Abstract
Because prepubertal testis tumors are rare, their management has historically been based on experience with the more common adult testis tumors. However, recent studies highlighting the natural history of these tumors and their response to therapy have resulted in a modern management algorithm that optimizes testicular preservation and minimizes the morbidity of adjuvant therapies. Many prepubertal testis tumors are benign and can be managed with testis-sparing tumor excision. Localized malignant tumors (yolk sac tumors) may be managed with excision alone. Recurrent tumors and metastatic disease can almost always be treated successfully with platinum-based chemotherapy.
Key words: Testis tumor, Testicular cancer, Yolk sac tumor, Teratoma, Testis-sparing surgery
Testicular tumors are far more common in adults than in children. For this reason, management of pediatric testis tumors has been based on experience in adults. Indeed, testicular tumors in adults and children are similar in many ways. In both cases, the tumors usually present with a testicular mass and are initially treated with excision of the primary tumor. In both children and adults, testis tumors are particularly sensitive to platinum-based chemotherapy, which has revolutionized the management of testicular cancer throughout the age spectrum.1,2
However, there are important differences between testis tumors occurring in children and those occurring in adults. These differences involve tumor histopathology, malignant potential, and pattern of metastatic spread. The patients themselves are also dissimilar, with different concerns regarding surgical morbidity and preservation of testicular function. These differences are of enough significance to warrant a distinct approach to the treatment of prepubertal tumors.
Epidemiology
There is a bimodal age distribution for the incidence of testis tumors, with one peak occurring during the first 2 years of life and a second, larger peak occurring in young adulthood. The incidence of pediatric testis tumors is 0.5 to 2.0 per 100,000 children, accounting for 1% to 2% of all pediatric tumors.3 In 1984, Weissbach and colleagues4 reviewed the proportion of histologic types prevalent among adult and pediatric testis tumors. The investigators studied 1062 adult tumors in the Bonn registry and 1169 pediatric tumors extracted from a review of the literature. Among adults, seminomas and mixed germ cell tumors (MGCT) accounted for 89% of cases, with stromal tumors accounting for 8% and yolk sac tumors and teratomas accounting for 1% each. In contrast, 49% of pediatric tumors were yolk sac tumors, 29% were stromal, 13% were teratomas, and only 9% were seminomas or MGCT. The study included adolescents among the cases of “pediatric tumors.” However, when patients are divided along the line of puberty, virtually no prepubertal tumors are seminomas or MGCT.
Table 1 summarizes the distribution of prepubertal testis tumors (children aged <12 years) in the Prepubertal Testis Tumor Registry of the Urologic Section of the American Academy of Pediatrics.5 The majority of primary testis tumors in the registry were yolk sac tumors, followed by teratomas and stromal tumors. Because teratomas and most stromal tumors are benign in children, it would follow that fewer than two thirds of prepubertal testis tumors have malignant potential, compared with 90% of tumors in adults. It is even possible that the majority of prepubertal tumors are benign. Several single-center studies suggest that teratomas are more common than yolk sac tumors in pediatric patients; however, these studies were not limited to prepubertal patients.6–9
Table 1.
Distribution of Tumor Types in the Prepubertal Testis Tumor Registry of the Urologic Section of the American Academy of Pediatrics
| Tumor Type | No. of Patients (%) |
|---|---|
| Germ cell | |
| Yolk sac | 244 (62) |
| Teratoma/epidermoid cyst | 105 (26) |
| Stromal | |
| Leydig cell | 5 (1) |
| Sertoli cell | 10 (3) |
| Juvenile granulosa cell | 11 (3) |
| Unspecified stromal | 16 (4) |
| Other | |
| Gonadoblastoma | 4 (1) |
Data from Ross JH et al. J Urol. 2002;168:1675–1679.5
Evaluation
The majority of patients with testis tumors present with a testicular mass noted by the patient, a parent, or a health care provider. These masses are typically hard and painless and must be distinguished from extratesticular masses, such as epididymal cysts. When the physical examination is equivocal, ultrasound is an excellent tool for distinguishing intratesticular from extratesticular masses. Although ultrasound cannot reliably distinguish malignant from benign testicular tumors, cystic tumors are more likely to be benign. On occasion, a patient will present with a hydrocele. Because hydroceles are common in children and tumors are rare, most prepubertal patients with a hydrocele do not have a tumor. However, if a child presents with a hydrocele and the testis cannot be easily palpated, ultrasound should be performed.
