Abstract
Background
Patients' attitudes towards the management of minor ailments influence help-seeking behaviour. Up-to-date information about patients' attitudes is valuable for understanding changes in help-seeking behaviour.
Aim
To describe changes in patients' attitudes between 1987 and 2001, and to explain the relationship between patients' attitudes and attributes of practices, practitioners and patients.
Design
Two cross-sectional, Dutch National Surveys of General Practice (1987 and 2001; n = 9579 and n = 8405 patients, respectively).
Setting
General practice in the Netherlands.
Method
Patients' attitudes were evaluated in health interviews. Data were analysed using multilevel regression analysis.
Results
In 2001, patients' attitudes showed a shift away from consulting their GP for minor ailments. Attitudes are uniform across different types of practice, and mainly differ between patients. In 1987 as well as in 2001 the factors associated with firm beliefs about the benefits of GP's care in case of minor ailments were male, older age, lower educational level, a non-Western cultural background, and a visit to the GP in the past 2 months. Furthermore, the association between health status and beliefs about GPs dealing with minor ailments is more marked in 2001. Compared to 1987, the influences of GPs and the practice are more intertwined in 2001.
Conclusions
Patients' attitudes towards the management of minor ailments have changed over the years, which implies that strategic action by the profession and the government has affected the way the public uses primary care. However, a marginal group of patients (elderly, less-educated, non-Western) is lagging behind this trend, and continuing to consult GPs for minor ailments.
Keywords: attitude to health, minor ailments, primary health care
INTRODUCTION
Relative shortages in personnel and high workloads of GPs require strategies to reduce ‘inappropriate’ use of GPs' care. From a GP's viewpoint, a significant part of inappropriate demand for services is generated by consultations for minor ailments. In a British study, many GPs expressed frustration at the level of minor ailment workload.1 Minor ailments are self-limiting and can be relieved with over-the-counter medication or other self-care strategies. Nonetheless, some patients decide to consult their GP for minor ailments whereas others do not.2 Variation in help-seeking behaviour is most pronounced among self-limiting health ailments, such as a sore throat or headache. Differences in help-seeking behaviour can be explained by three factors: medical need (morbidity), enabling factors (access to care, individual resources), and predisposing factors (demographic, social structure, health beliefs, psychological attributes).3,4 The ‘health belief model’ further focuses on these predisposing factors in relation to the use of care.5,6 According to this model, patients' perceived vulnerability, beliefs about the benefits of care and barriers to care are important factors influencing medical help-seeking and satisfaction with care. High users of health care are more likely to adopt a ‘doctor knows best’ attitude; they perceive themselves as having less control of their own health. Entrenched beliefs about the benefits of health care are associated with older age, lower income and less education.2 The focus of this article is on patients' attitudes towards the management of minor ailments.
In the Netherlands, the past few decades have seen information campaigns by GPs and policy strategies aimed at actively discouraging consultations for minor ailments. Patients are encouraged to employ self-care: part of the medication for minor ailments has been taken out of the insurance package and websites have been created to provide information on both a healthy lifestyle and the management of minor complaints. All this will have influenced patients' beliefs about whether to consult a GP in the case of minor ailments.
In addition, as a consequence of out-of-hours services being clustered, more GPs working part-time and more group practices, patients increasingly do not consult their regular GP – and this may also have influenced patients' consulting behaviour.
Accordingly, in the light of changes in Western society (for example, more assertive patients and increased individual focus on health), as well as changes in Dutch health care (such as changes in the insurance package) and in Dutch general practice (such as changes in out-of-hours services), up-to-date information about patients' attitudes is valuable, because knowledge of patients' attitudes may lead to a better understanding of help-seeking behaviour.
This study aims:
To describe changes in patients' attitudes towards the management of minor ailments between 1987 and 2001, and to evaluate the extent to which variation in patients' attitudes can be attributed to patients, GPs or practices;
To explain the relationship between patients' attitudes and characteristics of patients, GPs and practices, and to evaluate the extent to which the effects of these characteristics may have changed between 1987 and 2001.
