Abstract
Objective. To describe patterns of vision care among Medicaid-enrolled children.
Methods. We evaluated claims data over a 1-year period among children who were 18 years and younger, living in Michigan, and continuously enrolled in Medicaid but did not have a complex medical condition or were disabled. For this study, vision care comprised eye care services provided by optometrists or ophthalmologists and lens services, including dispensing and fitting of corrective lenses.
Results. Children in rural counties had increased odds of receiving eye care (odds ratio [OR]: 1.24) or lens services (OR: 1.22) compared with those in urban counties. In urban counties, non-Hispanic white children had greater odds than Hispanic or nonwhite children to have eye care (OR: 1.37) and lens services (OR: 1.37). An increasing supply of eye care professionals per population within a county was associated with decreased vision care in urban counties and slightly increased eye care and no changes in lens services in rural counties. Urban children who received mostly fee-for-service Medicaid had greater odds of receiving vision care than those with longer periods of managed care. Rural children who received mostly fee-for-service Medicaid had greater odds of eye care but similar odds of lens services. Regardless of urban/rural status, girls had increased odds of receiving eye care (OR: 1.24 for urban, 1.20 for rural) and lens services (OR: 1.36 for urban, 1.24 for rural).
Conclusions. Patterns emerged that suggest underutilization or overutilization of vision care services. Such differences may have an impact on the development of children or waste limited health care resources.
Visual impairment, including refractive error, is common, affecting as many as 20% of all children.1 Although the impact of uncorrected visual impairment on educational attainment is unclear,2 professional groups advocate routine screening.3-6
Little is known about the current delivery of vision care services for children, including diagnostic evaluation by optometrists and ophthalmologists or the dispensing of corrective lenses. Understanding patterns of vision care, including factors associated with the receipt of such care, is important in ensuring optimal delivery of services for children. However, interpreting data regarding the delivery of vision care is challenging because there is no accepted “gold standard” for determining when treatment is required, and there are important variations in practice among optometrists and ophthalmologists in both diagnostic and treatment strategies.7-9 As a result, there is debate regarding the true prevalence of visual impairment and the threshold at which corrective lenses should be prescribed.10
Although few data are available regarding the prevalence of visual impairment among children, recent evidence suggests that the prevalence of visual impairment among children varies by race/ethnicity.10 For example, black and white children had a lower prevalence of myopia than did Asian or Hispanic children. In contrast, white children had the highest prevalence of hyperopia and Asian and Hispanic children had the highest prevalence of astigmatism. This study also found that girls were more likely than boys, regardless of race/ethnicity, to have visual impairment. Unfortunately, these data cannot be used to predict the overall prevalence of correctable visual impairment because data were collected only about each child’s right eye, which would underestimate certain types of visual impairment (eg, amblyopia, anisometropia). Furthermore, the definitions of the various types of visual impairment were not based on an accepted clinical standard, as none exists, and these definitions were not linked to treatment or outcome. Finally, the generalizability of these results may be limited by volunteer bias or by clustering because study population was recruited at 4 locations across the country, each of which targeted children of a specific race/ethnicity.
There is evidence to suggest that variation in the underlying prevalence of visual impairment is not solely responsible for differences in the receipt of vision care services. In previous work using national data sets, we found variations in the receipt of vision care by race/ethnicity, modified by health insurance status.11,12 Black or Hispanic children had lower odds of receiving care from an optometrist or an ophthalmologist than non-Hispanic/nonblack children, regardless of age, gender, family income, or health insurance status. We also found that uninsured black or Hispanic children had lower odds than uninsured nonblack/non-Hispanic children to have corrective lenses. However, black or Hispanic children with public or private insurance had similar odds as non-Hispanic/nonblack children of having corrective lenses. This suggested that financial access to care is important in overcoming barriers to the correction of visual impairment.
With those findings in mind, we hypothesized that financial access to vision services and the availability of optometrists and ophthalmologists within a community are key factors in the receipt of eye care or corrective lenses. We also hypothesized that with financial access barriers absent, racial/ethnic differences in the receipt of eye care or use of corrective lenses could be explained by the availability of eye care and other demographic factors, including age, gender, and rural/urban residency.
