Abstract
Context: Exposure of the human body to cold is perceived as a stressor and results in a sympathetic response geared at maintaining core temperature. Application of ice to the periphery may lead to a decrease in core temperature, which may counteract the therapeutic effects of cryotherapy.
Objective: To determine if core temperature is lowered by the application of an ice bag to the ankle joint complex.
Design: A within-subjects, repeated-measures design.
Setting: The University of Virginia General Clinical Research Center.
Patients or Other Participants: Twenty-three healthy adults aged 19 to 39 years.
Intervention(s): Subjects were admitted to the hospital on 2 separate occasions. During one admission, subjects had a 20-minute ice treatment applied to their ankles; in the other admission, a bag of marbles was applied. Temperature measurements were recorded at 6 time intervals: baseline (before ice application), immediately after ice application, 10 and 20 minutes after ice application, and 10 and 20 minutes after ice removal.
Main Outcome Measure(s): We measured core temperature and ankle and soleus muscle surface temperatures. A mixed-effects model analysis of variance with repeated measures was used to determine if differences existed in core temperature and ankle and soleus surface temperatures between conditions (cryotherapy and control) and over time.
Results: Core temperature did not change after ice application or ice removal ( P > 0.05). The average core temperatures during the cryotherapy and control conditions were 36.72°C ± 0.42°C and 36.45°C ± 1.23°C, respectively.
Conclusions: A 20-minute cryotherapy treatment applied to the ankle did not alter core temperature.
Keywords: cryotherapy, cold, ice, temperature
Cryotherapy is commonly used immediately after acute musculoskeletal injuries to prevent swelling and secondary hypoxic injury and to reduce muscle spasm. 1 Furthermore, cryotherapy reduces pain 2 3 and may increase motoneuron pool excitability, 4 5 which enhances a patient's ability to perform therapeutic exercises. Therapeutic exercises are thought to be critical to recovery from injury.
Cutaneous cold application to the trunk can alter core body temperature. 6–8 Additionally, cold application to the knee has been shown to decrease core temperature in dogs. 9 Normal core body temperature is 36.9°C, and hypothermia is achieved after only small declines in core temperature (1.9°C or approximately 5%), which result in increased metabolic and respiratory rates and induce a shivering response. 10 Further declines in core temperature can lead to behavioral, cardiovascular, respiratory, renal, hematologic, endocrine, metabolic, and musculoskeletal alterations. 11
Presently, only the local effects are considered as contributors to recovery from injury or as an adjuvant to allow for therapeutic exercise. The additional effects that result from core temperature change may enhance or counteract the local effects of cryotherapy. For example, shivering, which is initiated in an attempt to maintain core body temperature, results in involuntary muscle contractions, possibly leading to increases in the temperature of structures we are attempting to cool. If the goal of the treatment is to decrease intramuscular temperature, this temperature increase may counteract the local effects of ice.
Because maintaining core body temperature plays a role in maintaining physical function (eg, preventing loss of strength and manual dexterity), it is important for us to understand if commonly used cryotherapy treatments can lead to declines in core body temperature. We are aware of no previous research examining the effects of peripheral ice bag application on core body temperature. Therefore, the purpose of our study was to determine if applying a cryotherapy treatment to the ankle would result in a decline in core body temperature. We hypothesized that a 20-minute cryotherapy treatment applied to the surface of the ankle joint complex would not alter core body temperature.
METHODS
We used a 2 × 6 factorial design in this study. The 2 independent variables were condition (cryotherapy and control) and time (baseline, immediately after application, 10 and 20 minutes after application, and 10 and 20 minutes after removal). The dependent variables were core temperature, ankle surface temperature, and soleus muscle surface temperature.
Subjects
Twenty-three healthy subjects (8 women and 15 men, age = 25 ± 14 years, height = 174 ± 10 cm, mass = 74 ± 17 kg) with no previous lower extremity injuries in the past 2 years volunteered to participate. Subjects were assessed for inclusion criteria by a preparticipation history questionnaire and a physical examination. Subjects were excluded if they reported a previous adverse reaction to ice. Informed consent was obtained before subject participation. Human subject approval was obtained from the Human Investigations Committee at the University of Virginia before the study began.
