Abstract
Antigen stimulation of mast cells via FcɛRI, the high-affinity receptor for IgE, triggers a signaling cascade that requires Ca2+ mobilization for exocytosis of secretory granules during an allergic response. This study investigates critical signaling components by using mutant RBL mast cells that are defective in antigen-stimulated phospholipase Cγ (PLCγ) activation, as well as other signaling activities downstream of stimulated tyrosine phosphorylation. We show that the expression of activated versions of the Cdc42 or Rac1 GTPase restores antigen-stimulated Ca2+ mobilization necessary for degranulation in these mutant cells. Wild-type Cdc42 and Rac1, as well as activated Cdc42 containing effector domain mutations, all fail to restore antigen-stimulated signaling leading to exocytosis. Expression of oncogenic Dbl, a guanine nucleotide exchange factor for Cdc42 and Rac1, partially restores sustained Ca2+ mobilization and degranulation, suggesting that activation of endogenous Cdc42 and/or Rac1 is impaired in the mutant cells. Overexpression of PLCγ1 with either activated Cdc42 or Rac1 synergistically stimulates degranulation, consistent with a critical defect in PLCγ activation in these cells. Thus, our results point to activation of Cdc42 and/or Rac1 playing an essential role in antigen stimulation of early events that culminate in mast cell degranulation.
Mast cells and basophils generate many of the symptoms that accompany an allergic reaction by releasing secretory granule contents, including histamine and serotonin, in response to antigen-mediated crosslinking of IgE antibody bound to FcɛRI, the high-affinity IgE receptor at the cell surface. Receptor aggregation initiates a signaling cascade involving the recruitment and activation of several tyrosine kinases and other signaling proteins that function to stimulate degranulation (1, 2). A pivotal step in this signaling cascade is the activation of phospholipase Cγ1 (PLCγ1) and 2 (PLCγ2), which catalyze the cleavage of the lipid substrate phosphatidylinositol-4,5-bisphosphate into two important signaling intermediates in this pathway, diacylglycerol, a stimulator of protein kinase C, and inositol 1,4,5-trisphosphate (IP3), a ligand for the IP3 receptor Ca2+ channel in the endoplasmic reticulum (ER) membrane that induces a rise in cytoplasmic Ca2+ levels (3).
We have recently suggested that the Rho GTPases, Cdc42 and Rac1, may regulate the IP3/Ca2+ signaling cascade in the RBL-2H3 mast cell line (4). Members of the Rho family of GTPases undergo activation by GTP/GDP exchange and have been linked to the control of many critical cellular functions, including cytoskeletal rearrangement, transcriptional activation, and cell cycle progression (5). We found that RBL-2H3 cells expressing activated Cdc42 and Rac1 displayed elevated levels of antigen-stimulated IP3 formation, Ca2+ mobilization, and degranulation, whereas dominant-negative mutants partially inhibited these processes.
To more critically examine whether activation of Cdc42 and/or Rac1 is required for FcɛRI signaling leading to Ca2+ mobilization and degranulation, we used a mutant RBL cell line B6A4C1 that is defective in these processes. These cells were originally isolated after chemical mutagenesis of RBL-2H3 cells, displaying defects in antigen-stimulated degranulation and cell surface expression of a mast cell-specific ganglioside (6, 7). B6A4C1 cells were subsequently found to exhibit normal antigen-stimulated tyrosine phosphorylation of signaling proteins, but were defective in phospholipase activation and calcium mobilization (8). Antigen-stimulated degranulation is minimal in these mutant cells, but bypassing the IgE receptor with a Ca2+ ionophore results in a full degranulation response. Because these results indicated that some aspect of the IP3/Ca2+ signaling pathway is impaired in the mutant cell line, we investigated whether expression of activated Cdc42 and/or Rac1 could rescue the mutant phenotypes. We show here that either activated Cdc42 or Rac1 restores antigen-stimulated Ca2+ mobilization and degranulation to wild-type levels in the B6A4C1 cell line. Furthermore, coexpression of activated Cdc42/Rac1 and PLCγ1 synergistically stimulates degranulation, indicating that these Rho family proteins play an important role in an early FcɛRI-coupled signaling event.
Materials and Methods
Cell Culture and Reagents.
RBL-2H3 and B6A4C1 cells were maintained in monolayer culture in modified Eagle's medium (MEM) supplemented with 20% FBS/2% l-glutamine/50 μg/ml gentamicin sulfate at 37°C in a 5% CO2 incubator. Experiments were typically performed 3–4 days after passage.
Vaccinia Virus Construction and Infection.