We based our evaluation of these hypotheses on an insured population of children with a uniform vision care benefit, allowing us to control for variability in financial access. We used administrative claims and utilization data from the Michigan Medicaid program, which provides coverage for evaluation and treatment by optometrists and ophthalmologists as well as corrective lenses and services by optometrists, ophthalmologists, and corrective lens suppliers. Our focus on Michigan is intended to minimize bias as a result of variability in children’s access to initial vision screening services, which may be an important pathway to subsequent vision care services. Vision screening by trained screening technicians is offered to all children in Michigan within both public and private schools beginning in first grade and ending in either 11th grade or driver education classes.13
METHODS
Data Source
We based our study on a retrospective analysis of Michigan Medicaid administrative claims data for services furnished during calendar year 2001. Data were obtained from Medicaid program enrollment files and vision services claims from all Medicaid fee-for-service and managed care plans; both types of plans provide the same type of claims data to the state. Demographic data and enrollment status were obtained from Medicaid program enrollment files and included date of birth, gender, race/ethnicity, and county of residence. In addition, population counts for all residents were obtained by county.14 This study was approved by the University of Michigan Medical School Institutional Review Board.
Subjects
Children 18 years of age and younger in 2001 were included in this analysis. Several inclusion/exclusion criteria were applied to derive our study sample. A total of 831 978 children 18 years of age and younger were enrolled in the Michigan Medicaid program for at least 1 month during calendar year 2001. We included children with continuous Medicaid enrollment to minimize the likelihood of incomplete administrative claims data. To be considered continuously enrolled, children older than 1 year were required to have at least 11 months of Medicaid enrollment in 2001, whereas those younger than 1 year were required to be enrolled for all months in 2001. As a result, we excluded 353 870 (42.5%) children with discontinuous Medicaid enrollment. We also excluded children with disabilities and complex medical conditions because of their greater likelihood of receiving intensive vision care services. Children with disabilities or complex medical conditions were identified on the basis of enrollment in the state’s Children With Special Health Care Needs (Title V) program or in the Supplemental Security Income program. Although this strategy would not identify all children with chronic illness, such as moderate persistent asthma, it would identify those with increased need for vision care, such as those with retinopathy of prematurity or with juvenile rheumatoid arthritis. Of the 478 108 children were 18 years and younger and were continuously enrolled in Medicaid, 10 364 (2.2%) children were receiving services through the Children With Special Health Care Needs program, and 31 764 (6.6%) children were receiving services through Supplemental Security Income programs (5604 children were enrolled in both programs). Consequently, a total of 36 524 children with disabilities or complex medical conditions were excluded, which yielded our study sample of 441 584 children (53.1% of the initial population).
Outcomes Measured
The main outcome of this study was the receipt over a 1-year period of vision care, which we divided into eye care and lens services, on the basis of procedure codes reported on the administrative claims (a detailed listing of codes is available from the authors on request). Eye care included services for any eye examination by an optometrist or ophthalmologist, refraction, any office/outpatient visit or consultation with an optometrist or ophthalmologist, strabismus surgery, or vision training. Emergency services, such as ocular wound repair, was not included. Surgery performed by ophthalmologists but not directly related to vision care, such as nasolacrimal duct surgery, was not included. Lens services included claims for dispensing corrective lenses or frames or any procedure code for fitting of corrective lenses. These lens services could be provided by optometrists, ophthalmologists, or vision services providers, who are licensed to dispense and fit corrective lenses but do not prescribe lenses or provide other eye care. There were a total of 363 187 vision care service claims for children in the study population. The rate of vision care use during the study year was defined as the proportion of children with 1 or more claims.