Instrumentation
We used a datalogger (MSS-3000; Commtest Instruments, Christchurch, New Zealand) in conjunction with thermocouples (Copper/constant type T thermocouples of the ball junction type; TX-31, HQ Inc, Columbus, OH) accurate to ±1.0°C to monitor surface interface temperature and ambient air temperature. Core temperature was assessed with the CorTemp 2000 Wireless Core Body Temperature Monitoring System and CorTemp disposable temperature sensors (CorTemp, HTI Technologies Inc, Palmetto, FL). The core temperature sensor is capable of monitoring core body temperature continuously as it travels through the digestive system. Each CorTemp temperature sensor is individually calibrated at the factory, and the calibration adjustment is entered into the wireless monitoring system before use, ensuring a temperature accuracy of ±0.1°C. Previous authors 12 have revealed a strong correlation ( r = 0.94) between rectal temperature and gut temperature as assessed with CorTemp sensors.
Testing Procedures
All 23 subjects completed both testing conditions (cryotherapy and control). Testing conditions were separated by at least 3 days. Each subject was considered a block, and the sequence of the admissions was assigned to each subject by way of a computer-generated random permutation.
Cryotherapy and Control Testing Sessions
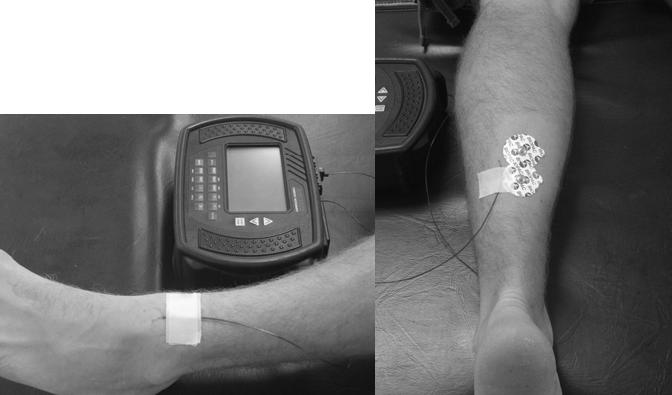
Subjects were admitted into the General Clinical Research Center the evening before testing. They ingested the core temperature pill at 11:00 pm and were then asked to prepare for bed; lights were turned off by midnight. Subjects were awoken at 5:50 am and were asked to void. Subjects then returned to bed and remained lying down until the completion of testing. Surface thermocouples were affixed to subjects' skin over the anterior aspect of the ankle and over the midbelly of the soleus muscle ( Figure). A single thermocouple was also allotted to record ambient air temperature. Beginning at 6:30 am, baseline core and surface temperature measurements were gathered. Subjects then had a cryotherapy treatment (an ice bag weighing approximately 0.91 kg) secured to the anterior aspect of the ankle joint (the ice bag was made to cover a surface area from the medial malleolus to the lateral malleolus). Temperature measurements were recorded immediately and at 10 minutes and 20 minutes after cryotherapy application. The ice bag was removed at the 20-minute mark. Measurements were also recorded at 10 and 20 minutes after removal. Once testing was completed, the thermocouples were removed and subjects were fed and then discharged from the Center.
Placement of the surface thermocouples on the ankle (left) and on the soleus muscle (right).
For the control condition, subject admission to the Center was as described above. All temperature measurements were time matched to the cryotherapy condition. However, instead of a cryotherapy treatment, a bag filled with marbles was applied to the anterior aspect of the ankle.
Statistical Analysis
Core, ankle surface, and soleus muscle surface temperature data were analyzed as univariate response variables by way of mixed-effects analyses of variance. The experimental condition (cryotherapy or control) and the measurement time (baseline, immediately after application, 10 and 20 minutes after application, and 10 and 20 minutes after removal) served as the independent factors. Univariate F tests and Sidak t multiple comparison procedures were used to make post hoc comparisons. Statistical significance was assessed at P ≤ .05. Where core temperature data points were missing, we estimated and replaced the missing values by multiple linear regression. All statistical analyses were conducted with the statistical software of SPSS (version 10.1; SPSS Inc, Chicago, IL).
