Universities in England have recently been invited to bid for additional medical student numbers from 2006, and consider increasing numbers further from 2008.1 Do we need more doctors, or are there alternatives to expansion of medical education?
BACKGROUND
Since before the creation of the National Health Service, governments have planned the labour market for doctors, forecasting their demand and supply and adjusting medical school intake. A regular cycle of `shortages' and `surpluses' have been forecast, with little changing methods, despite regular critiques over 30 years.2-5 Medical school intake appears to have been guided largely by political forces; either to create more NHS activity, or to control public expenditure. The implicit assumption is that the average level of activity per doctor is constant, so overall activity can only be affected by adjusting the size of the workforce. This limits the potential for change without the time lag of medical training, and neglects the role of financial and non-financial incentives in influencing overall activity and reducing variations in practice.
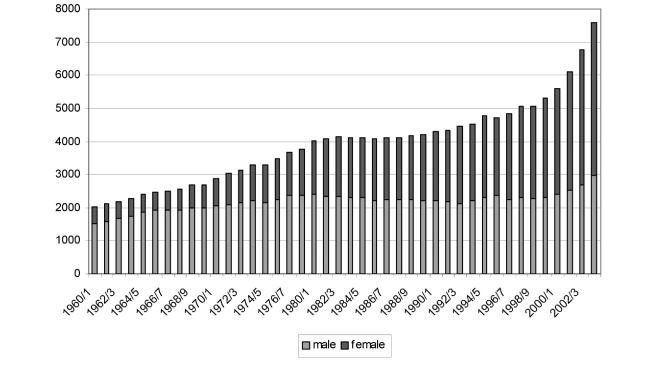
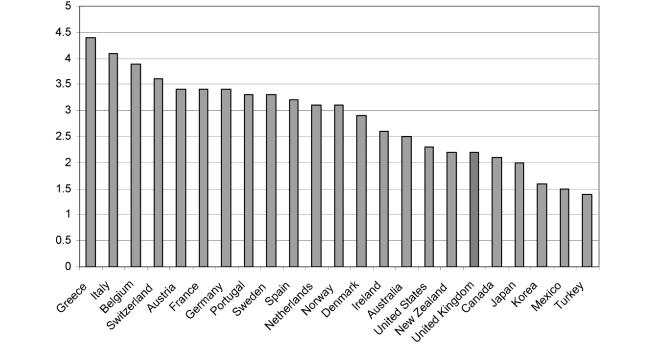
Figure 1 shows a time trend of UK medical school intake, illustrating a gradual increase since the 1960s, with a sharp increase from 5062 in 1998/1999 to 7932 in 2004/2005, over 50% in just 6 years.6 The number of doctors per 1000 population has been rising steadily, even without the new doctors in training since 1998, but this figure (2.3/1000 in 1993) remains below the OECD (Organisation for Economic Co-operation and Development) average of 2.9 physicians per 1000 population (Figure 2).7 There has also been a shift towards more consultant posts and a change in work balance towards management and administration.
Figure 1.
UK medical school intake, 1960-present, by gender (Ref. 6)
Figure 2.
Doctors per 1000 population, selected OECD countries, 2003 (Ref. 7)
The challenges of medical workforce planning are international, with similar policy imperatives, and similar neglect of practice variations and incentive structures. Migration of doctors complicates things further—they are in demand worldwide, and are ever more able and willing to move, to broaden their experience and/or improve their income.8 This creates practical and ethical problems, particularly in countries with workforce shortages and in the developing world. Policy makers increasingly recognize the need for integrated and systematic planning of the healthcare workforce; but the transition from principle to practice remains slow. Internationally, processes are generally mechanistic, neglecting incentives, skill mix and performance management.9
In exploring the debate surrounding further medical school expansion, literature is reviewed here on associations between medical staffing and patient health outcomes; the impact of teaching hospital status; and the potential of changing skill mix.
METHODS
Time and resource constraints precluded the conduct of a full systematic review; but attempts were made to use an objective and scientific approach where possible, particularly using systematic methods of electronic literature searching, with comprehensive search strategies and cautious appraisal of the quality of studies. A search strategy was developed for each of the key questions, aiming to identify primarily review and systematic review articles, but also significant primary research in the field. Electronic searches were conducted in the Cochrane Library, Medline, Embase, CINAHL, and HMIC, for the time period 1985 to 2005. Relevant health and government related websites were explored to identify reports and other grey literature. Bibliographies of identified reviews were examined, and experts in the field were contacted for personal recommendations.
