Abstract
Problem: There are wide variations in hospital mortality. Much of this variation remains unexplained and may reflect quality of care.
Setting: A large acute hospital in an urban district in the North of England.
Design: Before and after evaluation of a hospital mortality reduction programme.
Strategies for change: Audit of hospital deaths to inform an evidence-based approach to identify processes of care to target for the hospital strategy. Establishment of a hospital mortality reduction group with senior leadership and support to ensure the alignment of the hospital departments to achieve a common goal. Robust measurement and regular feedback of hospital deaths using statistical process control charts and summaries of death certificates and routine hospital data. Whole system working across a health community to provide appropriate end of life care. Training and awareness in processes of high quality care such as clinical observation, medication safety and infection control.
Effects: Hospital standardized mortality ratios fell significantly in the 3 years following the start of the programme from 94.6 (95% confidence interval 89.4, 99.9) in 2001 to 77.5 (95% CI 73.1, 82.1) in 2005. This translates as 905 fewer hospital deaths than expected during the period 2002-2005.
Lessons learnt: Improving the safety of hospital care and reducing hospital deaths provides a clear and well supported goal from clinicians, managers and patients. Good leadership, good information, a quality improvement strategy based on good local evidence and a community-wide approach may be effective in improving the quality of processes of care sufficiently to reduce hospital mortality.
PROBLEM
Hospital mortality has been used to assess quality of care since Florence Nightingale's comparisons of hospitals in the Crimea and in London in the 19th century.1 Wide variations in hospital mortality have been a consistent finding. Some of this variation can be explained by variables such as the case mix of patients being treated. However, much remains unexplained and may reflect variation in quality of care.2
In 2002 Bradford Teaching Hospitals Trust joined an international programme, Pursuing Perfection, organized by the Institute for Healthcare Improvement aimed at improving quality of care. The initial focus for this programme was on redesigning patient pathways. In August 2002 the focus moved to hospital mortality and a commitment by senior managers and clinical staff in the hospital to eliminate all unnecessary hospital deaths.
SETTING
Bradford Teaching Hospitals Trust is a large acute healthcare trust in the North of England. The hospital has 1200 beds and treats 300 000 out-patients, 100 000 inpatients and 100 000 accident and emergency attendees every year. In 2005 there were 1153 hospital deaths.
DESIGN
The programme started with a review of hospital deaths to inform the change strategies. A detailed case-note audit of consecutive hospital deaths was undertaken to identify gaps in current quality of care. A team consisting of an intensivist, lead clinician, pharmacist and nurse were established for four specialties with the majority of hospital deaths: care of the elderly, medicine, surgery and trauma and orthopaedics. Each team was asked to audit a convenience sample of case notes of 30 consecutive patient deaths using a detailed structured audit form: 118 patient records were reviewed. Analysis revealed a high prevalence of suboptimal clinical observations, hospital acquired infections, medication errors. In addition, an audit of 411 consecutive hospital deaths was carried out by the palliative care team to identify patients coming in to hospital to die, or being kept in hospital for too long prior to death. Frequencies of the key findings are shown in Box 1.
Box 1 Results of hospital audit on consecutive deaths % (n)
Suboptimal clinical observations: 61% (72)
Hospital acquired infection: 23% (27)
Medication errors: 11% (13)
Deaths within 24 hours in hospital: 24% (99)
Deaths after 2 weeks in hospital: 27% (111)
STRATEGIES FOR CHANGE
A hospital mortality reduction group was established by the chief executive to coordinate a strategic approach to reducing hospital mortality. The results of the audit were used to direct the change strategies and identify the priority areas. Objectives were set based on the gaps in care identified around clinical observations, medication errors, end-of-life care and infection control:
Surveillance
Although surgical deaths were routinely reviewed in the hospital, most deaths were non-surgical. A surveillance system was established to increase awareness and review of deaths. This included:
monthly statistical process control charts for each department
feedback of summaries of routine data collection from hospital data and death certificates for each hospital death
regular review of statistical control chart for departmental mortality by the Trust Board and management committees.
Information from the control charts and routine hospital data were used to trigger a more in-depth investigation through case-note audit. A standardized audit tool was developed to review specific areas including quality of clinical observations, prescribing and medicines management, infection control and treatment, thromboprophylaxis, appropriateness of location of care and communication between health professionals.