Construction of wild-type, dominant-active, and dominant-negative forms of myc-tagged Cdc42 and Rac1 in vaccinia virus have been described (4). The viruses encoding oncogenic Dbl (o-Dbl), PLCγ1, and the effector domain mutants Cdc42V12,F37 and Cdc42V12,Y40 were constructed in a similar manner. The o-Dbl construct was hemagglutinin-tagged at the N terminus and includes residues 498–925 of the full-length proto-Dbl. The PLCγ1 construct was kindly provided by S. G. Rhee (National Institutes of Health, Bethesda) and subsequently modified with a N-terminal hemagglutinin tag. Both of the effector domain mutants of Cdc42 were myc-tagged at the N terminus. Viruses that exhibited a high level of expression as determined by Western blot were amplified in HeLa cells and stored in small aliquots at −80°C. Titers of amplified viral stocks generally ranged from 106-107 pfu/μl.
Before infection, viruses taken from −80°C were sonicated briefly, incubated with an equal volume of 0.25 mg/ml trypsin for 30 min at 37°C, and resonicated to disrupt viral aggregates. Cells were infected with the indicated pfu per cell in MEM supplemented with 5% FBS/2% glutamine/50 μg/ml gentamicin sulfate/1 μg/ml anti-2,4-dinitrophenyl IgE for 6 h.
Degranulation Assays.
RBL cells were plated in 48-well plates at a density of 2.5 × 105 cells per well overnight at 37°C and infected the following day. Infected cells were washed twice in Tyrode's buffer [135 mM NaCl/5 mM KCl/1.8 mM CaCl2/1 mM MgCl2/5.6 mM glucose/1 mg/ml BSA/20 mM Hepes (pH 7.4)] and stimulated with 100 ng/ml multivalent dinitrophenyl-BSA (DNP/BSA) for 1 h at 37°C. β-Hexosaminidase release was measured as described (4).
Ca2+ Measurements.
RBL cells were plated in 100-mm plates at a density of 4 × 106 cells per plate overnight at 37°C and infected the following day. Infected cells were harvested, washed twice, and resuspended in Tyrode's buffer supplemented with 0.25 mM sulfinpyrazone at 1 × 106 cells/ml, and then loaded with 0.5 μM indo-1/acetoxymethyl ester (Calbiochem) for 1 h with constant agitation at 37°C. Cells were then washed twice and resuspended in Tyrode's buffer and 0.25 mM sulfinpyrazone at 1 × 106 cells/ml. Aliquots (3 ml) of cell suspension were added to acrylic cuvettes maintained at 37°C and constantly stirred during the course of the experiment. DNP/BSA was added at 100 ng/ml to initiate Ca2+ signaling. For experiments that specifically evaluate release of Ca2+ from ER stores, 4 mM EDTA was added to cells before DNP/BSA stimulation. Indo-1 was excited at 330 nm and fluorescence emission was monitored at 400 nm with a Perkin–Elmer LS-5 fluorescence spectrophotometer.
Cell Lysis and Western Blotting.
RBL cells infected for 6 h with virus expressing PLCγ1 or o-Dbl, or uninfected cells, were washed with PBS and lysed in buffer A [40 mM Hepes (pH 7.4)/1% Triton X-100/1 mM EDTA/150 mM NaCl/50 mM NaF/1 mM sodium orthovanadate/10 μg/ml leupeptin/10 μg/ml aprotinin/1 mM PMSF) for 30 min rocking at 4°C. Lysates were precleared by centrifugation at 12,000 × g for 5 min and denatured by boiling for 3 min in SDS sample buffer. Whole-cell lysates were resolved by SDS/PAGE and transferred to nitrocellulose membranes. For Western blot detection, rabbit anti-PLCγ1 and rabbit anti-Dbl (both from Santa Cruz Biotechnology) were used at a 1:1000 dilution. Blots were developed by using donkey anti-rabbit coupled to horseradish peroxidase at a dilution of 1:10,000 and the enhanced chemiluminescence detection system (Amersham International).
Results
Activated Cdc42 and Rac1 Restore Degranulation to Wild-Type Levels in B6A4C1 Cells.
The dominant-active Cdc42V12 and Rac1V12 mutants have been extensively used as a means of sustaining continual stimulation of effector targets to probe Rho GTPase function. Cdc42V12 and Rac1V12 maintain their activated state by being unable to hydrolyze bound GTP. By using a vaccinia virus expression system, we introduced these mutants into B6A4C1 cells to determine whether activated Cdc42 and Rac1 can reconstitute antigen-stimulated degranulation to the levels observed in parental RBL-2H3 cells.