RESULTS
Will more doctors improve patient health?
The UK NHS is widely believed to be under-staffed with doctors, compared with international health systems. Established evidence on nurse staffing levels and outcomes exists,10-12 but the association between doctor numbers and patient outcomes is relatively under-researched. One review13 found support for definite but small increases in the quality of care through increasing physician supply, but other factors including influencing patient lifestyles or physician incentives can have a much larger impact on outcomes. Hewitt et al.'s scoping review of the evidence on health workforce and health outcomes10 focused largely on nurse staffing levels and grades, but findings emerged in relation to physicians. In terms of all staff, higher professional:patient ratios `were associated with a reduction in mortality, failure-to-rescue events, infections, readmissions and complications'. Higher general practitioner: population ratios in one study were associated with lower infant mortality, all-cause mortality and mortality from acute myocardial infarction.14 Ecological evidence suggested that a 1% increase in the supply of primary care physicians could reduce deaths by 0.08/100 000 population. Overall, the review concluded that studies finding a significant relationship tended to have adjusted inadequately for condition severity, so conclusions could not be drawn.10 There was also considerable heterogeneity between study designs; and reviews, though able to describe the probable direction of association between doctor numbers and outcomes, did not find enough evidence to estimate the magnitude of association or establish causation. Finally, the measurement of `outcome' tends to be restricted to easily quantifiable events like mortality rates, rather than broader measures of patient health.
In a study aiming to identify factors explaining standardised hospital mortality ratios, Jarman et al.15 found that although emergency admissions best anticipated mortality variations, the next best estimators were ratios of doctors per bed in hospitals and GPs per head of population in primary care. Furthermore, low GP numbers were significantly correlated with higher emergency admissions. This analysis usefully applied routinely collected data, but was criticised for various reasons, including variable misspecification,16 data shortcomings,17 and misleading measures of hospital performance.18
Cross-national data has also explored this issue. One study19 explored mortality rates across 21 OECD countries from 1970-1995, considering health status as explained by medical care inputs, medical care institutions, public health interventions and background variables. The number of doctors per 1000 population was used as a proxy for medical care inputs, and found to be strongly and significantly associated with premature mortality. When holding other factors constant, a 10% increase in doctors could result in a 4% reduction in premature mortality in women and 3% in men. Another international study20 found that doctors, nurses and midwives together significantly lower maternal, infant and under-5 mortality after controlling for other variables. Disaggregated analysis found doctors were still significant, although nurses and midwives were not. These analyses must however be interpreted cautiously. Large-scale cross-country population studies may oversimplify complex variations, and are only as good as the data on which they rest.
In summary, evidence suggests that improvements in patient outcomes may be made through increasing the supply of doctors and other staff, but the optimal doctor:population ratio is still unclear. Without this information, it is difficult to determine the appropriate medical school intake. Research demonstrating associations between nurse staffing and mortality21 has led in California to a state-wide nurse-bed ratio since January 2005. This strong policy effect, vigorously advocated by researchers, should be supplemented with time series evidence on whether returns to investment in higher staffing ratios are increasing, constant or decreasing.22 In some poorly staffed hospitals, investment in both doctors and nurses could potentially improve patient outcomes. However, where do diminishing returns set in, and what are the substitution possibilities between nurses and doctors?
What is the impact of more teaching hospitals?
As well as directly improving patient health by increasing the doctor:population ratio, expanding medical school intake may have an indirect impact on health, through creating new `teaching hospitals', with associated service implications. A review of outcome differences between teaching and non-teaching hospitals,23 found most studies were North American, and most UK studies related to cancer. Most of the studies reviewed concluded that costs were higher in the teaching hospitals examined: perhaps because of higher use of diagnostic tests, invasive therapeutic procedures and expensive drug therapies. Some papers reported lower mortality rates in teaching hospitals, but several found no difference and results were inconsistent. The review identified a number of study limitations, particularly relating to heterogeneity of hospitals and patient case mix, limited generalizability and small sample size.