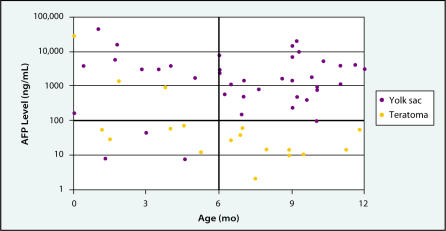
Tumor markers typically used in the evaluation and management of adult testis tumors include human chorionic gonadotropin (HCG) and α-fetoprotein (AFP). Although HCG is elaborated in a significant number of MGCT, this tumor type is vanishingly rare in prepubertal patients. Therefore, HCG is not a helpful marker in the prepubertal population. On the other hand, AFP levels are elevated in 90% of patients with yolk sac tumors and can be helpful in the preoperative distinction between yolk sac and other tumors (almost all of which are benign). One caveat is that AFP levels are quite high in healthy infants. Although highly variable, AFP levels are approximately 50,000 ng/mL in newborns, dropping to 10,000 ng/mL by age 2 weeks, 300 ng/mL by age 2 months, and 12 ng/mL by age 6 months.10 Therefore, AFP levels among patients with yolk sac tumors and benign tumors overlap during the first 6 months of life, making AFP less helpful in distinguishing tumor types in young infants (Figure 1).11
Figure 1.
α-Fetoprotein (AFP) levels for infants with teratomas or yolk sac tumors in the Prepubertal Testis Tumor Registry of the Urologic Section of the American Academy of Pediatrics. Adapted from Ross JH et al. J Urol. 2002;168:1675–1679.5
Because many, if not most, prepubertal tumors are benign, the metastatic evaluation may be deferred until a histologic diagnosis of the primary tumor is obtained. A preoperative metastatic evaluation may be undertaken in patients older than 6 months who have elevated AFP levels and likely harbor yolk sac tumors. Metastases from yolk sac tumors typically occur in the lungs and retroperitoneal lymph nodes. A chest x-ray or computerized tomography (CT) scan, as well as an abdominal CT scan, should be obtained, and postoperative AFP levels should be followed. The half-life of AFP is approximately 5 days. Failure of an elevated AFP to decline as expected after removal of the primary tumor is attributed to persistent metastatic disease.
Surgical Management
One of the major paradigm shifts in the management of prepubertal testis tumors involves the management of the primary tumor. Except for tumors in children older than 6 months with elevated AFP levels (who most likely harbor yolk sac tumors), the initial surgical management of a prepubertal testis tumor is excisional biopsy with frozen section analysis. This strategy is supported by the fact that, compared with adult tumors, for which inguinal orchiectomy is standard surgical management, a high percentage of prepubertal tumors are benign. In addition, the desire to preserve testicular tissue may be more compelling in a child who has yet to experience puberty.
The exploration is accomplished through an inguinal incision with occlusion of the testicular vessels. If the frozen section reveals a likely malignancy, the entire testis is removed. If a benign histology is confirmed (usually teratoma), the remaining testis is closed with chromic suture and returned to the scrotum. Concerns regarding testis-sparing surgery have been allayed by recent studies investigating the malignant potential of the surrounding tissue in testes harboring a teratoma. In adults, 88% of testes with a teratoma harbor carcinoma in situ (CIS) elsewhere in the testis. In studies of prepubertal teratomas, with the exception of 1 case, no such finding has been evident.12–14
Rushton and colleagues13 reviewed the histopathology of 17 testes removed because of teratomas. No multifocal tumor or CIS was found in any specimen. In initial small series of patients undergoing testis-sparing surgery for prepubertal benign tumors, there have been no cases of recurrent tumor in the preserved testicular remnants.8,9,12,13,15 In 1999, Sugita and colleagues9 reported on 27 patients with teratomas, 17 of whom underwent partial orchiectomy. With a mean follow-up of 10 years, there were no recurrences and no cases of testicular atrophy. In these studies, testes undergoing testis-sparing tumor excision appeared to maintain normal testicular volume postoperatively.