Independent Variables
Independent variables from the Medicaid database included age, gender, race/ethnicity, address, and a classification of Medicaid insurance type on the basis of the number of months enrolled in either Medicaid managed care or fee-for-service plans. Race/ethnicity was categorized as Hispanic or nonwhite and non-Hispanic white. Each child was classified as living in an urban or a rural county on the basis of whether his or her county of residence included a metropolitan statistical area, as defined by the US Census Bureau.15 Using this definition, 26 counties were designated as urban with the remaining 57 counties being classified as rural areas. Medicaid insurance type was categorized as mostly managed care (managed care ≥9 months), mostly fee-for-service (fee-for-service ≥9 months), or mixed fee-for-service/managed care.
The concentration of eye care providers in each county was also included as an independent variable. This was determined by adding the number of optometrists licensed in each county in 2001, provided by the Michigan Department of Consumer and Industry Services, to the number of ophthalmologists in each county in 2001, from the Area Resource File,16 and dividing by the population size, according to the 2000 census.17 The calculated concentration may under- or overestimate the availability of eye care to an individual within each county because of variations in the availability of individual eye care providers, some providers practice within >1 county, and individuals may cross into another county for eye care. We therefore categorized counties on the basis of the overall supply of eye care within the state to low (<25th percentile), medium (25th-75th percentile), and high (>75th percentile) supply.
Statistical Analysis
We first evaluated the relationship between each individual independent variable and the outcome measures using Pearson χ2 tests of independence. Logistic regression modeling was used to determine the relative association between each significant independent variable and each of the outcome measures. For ensuring that the analyses are robust and not biased by care provided within the most populous county (Wayne), which includes a major urban center (Detroit), a sensitivity analysis was performed in which the logistic regression models were reanalyzed without data from this county. All findings from the regression modeling are reported as odds ratios (ORs) and their 95% confidence intervals (CIs). All analyses were performed using Stata 8 (Stata Corporation; College Station, TX)
RESULTS
Study Population
Table 1 summarizes the characteristics of the 441 584 continuously enrolled children in the study population. Overall, there was nearly an even distribution by race/ethnicity (46.6% non-Hispanic white, 52.4% Hispanic or nonwhite, 1% missing), and most of the children lived in urban counties (84.2%). The proportion of Hispanic or nonwhite children living in rural counties was less than in urban ones (8.9% vs 60.6%; P < .001).
TABLE 1.
Demographic Characteristics of the Study Population
| N | 441 584 |
| Age, y (mean ± SD) | 7.7 ± 5.2 |
| Gender | |
| Male | 50.1% |
| Female | 49.9% |
| Race/ethnicity | |
| Hispanic or nonwhite | 52.4% |
| Non-Hispanic white | 46.6% |
| Missing | 1.0% |
| Urban/rural status | |
| Urban | 84.2% |
| Rural | 15.8% |
| Medicaid type | |
| Mostly managed care | 12.6% |
| Mixed fee-for-service/managed care | 76.8% |
| Mostly fee-for-service | 10.7% |
| Eye care supply in county of residence | |
| Low (<25th percentile) | 5.7% |
| Medium (25th-75th percentile) | 71.3% |
| High (>75th percentile) | 23.0% |
Distribution Of Optometrists And Ophthalmologists
A total of 1254 optometrists and 576 ophthalmologists served the 9.94 million residents of Michigan during 2001. The median concentration of optometrists was 1.3 per 10 000 people and ranged from none in 10 rural counties with a total population of 134 000 to 5.2 per 10 000 people in 1 rural county with a population of 40 500. The median concentration of ophthalmologists was 0.1 per 10 000 people and ranged from none in 39 rural counties and 2 urban counties with a total population of 1.11 million people to 1.8 per 10 000 people in 1 urban county with a total population of 323 000. Each county was classified on the basis of the overall concentration of eye care providers into low supply (<25th percentile, 1.0 per 10 000 population), medium supply (between the 25th and 75th percentiles, 1.0-2.1 per 10 000 population), or high supply (>75th percentile, 2.1 per 10 000 population). Although ophthalmologists were more concentrated in urban counties (P < .001), the concentration of optometrists was not associated with urban/rural status of the county (P = .3). Similarly, the overall distribution of eye care providers was not associated with urban/rural status of the county (P = .2).