Clinical observations
The sub-optimal clinical observations prompted action to improve reliability. The modified early warning score (MEWS)3 score was introduced through a series of training sessions for nursing staff.4 This simple scoring tool prompts the recording of optimal observations, indicates the severity of a patient's clinical condition and identifies to when clinical intervention is required. The score was integrated into a standardized clinical observation record and the training has been extended to junior medical staff. In conjunction with the score, a series of training sessions on acute life threatening emergency recognition and treatment (ALERT) were run and continue to be provided for all clinical staff.
Place of death
The audit results indicated that some patients were being admitted to hospital to die, and many patients were being kept in hospital for long periods prior to death. The palliative care team were involved in developing and supporting the use of end of life care guidelines. Hospital staff in each department were trained to diagnose dying and plan appropriately according to the patient's wishes with information about the services available in the community. In addition, a nursing home education project commenced to encourage nursing homes to care for dying patients rather than admit them to hospital.
Infection control
The hospital policy was revised and strengthened to reduce potential hospital acquired infection. Key changes included:
hand hygiene campaigns and introduction of near-patient alcohol rub
staff awareness sessions
improvement of ward cleaning routines
compulsory induction training for all staff
antibiotic guidelines for the hospital
increased surveillance and feedback of infection rates.
Medication errors
Although the audit had not demonstrated a link between the medication errors and any patient deaths, a programme of work was established to improve patient safety. The following areas were targeted:
-
The review of the prescribing and administration of high risk medicines, including warfarin, heparin, potassium and methotrexate. This involved the modification and use of a trigger tool to monitor adverse drug events.
One key result from the trigger tool was to demonstrate problems with out-of-range anticoagulant international normalized ratio values. This prompted a full case note review of patients with high values and resulted in the review of anticoagulant prescribing guidelines and revision and standardization of prescription charts.
In addition, a programme of work to reduce the potential for drug allergy reactions was implemented. This included revision of all drug charts and prescribing prompts were incorporated on the charts.
Reducing medication errors during admission and discharge. Gaps in communication between primary and secondary care were identified. Discharge letters were revised to highlight changes in medications and an electronic system for accessing primary care records of patients admitted to hospital was introduced.
All five components of the programme were developed and implemented during the first 6 months in 2004. The project board of senior clinicians and managers met regularly to review and encourage progress.
EFFECTS
Hospital mortality was taken as the main measure of change. It is a clearly defined event and the ultimate measure of our change strategy. We monitored Hospital Standardized mortality rates calculated by the Doctor Foster unit at Imperial College.5 These death rates are adjusted for age, sex, diagnosis, index of multiple deprivation quintile of the patient's super output area of residence, and admission method (elective or non-elective). The norms are based on the national values for England in the preceding full year. 95% confidence intervals for the hospital standardized mortality ratios were calculated using Byar's approximation.
LESSONS LEARNT
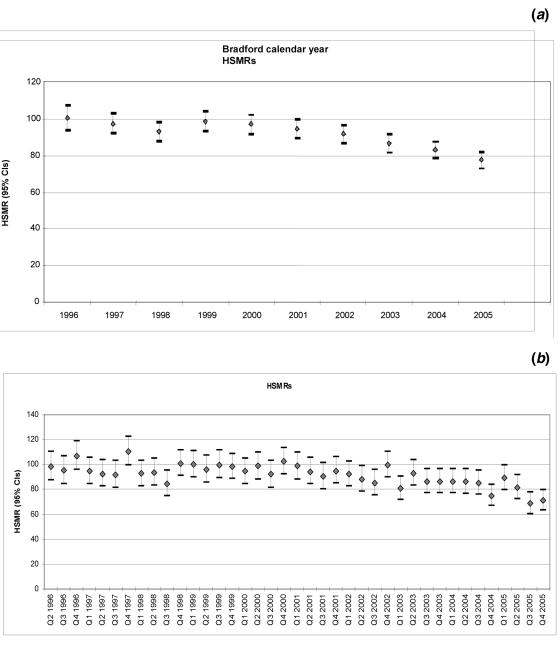
Bradford's hospital standardized mortality ratios for 1996-2005 demonstrate that mortality in the hospital has been historically average or below average prior to 2002 (Figure 1).
Figure 1.
Hospital standardized mortality ratios (HSMRS)—(a) annually and (b) quarterly—for Bradford Teaching Hospitals Trust for period 1996 to 2005. Hospital mortality programme started in August 2002. CI, confidence interval
Hospital standardized mortality ratios fell significantly in the 3 years following the start of the programme from 94.6 (95% CI 89.4, 99.9) in 2001, the year prior to the commencement of the mortality programme to 77.5 (95% CI 73.1, 82.1) in 2005 (Table 1). This translates to 905 fewer deaths than would have been expected during the period 2002-2005. Because the standardization is based on national death rates for the preceding year; and because these are reducing at about 2% overall per year, these figures could be increased by 2% per year cumulatively to give an idea of the absolute numbers of fewer deaths that would be measured if the measurement basis were not changed annually.