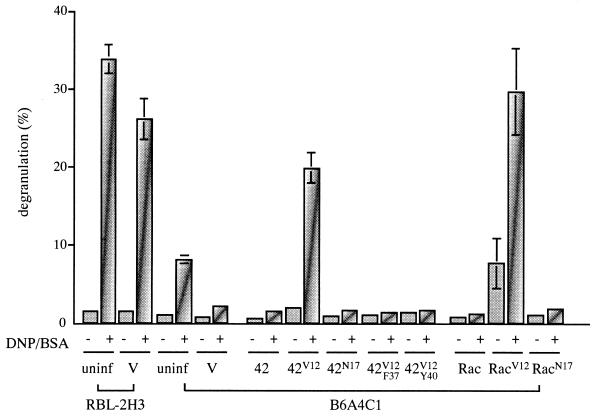
The B6A4C1 cell line exhibits a marked decrease in antigen-stimulated degranulation compared with RBL-2H3 cells (Fig. 1). Infection with an empty vaccinia virus vector control reduced stimulated degranulation in both cell lines, such that it became indistinguishable from spontaneous release in B6A4C1 cells. As summarized in Fig. 1 for multiple experiments, infection of B6A4C1 cells with the dominant-active mutants, Cdc42V12 and Rac1V12, significantly enhanced antigen-stimulated degranulation by ≈10-fold and 15-fold, respectively, compared with stimulated mutant cells infected with empty vector, thereby restoring stimulated degranulation to ≈80% and 120%, respectively, of the levels obtained with RBL-2H3 cells infected with empty vector. In contrast, expression of wild-type Cdc42 and Rac1 or dominant-negative Cdc42N17 and Rac1N17 did not cause any significant change in antigen-stimulated degranulation. Consistent with this, B6A4C1 cells expressed endogenous Cdc42 and Rac1 as in RBL-2H3 cells (data not shown). Unstimulated B6A4C1 cells expressing Rac1V12 exhibited a small amount of degranulation during the secretion assay, suggesting that activated Rac1 can partially bypass the need for antigen stimulation of degranulation in these cells. Total β-hexoaminidase content was not significantly altered in cells infected with any of the constructs used, indicating that degranulation did not detectably occur during the initial vaccinia infection period. The different mutants of Cdc42 or Rac1 were expressed at comparable protein levels in B6A4C1 cells (data not shown), as seen in RBL-2H3 cells (4).
Figure 1.
Dominant-active Cdc42 and Rac1 rescue degranulation in B6A4C1 cells. β-Hexosaminidase release was measured in RBL-2H3 and B6A4C1 cells infected with 20 pfu/cell of vector or left uninfected and in B6A4C1 cells infected with different forms of Cdc42 and Rac1, on stimulation with 100 ng/ml DNP/BSA or left unstimulated. Degranulation is given as the percent of total cellular β-hexosaminidase released, as measured by treatment of cells in parallel with 0.5% Triton X-100. Error bars represent the standard deviation of at least three independent experiments.
To examine the requirement for Rho GTPase binding to downstream effector targets in restoring degranulation in B6A4C1 cells, we introduced two point mutations, F37A and Y40C, separately, into the Switch I effector-binding domain (residues 32–40) of Cdc42V12. The F37A mutation blocks Cdc42-dependent activation of Rac1-induced membrane ruffles, whereas the Y40C mutation prevents interaction with targets containing the CRIB domain such as PAK or WASP (9). Expression of Cdc42V12,Y40 or Cdc42V12,F37 completely eliminated the enhanced level of secretion observed on infection with Cdc42V12 (Fig. 1), indicating that downstream targets necessary for activating degranulation must bind to the Switch I region of Cdc42/Rac1.
Reconstitution of Ca2+ Mobilization by Cdc42V12 and Rac1V12 in B6A4C1 Cells.