RESULTS
Core Temperature
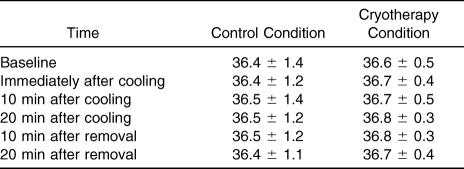
Data points were missing for a few subjects as a result of difficulties with the CorTemp monitoring system (3 data points for subject 18 during the control condition, 1 data point for subject 9 during the cryotherapy condition, and all data points for subject 11 during the control condition). No differences in core temperature were detected between conditions over time (F 5,110 = 0.51, P = .77) ( Table 1). Core temperature was not different between the cryotherapy and control conditions (F 1,22 = 1.14, P = .30) and also did not differ over time when collapsed across condition (F 5,110 = 0.89, P = .49).
Table 1. Core Temperatures (°C) for the Control and Cryotherapy Conditions Before, During, and After Ice Bag Application to the Ankle Joint Complex (Mean ± SD).
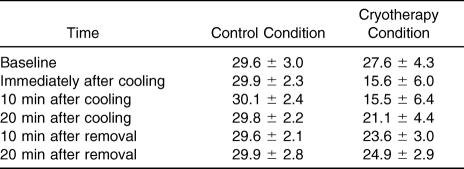
Ankle Surface Temperature
Ankle surface temperature was different between conditions over time (F 5,110 = 39.74, P = .0001). During the cryotherapy condition, ankle surface temperatures recorded immediately after application, 10 and 20 minutes after application, and 10 and 20 minutes after removal were lower than the ankle surface temperature at baseline ( P < .01) ( Table 2). During the control condition, no differences were noted over time for ankle surface temperature ( P > .05) ( Table 2). No differences were noted at any times when data were collapsed across conditions ( P > .05).
Table 2. Ankle Surface Temperatures (°C) for the Control and Cryotherapy Conditions Before, During, and After Ice Bag Application to the Ankle Joint Complex (Mean ± SD).
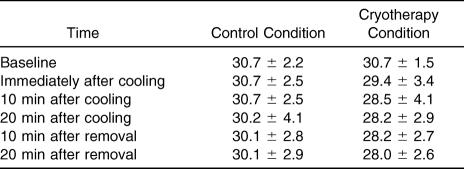
Soleus Muscle Surface Temperature
Soleus muscle surface temperature was different between conditions over time (F 5,110 = 3.08, P = .012). During the cryotherapy condition, soleus muscle surface temperatures recorded at 20 minutes after application and at 10 and 20 minutes after removal were lower than the soleus surface temperature at baseline ( P < .05) ( Table 3). Additionally, the soleus surface temperature recorded immediately after application was different from the temperature recorded at 20 minutes after removal ( P < .05). During the control condition, no differences were noted over time for ankle surface temperature ( P > .05) ( Table 3). No differences were noted at any times when data were collapsed across conditions ( P > .05).
Table 3. Soleus Muscle Surface Temperatures (°C) for the Control and Cryotherapy Conditions Before, During, and After Ice Bag Application to the Ankle Joint Complex (Mean ± SD).
DISCUSSION
Our results demonstrate that peripherally cooling the ankle's surface did not alter core body temperature. Surface cooling has previously been shown to alter core temperature, 6–8 although the methods that were used in these studies have involved various types of cold application applied to the core as opposed to the ankle. Additionally, the duration of the treatment and the type of cooling (passive versus active cooling) differed from that in our investigation. These 3 variations may help explain the differences in findings.