Table 1.
Annual deaths in hospital and standardized mortality rates (HSMR, 95% confidence interval) for 1996-2005
| Trend (Calendar Year) | Spells | % | Deaths | % | Expected | % | HSMR RR | Low | High | O-E | O-E change |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1996 | 18196 | 7% | 953 | 5.20% | 948 | 5.20% | 100.5 | 94.2 | 107.1 | 5 | |
| 1997 | 24265 | 9.40% | 1264 | 5.20% | 1298.6 | 5.40% | 97.3 | 92 | 102.9 | −34.6 | 39.6 |
| 1998 | 24577 | 9.50% | 1271 | 5.20% | 1367.1 | 5.60% | 93 | 87.9 | 98.2 | −96.1 | 101.1 |
| 1999 | 25407 | 9.80% | 1354 | 5.30% | 1374.9 | 5.40% | 98.5 | 93.3 | 103.9 | −20.9 | 25.9 |
| 2000 | 25130 | 9.70% | 1320 | 5.30% | 1360.2 | 5.40% | 97 | 91.9 | 102.4 | −40.2 | 45.2 |
| 2001 | 25880 | 10% | 1266 | 4.90% | 1338.9 | 5.20% | 94.6 | 89.4 | 99.9 | −72.9 | 77.9 |
| 2002 | 27302 | 10.60% | 1279 | 4.70% | 1395.5 | 5.10% | 91.7 | 86.7 | 96.8 | −116.5 | 121.5 |
| 2003 | 27780 | 10.70% | 1228 | 4.40% | 1416.6 | 5.10% | 86.7 | 81.9 | 91.7 | −188.6 | 193.6 |
| 2004 | 29615 | 11.50% | 1190 | 4% | 1434.6 | 4.90% | 82.9 | 78.3 | 87.8 | −244.6 | 249.6 |
| 2005 | 30217 | 11.70% | 1153 | 3.80% | 1488.4 | 4.90% | 77.5 | 73.1 | 82.1 | −335.4 | 340.4 |
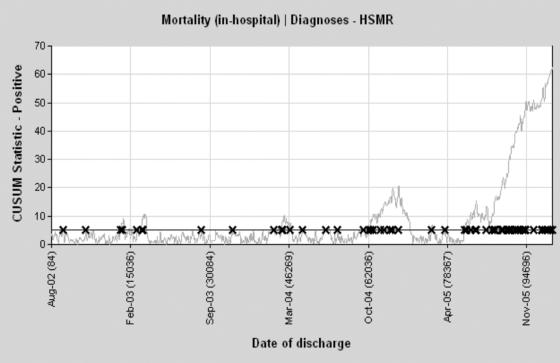
Figure 2 shows the CUSUM (cumulative sum) chart for mortality. The graph plots the cumulative sum of a function of the difference between the hospital's actual deaths and its expected deaths based on national data. The expected deaths are derived from logistic regression models for a particular diagnosis or group of diagnoses in which death is modelled against year, age, sex, admission method (emergency or elective), diagnosis, and index of multiple deprivation quintile of the patient's super output area of residence.6 This CUSUM graph is set to detect an odds ratio of 0.5 for the trust compared with all England: if a patient dies, the chart falls and if they survive, the chart rises. The rising slope demonstrates the periods when mortality was lower than expected.
Figure 2.
CUSUM (cumulative sum) chart of hospital mortality. HSMR, hospital standardized mortality ratios. The rising slope demonstrates the periods when mortality was lower than expected (see p. 303 for more detailed explanation)
DISCUSSION
This paper describes how mortality intelligence was used constructively to trigger closer investigation of processes of clinical care across medical and surgical specialties. This investigation led to common themes of quality improvement across the hospital. During the course of the programme we observed statistically significant reductions in our hospital standardized mortality ratios. The fact that Bradford's hospital mortality was below average to begin with makes the further reduction particularly notable. This was not a case of a hospital with a high rate regressing to the mean.
Attribution is inevitably difficult in a simple before and after comparison we would be cautious in implying a causal association. However, it may be that our changes in practice translated into improvements that were significant enough to reduce unnecessary deaths.