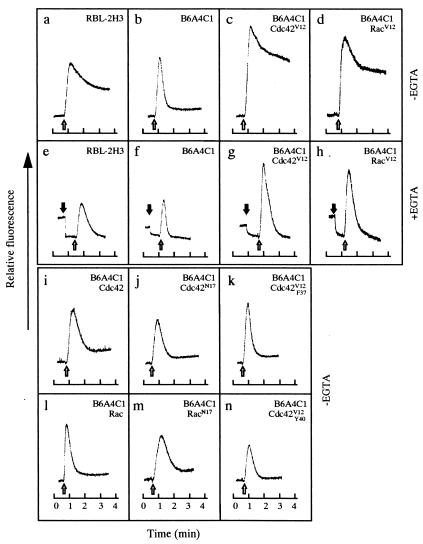
We next investigated whether sustained Ca2+ mobilization could be restored in B6A4C1 on antigen stimulation, because the signaling defect in these mutant cells was previously determined to be upstream of IP3 production (8). Ca2+ mobilization is initiated by IP3-dependent opening of IP3 receptor Ca2+ channels in the ER membrane (10, 11). The resultant depletion of Ca2+ from ER stores, in turn, activates the influx of extracellular Ca2+ necessary for sustained intracellular Ca2+ elevation (12). Antigen-stimulated changes in cytoplasmic Ca2+ were monitored by using indo-1 fluorescence (Fig. 2). On antigen stimulation (Fig. 2b, ➩), B6A4C1 cells infected with empty vector exhibited a transient increase in cytoplasmic Ca2+ contributed primarily by the release of Ca2+ from ER stores. These cells did not maintain the more sustained increase in cytoplasmic Ca2+ derived primarily from influx, which is normally observed in wild-type 2H3 cells (Fig. 2a) (13). Expression of either Cdc42V12 or Rac1V12 in B6A4C1 cells significantly enhanced both the initial and sustained phases of antigen-stimulated Ca2+ signaling (Fig. 2 c and d). To determine whether these GTPases play a role in stimulating the release of Ca2+ from ER stores, indo-1 experiments were performed in the presence of EGTA to chelate extracellular Ca2+. On EGTA addition (Fig. 2 e–h, ➞), indo-1 fluorescence decreased to a lower baseline level, caused in part to the release of Ca2+ from small amounts of extracellular indo-1. Subsequent antigen stimulation of B6A4C1 cells expressing Cdc42V12 or Rac1V12 (Fig. 2 g and h, ➩) triggered an enhanced transient release of Ca2+ from ER stores compared with cells infected with empty vector (Fig. 2f). This indicates that both Cdc42 and Rac1 can act upstream of stimulated Ca2+ release from ER stores in restoring functional Ca2+ mobilization in the mutant B6A4C1 cells. In contrast, mutant cells expressing wild-type Cdc42/Rac1 (Fig. 2 i and l), dominant-negative Cdc42N17/Rac1N17 (Fig. 2 j and m), and the two effector domain mutants, Cdc42V12,F37 and Cdc42V12,Y40 (Fig. 2 k and n), failed to restore sustained Ca2+ signaling, consistent with the degranulation results. Taken together, these results suggest that the mutant cell line is unable to produce sufficient amounts of antigen-stimulated IP3 to sustain the elevated levels of cytoplasmic Ca2+ required to stimulate degranulation. By restoring this capacity in the mutant cell line, Cdc42V12 and Rac1V12 can effectively reconstitute antigen-stimulated Ca2+ mobilization and degranulation.
Figure 2.
Dominant-active Cdc42 and Rac1 restore total Ca2+ mobilization and release of Ca2+ from ER stores in B6A4C1 cells. RBL-2H3 cells were infected with 20 pfu/cell of vector (a and e) and B6A4C1 cells were infected with 20 pfu/cell of vector (b and f); Cdc42V12 (c and g); Rac1V12 (d and h); Cdc42 (i); Cdc42N17 (j); Cdc42V12,F37 (k); Rac1 (l); Rac1N17 (m); and Cdc42V12,Y40 (n) for 6 h at 37°C and loaded with indo-1. Overall Ca2+ responses were monitored by indo-1 fluorescence in response to stimulation with 100 ng/ml DNP/BSA (➩). To specifically measure the release of Ca2+ from ER stores (e–h), loaded cells were treated with 4 mM EDTA (➞) and then stimulated with 100 ng/ml DNP/BSA. For 2H3 cells infected with vector and for B6A4C1 cells infected with vector, Cdc42V12 or Rac1V12 (a–h), measurements of the Ca2+ responses in the absence and presence of EGTA were performed concurrently. Traces shown are representative of at least three independent experiments.
o-Dbl Partially Rescues Antigen-Stimulated Degranulation and Ca2+ Signaling in B6A4C1 Cells.
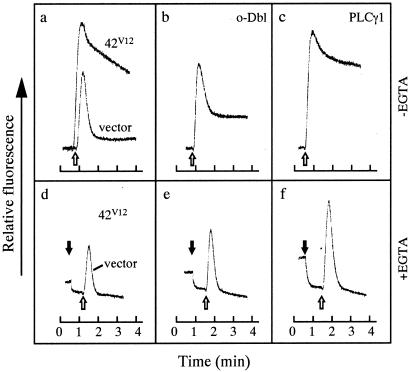
To examine whether the activation of either Cdc42 or Rac1 is defective in the mutant cell line, we constructed a vaccinia virus expressing o-Dbl, a truncated form of proto-Dbl, that acts as a potent guanine nucleotide exchange factor for these Rho GTPases (14, 15) (Fig. 3 Inset, lanes 1 and 2). B6A4C1 cells expressing o-Dbl displayed a significant enhancement of antigen-stimulated degranulation, although this was less than the enhancement obtained with an equivalent amount of Cdc42V12 virus (Fig. 3). Similarly, expression of o-Dbl partly rescued Ca2+ signaling, enhancing both the sustained Ca2+ influx (Fig. 4b) and release from ER stores (Fig. 4e), to levels intermediate between those of the empty vector control and Cdc42V12 in antigen-stimulated cells (Fig. 4 a and d). This partial restoration of stimulated degranulation and Ca2+ mobilization by o-Dbl suggests that endogenous Cdc42 and Rac1 are functional, and that B6A4C1 cells may be defective in the upstream activation of these Rho GTPases. The less potent effects of o-Dbl compared with Cdc42V12 and Rac1V12 may reflect difficulties in achieving the proper localization of the nucleotide exchange factor, given that Dbl is normally expressed in brain and adrenal glands, and may not be properly localized in the RBL mast cells.
