Abstract
Context: Methicillin-resistant Staphylococcus aureus (MRSA) was once primarily a hospital-acquired organism, but now community-acquired MRSA (CA-MRSA) is causing outbreaks among otherwise healthy sport participants.
Objective: To investigate MRSA skin and soft tissue outbreaks within a collegiate football team and the effect of infection control measures over 3 years.
Design: Retrospective analysis.
Setting: College.
Patients or Other Participants: Collegiate football team.
Intervention(s): Infection control measures included education, following Centers for Disease Control and Prevention recommendations, nasal cultures, hexachlorophene 3% soap, disposable towels, and hand sanitizers.
Main Outcome Measure(s): Number of MRSA infections and hospitalizations.
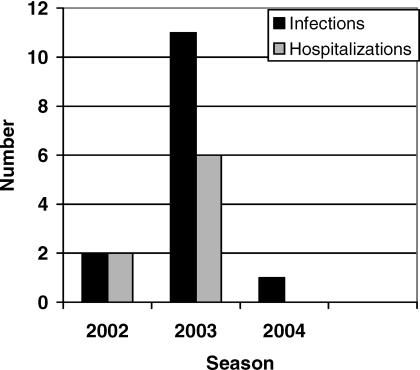
Results: Complicated skin and soft tissue infections (those requiring surgical debridement and/or hospitalization) were diagnosed in 2 (1.8%) of 107 players in 2002, 17 (15.8%) of 107 players in 2003, and 1 (0.96%) of 104 players in 2004.
Conclusions: Outbreaks of CA-MRSA in sports teams are very serious, and recognition is crucial. Treatment includes incision for proper drainage, bacterial culture and sensitivity, and appropriate antibiotic therapy. Infection control measures include educating athletes and staff, following Centers for Disease Control and Prevention recommendations, identifying CA-MRSA carriers with nasal cultures, introducing hexachlorophene 3% soap intermittently in the showers, making alcohol-based hand sanitizers available on the field, disinfecting weight training and rehabilitation equipment, and using disposable towels on the field during practices and games.
Keywords: infectious disease, cellulitis, spider bites
Contact sport participants are at increased risk for skin and soft tissue infections (SSTIs) because of the frequency of skin trauma and crowded conditions during the training season. Traditionally, the 2 most common bacterial causes of these infections are Staphylococcus aureus and Streptococcus pyogenes (Group A streptococcus). In recent years, a new pathogen, community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA), has been identified and described as increasingly important, although its true incidence is not known. 1 These new Staphylococcus aureus clones are believed to be more virulent and have been responsible for several outbreaks among collegiate and professional sport teams. 2–6 The high morbidities associated with these outbreaks call for more effective strategies for disease control and prevention.
We present a 3-year retrospective study of an outbreak of CA-MRSA SSTIs in a collegiate football team and discuss the strategies used to contain the outbreak, their implementation, and their effectiveness.
METHODS
During the 2002 football season, 2 players were hospitalized with severe SSTIs caused by MRSA. We enhanced surveillance of all team members for the rest of that season and subsequent seasons. All athletes with skin lesions were evaluated by the team's athletic trainers; those with possible infections were evaluated by one of the team physicians or by the student health center. Bacterial cultures of skin lesions were sent to a central laboratory, and available specimens were evaluated by the local public health department. Representatives from the public health department collected MRSA isolates from wound cultures and nasal swabs for pulsed field gel electrophoresis analysis.
We defined a definite case as a culture-confirmed MRSA abscess or cellulitis that occurred between August 2002 and December 2004. Probable cases were defined as athletes with abscesses occurring during this period that were not cultured but whose clinical complaints (severe pain at the site, “insect bite” as a cause, rapid onset) suggested CA-MRSA infection. An examination of hygienic practices at the team center, including towel use and shaving, was undertaken. On-site monitoring of hygienic practices at the facilities, including laundering of towels, was also performed.
RESULTS
All subjects were otherwise healthy college-aged males who were active participants on the football team. A review of the medical records of past seasons found no cases of complicated SSTIs (cSSTIs), or SSTIs requiring surgical debridement and/ or hospitalization caused by MRSA over the prior 20 years. During the 3 seasons of the study (2002, 2003, and 2004), we identified 14 confirmed cases of cSSTIs caused by CA-MRSA ( Figure 1). The spectrum of disease ranged from a small abscess requiring outpatient surgical drainage to a case of necrotizing fasciitis requiring hospitalization and multiple surgeries. Eight players required hospitalization.