Another change in the management of prepubertal testis tumors has been a shift away from retroperitoneal lymph node dissection (RPLND), which was once a standard component of treatment.16–18 The rationale for this dissection in select adult patients is the likelihood of retroperitoneal disease and the ability to avoid the morbidity of chemotherapy. Several characteristics of prepubertal tumors argue against the use of RPLND in children. Approximately 80% of prepubertal patients with testis tumors have clinical stage I disease (disease limited to the testis and completely excised) and, with observation alone, the recurrence rate for these patients is approximately 20%. In addition, nearly all recurrences can be salvaged with chemotherapy. Among prepubertal patients with metastatic disease, a minority have disease limited to the retroperitoneum19; the majority have disease in the chest (with or without retroperitoneal disease).
Finally, the morbidity associated with abdominal surgery is greater for children than for adults. Children have a particularly high rate of postoperative bowel obstruction. In addition, it is unclear whether a nerve-sparing approach is technically feasible in small children. For prepubertal testis tumors, RPLND is limited to patients with persistent retroperitoneal masses following chemotherapy—an extremely rare occurrence.
Adjuvant Therapy for Yolk Sac Tumors
As with most malignancies, adjuvant therapy for yolk sac tumors is based on tumor stage. Various cancer study groups employ different staging systems. In most cases, the staging systems are designed for all pediatric malignant germ cell tumors, of which testis tumors comprise only a small percentage. In all series, the number of patients with metastatic testis tumors has been small, making it impossible to delineate response rates and tumor behavior based on the extent of metastatic disease. Indeed, in large studies, all metastatic testis tumors are treated the same, regardless of the degree of metastatic disease. Therefore, the important distinction among testis tumors is between stage I disease and tumors with any degree of residual or metastatic disease.
The majority of patients with prepubertal testis tumors present with stage I disease—80% in the Prepubertal Testis Tumor Registry.5 Recent studies suggest that these patients can be safely managed with observation, followed by chemotherapy for patients whose tumors recur.20–25 The United Kingdom Children’s Cancer Study Group recently reported its results employing observation for stage I yolk sac tumor of the testis and platinum-based chemotherapy (etoposide, carboplatin, and bleomycin) for metastatic disease.20 Of 51 stage I tumors, 11 (22%) recurred, all of which were cured with chemotherapy. Twenty-two patients had radiographic evidence of metastatic disease or persistently elevated AFP levels following orchiectomy; all were cured with chemotherapy.
The potential toxicities of chemotherapy include myelosuppression, ototoxicity, renal toxicity from platinum-based agents, and pulmonary toxicity from bleomycin. In the United Kingdom study, which utilized carboplatin rather than cisplatin, high-grade ototoxicity was rare, occurring in only 2 of the 137 patients with malignant germ cell tumors treated with this protocol. However, carboplatin is more myelotoxic, and high-grade myelotoxicity was common in this study, although no patient died as a result. No significant renal toxicity occurred.20
The German Society of Pediatric Oncology reported treatment results of 110 testicular yolk sac tumors.21 A total of 105 patients had stage I disease, 91 of whom initially received orchiectomy alone. Fourteen (15%) of these 91 patients had tumor recurrence. These 14 patients, along with 5 patients who had metastases at presentation, received 4 cycles of vinblastine, bleomycin, and cisplatin. All patients with recurrent stage I disease were cured, as were 4 of the 5 patients with metastatic disease. The overall cure rate was 99%. There were no cases of pulmonary toxicity or ototoxicity.21
A study conducted by the US Pediatric Intergroup (now the Children’s Oncology Group) reported results of treatment in 65 patients with stage I disease and 14 patients with limited metastatic disease (microscopic residual disease, retroperitoneal lymphadenopathy <2 cm, and/or persistent tumor marker elevation).22 Patients with stage I disease received orchiectomy alone, and 11 (18%) of these patients had tumor recurrence. All 11 patients with recurrent disease, as well as the 14 patients with metastatic disease, were successfully treated with 4 cycles of cisplatin, etoposide, and bleomycin.