The application of an ice bag to a joint surface is a type of passive cold therapy. In passive cold therapy, no active cooling mechanism is used to circulate the cooling medium (eg, ice bag, cold pack). Passive cooling can be accomplished through a simple transfer of heat by application of a cold vehicle. Active cooling (eg, Game Ready Accelerated Recovery System; Game Ready Inc, Berkeley, CA) uses a dynamic method to maintain the cold temperature. The cold agent is continuously circulated to maintain the desired temperature. Active cooling methods have been shown to result in larger decreases in core temperature. 13
Probably more important than the cooling method used is the location of the cooling on the body. The body can be generally thought of as core (trunk and head) and peripheral (extremities) compartments. 14 Surface cooling has resulted in core temperature decreases when the core (ie, the trunk) is directly cooled. 6–8 A limitation of heat dissipation via the skin surface is that changes in core temperature are likely delayed because heat must be brought to the skin surface by blood from the core, cooled by conduction and convection, and then delivered back to the core tissue to cool the core. 6 When the cooling medium is applied directly to the core's surface, the distance the heat must travel is shorter and therefore would likely result in more substantial changes. Furthermore, when ice is applied to the trunk as opposed to the ankle, the surface area that is cooled is larger, which may also contribute to the difference in findings.
Another factor that we must consider when interpreting our results is the duration of the cryotherapy treatment. When active cooling measures were used and cooling was applied to the body's core, treatments longer than 20 minutes (eg, 1 hour) were necessary to cause significant drops in core temperature (>1°C). 6 7 However, other authors 9 have shown that 15 minutes of active cooling at the knee can lead to a significant decline in core temperature. We contend that even if we had applied the ice bag for 1 hour, the core temperature would not have been altered. During this time period, conductive heat gain to the ice bag may cause the ice to completely melt, resulting in increased temperature of our treatment mechanism and failure to provide the necessary cold threshold to result in core temperature changes.
Bocobo et al 9 examined the effects of ice bag and ice immersion treatments applied to the knee joint on the intra-articular and core temperatures of dogs. A 0.5°C decrease in core temperature was noted after 30 minutes of ice bag application, whereas a 1.6°C decline in core temperature was seen after only 15 minutes of ice immersion. Our findings agree with the work of Bocobo et al 9 showing that core temperature remains stable during a cryotherapy treatment applied to a joint. However, it appears that ice immersion treatments may result in a significant decline in core body temperature and thus warrant future investigation.
A decline in surface temperature after ice bag application to a joint has been previously reported in the literature. Oosterveld and Rasker 15 and Oosterveld et al 16 reported an average decline of approximately 16°C after applying ice to the knee for 30 minutes. We saw an average decline of 12.2°C in surface temperature when applying an ice bag to the ankle for 20 minutes. The slightly larger temperature decline in the 2 previous studies may be attributable to the longer treatment time. It should be mentioned that the large declines in surface temperature seen in this study are not reflective of intra-articular or muscle temperatures. Skin temperature, as altered with cryotherapy, serves as a poor predictor of intramuscular temperature 1 and does not reflect absolute intra-articular temperatures. 15–17
CONCLUSIONS
Typical 20-minute cryotherapy treatments used in the rehabilitation setting did not decrease core body temperature. Passive cooling of a joint should be used for its proven local indications.
Acknowledgments
This study was supported in part by a grant from the National Institutes of Health to the University of Virginia General Clinical Research Center, number M01RR00847. Additional support was provided by Doris Haverstack, MD, from the University of Virginia School of Medicine. We thank Danny Mistry, MD, ATC, for performing the physical examinations and James Patrice, MS, for his assistance with the statistical analysis.
REFERENCES
- Knight KL. Cryotherapy in Sport Injury Management. Champaign, IL: Human Kinetics; 1995.