Provision of Vision Services
Overall, 8.9% of the children received vision services, including care from an optometrist or ophthalmologist and lens services (4.4%), care from an optometrist or ophthalmologist only (4.2%), and lens services only (0.4%). Most eye care was provided by optometrists alone (76.0%). The remainder of care was provided by ophthalmologists alone (19.8%) or optometrists and ophthalmologists together (4.2%).
Optometrists alone or in conjunction with vision care suppliers provided 75.7% of the lens services. Another 23.0% of the lens services were provided by ophthalmologists alone or in conjunction with vision suppliers. The remaining lens services were provided by optometrists and ophthalmologists, with or without vision care suppliers (0.4%) or by vision suppliers alone (0.9%).
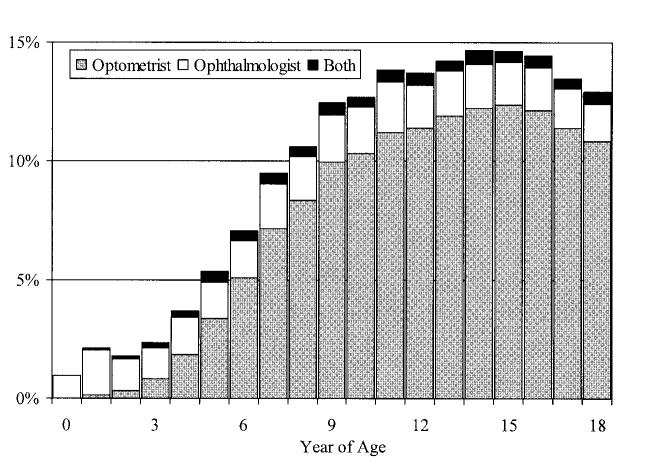
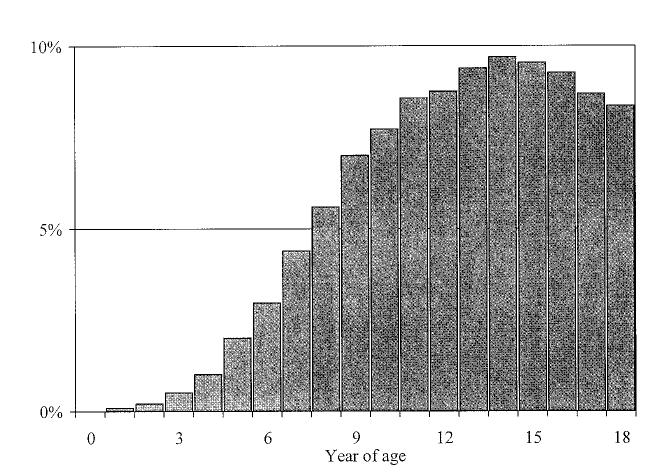
Factors Associated With the Receipt of Vision Services: Bivariate Analyses
The rate of receipt of vision services increased with age (Figs 1 and 2), except for a slight decrease in care from an optometrist or ophthalmologist for those older than 15 years compared with 15-year-olds (13.7% vs 14.6%; P = .004) and a decrease in the rate of lens services for those older than 14 years compared with 14-year-olds (9.0% vs 9.7%; P = .009). The proportion of care provided by ophthalmologists decreased with age (Fig 1). Ophthalmologists alone provided 55.3% of the care for children younger than 5 years but only 14.9% of the care for children 5 years and older (P < .001).
Fig 1.
Proportion who received eye care by year of age and by type of eye care provider.
Fig 2.
Proportion who received lens services by year of age.
Overall, the receipt of eye care and lens services was greater among girls than boys, among non-Hispanic white children than Hispanic or nonwhite children, in rural counties than urban counties, and among those who had fee-for-service Medicaid for the longest time (Table 2). Residence in an urban county was associated with the greatest overall difference in the receipt of vision services apart from age. In urban counties, non-Hispanic white children were more likely than Hispanic or nonwhite children to receive eye care (9.0% vs 7.2%; P < .001) and lens services (5.0% vs 4.0%; P < .001). However, in rural counties, there was no association between race/ethnicity and either eye care (11.8% vs 11.5%; P = .44) or lens services (6.5% vs 6.4%; P = .73).