A summary of these 3 studies is presented in Table 2. Clearly, the outlook for prepubertal yolk sac tumors is excellent. Stage I tumors are best managed with orchiectomy and observation. Observation should include frequent chest and abdominal imaging and measurement of AFP levels. Patients with recurrent disease or metastases at presentation can expect excellent results with platinum-based multiagent chemotherapy. Future studies will focus on reducing the morbidity for patients requiring chemotherapy by reducing the number of agents and/or cycles of therapy administered.
Table 2.
Results of 3 Large Multicenter Studies of Pediatric Testis Tumors
| Patients | Recurrence Rate | Survival | Survival of Patients | ||
|---|---|---|---|---|---|
| No. of | With Stage I | of Stage I Tumors | for Stage I | With Residual | |
| Study | Patients | Tumors, % | on Observation, % | Tumors, % | Disease/Metastases, % |
| United Kingdom Children’s | 73 | 70 | 22 | 100 | 100 |
| Cancer Study Group20 | |||||
| German Cooperative Studies21 | 110 | 95 | 15 | 100 | 80 |
| US Pediatric Intergroup Study22 | 79 | 82 | 18 | 100 | 100 |
| Total, average | 262 | 84 | 17 | 100 | 98 |
Teratomas and Epidermoid Cysts
Teratomas are the most common benign tumors in prepubertal patients. The median age of prepubertal teratoma presentation is 13 months, with several cases reported as presenting during the neonatal period.11,26 Histologically, teratomas consist of tissues representing the 3 germinal layers: endoderm, mesoderm, and ectoderm. Epidermoid cysts are benign tumors composed entirely of keratin-producing epithelium. They are to be distinguished from dermoid cysts, which contain skin and skin appendages, and from teratomas, which contain derivatives of other germ cell layers. Teratomas and epidermoid cysts are universally benign in prepubertal children.
As previously discussed, testis-sparing surgery is a reasonable consideration for prepubertal patients with teratomas or epidermoid cysts (Figure 2).12,13 Frozen sections should be obtained to confirm the diagnosis. In older children with teratomas, surrounding testicular parenchyma must be carefully evaluated. If there is histologic evidence of pubertal changes, an orchiectomy should be performed, because teratomas are potentially malignant in postpubertal males. Biopsies of surrounding testicular parenchyma are probably not necessary in prepubertal patients.13,14,27 Although 88% of testes removed for adult teratoma contain areas of intratubular germ cell neoplasia, this has generally not been the case for epidermoid cysts or for pediatric teratomas.
Figure 2.
Testis-sparing surgery for a large benign cystic tumor: (A) incision in the testicle with the cord occluded through an inguinal incision; (B) cyst enucleation; (C) closed testicular remnant, which will be replaced in the scrotum.
For patients with epidermoid cysts and prepubertal patients with teratomas, no radiographic studies or follow-up for the development of metastatic disease is required. Because of the potential for malignancy, postpubertal patients with teratomas should be evaluated and followed on the same protocol as adults with potentially malignant germ cell tumors.
Gonadal Stromal Tumors
Stromal tumors include Leydig cell, Sertoli cell, juvenile granulosa, and mixed or undifferentiated tumors. Stromal testis tumors are rare in children, and there are no large series to guide their management. However, anecdotal reports and small series in the literature offer some experience on which to base therapy.28
Leydig Cell Tumors
Leydig cell tumors are universally benign in children.3,28 They usually present in children aged 5 to 10 years with precocious puberty. Most patients present with virilization. Although feminization (particularly gynecomastia) is common in adults, it is a rare occurrence in children and, when present, is usually superimposed on the virilizing signs. Persistence of androgenic effects following excision may be due to a contralateral tumor, but this is uncommon in children. Because Leydig cell tumors are sometimes difficult to detect on physical examination, an ultrasound may be necessary to rule out a contralateral tumor.