Figure 3.
o-Dbl and PLCγ1 partially restore degranulation in B6A4C1 cells. B6A4C1 cells were infected with either 60 pfu/cell of empty vector, Cdc42V12, or o-Dbl, or 20 pfu/cell of empty vector, Cdc42V12, or PLCγ1 for 6 h at 37°C. Degranulation assays were performed as described in Fig. 1 and Materials and Methods. Error bars represent the standard deviation of at least three independent experiments. B6A4C1 cells infected with 60 pfu/cell of o-Dbl (Inset, lane 2) or 20 pfu/cell of PLCγ1 (Inset, lane 4) for 6 h at 37°C, or left uninfected (Inset, lanes 1 and 3) were lysed, proteins were resolved by SDS/PAGE, and the virus-expressed proteins were detected by Western blotting by using anti-Dbl or anti-PLCγ1 antibodies.
Figure 4.
PLCγ1 expression enhances Ca2+ signaling to the same level as dominant-active Cdc42, whereas o-Dbl exhibits partial rescue in B6A4C1 cells. B6A4C1 cells were infected with 20 pfu/cell of vector and Cdc42V12 (a and d); o-Dbl (b and e); and PLCγ1 (c and f) for 6 h at 37°C and loaded with indo-1. Overall Ca2+ responses were measured in response to stimulation with 100 ng/ml DNP/BSA (➩). To measure release of Ca2+ from ER stores (d–f), loaded cells were treated with 4 mM EDTA (➞) and then stimulated with 100 ng/ml DNP/BSA. Measurements of the Ca2+ responses in the absence and presence of EGTA were performed concurrently. Traces shown are representative of at least three independent experiments.
Activated Cdc42/Rac1 and PLCγ1 Synergistically Activate Degranulation in B6A4C1 Cells.
We previously obtained evidence suggesting that activated Cdc42 interacted with PLCγ1, although we were not able to establish that Cdc42 binding regulated PLCγ1 activity (4). To further examine a possible functional link between Cdc42 or Rac1 and PLCγ1, we constructed a PLCγ1 vaccinia virus to determine whether PLCγ1 overexpression (Fig. 3 Inset, lanes 3 and 4) could restore signaling in B6A4C1 cells and whether Cdc42V12/Rac1V12 could work together with PLCγ1 to stimulate Ca2+ mobilization and degranulation.
Overexpression of PLCγ1 restored antigen-stimulated degranulation to a modest extent in B6A4C1 cells, compared with the more enhanced level of degranulation displayed by cells infected with Cdc42V12 under the same conditions (Fig. 3). In contrast, PLCγ1 reconstituted total Ca2+ signaling (Fig. 4c) and initial release from ER stores (Fig. 4f) as effectively as Cdc42V12 (Fig. 4 a and d). This differential rescue of degranulation and Ca2+ mobilization by PLCγ1 suggests that reconstitution of the stimulated Ca2+ response by activated Cdc42/Rac1 may only partially account for the functional role of these Rho GTPases in stimulated degranulation.