Figure 1. Methicillin-resistant Staphylococcus aureus infections (confirmed) and hospitalizations in 3 football seasons .
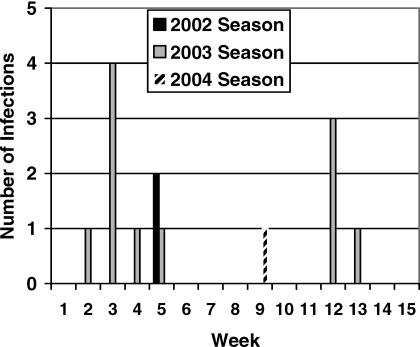
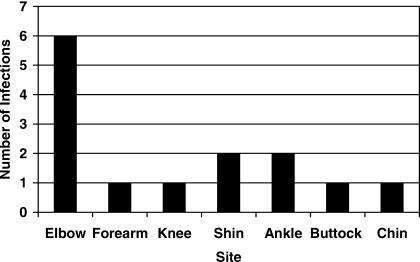
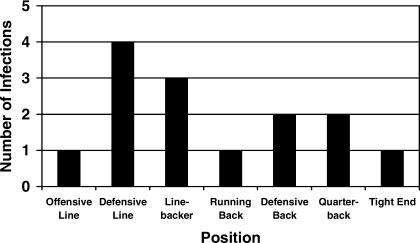
The timeline for reporting CA-MRSA SSTIs in this investigation was established by defining the first day of the season as the day the team reported to training camp. Weeks were counted from that first day. Over the 3 seasons, 64.3% (9/14) of all infections occurred between weeks 2 and 5 of the season ( Figure 2). The most common site of infection was the elbow (6/14, 42.8%) ( Figure 3). Defensive linemen (4) and linebackers (3) had 50.0% (7/14) of MRSA infections, but players at 5 other positions also experienced MRSA infections ( Figure 4).
Figure 2. Timeline of methicillin-resistant Staphylococcus aureus infections (confirmed cases) over 3 seasons .
Figure 3. Community-acquired methicillin-resistant Staphylococcus aureus skin and soft tissue infection lesion sites (n = 14) .
Figure 4. Methicillin-resistant Staphylococcus aureus infections according to player position (n = 14) .
2002 Football Season
In the 2002 football season, 2 football players (1.8%) from a team of 107 had cSSTIs caused by CA-MRSA in the fifth week of the season. Player 1 presented with a painful pimple on his elbow, flu-like symptoms, and low-grade fever (100.0°F [37.8°C]). He was hospitalized on the day of presentation. Necrotizing fasciitis was confirmed at the time of surgery on the day of admission, and cultures showed only MRSA. The player underwent multiple surgical procedures but ultimately recovered. Player 2 was hospitalized with a painful abscess on his lower leg. A team physician performed surgical incision for drainage, and the athlete received intravenous and oral antibiotic therapy. The MRSA isolates were indistinguishable on pulsed field gel electrophoresis.
2003 Football Season
In the 2003 football season, 17 football players from a team of 107 (15.8%) were identified with cSSTIs. All required surgical incision and drainage. A total of 11 players (10.3%) had confirmed cases, with cSSTIs that were incised and cultures that showed MRSA; 6 of the 11 were hospitalized. Six players (5.6%) had probable cases, with abscesses requiring incision and drainage, but no cultures were performed.
Of the 17 cases of cSSTIs, 13 (76.5%) occurred from weeks 2 through 5. Players presented with 3 additional MRSA skin infections in week 12, and the athlete with the final MRSA infection was hospitalized in week 14. All available MRSA wound isolates were identified on pulsed field gel electrophoresis as the same strain (US-300) of CA-MRSA. Environmental cultures were taken in the athletic training room and in the football locker room. All environmental samples were negative for MRSA. Staff athletic trainers, athletic equipment staff, and students working with the football program had nasal cultures toward the end of the season. None tested positive for MRSA.
2004 Football Season
One infection occurred in the 2004 football season. The player was a quarterback who had had a similar infection the previous season. The MRSA was confirmed by culture, and the athlete was treated with incision for proper drainage and antibiotic therapy.