- Saito N, Horiuchi H, Kobayashi S, Nawata M, Takaoka K. Continuous local cooling for pain relief following total hip arthroplasty. J Arthroplasty. 2004;19:334–337. doi: 10.1016/j.arth.2003.10.011. [DOI] [PubMed] [Google Scholar]
- Barber FA, McGuire DA, Click S. Continuous-flow cold therapy for outpatient anterior cruciate ligament reconstruction. Arthroscopy. 1998;14:130–135. doi: 10.1016/s0749-8063(98)70030-1. [DOI] [PubMed] [Google Scholar]
- Krause BA, Hopkins JT, Ingersoll CD, Cordova ML, Edwards JE. The relationship of ankle cooling and rewarming to the human soleus H reflex. J Sport Rehabil. 2000;9:1–10. [Google Scholar]
- Hopkins JT, Stencil R. Ankle cryotherapy facilitates soleus function. J Orthop Sports Phys Ther. 2002;32:622–627. doi: 10.2519/jospt.2002.32.12.622. [DOI] [PubMed] [Google Scholar]
- Plattner O, Xiong J, Sessler DI. Rapid core-to-peripheral tissue heat transfer during cutaneous cooling. Anesth Analg. 1996;82:925–930. doi: 10.1097/00000539-199605000-00006. et al. [DOI] [PubMed] [Google Scholar]
- Kurz A, Sessler DI, Birnbauer F, Illievich UM, Spiss CK. Thermoregulatory vasoconstriction impairs active core cooling. Anesthesiology. 1995;82:870–876. doi: 10.1097/00000542-199504000-00008. [DOI] [PubMed] [Google Scholar]
- Zweifler RM, Voorhees E, Mahmood MA, Parnell M. Rectal temperature reflects tympanic temperature during mild induced hypothermia in nonintubated subjects. J Neurosurg Anesthesiol. 2004;16:232–235. doi: 10.1097/00008506-200407000-00008. [DOI] [PubMed] [Google Scholar]
- Bocobo C, Fast A, Kingery W, Kaplan M. The effect of ice on intra-articular temperature in the knee of the dog. Am J Phys Med Rehabil. 1991;70:181–185. doi: 10.1097/00002060-199108000-00004. [DOI] [PubMed] [Google Scholar]
- Stocks JM, Taylor NA, Tipton MJ, Greenleaf JE. Human physiological responses to cold exposure. Aviat Space Environ Med. 2004;75:444–457. [PubMed] [Google Scholar]
- Pozos RS, Danzl DF. Human physiological responses to cold stress and hypothermia. In: Lounsbury DE, Bellamy RF, eds. Medical Aspects of Harsh Environments. Vol I. Washington, DC: Department of the Army, Office of The Surgeon General; 2002:351–382 .
- Edwards B, Waterhouse J, Reilly T, Atkinson G. A comparison of the suitabilities of rectal, gut, and insulated axilla temperatures for measurement of the circadian rhythm of core temperature in field studies. Chronobiol Int. 2002;19:579–597. doi: 10.1081/cbi-120004227. [DOI] [PubMed] [Google Scholar]
- Selkirk GA, McLellan TM, Wong J. Active versus passive cooling during work in warm environments while wearing firefighting protective clothing. J Occup Environ Hyg. 2004;1:521–531. doi: 10.1080/15459620490475216. [DOI] [PubMed] [Google Scholar]
- Matsukawa T, Sessler DI, Sessler AM, Schroeder M, Ozaki M, Kurz A, Cheng C. Heat flow and distribution during induction of general anesthesia. Anesthesiology. 1995;82:662–673. doi: 10.1097/00000542-199503000-00008. [DOI] [PubMed] [Google Scholar]
- Oosterveld FG, Rasker JJ. Effects of local heat and cold treatment on surface and articular temperature of arthritic knees. Arthritis Rheum. 1994;37:1578–1582. doi: 10.1002/art.1780371104. [DOI] [PubMed] [Google Scholar]
- Oosterveld FG, Rasker JJ, Jacobs JW, Overmars HJ. The effect of local heat and cold therapy on the intraarticular and skin surface temperature of the knee. Arthritis Rheum. 1992;35:146–151. doi: 10.1002/art.1780350204. [DOI] [PubMed] [Google Scholar]
- Warren TA, McCarty EC, Richardson AL, Michener T, Spindler KP. Intra-articular knee temperature changes: ice versus cryotherapy device. Am J Sports Med. 2004;32:441–445. doi: 10.1177/0363546503258864. [DOI] [PubMed] [Google Scholar]