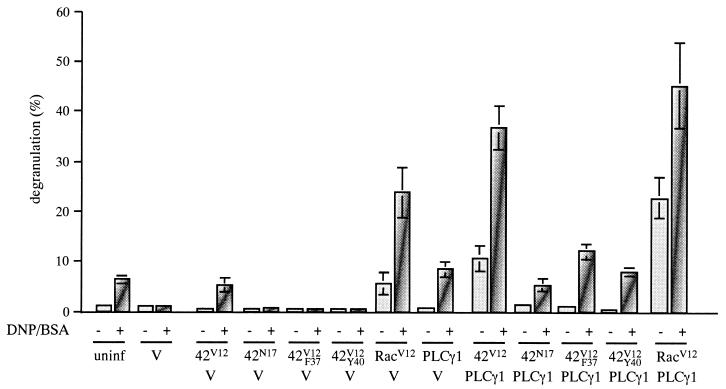
To examine the effects of coexpression of PLCγ1 with Cdc42V12/Rac1V12, B6A4C1 cells were infected simultaneously with 75% of each titer used in previous experiments. Under these conditions, coinfection of empty vector with Cdc42V12, Rac1V12, or PLCγ1 produced smaller increases in antigen-stimulated degranulation compared with infection with the single viruses alone (compare Fig. 5 with Figs. 1 and 3). On coinfection of PLCγ1 with Cdc42V12 or Rac1V12, significant degranulation was stimulated even in the absence of antigen (Fig. 5), with PLCγ1/Cdc42V12 generating ≈11% degranulation, and PLCγ1/Rac1V12, yielding ≈23% degranulation, whereas the individual viruses generated a sum of ≈1% and 6%, respectively. Thus, both activated Cdc42 and activated Rac1 can work in a synergistic fashion with PLCγ1 to promote degranulation and thereby bypass the requirement for activation of the IgE receptor.
Figure 5.
Coexpression of PLCγ1 with either dominant-active Cdc42 or Rac1 synergistically activates degranulation in B6A4C1 cells. B6A4C1 cells were coinfected with 15 pfu/cell of each of two viruses (30 pfu/cell total) as indicated, or infected with 30 pfu/cell of vector, for 6 h at 37°C, or left uninfected. Degranulation assays were performed as described in Fig. 1 and Materials and Methods. Error bars represent the standard deviation of at least three independent experiments.
On antigen stimulation, coinfection of Cdc42 and PLCγ1 further enhanced degranulation to ≈37%, which is more than twice the value that would be expected if the actions of Cdc42V12 and PLCγ1 were simply additive. Similarly, coexpression of Rac1V12 and PLCγ1 yielded ≈45% antigen-stimulated degranulation, whereas the individual viruses generated a sum of ≈33%. In contrast, coinfection of PLCγ1 with dominant-negative Cdc42N17 did not exhibit synergistic activation, but instead yielded a lower level of degranulation (≈5%) compared with that displayed by PLCγ1 expression alone (≈9%), thus suggesting that the activation of endogenous Cdc42 may be necessary to stimulate PLCγ1 activity. Furthermore, coinfection of PLCγ1 with either of the effector domain mutants, Cdc42V12,F37 and Cdc42V12,Y40, also prevented the synergy between Cdc42V12/Rac1V12 and PLCγ1, producing antigen-stimulated degranulation levels similar to that measured for PLCγ1 expression alone. The capacity of PLCγ1 and Cdc42V12/Rac1V12 to synergistically activate degranulation, in the presence and absence of antigen, together with the inhibitory effects produced by dominant-negative Cdc42, suggest that these proteins are functionally coupled and play key roles in antigen-stimulated degranulation.
Discussion
This study provides the first direct evidence for a critical role for Cdc42/Rac1 in receptor-stimulated Ca2+ mobilization. This conclusion is based on an analysis of the B6A4C1 mutant RBL mast cell line, which exhibits a unique phenotype: normal FcɛRI-mediated tyrosine phosphorylation, including phosphorylation of the Syk tyrosine kinase substrates PLCγ1 and PLCγ2, but no detectable PLCγ activity, and a general absence of downstream signaling, including phospholipase D activation, phospholipase A2 activation, actin polymerization, and degranulation (8). This phenotype suggests a defect in a key biochemical event that couples the antigen-stimulated tyrosine phosphorylation cascade to downstream lipase activation. The capacity of activated Cdc42 and Rac1 to restore antigen-stimulated Ca2+ mobilization and degranulation to wild-type levels in these mutant cells provides strong evidence that activation of these Rho family members by antigen is a key event in the normal sequelae of FcɛRI-mediated signal transduction in mast cells.
The mechanism by which activated Cdc42/Rac1 participates in the restoration of sustained Ca2+ mobilization and degranulation in B6A4C1 cells is not yet clear. Our previous study provided evidence that GTP-bound Cdc42 binds selectively to a PLCγ1 species with a slightly faster mobility on SDS/PAGE than bulk PLCγ1 (4). Thus, Cdc42/Rac1 may activate PLCγ1 by direct interaction, perhaps analogous to the direct activation of PLCβ2 by Rho family members (16). Alternatively, Cdc42/Rac1 may activate a pathway that synergizes with activated PLCγ to stimulate IP3 production. Previous evidence that Cdc42 and/or Rac1 participate in the activation of phosphatidylinositol 4-phosphate 5-kinase (17) and phospholipase D (18) may be relevant to our findings, because the former enzyme catalyzes the synthesis of phosphatidylinositol-4,5-bisphosphate, the substrate for PLC, and the latter provides a key cofactor (phosphatidic acid) for this synthesis (19). Consistent with our findings, Ali et al. (20) previously showed that GDPβS prevents antigen-stimulated inositol phosphate production in streptolysin O-permeabilized RBL cells.
