thompson, C. Wilhelmsen, M. Zimmerman, M. A. Ichou, S. E. Steffen, C. S. Schmaljohn, A. L. Schmaljohn, and P. B. Jahrling. 2004. Smallpox DNA vaccine protects nonhuman primates against lethal monkeypox. J. Virol. 78:4433-4443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu, G., M. J. Wang, M. J. Miller, G. N. Holland, D. A. Bruckner, R. Civen, L. A. Bornstein, L. Mascola, M. A. Lovett, B. J. Mondino, and D. A. Pegues. 2004. Ocular vaccinia following exposure to a smallpox vaccinee. Am. J. Ophthalmol. 137:554-556. [DOI] [PubMed] [Google Scholar]
- 17.Katz, E., B. M. Ward, A. S. Weisberg, and B. Moss. 2003. Mutations in the vaccinia virus A33R and B5R envelope proteins that enhance release of extracellular virions and eliminate formation of actin-containing microvilli without preventing tyrosine phosphorylation of the A36R protein. J. Virol. 77:12266-12275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khodakevich, L., Z. Jezek, and D. Messinger. 1988. Monkeypox virus: ecology and public health significance. Bull. W. H. O. 66:747-752. [PMC free article] [PubMed] [Google Scholar]
- 19.Kidokoro, M., M. Tashiro, and H. Shida. 2005. Genetically stable and fully effective smallpox vaccine strain constructed from highly attenuated vaccinia LC16m8. Proc. Natl. Acad. Sci. USA 102:4152-4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kimura, M., and H. Sakai. 1996. Complications of smallpox vaccination. Clin. Virol. 24:30-39. [Google Scholar]
- 21.Kitamura, T. 1999. Smallpox eradication and future prospect of smallpox vaccine. Clin. Virol. 27:378-384. [Google Scholar]
- 22.Lane, J. M., and J. Goldstein. 2003. Adverse events occurring after smallpox vaccination. Semin. Pediatr. Infect. Dis. 14:189-195. [DOI] [PubMed] [Google Scholar]
- 23.Miller, J. R., N. M. Cirino, and E. F. Philbin. 2003. Generalized vaccinia 2 days after smallpox revaccination. Emerg. Infect. Dis. 9:1649-1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morikawa, S., T. Sakiyama, H. Hasegawa, M. Saijo, A. Maeda, I. Kurane, G. Maeno, J. Kimura, C. Hirama, T. Yoshida, Y. Asahi-Ozaki, T. Sata, T. Kurata, and A. Kojima. 2005. An attenuated LC16m8 smallpox vaccine: analysis of full-genome sequence and induction of immune protection. J. Virol. 79:11873-11891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murphy, J. G., R. S. Wright, G. K. Bruce, L. M. Baddour, M. A. Farrell, W. D. Edwards, H. Kita, and L. T. Cooper. 2003. Eosinophilic-lymphocytic myocarditis after smallpox vaccination. Lancet 362:1378-1380. [DOI] [PubMed] [Google Scholar]
- 26.Nagata, N., T. Iwasaki, Y. Ami, A. Harashima, I. Hatano, Y. Suzaki, K. Yoshii, T. Yoshii, A. Nomoto, and T. Kurata. 2001. Comparison of neuropathogenicity of poliovirus type 3 in transgenic mice bearing the poliovirus receptor gene and cynomolgus monkeys. Vaccine 19:3201-3208. [DOI] [PubMed] [Google Scholar]
- 27.Nagata, N., H. Shimizu, Y. Ami, Y. Tano, A. Harashima, Y. Suzaki, Y. Sato, T. Miyamura, T. Sata, and T. Iwasaki. 2002. Pyramidal and extrapyramidal involvement in experimental infection of cynomolgus monkeys with enterovirus 71. J. Med. Virol. 67:207-216. [DOI] [PubMed] [Google Scholar]
- 28.Neubauer, H., U. Reischl, S. Ropp, J. J. Esposito, H. Wolf, and H. Meyer. 1998. Specific detection of monkeypox virus by polymerase chain reaction. J. Virol. Methods 74:201-207. [DOI] [PubMed] [Google Scholar]
- 29.Newsome, T. P., N. Scaplehorn, and M. Way. 2004. SRC mediates a switch from microtubule- to actin-based motility of vaccinia virus. Science 306:124-129. [DOI] [PubMed] [Google Scholar]
- 30.Reed, K. D., J. W. Melski, M. B. Graham, R. L. Regnery, M. J. Sotir, M. V. Wegner, J. J. Kazmierczak, E. J. Stratman, Y. Li, J. A. Fairley, G. R. Swain, V. A. Olson, E. K. Sargent, S. C. Kehl, M. A. Frace, R. Kline, S. L. Foldy, J. P. Davis, and I. K. Damon. 2004. The detection of monkeypox in humans in the Western Hemisphere. N. Engl. J. Med. 350:342-350. [DOI] [PubMed] [Google Scholar]
- 31.Saurina, G., S. Shirazi, J. M. Lane, B. Daniel, and L. DiEugenia. 2003. Myocarditis after smallpox vaccination: a case report. Clin. Infect. Dis. 37:145-146. [DOI] [PubMed] [Google Scholar]
- 32.Schmelz, M., B. Sodeik, M. Ericsson, E. J. Wolffe, H. Shida, G. Hiller, and G. Griffiths. 1994. Assembly of vaccinia virus: the second wrapping cisterna is derived from the trans Golgi network. J. Virol. 68:130-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Semba, R. D. 2003. The ocular complications of smallpox and smallpox immunization. Arch. Ophthalmol. 121:715-719. [DOI] [PubMed] [Google Scholar]
- 34.Smith, G. L., A. Vanderplasschen, and M. Law. 2002. The formation and function of extracellular enveloped vaccinia virus. J. Gen. Virol. 83:2915-2931. [DOI] [PubMed] [Google Scholar]
- 35.Takahashi-Nishimaki, F., S. Funahashi, K. Miki, S. Hashizume, and M. Sugimoto. 1991. Regulation of plaque size and host range by a vaccinia virus gene related to complement system proteins. Virology 181:158-164. [DOI] [PubMed] [Google Scholar]
- 36.Takahashi-Nishimaki, F., K. Suzuki, M. Morita, T. Maruyama, K. Miki, S. Hashizume, and M. Sugimoto. 1987. Genetic analysis of vaccinia virus Lister strain and its attenuated mutant LC16m8: production of intermediate variants by homologous recombination. J. Gen. Virol. 68:2705-2710. [DOI] [PubMed] [Google Scholar]
- 37.Weltzin, R., J. Liu, K. V. Pugachev, G. A. Myers, B. Coughlin, P. S. Blum, R. Nichols, C. Johnson, J. Cruz, J. S. Kennedy, F. A. Ennis, and T. P. Monath. 2003. Clonal vaccinia virus grown in cell culture as a new smallpox vaccine. Nat. Med. 9:1125-1130. [DOI] [PubMed] [Google Scholar]
- 38.Whitman, T. J., M. A. Ferguson, and C. F. Decker. 2003. Cardiac dysrhythmia following smallpox vaccination. Clin. Infect. Dis. 37:1579-1580. [DOI] [PubMed] [Google Scholar]
- 39.Zaucha, G. M., P. B. Jahrling, T. W. Geisbert, J. R. Swearengen, and L. Hensley. 2001. The pathology of experimental aerosolized monkeypox virus infection in cynomolgus monkeys (Macaca fascicularis). Lab. Investig. 81:1581-1600. [DOI] [PMC free article] [PubMed] [Google Scholar]