TABLE 2.
Demographic Factors Associated With the Receipt of Vision Care Services
| Eye Care |
Lens Services |
|||
|---|---|---|---|---|
| % | P | % | P | |
| Overall (n = 441 584) | 8.5 | 4.7 | ||
| Gender | < .001 | < .001 | ||
| Male (n = 221 144) | 7.7 | 4.1 | ||
| Female (n = 220 440) | 9.3 | 5.4 | ||
| Race/ethnicity | < .001 | < .001 | ||
| Hispanic or nonwhite (n = 231 543) | 7.3 | 4.1 | ||
| Non-Hispanic white (n = 205 785) | 9.9 | 5.4 | ||
| Urban/rural residency | < .001 | < .001 | ||
| Urban (n = 371 860) | 7.9 | 4.4 | ||
| Rural (n = 69 724) | 11.8 | 6.5 | ||
| Medicaid insurance type | < .001 | = .002 | ||
| Mostly managed care (n = 55 498) | 8.5 | 4.6 | ||
| Mixed fee-for-service/managed care (n = 339 034) | 8.3 | 4.7 | ||
| Mostly fee-for-service (n = 47 052) | 10.3 | 5.0 | ||
| Eye care supply in county of residence | ||||
| Low (<25th percentile) | 11.1 | < .001 | 6.4 | < .001 |
| Medium (25th-75th percentile) | 8.3 | 4.7 | ||
| High (>75th percentile) | 8.7 | 4.5 | ||
Children in counties with a low supply of eye care specialists were more likely to receive vision services than those in counties with a medium or high supply of eye care specialists (P < .001; Table 2). In urban counties, low supply was associated with the highest receipt of eye care (low 11.0%, medium 7.8%, high 7.9%; P < .001) and lens services (low 6.4%, medium 4.4%, high 4.1%; P < .001). In contrast, in rural counties, eye care was associated with a higher supply of eye care specialists (low 11.2%, medium 11.7%, high 12.5%; P = .001), and lens services were not associated with the supply of eye care specialists (low 6.4%, medium 6.6%, high 6.4%; P = .5)
Factors Associated With the Receipt of Vision Care: Logistic Regression Analyses
Overall, rural status was associated with increased odds of vision care. Comparing rural with urban residents, the unadjusted OR was 1.56 (95% CI: 1.52-1.60) for the receipt of eye care and 1.52 (95% CI: 1.47-1.57) for lens services. When adjusted for age, gender, race/ethnicity, Medicaid insurance type, and supply of eye care providers, the OR was 1.24 (95% CI: 1.21-1.28) for the receipt of eye care and 1.22 (95% CI: 1.17-1.27) for lens services.
Because of the interaction between urban/rural status and both race/ethnicity and eye care supply, we developed separate logistic regression models for the receipt of eye care (Table 3) and lens services (Table 4) stratified by rural/urban status. After adjusting for all variables in the models, girls had greater odds than boys of receiving eye care or lens services, regardless of urban/rural status. The multivariate results were consistent with the bivariate findings related to the interaction between urban/rural location and race/ethnicity. Among children in urban counties, non-Hispanic white children had greater odds of receiving eye care and lens services. However, in rural counties, there was no association between race/ethnicity and the rate of vision care. Enrollment in fee-for-service Medicaid was associated with increased odds of vision care, although we found some differences between urban and rural children. Urban children who received mostly fee-for-service Medicaid had greater odds of receiving all forms of vision care than those with longer periods of managed care, whereas their rural counterparts had greater odds of eye care but similar odds of lens services. In urban counties, medium and high eye care supply compared with low eye care supply was associated with decreased odds of vision care. In contrast, in rural counties, medium and high eye care supply was associated with a small increase in odds for eye care and was not associated with lens services.
TABLE 3.