Perhaps the most fundamental goal in improving quality of care in hospitals is to eliminate unnecessary deaths. Mortality is a clearly defined and important outcome in healthcare and therefore relatively simple to collect and measure. In many hospitals the review of mortality intelligence tends to be confined to surgical specialties. Analysis has tended to be either through case note audit of individual patient deaths which can be selective or partial, or judgementally as a comparison with other hospital departments as part of an aggressive and critical approach such as `league tables'. Such unsophisticated comparisons of mortality between hospitals or clinicians can be misinterpreted and used for judgment and blame.7
There are a number of factors that we feel have made the greatest impact and would provide lessons that could be transferred to other hospital settings.
Leadership. The promise to `reduce all unnecessary deaths' was a commitment by the chief executive and hospital board. This high level backing was able to align hospital systems such as audit, information services, training and clinical directorates to a common goal. The importance of this goal was clear to clinicians, managers and patients.
Contextual analysis. We based the strategy of our mortality reduction programme on good evidence obtained from a rigorous hospital-wide audit of 118 deaths that was extended to over 500 deaths during the first year. This identified a number of gaps in quality of care that were addressed in the subsequent strategy.
Strong professional support. Mortality reduction is a goal that is common to all health professionals and the programme attracted clear commitment across the hospital and strong support from consultant medical staff. The hospital has a strong tradition of consultantled medical care.
Measurement. Using statistical process control charts and summaries of patient deaths we were able to present mortality data in simple formats that encouraged a reflective approach to the continuous monitoring of patient deaths in each department. The control charts provided a valuable tool for monthly review of mortality and identification of non-random variation.8-11 They are easy to use and simple to understand for non-statisticians. More importantly they are statistically robust and promote an objective assessment of variation rather than selective interpretation of single data points. Their introduction can lead to improved monitoring and investigation of hospital deaths both in individual departments and by senior managers and the Trust Board.8 This in turn has led to a greater understanding of the processes of care that can be improved to reduce unnecessary deaths.
Partnership across a whole health community. Working with the community palliative care team and local nursing homes enabled us to ensure that patients were allowed to choose their place of death rather than being admitted automatically to hospital.
Communication, training and awareness. Work on improving the quality of key processes of clinical care such as clinical observations, medication safety and infection control probably contributed to on-going awareness and improvement of quality.
Acknowledgments We are very grateful to all the clinical governance leads and staff at Bradford Teaching Hospitals Trust for their enthusiastic involvement and commitment to providing safer healthcare. We thank our colleagues from the Community of Practice team for their support through the national programme and providing data on comparative mortality rates.
Funding No funding was received for this programme.
Competing interests None.
References
- 1.Nightingale F. Hospital Statistics and Hospital Plans. London: Emily Faithfull & Co;1862.
- 2.Jarman B, Gault S, Alves B, et al. Explaining differences in English hospital death rates using routinely collected data. BMJ 1999; 318: 1515-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Subbs CP, Kruger M, Rutherford P, Genne L. Validation of a modified Early Warning Score in medical admissions. Q J Med 2001;94: 521-6 [DOI] [PubMed] [Google Scholar]
- 4.Morgan RJM, Williams F, Wright MM. An early warning scoring system for detecting developing critical illness. Clin Intensive Care 1997;8: 100 [Google Scholar]
- 5.Jarman B, Bottle A, Aylin P. Monitoring changes in hospital standardised mortality ratios. BMJ 2005;330: 329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jarman B, Bottle A, Aylin P, Browne M. Monitoring changes in hospital standardised mortality ratios. BMJ 2005;330: 329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lilford R, Mohammed MA, Spiegelhalter D, Thomson R. Use and misuse of process and outcome data in managing performance of acute medical care: avoiding institutional stigma. Lancet 2004;363: 1147-54 [DOI] [PubMed] [Google Scholar]
- 8.Benneyan J C, Lloyd R C, Plsek P E. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care 2003;12: 458-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohammed M A, Cheng K K, Rouse A, et al. Bristol, Shipman, and clinical governance: Shewhart's forgotten lessons. Lancet 2001; 357: 463-67 [DOI] [PubMed] [Google Scholar]
- 10.Lim T O. Statistical process control tools for monitoring clinical performance. Int J Qual Health Care 2003;15: 3-4 [DOI] [PubMed] [Google Scholar]
- 11.Poloniecki J, Sismanidis C, Bland M, Jones P. Retrospective cohort study of false alarm rates associated with a series of heart operations: the case for hospital mortality monitoring groups. BMJ 2004;328: 375-9 [DOI] [PMC free article] [PubMed] [Google Scholar]