In addition to a role in antigen-stimulated Ca2+ mobilization, it is possible that Cdc42/Rac1 activates a separate biochemical event that is also important for antigen-stimulated degranulation. We in fact observed that overexpression of PLCγ1 fully restores antigen-stimulated Ca2+ mobilization, but only poorly restores the degranulation response (Figs. 3 and 4). Furthermore, this response is fully restored by the synergistic effects of cotransfected PLCγ1 and activated Cdc42/Rac1 (Fig. 5). Activation of phospholipase D has been shown to correlate with reconstitution of antigen-stimulated degranulation in permeabilized RBL cells under conditions of buffered free Ca2+ (21), so it is possible that activation of phospholipase D by Cdc42/Rac1 (18) accounts for this second step in the signaling cascade that leads to stimulated exocytosis. Activation of Rho family GTPases is also known to stimulate actin polymerization in peritoneal mast cells (22, 23), but this function is unlikely to be important for the role of Cdc42/Rac1 in stimulated exocytosis in RBL cells. Inhibition of these cytoskeletal changes by cytochalasin D fails to inhibit exocytosis, and actually enhances the earliest signaling events stimulated by antigen in these cells (13, 24). In summary, although the precise mechanism by which activated Cdc42/Rac1 restores antigen-stimulated Ca2+ mobilization and degranulation in the B6A4C1 cells is still not fully understood, it is apparent that these Rho family proteins must act early in the cascade of signaling events.
Our observations that o-Dbl can partially restore sustained Ca2+ mobilization and degranulation in B6A4C1 cells (Figs. 3 and 4) are consistent with the hypothesis that these cells are defective in Cdc42/Rac1 activation by antigen. However, the endogenous guanine nucleotide exchange factor that normally participates in this process in RBL-2H3 cells has not yet been identified, and it is not yet clear whether the biochemical defect in B6A4C1 cells exists at the level of, or is upstream from, the exchange factor. Recent molecular genetic studies have shown that the Rac1 exchange factor Vav plays an important role in T and B cell signaling leading to IL-2 production (25, 26), but the phenotype of the Vav−/− T and B cells only partially resembles that of the B6A4C1 cells. The capacity of activated Cdc42 but not activated Rac1 to restore lipid raft biosynthesis in B6A4C1 cells (8) suggests that activation of Cdc42 is the primary defect in these mutant cells. The capacity of activated Rac1 to reconstitute Ca2+ mobilization and degranulation in these cells can be explained by postulating that Rac1 is downstream of Cdc42 in the FcɛRI signaling cascade but not in the effector pathways important for lipid raft biosynthesis. Our finding that the F37A mutation prevents Cdc42V12 from reconstituting antigen-stimulated Ca2+ mobilization (Fig. 2) and degranulation (Fig. 1) is consistent with this hypothesis. Interestingly, this mutation fails to prevent Cdc42V12 from reconstituting lipid raft biosynthesis (E. Hong-Geller and D. Holowka, unpublished observations), suggesting that a region in Cdc42 distinct from this effector domain may mediate lipid raft biosynthesis.
In conclusion, our results provide evidence for a key role for Cdc42 and Rac1 in early FcɛRI-mediated signaling. They indicate that these Rho family members are critical for antigen-stimulated Ca2+ mobilization leading to degranulation, and this may turn out to be of more general importance for antigen receptors in the immune response.
Acknowledgments
We thank C. Fewtrell for the use of her fluorescence spectrophotometer; B. Moss and S. G. Rhee for sharing reagents; and C. Westmiller for secretarial assistance. This work is supported by an American Cancer Society postdoctoral fellowship (to E.H.); and National Institutes of Health Grants GM47458 (to R.A.C.) and AI22449 (to D.H. and B.B.).
Abbreviations
- PLCγ
phospholipase Cγ
- IP3
inositol-1,4,5-triphosphate
- ER
endoplasmic reticulum
- DNP/BSA
dinitrophenyl-BSA
- o-Dbl.