Logistic Regression Analysis of the Factors Associated With the Receipt of Eye Care in Urban and Rural Counties*
| Urban, OR (95% CI) | Rural, OR (95% CI) | |
|---|---|---|
| Age, y | ||
| ≤5 | 0.24 (0.23-0.25) | 0.25 (0.230.27) |
| 6-8 | 1 (Reference) | 1 (Reference) |
| 9-13 | 1.56 (1.51-1.61) | 1.53 (1.43-1.63) |
| 14-16 | 1.66 (1.60-1.73) | 1.60 (1.48-1.73) |
| 17-18 | 1.40 (1.33-1.47) | 1.36 (1.24-1.50) |
| Gender | ||
| Male | 1 (Reference) | 1 (Reference) |
| Female | 1.24 (1.21-1.27) | 1.20 (1.14-1.26) |
| Race/ethnicity | ||
| Hispanic or nonwhite | 1 (Reference) | 1 (Reference) |
| Non-Hispanic white | 1.37 (1.34-1.40) | 0.97 (0.89-1.06) |
| Medicaid insurance type | ||
| Mostly managed care | 1 (Reference) | 1 (Reference) |
| Mixed fee-for-service/managed care | 0.95 (0.92-0.99) | 1.00 (0.93-1.08) |
| Mostly fee-for-service | 1.69 (1.60-1.79) | 1.30 (1.20-1.42) |
| Eye care supply in county of residence | ||
| Low (<25th percentile) | 1 (Reference) | 1 (Reference) |
| Medium (25th-75th percentile) | 0.71 (0.66-0.76) | 1.09 (1.03-1.16) |
| High (>75th percentile) | 0.74 (0.69-0.79) | 1.11 (1.03-1.19) |
Overall, rural children had greater odds of receiving eye care (adjusted OR: 1.24; P < .001). ORs and 95% CIs are adjusted for all factors listed.
TABLE 4.
Logistic Regression Analysis of the Factors Associated With Lens Services in Urban and Rural Counties*
| Urban, OR (95% CI) | Rural, OR (95% CI) | |
|---|---|---|
| Age, y | ||
| ≤5 | 0.12 (0.11-0.13) | 0.14 (0.12-0.16) |
| 6-8 | 1 (Reference) | 1 (Reference) |
| 9-13 | 2.00 (1.91-2.09) | 1.95 (1.78-2.14) |
| 14-16 | 2.21 (2.10-2.33) | 2.34 (2.12-2.59) |
| 17-18 | 1.88 (1.77-2.01) | 1.97 (1.75-2.22) |
| Gender | ||
| Male | 1 (Reference) | 1 (Reference) |
| Female | 1.36 (1.31-1.40) | 1.24 (1.17-1.32) |
| Race/ethnicity | ||
| Hispanic or nonwhite | 1 (Reference) | 1 (Reference) |
| Non-Hispanic white | 1.37 (1.32-1.41) | 0.95 (0.85-1.06) |
| Medicaid insurance type | ||
| Mostly managed care | 1 (Reference) | 1 (Reference) |
| Mixed fee-for-service/managed care | 1.01 (0.96-1.06) | 0.92 (0.84-1.01) |
| Mostly fee-for-service | 1.68 (1.56-1.81) | 1.05 (0.94-1.18) |
| Eye care supply in county of residence | ||
| Low (<25th percentile) | 1 (Reference) | 1 (Reference) |
| Medium (25th-75th percentile) | 0.69 (0.63-0.76) | 1.07 (0.99-1.15) |
| High (>75th percentile) | 0.67 (0.61-0.74) | 0.99 (0.91-1.09) |
Overall, rural children had greater odds of receiving lens services (adjusted OR: 1.22; P < .001). ORs and 95% CIs are adjusted for all factors listed.
Sensitivity Analysis
Excluding from the analysis the children who resided in the largest urban county did not change the direction or statistical significance of the adjusted ORs for the receipt of either eye care or lens services.
DISCUSSION
Important and unexpected patterns of vision care emerged among these Medicaid-enrolled children. Contrary to our initial hypotheses, we found that the odds of receiving vision care were greater in rural counties than in urban ones. Furthermore, urban/rural differences modified the relationship between the other demographic factors and the receipt of vision care. We initially believed that after adjusting for the supply of eye care providers, the rate of vision care would be lower in rural counties because of barriers related to greater travel distances for care.