A prospective US cohort study24 examined the value and cost of teaching hospitals, exploring a sample of over 15 000 patients at intensive care units in 20 teaching and 17 non-teaching units. They found that teaching hospitals had better survival rates, after adjusting for severity, but at higher cost (largely due to higher rates of diagnostic testing and therapeutic interventions).
Another US study25 also explored quality of care and mortality rates in teaching or non-teaching hospitals, in patients with acute myocardial infarction. Admission to a teaching hospital showed significant association with better quality of care for three out of their four indicators (appropriate use of aspirin, ACE inhibitors and beta blockers). Mortality differences favoured teaching hospitals at all time periods, after adjustment for patient characteristics.25 However, this study was criticized with suggestions that the reported survival advantage of teaching hospitals `may be overstated or even illusory'.26
Generalizing results from USA settings to the current UK medical school expansion is difficult. Separating the influence of teaching hospital status from other associated issues, including patient case mix and availability of technology, is methodologically complex. Teaching hospitals themselves are extremely heterogeneous, and this has increased substantially with the expansion of medical schools in recent decades.
Anecdotal evidence suggests a number of other potential benefits for health services of creation and expansion of medical schools. These lack an evidence base, but may include: recruitment and retention; ability to attract funding; benefits from a research ethic; and benefits to staff morale. However, more experienced consultants are likely to be more expensive, and the opportunity cost of teaching and research may be consultants with less time for or interest in everyday services, resulting in lower clinical activity. Tangible benefits and costs could be informed by a well-designed prospective research study, but even with better information it is difficult to speculate on the implications for continuing expansion. A new `teaching hospital' created by a new medical school, has characteristics very different to a long-standing teaching hospital, with established historical practices and expenditure. `Rebadging' is unlikely to create benefits to local services, and any benefits will diminish as medical school intake continues to expand. They could also result in `Cinderella' health services where there is no associated medical school, making recruitment and retention of medical specialists progressively more difficult.
Do current trends support expansion of medical schools?
Even without the potential direct and indirect outcomes from increasing medical school intake, expansion may be justified to maintain existing service levels if productivity is changing, or to reduce reliance on international medical graduates.
In healthcare, monitoring productivity would ideally mean measuring `health' produced as a result of inputs into healthcare, particularly staff time but also other resource inputs. Health status measures are not yet used to measure population health over time, although this may be developing.27-29 Meanwhile, proxy measures of activity are often used.30,31 It is possible to measure activity at individual consultant level, and to observe variation between individuals.32,33
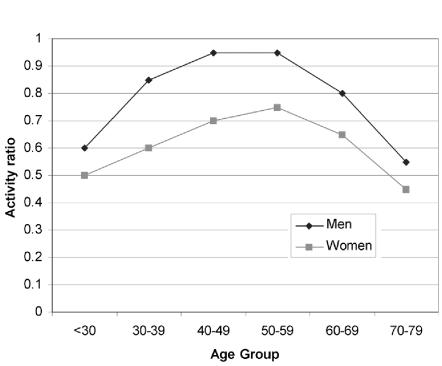
There is a clear trend towards more women doctors, working in all areas of care. Figure 1 illustrates the sharp rise in the proportion of women medical students.6 The work of Goldacre and colleagues34,35 confirms that women are more likely to work part-time, and take career breaks; but also they may be less likely to take early retirement. Data from other countries (e.g. Canada, see Figure 336) suggests that there may be differences in the productivity rates of male and female doctors across all age groups. If this is true in the UK, or if women have different patterns of work or different life-cycle contributions from men, this may influence future workforce planning.
Figure 3.
Activity ratios by age and gender in Canada, 2002/2003 (Ref. 36). Activity ratios compare the relative amount of work two groups of physicians do, as measured by fee-for-service activity, taking into account which provinces in which they practise in and the which specialties they practise. A ratio of 1.0 represents a typical full-time physician in fee-for-service practice
Increasingly, both male and female doctors are likely to work part-time—a trend also evident in other similar health systems. There are a number of potential explanations for this; the simplest is that doctors can afford to work part-time and achieve a more satisfactory work-life balance. This might be particularly relevant following the recent contract renegotiations, with significant pay increases for both consultants and GPs. Other explanations include the level of stress faced by doctors, as a result of the job itself and also the uncertainty relating to system reform. Again if these trends remain, they may support expansion of the medical workforce.