Leydig cell tumors may be treated with testis-sparing excision. However, even after successful removal of a solitary tumor, androgenic changes are not completely reversible, and some children may proceed through premature puberty due to activation of the hypothalamic-pituitary-gonadal axis.
Sertoli Cell Tumors
Sertoli cell tumors account for only 2% of primary prepubertal testis tumors. They are usually well circumscribed and often lobulated. Cysts are common. A review of 60 cases of Sertoli cell tumors reported only 4 cases in patients younger than 20 years—the youngest patient being age 15 years.29 Approximately 10% of adult Sertoli cell tumors are malignant. The median age of patients with Sertoli cell tumors in the Prepubertal Testis Tumor Registry was 6 months, with a range of 4 months to 10 years.28 There were no reports of metastatic disease. Sertoli cell tumors are usually hormonally inactive in children, although they may occasionally cause gynecomastia or isosexual precocious puberty. Although all reported cases to date in children younger than 5 years have been benign, there have been a few cases of malignant Sertoli cell tumors in older children.30,31
Orchiectomy is sufficient treatment of Sertoli cell tumor in infants; however, a metastatic evaluation could be considered for infants in whom histologic findings are worrisome. Older children should undergo abdominal CT and chest x-ray to rule out metas-tases. When metastatic disease is present, aggressive combination treatment including RPLND, chemotherapy, and radiation therapy should be considered.
The large-cell calcifying Sertoli cell tumor is a clinically and histologically distinct entity, with a higher incidence of multifocality and hormonal activity.3,32,33 These tumors are composed of large cells with abundant cytoplasm and varying degrees of calcification, ranging from minimal amounts to massive deposits. Whereas standard Sertoli cell tumors are more common in adults, large-cell calcifying Sertoli cell tumors are found predominantly in children and adolescents. Most patients present with a testicular mass. Approximately one fourth of patients have bilateral and multifocal tumors. The presence of calcifications results in a characteristic ultrasound appearance with multiple hyperechoic areas. Approximately one third of patients with large-cell calcifying Sertoli cell tumors have an associated genetic syndrome and/or endocrine abnormality. Although occasionally malignant in adults, large-cell calcifying Sertoli cell tumors have been universally benign in patients younger than 25 years. Orchiectomy is sufficient treatment in children.
Juvenile Granulosa Cell Tumor
Testicular juvenile granulosa cell tumors are stromal tumors bearing a light microscopic resemblance to ovarian juvenile granulosa cell tumors. However, the histologic origin of this tumor in the testes is unclear. Granulosa cell tumors occur almost exclusively in the first year of life and most often in the first 6 months. Of 22 tumors in newborns in the Prepubertal Testis Tumor Registry, 6 were juvenile granulosa cell tumors, 6 were yolk sac tumors, and 6 were unspecified stromal tumors.26 Structural abnormalities of the Y chromosome and mosaicism are common in boys with juvenile granulosa cell tumors.30 Several cases have been described in association with ambiguous genitalia.34 These tumors are hormonally inactive and benign. Although these children should undergo chromosomal analysis, no treatment or metastatic evaluation is required beyond excision.28
Mixed or Undifferentiated Tumors
Histologically mixed or undifferentiated stromal tumors consist of areas of gonadal stromal neoplasia and undifferentiated regions of spindle cells, which may exhibit a high mitotic rate. These stromal tumors have an epidemiology similar to that of granulosa cell tumors.28 Although some of these tumors have histologic characteristics commonly associated with malignancy, most are benign.