INTERVENTIONS
2002 Football Season
After we identified 2 cases in week 5, an investigation was initiated by the Los Angeles County Department of Health Services. The following measures were then instituted: use of hexachlorophene 3% (Phisohex, Sanofi-Synthelab, Inc, New York, NY) in the showers and bathrooms, covering all open wounds to prevent spread of infection, increased emphasis on athletic trainer hygiene and universal precautions, not allowing athletes in whirlpools when they had open wounds, and discontinuing multiuse lotions with pumps or other preparations for massage because of the concern about the possibility of bacterial transmission. Players were instructed on the importance of showering; advised to refrain from sharing towels, equipment, and personal items; and directed to report any suspicious skin lesions to the medical staff immediately. No further SSTIs occurred that season.
2003 Football Season
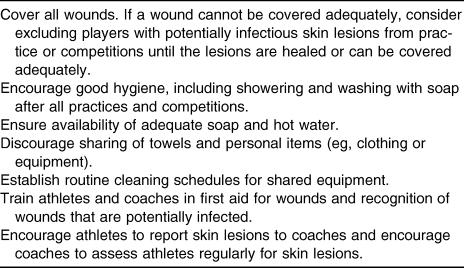
At the start of the season, players received instructions as in the previous season. Also included this time were instructions to have all open wounds covered by a staff athletic trainer before practices or games. At week 3, after 5 infections were identified, a meeting to discuss infection control strategies was held, involving staff athletic trainers, team physicians, and a consultant infectious disease physician. Topics included recognizing common signs and symptoms of MRSA-associated SSTIs; bacterial transmission; appropriate treatment options; review of infection control techniques in the athletic training room, locker room, weight room, and laundry facility; personal hygiene; and educating administrators, coaches, and athletes. Many of these strategies were adopted from the published Centers for Disease Control and Prevention measures for preventing staphylococcal skin infections among sports participants ( Table 1).
Table 1. Centers for Disease Control and Prevention Measures for Preventing Staphylococcal Skin Infections Among Sports Participants4.
A protocol was developed for the treatment of cSSTIs. All abscesses received incision and drainage, and wound cultures were taken whenever possible. Patients received antibiotic therapy with doxycycline 100 mg twice a day and rifampin 600 mg daily for 7 days. All open wounds were covered with dressings to prevent transmission. Patients with abscesses too large to drain in the outpatient setting or with severe cellulitis and those who did not respond to antibiotic therapy were hospitalized for intravenous antibiotic therapy and surgical debridement as needed.
Infection-control strategies were reviewed and implemented. Athletes who had just practiced, played, or worked out were instructed to shower before entering the athletic training room. Treatment tables, taping tables, and rehabilitation equipment in the athletic training and weight rooms were sprayed with disinfectant frequently throughout the day. The cotton towels used to wipe ultrasound gel and massage lotion and those that were placed between the athlete and hot pack covers were deposited in a hamper clearly marked “soiled” for laundering after each use. Athletic trainers were instructed to wash their hands with soap and water after each treatment. After week 12, disposable paper towels were used on the practice field and at games to prevent sharing towels and the spread of bacteria. Used towels were discarded immediately. Alcohol-based hand sanitizers were made available to all medical staff when on the practice field or at games. Laundry procedures were discussed with the equipment staff. Investigations showed that the water in the laundry facility did not reach the recommended temperature of 140°F (60°C), so water temperatures were increased to meet the recommendation.
The head athletic trainer instructed the players to shower after practices, workouts, and games with the soap provided in the dispensers and to use hot water; to put soiled laundry and towels in the hampers labeled “soiled”; to refrain from sharing towels, clothes, and equipment; to show all pimples, boils, spider bites, lacerations, and abrasions to medical staff immediately; and to have all open or draining wounds covered by staff athletic trainers. Signs were posted in the locker room and outside the athletic training room. Phisohex was installed in the soap dispensers of the showers and bathrooms of the football locker room in week 3 and maintained until week 8.