Finally, international concern has been expressed about the ethics of medical workforce migration, and the potential impact of doctors moving from Africa and other developing countries to the West, particularly the UK, USA, Canada and Australia. Policies have been introduced to reduce this `reverse foreign aid' by many developed countries. If the UK is to move towards `self-sufficiency' in its medical workforce, further domestic expansion may be necessary. However, it appears ethical and potentially beneficial for some countries (most notably India) to `export' doctors, and there is no reason why expanding the UK medical workforce should not include purchasing from these `exporting' countries.
Are there alternatives to expansion?
Alternatives to expanding medical school intake might include changing the skill mix of care delivery, substituting other health professionals, or increasing `productivity' of healthcare teams.
A number of systematic reviews have addressed skill mix and substitution issues. In a review of skill mix literature,37 a higher proportion of registered nurses was found to be associated with reduced adverse events in inpatient units, and `... an additional person of any grade does more of everything'. This highlights the role of total staff numbers, and the importance of flexibility to undertake any necessary task. In primary care, a review of substitution literature38 found that patient health outcomes were similar between doctors and nurses; also that nurse-led care was associated with higher patient satisfaction, probably arising from longer consultations, greater provision of information and higher recall. However, the review identified methodological limitations to existing research, particularly short follow-up and underpowered studies. Cost savings arose from salary differentials, but were counteracted by lower nurse productivity (if tasks are completed more slowly), and nurses generating new demand or meeting previously unmet patient needs.
Box 1 Arguments for and against expansion of medical schools
Arguments favouring expansion
Higher doctor numbers may be associated with better patient outcomes, although evidence is weak. However, simply expanding doctor numbers is an extremely expensive allocation of available resources, and other changes (e.g. in incentives or skill mix) could be significantly more cost effective
Teaching hospitals may generate better patient outcomes than non-teaching hospitals, but at significantly greater expense. The source of these differences is unclear, and may not be transferable through the creation of new medical schools
It may be thought necessary to expand the workforce to compensate for reduced NHS activity over time, including the apparent decline in productivity, growing restrictions on hours worked, increasing feminisation of the workforce, increases in part-time working and early retirement. Recent pay increases for doctors may exacerbate these trends by making reduced NHS hours and early retirement affordable while maintaining a healthy target income
Increases in NHS expenditure, and general economic growth and improvements in personal income, have created more demand for healthcare and constantly increasing patient expectations.
Arguments against expansion
Medical workforce planning remains dominated by issues that are poorly measured and managed, including the assumption of fixed doctor-activity ratios when practice variation is large and uncontrolled. Variations in activity of the existing medical workforce should be addressed before any further expansion
Improved incentive systems along with better performance management could perhaps reduce or even reverse the apparent decline in participation and productivity, reducing the need for increased medical school intake by creating more activity from the existing stock of doctors
There are financial and political risks to further investment in increasing the medical workforce, in the presence of diminishing returns, as this may increase the rate of productivity decline. Further expansion of the medical workforce may undermine the potential for more efficient skill mix in the delivery of care
Recent healthcare reform has produced potential for supplier induced demand and system level cost inflation. Such pressures, if accompanied by hasty medical school expansion, could `crowd out' service improvements and threaten the long-term viability of the NHS
Any assessment of the costs of expanding the medical workforce must take into account the costs of their decisions, rather than just the wage costs of new members of medical staff. Injudicious medical school expansion creates challenging expenditure implications
As supply of medical staff increases, it becomes inevitable that referral and treatment thresholds will change, inflating the demand for care and increasing expenditure. This could create further supplier-induced demand and cost inflation, which may be irreversible over decades
Expanding medical school intake will further create difficulties in meeting the demand for training posts. Even now there appears to be excess demand for these posts, with anecdotal reports of 1400 applicants for one post in London
Expanding the medical workforce alone is unlikely to improve the distribution of doctors, by geography or specialty.