There are inadequate data in the literature to formulate rigid guidelines for managing patients with mixed or undifferentiated tumors. Histologic features do not appear to correlate with invasive or metastatic potential. Although aggressive behavior has not been documented in young infants, there are reports of such behavior in older children. Because orchiectomy cures most of these patients, RPLND and adjuvant therapy are probably not appropriate in the absence of radiographic evidence of metastatic disease. However, given the uncertainty, postoperative evaluation and follow-up for the development of metastatic disease seems prudent.
Summary
Prepubertal testis tumors are distinct from their adult counterparts in their histology and natural history. Over the past 2 decades, studies have highlighted these differences and resulted in a distinct management approach to prepubertal patients. Except when preoperative AFP levels are consistent with a yolk sac tumor, most patients should undergo an excisional biopsy with frozen section. If a benign tumor is found, the testicular remnant should be closed and replaced in the scrotum. If a yolk sac tumor is found, an orchiectomy should be performed. Most yolk sac tumors are limited to the testis and may be followed closely without adjuvant therapy. The 15% to 20% of patients with recurrent disease, as well as those who present with metastatic disease, can nearly all be cured with platinum-based chemotherapy.
Teratomas, epidermoid cysts, and most stromal tumors are benign and may be released from oncologic follow-up. Older patients with Sertoli cell tumors and patients with undifferentiated stromal tumors should undergo metastatic evaluation. With modern management, many prepubertal patients with testis tumors can retain their affected testis, and even the majority of patients with yolk sac tumors can avoid the morbidity of chemotherapy and RPLND without sacrificing a nearly 100% cure rate.
Main Points.
There are important differences between testis tumors occurring in children and those occurring in adults. These differences, which involve tumor histopathology, malignant potential, and pattern of metastatic spread, are of enough significance to warrant a distinct approach to the treatment of prepubertal tumors.
In the Prepubertal Testis Tumor Registry of the Urologic Section of the American Academy of Pediatrics, the majority of primary testis tumors were yolk sac tumors, followed by teratomas and stromal tumors. Because teratomas and most stromal tumors are benign in children, it would follow that fewer than two thirds of prepubertal testis tumors have malignant potential, compared with 90% of tumors in adults.
Except for tumors in children older than 6 months with elevated α-fetoprotein levels (who most likely harbor yolk sac tumors), the initial surgical management of a prepubertal testis tumor is excisional biopsy with frozen section analysis.
Stage I tumors are best managed with orchiectomy and observation. Patients with recurrent disease or metastases at presentation can expect excellent results with platinum-based multiagent chemotherapy.
For patients with epidermoid cysts and prepubertal patients with teratomas, no radiographic studies or follow-up for the development of metastatic disease is required. Because of the potential for malignancy, postpubertal patients with teratomas should be evaluated and followed on the same protocol as adults with potentially malignant germ cell tumors.
References