References
- 1.Hamawy M M, Mergenhagen S E, Siraganian R P. Cell Signalling. 1995;7:535–544. doi: 10.1016/0898-6568(95)00024-j. [DOI] [PubMed] [Google Scholar]
- 2.Kinet J P. Annu Rev Immunol. 1999;17:931–972. doi: 10.1146/annurev.immunol.17.1.931. [DOI] [PubMed] [Google Scholar]
- 3.Berridge M J. Nature (London) 1993;361:315–325. doi: 10.1038/361315a0. [DOI] [PubMed] [Google Scholar]
- 4.Hong-Geller E, Cerione R A. J Cell Biol. 2000;148:481–494. doi: 10.1083/jcb.148.3.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall A. Science. 1998;279:509–514. doi: 10.1126/science.279.5350.509. [DOI] [PubMed] [Google Scholar]
- 6.Stracke M L, Basciano L K, Siraganian R P. Immunol Lett. 1987;14:287–292. doi: 10.1016/0165-2478(87)90006-x. [DOI] [PubMed] [Google Scholar]
- 7.Stephan V, Guo N, Ginsburg V, Siraganian R P. J Immunol. 1991;146:4271–4277. [PubMed] [Google Scholar]
- 8.Field K A, Apgar J R, Hong-Geller E, Siraganian R P, Baird B, Holowka D H. Mol Biol Cell. 2000;11:3661–3673. doi: 10.1091/mbc.11.10.3661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lamarche N, Tapon N, Stowers L, Burbelo P D, Aspenstrom P, Bridges T, Chant J, Hall A. Cell. 1996;87:519–529. doi: 10.1016/s0092-8674(00)81371-9. [DOI] [PubMed] [Google Scholar]
- 10.Ferris C D, Huganir R L, Supattapone S, Solomon S H. Nature (London) 1989;342:87–89. doi: 10.1038/342087a0. [DOI] [PubMed] [Google Scholar]
- 11.Mignery G A, Sudhof T C. EMBO J. 1990;9:3893–3898. doi: 10.1002/j.1460-2075.1990.tb07609.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoth M, Penner R. Nature (London) 1992;355:353–356. doi: 10.1038/355353a0. [DOI] [PubMed] [Google Scholar]
- 13.Pierini L, Harris N T, Holowka D, Baird B. Biochemistry. 1997;36:7447–7456. doi: 10.1021/bi9629642. [DOI] [PubMed] [Google Scholar]
- 14.Eva A, Aaronson S A. Nature (London) 1985;316:273–275. doi: 10.1038/316273a0. [DOI] [PubMed] [Google Scholar]
- 15.Hart M J, Eva A, Evans T, Aaronson S A, Cerione R A. Nature (London) 1991;354:311–314. doi: 10.1038/354311a0. [DOI] [PubMed] [Google Scholar]
- 16.Illenberger D, Schwald F, Pimmer D, Binder W, Maier G, Dietrich A, Gierschik P. EMBO J. 1998;17:6241–6249. doi: 10.1093/emboj/17.21.6241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hartwig J H, Bokoch G M, Carpenter C L, Janmey P A, Taylor L A, Toker A, Stossel T P. Cell. 1995;82:643–653. doi: 10.1016/0092-8674(95)90036-5. [DOI] [PubMed] [Google Scholar]
- 18.Singer W D, Brown H A, Bokoch G M, Sternweis P C. J Biol Chem. 1995;270:14944–14950. doi: 10.1074/jbc.270.25.14944. [DOI] [PubMed] [Google Scholar]
- 19.Honda A, Nogami M, Yokozeki T, Nakamura H, Watanabe H, Kawamoto K, Nadayama K, Morris A J, Frohman M A, Kanaho Y. Cell. 1999;99:521–532. doi: 10.1016/s0092-8674(00)81540-8. [DOI] [PubMed] [Google Scholar]
- 20.Ali H, Collado-Escobar D M, Beaven M A. J Immunol. 1989;143:2626–2633. [PubMed] [Google Scholar]
- 21.Way G, O'Luanaigh N, Cockcroft S. Biochem J. 2000;346:63–70. [PMC free article] [PubMed] [Google Scholar]
- 22.Norman J C, Price L S, Ridley A J, Hall A, Koffer A. J Cell Biol. 1994;126:1005–1015. doi: 10.1083/jcb.126.4.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Norman J C, Price L S, Ridley A J, Koffer A. Mol Biol Cell. 1996;7:1429–1442. doi: 10.1091/mbc.7.9.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holowka D, Sheets E D, Baird B. J Cell Sci. 2000;113:1009–1019. doi: 10.1242/jcs.113.6.1009. [DOI] [PubMed] [Google Scholar]
- 25.Costello P S, Walters A E, Mee P J, Turner M, Reynolds L R, Prisco A, Sarner N, Zamoyska R, Tybulewicz V L J. Proc Natl Acad Sci USA. 1999;96:3035–3040. doi: 10.1073/pnas.96.6.3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Rourke L M, Tooze R, Turner M, Sandoval D M, Carter R H, Tybulewicz V L J, Fearon D T. Immunity. 1998;8:635–645. doi: 10.1016/s1074-7613(00)80568-3. [DOI] [PubMed] [Google Scholar]