A review of the role of nurse practitioners compared with doctors at first-point-of-contact in primary care39 found no differences in patients' health status, although nurse practitioners had statistically significantly longer consultations and made more investigations. The analysis was limited by considering only nurse practitioners, and by the few quality studies available. No conclusions regarding the costs of change could be drawn. Cooper and Stoflet40 also claim that `... non-physician clinicians throughout the range of disciplines can produce high quality outcomes under particular circumstances', with the strongest evidence found for least complex care, or care provided under the `umbrella' of physicians.
Nurse-substitution has been well researched in primary care.41 Nurse outcomes are often as good as those of doctors; and nurses may have superior interpersonal skills, producing greater patient satisfaction.41 Longer consultation times, more investigations and higher recall rates may, however, result in increased costs. From a long-term perspective, nurses are cheaper to train than doctors, but also have lower workforce participation rates, making cost savings less than anticipated. Most research fails to take into account that skill mix is highly dependent on experience as well as grade, therefore interpretations of `appropriate skill mix' inadequately represent actual requirements. The cost-effectiveness of substitution is unclear and under-researched.22,41
This is a developing research area and evidence is emerging about many different roles—e.g. radiographers for radiologists42, nurse endoscopists for medically trained endoscopists.43 The most significant risk with using substitution as a policy solution is that true substitution may not happen: nurses or other clinicians may deal with previously unmet needs or actively generate new demand for care. This has been observed in the USA, where `non-physician clinicians' often appear to operate as complements to rather than substitutes for medical practitioners.44 This does not reduce the physician's workload or contain costs of care.
It may be possible to influence `productivity' of medical staff, facilitating increases in NHS activity without further workforce expansion. In most sectors of the economy, productivity over time and between individuals or teams is monitored routinely. Outcomes from healthcare can be difficult to observe and manage, so process measures, particularly activity, are often used as a proxy. Measurement and management of activity is variable in the hospital sector,45 and lack of data collection makes it impossible to judge activity rates in primary care over time.
For decades, variations in medical practice have been described and discussed worldwide.46 There is considerable variation in individual consultant activity rates32,33 and addressing this variation may require better management and regulation of medical performance and `productivity', together with better incentive structures to encourage greater clinical activity from existing staff levels. Reward and contract mechanisms for doctors, and their inherent financial and non-financial incentives, are matters of immense policy importance. The impact of the new contracts for NHS consultants and GPs on `productivity', in terms of improving activity and quality, is uncertain. The new consultant contract gives no assurance that activity will be increased or even maintained. The GP contract contains explicit `good clinical practice' targets but their opportunity cost is unknown because of deficiencies in information systems, in particular the failure to collect data before implementation of the new contract.
It is important to note that expansion of the medical workforce does not necessarily result in an efficient or equitable distribution of doctors, either geographically or in terms of speciality distribution. One study47 found that expanding supply made inequities worse. With the unavoidable levels of student debt created by undergraduate training, there may be increasing potential for USA-style mechanisms to direct graduates (e.g. by debt repayment, scholarships or bonding arrangements) towards the specialties and areas which deliver improved patient outcomes where they are most needed. This could reduce the most acute shortages without expanding the whole workforce.
Conclusion
The time lag between expanding medical school intake and producing fully trained doctors creates substantial uncertainty and risk. There are clear arguments on both sides of this debate, which are summarized in Box 1. It is difficult to draw firm conclusions in an area where primary research evidence is limited in quantity and quality, and arguments are often contradictory. There are some arguments in favour of expansion; but when medical school intake has already expanded by 50% over the last 6 years, these should have been addressed already, and it appears extremely hasty to increase further before these doctors are even fully trained. Alongside other NHS cost pressures, further expansion may create substantial expenditure inflation that will be extremely difficult to reverse. There is considerable scope for greater investment in research on the causes of variations in productivity of the medical workforce, and on productivity trends. With better measurement and management of physician activity and variations in care, this should inform gradual adjustment of medical school intake, rather than precipitate large-scale expansion.
Acknowledgments This article was derived from a literature review funded by the Department of Health Policy Research and Development Programme.
We are indebted to Anne Burton for invaluable administrative assistance
Competing interests None declared.