Nasal cultures were performed on the entire team to identify MRSA carriers. Nasal cultures were taken from all available members (n = 106; 1 player was hospitalized with MRSA) of the team in week 4. Week 4 results showed 7 players (6.6%) colonized with MRSA and 19 players (17.9%) with methicillin-sensitive Staphylococcus aureus. Because of the CA-MRSA outbreak, all MRSA carriers (7) were decolonized with topical nasal mupirocin ointment and oral rifampin (600 mg daily for 10 days). Compliance was 100% because the athletes were closely monitored by staff athletic trainers. Nasal cultures were repeated in week 7 on all available team members (n = 107). All 7 players colonized with MRSA in week 4 were negative, but 4 new players (3.7%) showed MRSA in the nares. Those 4 players received the same decolonization treatment, after which all had negative repeat nasal cultures.
2004 Football Season
Nasal cultures were performed on the first day of the season at the time of physical examinations, and 104 football players provided nasal swabs. Three players (2.9%) tested positive for MRSA: 2 returning players and 1 player who was new to the team. Two of the players received decolonization treatment, and both were negative on reculture after treatment. The third player left the team before the culture was identified. Nasal cultures were not repeated for the remaining football players.
The head athletic trainer held a meeting on the first day of training camp to remind all football players to report immediately to a staff athletic trainer any skin lesions, such as spider bites, pimples, and boils. Players were warned of the dangers of sharing towels, clothing, equipment, and personal items and were instructed to have all open wounds covered by a staff athletic trainer before practice or games.
Phisohex was installed in the showers for the entire period of training camp and through the week of the first game. Phisohex was reintroduced into the showers and bathroom after the first and only case of MRSA infection in week 11 and was discontinued after week 13. Only disposable towels were used on the field for practices and games for the entire season to prevent sharing. All towels were discarded after each use. Hand sanitizers were made available to all sports medicine personnel to be used after person-to-person contact. Treatment tables and equipment were sprayed with disinfectant spray throughout the day. Hot water temperatures were consistently kept at 140°F (60°C) for laundry and showers. Signs remained posted in the locker room and outside the athletic training room reminding athletes to shower after workouts, practices, and games; not to share towels, clothing, or personal items; and to report any suspicious skin lesions or spider bites to a staff athletic trainer immediately.
DISCUSSION
In the past 2 decades, CA-MRSA has emerged as a major community pathogen. This new entity has a remarkable ability to strike children and young, healthy adults. 7 It has a predilection for skin and soft tissue and is more virulent than methicillin-sensitive Staphylococcus aureus, causing rapidly progressive cellulitis and necrotizing abscesses. 8–10 Team sport athletes are especially susceptible to CA-MRSA caused by skin trauma, such as turf burns, abrasions, shaving, and chafing. 2 3 Infections are facilitated by the sharing of towels and equipment and prolonged physical contact. 2 3 The Centers for Disease Control and Prevention and other organizations have reported outbreaks in football, fencing, and wrestling teams. 2–5
The high morbidities on our football team and others illustrate the importance of early recognition of this disease. In our experience, a striking clinical feature of CA-MRSA was pain out of proportion with physical examination. The pain was often described by athletes as the pain from a “spider bite.” We postulate that the Panton-Valentine leukocidin toxin, present in 95% of CA-MRSA isolates, 11 may be responsible for this symptom via induction of tissue necrosis. At early stages, the infection most resembles a boil or a pimple, which may rapidly progress to form an abscess, cellulitis, deep-seated furuncles, 12 13 or necrotizing fasciitis.
Because the organism is not susceptible to the beta-lactam antibiotics generally used as empiric treatment for SSTIs in the outpatient setting, its identification is necessary to provide appropriate therapy and to guide the use of infection control measures. All suspicious abscesses should be surgically drained and cultured. Incision and drainage alone may be sufficient for abscesses smaller than 5 cm without the need for adjunct antibiotics. 14 For those who need antibiotics, either trimethoprim-sulfamethazole or doxycycline in combination with rifampin are effective. This is the regimen used at our institution. Clindamycin may be active but is prone to cause antibiotic-associated diarrhea. 14 15
Decolonization is a controversial practice. The practice guidelines of the Infectious Disease Society of Washington 16 consider it ineffective and resistance promoting and recommend against it. Eradication is temporary, because the colonizer is frequently reinfected from household members or from contaminated household items. 17 Our experience shows that the athletes are consistently exposed to MRSA from the community and that cross-transmission occurs among team members. Decolonization is, therefore, temporary. However, in light of our outbreak, tight training schedule, and crowded dormitories, we decided to be proactive in identifying and eradicating MRSA colonization. In the setting of an outbreak, we believe decolonization may be indicated. However, as a standard practice, we do not endorse routine nasal cultures and decolonization.