Although childhood visual impairment is common, few previous data are available regarding the distribution of vision care, and we are unaware of previous data regarding patterns of vision care among children taking into account critical factors such as financial access to care and the local supply of eye care providers. There are only limited previous data describing primary care utilization differences between urban and rural residents, and these do not address pediatric vision care. Findings from one study suggest that rural adults are less likely to obtain preventive services, although those findings include both insured and uninsured people, and rural people are less likely to have insurance.18 In contrast, a study of medical care for children did not demonstrate lower rates of care among rural children.19 Thus, the patterns of care that emerge from our findings are complex and suggest suboptimal distribution of vision care.
In rural counties, increasing eye care supply was associated with a slight increase in the odds of eye care and no change in the receipt of lens care, suggesting that the availability of eye care does not significantly drive vision care. We were surprised to find, however, that in urban counties, increasing eye care supply was associated with decreased rates of both eye care and lens services. These data suggest that increasing the eye care supply in urban counties would not resolve the urban/rural differences in the receipt of vision care. The reason for the inverse relationship between the receipt of vision care and eye care supply in urban counties is unclear. One possible explanation is differences in provider acceptance of Medicaid coverage, with providers in urban markets with higher densities of eye care professionals less likely to care for Medicaid-enrolled children than in urban markets with lower densities of eye care professionals or rural markets, regardless of the density of eye care professionals. One limitation of the available data is that we are unable to determine whether individual providers accept Medicaid coverage. A second limitation is that we are unable to determine the exact site of care and therefore cannot determine the proportion of children who traveled to a county with a different urban/rural status for care. Future studies should focus on pathways to care, Medicaid acceptance, and the impact that Medicaid coverage has on the type of care delivered.
Regardless of rural/urban status, children with mostly fee-for-service Medicaid had greater odds of receiving eye care compared with those who had a longer period of time in Medicaid managed care. Children with mostly fee-for-service Medicaid in urban counties also had greater odds of receiving lens services. In contrast, Medicaid insurance type was not associated with lens services in rural counties. As with factors associated with eye care supply, the economic incentives and disincentives associated with Medicaid insurance type must be understood to ensure optimal vision care delivery.
No difference was found in receipt of vision care by race/ethnicity in rural counties. However, in urban counties, non-Hispanic white children had greater odds of receiving eye care and lens services than Hispanic or nonwhite children. As with our analysis of national data, girls had greater odds than boys of receiving eye care, regardless of other demographic factors.11,12
Because this analysis is based on administrative claims data, we are unable to determine whether these race/ethnicity and gender differences represent undertreatment, overtreatment, or differences in prevalence. Analyses of administrative claims data are subject to the completeness and accuracy of the coding of claims. However, extensive review of vision care claims data was performed to ensure that only claims related to vision care services were included in this analysis. Furthermore, we were unable to detect any systematic coding differences that would lead to the patterns observed in this study. Because medical coding does not always include all services provided within an encounter, we did not separately analyze specific types of eye care, such as eye dilation or refraction.
Our finding that race/ethnicity differences were found only in urban counties, in which the overall rate of vision screening was the lowest, suggests that variations in care are largely driven by differences in treatment and not in the underlying prevalence. A population-based study of vision impairment prevalence and associated vision care utilization is necessary to test this hypothesis.
Underutilization of vision care may have an adverse impact on the development of some children. In contrast, overutilization wastes limited health care resources. The patterns of care among these Medicaid-enrolled children suggest important small-area variations in the receipt of both eye care and lens services. Understanding the sources of these variations is critical to ensuring the optimal vision service delivery.20 Such research needs to involve both optometrists and ophthalmologists and not be based solely on agreed-on definitions of impairment but on the benefits that accrue to the individuals after treatment.
ACKNOWLEDGMENTS
Dr Kemper received support for this work from the National Eye Institute (1 K23 EY14023-01).
We thank the Michigan Department of Community Health for help in obtaining the Medicaid data.