References
- 1.Higher Education Funding Council for England (HEFCE). Increasing medical student numbers in England. Circular letter 25/2005 [http://www.hefce.ac.uk/pubs/circlets/2005/cl25_05]
- 2.Peacock A, Shannon R. The new doctors' dilemma. Practitioner 1968;Suppl 6: 9-13 [PubMed] [Google Scholar]
- 3.Maynard A, Walker A. Too many doctors? Lloyds Bank Review July 1977
- 4.Maynard A, Walker A. Doctor Manpower 1975-2000: Alternative Forecasts and Their Resource Implications (Research Paper No. 4, Royal Commission on the NHS). London: HMSO, 1978.
- 5.Maynard A, Walker A. Planning The Medical Workforce: Struggling Out Of The Time Warp (Centre for Health Economics Discussion paper 105). York: University of York, 1993
- 6.Webster R, Mellor D, Spavin B. Who are the doctors of tomorrow and what will they do? 9th Conference Of The International Medical Workforce Collaborative, Melbourne, November 2005 [http://www.health.nsw.gov.au/amwac/amwac/pdf/9_tomdocs_uk.pdf]
- 7.Health Data. Paris: Organisation for Economic Co-operation and Development, 2005
- 8.Mullan F. The metrics of the physician brain drain. N Engl J Med 2005; 353: 1810-18 [DOI] [PubMed] [Google Scholar]
- 9.Bloor K, Maynard A. Planning Human Resources In Health Care: Towards An Economic Approach. An International Comparative Review. Ottawa: Canadian Health Services Research Foundation, 2003
- 10.Hewitt C, Lankshear A, Maynard A, Sheldon T, Smith K. Health Service Workforce and Health Outcomes: a Scoping Study. York: University of York, Department of Health Sciences, 2003
- 11.Lankshear A, Sheldon TA, Maynard A. Nurse staffing and healthcare outcomes: a systematic review of the international research evidence. Adv Nurs Sci 2005; 28: 163-74 [DOI] [PubMed] [Google Scholar]
- 12.Curtin LL. An integrated analysis of nurse staffing and related variables: effects on patient outcomes. Online J Issues Nurs 30 September 2003 [PubMed]
- 13.Perrin JM, Valvona J. Does increased physician supply affect quality of care? Health Aff 1986; 5: 63-72 [DOI] [PubMed] [Google Scholar]
- 14.Gulliford MC. Availability of primary care doctors and population health in England: is there an association? J Public Health Med 2002; 24: 252-4 [DOI] [PubMed] [Google Scholar]
- 15.Jarman B, Gault S, Alves B, et al. Explaining differences in English hospital death rates using routinely collected data. BMJ 1999; 318: 1515-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hennell T. Differences in death rates in English hospitals. Effects of admission rates may have been understated. BMJ 1999;319: 854. [PMC free article] [PubMed] [Google Scholar]
- 17.Bunker JP, Black N. Differences in death rates in English hospitals. Data are inadequate basis for drawing conclusion of paper BMJ 1999; 319: 854-5 [PubMed] [Google Scholar]
- 18.West R. Principal variable is not what it seems in league tables. BMJ 2001;322: 1181. [PMC free article] [PubMed] [Google Scholar]
- 19.Or Z. Determinants of health outcomes in industrialised countries: a pooled cross country time series analysis. OECD Econ Surveys 2000; 30: 53-75 [Google Scholar]
- 20.Anand S, Barnighausen T. Human resources and health outcomes: cross-country econometric study. Lancet 2004;364: 1603-9 [DOI] [PubMed] [Google Scholar]
- 21.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout and job dissatisfaction. JAMA 2002;288: 1987-93 [DOI] [PubMed] [Google Scholar]
- 22.Lankshear A, Sheldon T, Maynard A, Smith K. Nursing challenges: are changes in the nursing role and skill mix improving patient care? Health Policy Matters 2005; issue 10 [http://www.york.ac.uk/healthsciences/pubs/HPM10.pdf]
- 23.Mathers J. Outcome Differences Between Teaching and Non-teaching Hospitals—a Literature Review. Mimeograph. Birmingham: University of Birmingham, 2000
- 24.Zimmerman JE, Shortell SM, Knaus WA, et al. Value and cost of teaching hospitals: a prospective, multicenter, inception cohort study. Crit Care Med 1993;21: 1432-42 [DOI] [PubMed] [Google Scholar]
- 25.Allison JJ, Kiefe CI, Weissman NW, et al. Relationship of hospital teaching status with quality of care and mortality for Medicare patients with acute MI. JAMA 2000;284: 1256-62 [DOI] [PubMed] [Google Scholar]
- 26.Thiemann DR, Coresh J, Oetgen WJ, Powe NR. Quality of care at teaching and nonteaching hospitals. JAMA 2000;284: 2994-5 [DOI] [PubMed] [Google Scholar]
- 27.Kind P, Williams A. Measuring success in healthcare - the time has come to do it properly. Health Policy Matters 2004; issue 9 [http://www.york.ac.uk/healthsciences/pubs/HPM9final.pdf
- 28.Appleby J, Devlin N. Measuring Success In The NHS: Using Patient-Assessed Health Outcomes To Manage The Performance of Health Care Providers. London, King's Fund/Dr Foster, 2004
- 29.Department of Health. Healthcare Output and Productivity: Accounting For Quality Change. London: Department of Health, 2005
- 30.Office of National Statistics. Public Service Productivity: Health. 2004. London: ONS.