- 1.Einhorn LH, Williams SD. Chemotherapy of disseminated testicular cancer. Cancer. 1980;46:1339–1344. doi: 10.1002/1097-0142(19800915)46:6<1339::aid-cncr2820460607>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 2.Flamant F, Baranzelli MD, Kalifa C, Lemerle J. Treatment of malignant germ cell tumors in children: experience of the Institut Gustave Roussy and the French Society of Pediatric Oncology. Crit Rev Oncol Hematol. 1990;10:99–110. doi: 10.1016/1040-8428(90)90002-a. [DOI] [PubMed] [Google Scholar]
- 3.Coppes MJ, Rackley R, Kay R. Primary testicular and paratesticular tumors of childhood. Med Pediatr Oncol. 1994;22:329–340. doi: 10.1002/mpo.2950220506. [DOI] [PubMed] [Google Scholar]
- 4.Weissbach L, Altwein JE, Stiens R. Germinal testicular tumors in childhood. Eur Urol. 1984;10:73–85. doi: 10.1159/000463762. [DOI] [PubMed] [Google Scholar]
- 5.Ross JH, Rybicki L, Kay R. Clinical behavior and a contemporary management algorithm for prepubertal testis tumors: a summary of the Prepubertal Testis Tumor Registry. J Urol. 2002;168:1675–1679. doi: 10.1097/01.ju.0000030749.27823.f5. [DOI] [PubMed] [Google Scholar]
- 6.Rushton HG, Belman AB. Testis-sparing surgery for benign lesions of the prepubertal testis. Urol Clin North Am. 1993;20:27–37. [PubMed] [Google Scholar]
- 7.Farivar-Mohseni H, Bagli DJ, McLorie G, et al. Prepubertal testicular and paratesticular tumours. J Urol. 1996;155(suppl):392A. [Google Scholar]
- 8.Shukla AR, Woodard C, Carr MC, et al. Testicular teratoma at the Children’s Hospital of Philadelphia: the role of testis preserving surgery. J Urol. 2002;167(suppl):109. [Google Scholar]
- 9.Sugita Y, Clarnette TD, Cooke-Yarborough CC, et al. Testicular and paratesticular tumours in children: 30 years’ experience. Aust N Z J Surg. 1999;69:505–508. doi: 10.1046/j.1440-1622.1999.01612.x. [DOI] [PubMed] [Google Scholar]
- 10.Wu JT, Book IL, Sudar K. Serum alpha-fetoprotein (AFP) levels in normal infants. Ped Res. 1981;15:50–52. doi: 10.1203/00006450-198101000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Grady R, Ross JH, Kay R. Epidemiological features of testicular teratoma in a prepubertal population. J Urol. 1997;158(3 pt 2):1191–1192. doi: 10.1097/00005392-199709000-00129. [DOI] [PubMed] [Google Scholar]
- 12.Ross JH, Kay R, Elder J. Testis sparing surgery for pediatric epidermoid cysts of the testis. J Urol. 1993;149:353–356. doi: 10.1016/s0022-5347(17)36080-9. [DOI] [PubMed] [Google Scholar]
- 13.Rushton HG, Belman AB, Sesterhenn I, et al. Testicular sparing surgery for prepubertal teratoma of the testis: a clinical and pathological study. J Urol. 1990;144:726–730. doi: 10.1016/s0022-5347(17)39567-8. [DOI] [PubMed] [Google Scholar]
- 14.Renedo DE, Trainer TD. Intratubular germ cell neoplasia (ITGCN) with p53 and PCNA expression and adjacent mature teratoma in an infant testis. Am J Surg Pathol. 1994;18:947–952. doi: 10.1097/00000478-199409000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Pearse BI, Glick RD, Abramson SJ, et al. Testicular-sparing surgery for benign testicular tumors. J Pediatr Surg. 1999;34:1000–1003. doi: 10.1016/s0022-3468(99)90777-7. [DOI] [PubMed] [Google Scholar]
- 16.Fernandes ET, Etcubanas E, Rao BN, et al. Two decades of experience with testicular tumors in children at St Jude Children’s Research Hospital. J Pediatr Surg. 1989;24:677–682. doi: 10.1016/s0022-3468(89)80718-3. [DOI] [PubMed] [Google Scholar]
- 17.Hopkins TB, Jaffe N, Colodny A, et al. The management of testicular tumors in children. J Urol. 1978;120:96–102. doi: 10.1016/s0022-5347(17)57058-5. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan WE, Firlit CF. Treatment of testicular yolk sac carcinoma in the young child. J Urol. 1981;126:663–664. doi: 10.1016/s0022-5347(17)54681-9. [DOI] [PubMed] [Google Scholar]