Footnotes
- OR
- odds ratio
- CI
- confidence interval
REFERENCES
- 1.Zadnik K. Myopia development in childhood. Optom Vis Sci. 1997;74:603–608. [PubMed] [Google Scholar]
- 2.US Preventive Services Task Force . Guide to Clinical Preventive Services. 2nd ed. International Medical Publishing; Alexandria, VA: 1996. [Google Scholar]
- 3.American Academy of Ophthalmology . Vision screening for infants and children: AAO Policy Statement. Available at: Accessed September 11, 2003. [Google Scholar]
- 4.American Academy of Pediatrics Committee on Practice and Ambulatory Medicine Section on Ophthalmology Eye examination and vision screening in infants, children, and young adults. Pediatrics. 1996;98:153–157. [PubMed] [Google Scholar]
- 5.American Optometric Association . The need for comprehensive vision examination of preschool and school-age children. Available at: Accessed September 11, 2003. [Google Scholar]
- 6.Broderick P. Pediatric vision screening for the family physician. Am Fam Physician. 1998;58:691–700. [PubMed] [Google Scholar]
- 7.Goss DA, Grosvenor TP, Keller JT, Marsh-Tootle W, Norton TT, Zadnik K. Care of the Patient With Myopia. American Optometric Association; St. Louis, MO: 1997. [Google Scholar]
- 8.Kemper AR, Clark SJ, Freed GL. Services provided for preschool-aged children with suspected amblyopia. J Pediatr Ophthalmol Strabismus. 2003;40:279–282. doi: 10.3928/0191-3913-20030901-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simon JW, Buckley EG, Drack AV, et al. Pediatric Ophthalmology and Strabismus. American Academy of Ophthalmology; San Francisco, CA: 2003. [Google Scholar]
- 10.Kleinstein RN, Jones LA, Hullett S, et al. Refractive error and ethnicity in children. Arch Ophthalmol. 2003;121:1141–1147. doi: 10.1001/archopht.121.8.1141. [DOI] [PubMed] [Google Scholar]
- 11.Kemper AR, Bruckman D, Freed GL. Receipt of specialty eye care by children. Ambul Pediatr. 2003;3:270–274. doi: 10.1367/1539-4409(2003)003<0270:rosecb>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 12.Kemper AR, Bruckman D, Freed GL. Prevalence and distribution of corrective lenses among school-aged children. Optom Vis Sci. 2004;81:7–10. doi: 10.1097/00006324-200401000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kemper AR, Fant KE, Bruckman D, Clark SJ. Evaluation of a hearing and vision screening program for school-aged children. Am J Prev Med. 2004;26:141–146. doi: 10.1016/j.amepre.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 14.US Department of Commerce Census Bureau . Census 2000 summary file. Available at: Accessed September 11, 2003. [Google Scholar]
- 15.US Department of Commerce Census Bureau . Michigan metropolitan areas, counties, and central cities. Available at: Accessed September 11, 2003. [Google Scholar]
- 16.Department of Health and Human Services. Health Resources and Services Administration. Bureau of Health Professions . Area Resource File (ARF) US Department of Health and Human Services; Rockville, MD: Feb, 2003. [Google Scholar]
- 17.US Census Bureau . State and county QuickFacts: Michigan. Available at: Accessed September 11, 2003. [Google Scholar]
- 18.Casey MM, Thiede Call K, Klingner JM. Are rural residents less likely to obtain recommended preventive healthcare services? Am J Prev Med. 2001;21:182–188. doi: 10.1016/s0749-3797(01)00349-x. [DOI] [PubMed] [Google Scholar]
- 19.Dovey S, Weitzman M, Fryer G, et al. The ecology of medical care for children in the United States. Pediatrics. 2003;111:1024–1029. doi: 10.1542/peds.111.5.1024. [DOI] [PubMed] [Google Scholar]
- 20.Coyte PC, Croxford R, Asche CV, To T, Feldman W, Friedberg J. Physician and population determinants of rates of middle-ear surgery in Ontario. JAMA. 2001;286:2128–2135. doi: 10.1001/jama.286.17.2128. [DOI] [PubMed] [Google Scholar]