- 31.Dawson D, Gravelle H, O'Mahoney M, et al. Developing New Approaches To Measuring NHS Outputs and Productivity, Research Paper 6. York: Centre for Health Economics, 2005.
- 32.Bloor K, Maynard A. Consultants: managing them means measuring them. Health Serv J 2002;112: 10-11 [PubMed] [Google Scholar]
- 33.Bloor K, Maynard A, Freemantle N. Variation in activity rates of consultant surgeons and the influence of reward structures in the English NHS. J Health Serv Res Policy 2004;9: 76-84 [DOI] [PubMed] [Google Scholar]
- 34.Davidson JM, Lambert TW, Goldacre MJ. Career pathways and destinations 18 years on among doctors who qualified in the United Kingdom in 1977: postal questionnaire survey. BMJ 1998;317: 1425-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lambert TW, Goldacre MJ. Career destinations seven years on among doctors who qualified in the United Kingdom in 1988: postal questionnaire survey. BMJ 1998;317: 1429-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Canadian Institute for Health Information. Canada's Health Care Providers. Ontario: CIHI. 2005
- 37.Currie V, Harvey G, West E, McKenna H, Keeney S. Relationship between quality of care, staffing levels, skill mix and nurse autonomy: literature review. J Adv Nurs 2005;51: 73-82 [DOI] [PubMed] [Google Scholar]
- 38.Laurant MGH, Hermens RPMG, Braspenning JCC, Sibbald B, Grol RPTM. Impact of nurse practitioners on workload of general practitioners: randomised controlled trial. BMJ 2004;328: 927-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 2002;324: 819-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cooper R, Stoflet S. Diversity and consistency: the challenge of maintaining quality in a multidisciplinary workforce. J Health Serv Res Policy 2004;9 (suppl 1): 39-47 [DOI] [PubMed] [Google Scholar]
- 41.Sibbald B, Shen J, McBride A. Changing the skill-mix of the health care workforce. J Health Serv Res Policy 2004;9 (suppl 1): 28-38 [DOI] [PubMed] [Google Scholar]
- 42.Brealey S, King DG, Hahn S, et al. The costs and effects of introducing selectively trained radiographers to an A&E reporting service: a retrospective controlled before and after study. Br J Radiol 2005; 78: 499-505 [DOI] [PubMed] [Google Scholar]
- 43.Williams JG et al. What Is The Cost-Effectiveness Of Endoscopy Undertaken By Nurses? A Multi-Institution, Nurse Endoscopy Trial (MINUET). Department of Health R&D Progamme, Health Technology Assessment report (in press) [DOI] [PubMed]
- 44.Grumbach K, Coffman J. Physicians and nonphysician clinicians: complements or competitors? JAMA 1998;280: 825-6 [DOI] [PubMed] [Google Scholar]
- 45.Maynard A, Bloor K. Trust and performance management in the medical marketplace. J R Soc Med 2003;96: 532-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wennberg J, Gittelsohn. Small area variations in health care delivery. Science 1973;182: 1102-8 [DOI] [PubMed] [Google Scholar]
- 47.Richardson J, Macarounas K, Millthorpe F, Ryan J, Smith N. An Evaluation of The Effect of Increasing Doctor Numbers In Their Geographical Distribution, Technical Paper 2. 1991. Victoria: Monash University, 1991