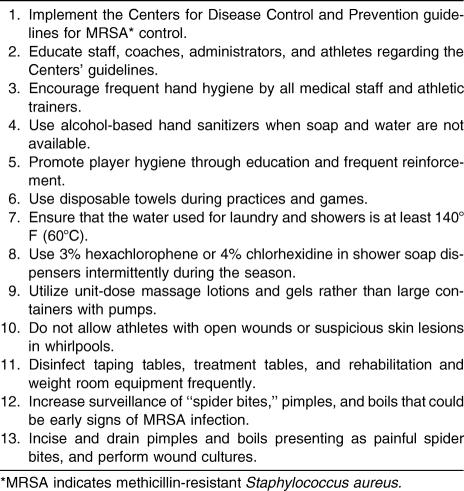
Infection control measures and prevention are vital to the disease containment effort. The Centers for Disease Control and Prevention have published recommendations for the prevention of CA-MRSA spread, and we modeled many of our interventions on their recommendations ( Table 2). Once in place, our interventions resulted in a significant decrease in MRSA cSSTIs. We feel that all the components of the infection control measures were important in contributing to our success.
Table 2. University of Southern California Infection Control Measures.
CONCLUSIONS
Today, CA-MRSA is increasingly recognized as the agent responsible for SSTI outbreaks among sport teams, causing significant morbidity and lost days of practice. In this paper, we described an outbreak in a collegiate football team and outlined the interventions taken to control the outbreak and prevent future recurrences. In summary, the Centers for Disease Control and Prevention guidelines are excellent principles that can reduce risk of CA-MRSA SSTIs among sports participants. 4 Intermittent use of Phisohex soap may reduce the incidence of SSTI in this population, although prolonged use is contraindicated because of toxicity, cost, and development of future resistance. Chlorhexidine 4% soap may be a better option. Nasal cultures, especially at the beginning of the season, may identify people who are colonized with MRSA. New or returning members can introduce CA-MRSA to the team. Although MRSA nasal colonization can be unpredictable, it is consistently introduced from the community. The use of nasal decolonization is controversial, and its effects may be temporary and lead to future drug resistance. Clinicians should have a high level of suspicion of CA-MRSA with any reported skin lesion that feels like a spider bite. Those SSTIs that present with an abscess should be incised and drained, and cultures should be taken at that time. Antibiotic use should be considered carefully by physicians. All sports medicine programs should review their infection control procedures. Disposable towels are strongly recommended on the field and during practices and games to discourage sharing and the spread of bacteria, and alcohol-based hand sanitizers should be made available on the field for practices and games.
Acknowledgments
We thank Laurene Mascola, MD, Chief of Acute Communicable Disease Control at the Los Angeles County Public Health Department, for her support and expertise during our MRSA outbreak experience. We also recognize Mike Garrett, Director of Athletics at the University of Southern California, for his leadership and trust at a time when there were more questions than answers.