- 19.Grady RW, Ross JH, Kay R. Patterns of metastatic spread in prepubertal yolk sac tumor of the testis. J Urol. 1995;153:1259–1261. [PubMed] [Google Scholar]
- 20.Mann JR, Raafat F, Robinson K, et al. The United Kingdom Children’s Cancer Study Group’s second germ cell tumor study: carboplatin, etoposide, and bleomycin are effective treatment for children with malignant extracranial germ cell tumors, with acceptable toxicity. J Clin Oncol. 2000;18:3809–3818. doi: 10.1200/JCO.2000.18.22.3809. [DOI] [PubMed] [Google Scholar]
- 21.Haas RJ, Schmidt P, Gobel U, Harms D. Testicular germ cell tumors: an update—results of the German Cooperative Studies 1982–1997. Klinische Padiatrie. 1999;211:300–304. doi: 10.1055/s-2008-1043804. [DOI] [PubMed] [Google Scholar]
- 22.Giller R, Cushing B, Marina N, et al. Outcome of surgery alone or surgery plus cisplatin/etoposide/bleomycin (PEB) for localized gonadal malignant germ cell tumors (MGCT) in children: a Pediatric Intergroup report (CCG8891/POG9048) [abstract] Med Ped Oncol. 1997;29:413. [Google Scholar]
- 23.Lo Curto M, D’Angelo P, Arrighini A, et al. Malignant germ cell tumours in childhood: the Italian experience. In: Jones WG, Appleyard I, Harnden P, Joffe JK, et al., editors. Germ Cell Tumours IV. London: John Libbey & Co Ltd; 1998. pp. 227–231. [Google Scholar]
- 24.Baranzelli MC, Patte C. The French experience in paediatric malignant germ cell tumours. In: Jones WG, Appleyard I, Harnden P, Joffe JK, editors. Germ Cell Tumours IV. London: John Libbey & Co Ltd; 1998. pp. 219–226. [Google Scholar]
- 25.Lin JN, Wang KL, Hung IJ, Yang CP. Management of yolk sac tumor of the testis in children. J Formos Med Assoc. 1994;93:393–396. [PubMed] [Google Scholar]
- 26.Levy D, Kay R, Elder J. Neonatal testis tumors: a review of the prepubertal testis tumor registry. J Urol. 1994;151:715–717. doi: 10.1016/s0022-5347(17)35068-1. [DOI] [PubMed] [Google Scholar]
- 27.Reinberg Y, Manivel JC, Llerena J, et al. Epidermoid cyst (monodermal teratoma) of the testis. Br J Urol. 1990;66:648–651. doi: 10.1111/j.1464-410x.1990.tb07202.x. [DOI] [PubMed] [Google Scholar]
- 28.Thomas JC, Ross JH, Kay R. Stromal testis tumors in children: a report from the prepubertal testis tumor registry. J Urol. 2001;166:2338–2340. doi: 10.1016/s0022-5347(05)65583-8. [DOI] [PubMed] [Google Scholar]
- 29.Young RH, Koelliker DD, Scully RE. Sertoli cell tumors of the testis, not otherwise specified: a clinicopathologic analysis of 60 cases. Am J Surg Pathol. 1998;22:709–721. doi: 10.1097/00000478-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Cortez JC, Kaplan GW. Gonadal stromal tumors, gonadoblastomas, epidermoid cysts, and secondary tumors of the testis in children. Urol Clin North Am. 1993;20:15–26. [PubMed] [Google Scholar]
- 31.Kolon TF, Hochman HI. Malignant Sertoli cell tumor in a prepubescent boy. J Urol. 1997;158:608–609. [PubMed] [Google Scholar]
- 32.Niewenhuis JC, Wolf MC, Kass EJ. Bilateral asynchronous Sertoli cell tumor in a boy with the Peutz-Jeghers syndrome. J Urol. 1994;152:1246–1248. doi: 10.1016/s0022-5347(17)32560-0. [DOI] [PubMed] [Google Scholar]
- 33.Proppe KH, Scully RE. Large-cell calcifying Sertoli cell tumor of the testis. Am J Clin Pathol. 1980;74:607–619. doi: 10.1093/ajcp/74.5.607. [DOI] [PubMed] [Google Scholar]
- 34.Young RH, Lawrence WD, Scully RE. Juvenile granulosa cell tumor—another neoplasm associated with abnormal chromosomes and ambiguous genitalia, a report of three cases. Am J Surg Pathol. 1985;9:737–743. doi: 10.1097/00000478-198510000-00005. [DOI] [PubMed] [Google Scholar]