REFERENCES
- Chambers HF. The changing epidemiology of Staphylococcus aureus? . Emerg Infect Dis. 2001;7:178–182. doi: 10.3201/eid0702.010204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazakova SV, Hageman JC, Matava M. A clone of methicillin-resistant Staphylococcus aureus among professional football players . N Engl J Med. 2005;352:468–475. doi: 10.1056/NEJMoa042859. et al. [DOI] [PubMed] [Google Scholar]
- Begier EM, Frenette K. Barrett NL, and the Connecticut Bioterrorism Field Epidemiology Response Team. A high-morbidity outbreak of methicillin-resistant Staphylococcus aureus among players on a college football team, facilitated by cosmetic body shaving and turf burns . Clin Infect Dis. 2004;39:1446–1453. doi: 10.1086/425313. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Methicillin-resistant Staphylococcus aureus infections among competitive sports participants: Colorado, Indiana, Pennsylvania, and Los Angeles County, 2000–2003 . MMWR Morb Mortal Wkly Rep. 2003;52:793–795. [PubMed] [Google Scholar]
- Lindenmayer JM, Schoenfeld S, O'Grady R, Carney JK. Methicillin-resistant Staphylococcus aureus in a high school wrestling team and the surrounding community . Arch Intern Med. 1998;158:895–899. doi: 10.1001/archinte.158.8.895. [DOI] [PubMed] [Google Scholar]
- Stacey AR, Endersby KE, Chan PC, Marples RR. An outbreak of methicillin-resistant Staphylococcus aureus infection in a rugby football team . Br J Sports Med. 1998;32:153–4. doi: 10.1136/bjsm.32.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herold BC, Immergluck LC, Maranan MC. Community-acquired methicillin-resistant Staphylococcus aureus in children with no identified predisposing risk . JAMA. 1998;279:593–598. doi: 10.1001/jama.279.8.593. et al. [DOI] [PubMed] [Google Scholar]
- Naimi ST, LeDell HK, Como-Sabetti K. Comparison of community and health care-associated methicillin-resistant Staphylococcus aureus infection . JAMA. 2003;290:2976–2984. doi: 10.1001/jama.290.22.2976. et al. [DOI] [PubMed] [Google Scholar]
- Young DM, Harris HW, Charlebois ED. An epidemic of methicillin-resistant Staphylococcus aureus soft tissue infections among medically underserved patients . Arch Surg. 2004;139:947–951. doi: 10.1001/archsurg.139.9.947. et al. [DOI] [PubMed] [Google Scholar]
- Ellis MW, Hospenthal DR, Dooley DP, Gray PG. Natural history of community-acquired methicillin-resistant Staphylococcus aureus colonization and infection in soldiers . Clin Infect Dis. 2004;39:971–979. doi: 10.1086/423965. [DOI] [PubMed] [Google Scholar]
- Diep BA, Sensabaugh GF, Somboona NS, Carleton HA, Perdreau-Remington F. Widespread skin and soft-tissue infections due to 2 methicillin-resistant Staphylococcus aureus strains harboring the genes for Panton-Valentine leucocidin . J Clin Microbiol. 2004;42:2080–2084. doi: 10.1128/JCM.42.5.2080-2084.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggett HC, Hennessy TW, Rudolph K. Community-onset methicillin-resistant Staphylococcus aureus associated with antibiotic use and the cytotoxin Panton-Valentine leukocidin during a furunculosis outbreak in rural Alaska . J Infect Dis. 2004;189:1565–1573. doi: 10.1086/383247. et al. [DOI] [PubMed] [Google Scholar]
- Yamasaki O, Kaneko J, Morizane S. The association between Staphylococcus aureus strains carrying Panton-Valentine leukocidin genes and the development of deep seated follicular infection . Clin Infect Dis. 2005;40:381–385. doi: 10.1086/427290. et al. [DOI] [PubMed] [Google Scholar]
- Lee MC, Rios AM, Aten MF. Management and outcome of children with skin and soft tissue abscesses caused by community-acquired methicillin-resistant Staphylococcus aureus . Pediatr Infect Dis J. 2004;23:123–127. doi: 10.1097/01.inf.0000109288.06912.21. et al. [DOI] [PubMed] [Google Scholar]
- Martinez-Aguilar G, Hammerman WA, Mason EO, Jr, Kaplan SL. Clindamycin treatment of invasive infections caused by community-acquired, methicillin-resistant and methicillin-susceptible Staphylococcus aureus in children . Pediatr Infect Dis J. 2003;22:593–598. doi: 10.1097/01.inf.0000073163.37519.ee. [DOI] [PubMed] [Google Scholar]
- Dellit T, Duchin J, Hofmann J, Olson EG. Interim guidelines for evaluation & management of community associated methicillin resistant Staphylococcus aureus skin and soft tissue infections in outpatient setting . Available at: http://www.doh.wa.gov/Topics/Antibiotics/providers_MRSA_guidelines.htm. Accessed September 2, 2004 .
- Kniehl E, Becker A, Forster DH. Bed, bath and beyond: pitfalls in prompt eradication of methicillin-resistant Staphylococcus aureus carrier status in healthcare workers . J Hosp Infect. 2005;59:180–187. doi: 10.1016/j.jhin.2004.06.016. [DOI] [PubMed] [Google Scholar]