METHOD
Study sample
Data from two Dutch National Surveys of General Practice were used.7,8 In the first Dutch National Survey of General Practice, data were collected between April 1987 and March 1988 in a stratified sample of 193 GPs in 103 practices, who served 335 000 patients in total. In the second National Survey of General Practice data were collected during 2001 in 104 representative general practices in the Netherlands, comprising 195 GPs, who served 385 461 patients in total. In both studies, a random sample of the Dutch-speaking population of the practices participated in an extensive health interview survey (1987, n = 13 066, response = 76.7%; 2001, n = 12 699, response = 64.5%). This interview contained questions about issues such as healthcare utilisation, opinions and life style. Additionally, background information about sociodemographic characteristics and subjective health status of all patients was collected. In both studies, questionnaires were used to collect information about characteristics of the participating GPs and practices.
Patients' expectations
The Nijmegen Expectation Questionnaire is a validated scale, used to assess patients' attitudes towards the management of minor ailments with regard to medical treatment (as compared to self-care).9 The Nijmegen Expectation Questionnaire was administered in 1987 (n = 9 579 responders) and in 2001 (n = 8 405 responders) as a part of the health interview. In the questionnaire, patients' attitudes are ascertained in 12 statements concerning the possible benefits of consulting a GP for various common symptoms (Box 1). Responders agree or disagree with the given statement on a 5-point scale. A higher score denotes stronger beliefs about the benefits of a GP's care for common health ailments. The internal consistency and construct validity of the Nijmegen Expectation Questionnaire were established in the 1987 national survey and confirmed in the 2001 second survey.
Box 1. Contents of the Nijmegen Expectation Questionnaire.
-
▸
Medicine prescribed by the GP will clear up diarrhoea quicker than an over-the-counter remedy.
-
▸
Sedatives prescribed by the GP are the correct remedy if you feel nervous and stressed.
-
▸
Pain in the neck and shoulders may be symptoms of a condition which definitely needs treatment.
-
▸
You recover from flu more quickly if you consult your GP.
-
▸
If you are feeling lethargic and tired, a tonic prescribed by the GP will work best.
-
▸
You should consult a doctor for a sore throat, just to be on the safe side.
-
▸
Stomach problems are better treated by a doctor than by self-medication.
-
▸
You should be examined by your doctor if you have a headache, in case there is something seriously wrong.
-
▸
You will recover more quickly from feebleness in the arm with treatment from the GP than without treatment.
-
▸
If you are nauseous and need to vomit, you're better off going to the doctor, as you never know what the cause might be.
-
▸
Remedies for a cold prescribed by a GP are better than those you buy yourself.
-
▸
You will get over a headache quicker with medicine from the GP than by taking something yourself.
How this fits in
Older age and a lower level of education are associated with beliefs about the benefit of GPs' care as compared to self-care. In general, patients' attitudes have shifted away from consulting their GP for minor ailments. Attitudes are uniform across different types of practice, and mainly differ between patients, indicating a general effect of professional and governmental strategies. However, a marginal group of patients (elderly, less-educated, non-Western) is lagging behind this trend and continuing to consult GPs for minor ailments.
Statistical analysis
The Nijmegen Expectation Questionnaire was administered in individuals from the age of 18 years; questionnaires with missing items were excluded from the analyses. The Student's t-test for independent samples was used to compare mean sum scores. Differences between effects of independent variables and the mean scores in 1987 and 2001 were tested with χ2 tests. Because of the hierarchical nature of the data (patients being clustered within GPs, nested in practices), multilevel analysis was used to analyse the relationship between patients' attitudes and the characteristics of patients, GPs and practices. Multilevel analysis is a statistical technique that extends single-level regression analysis to the situation where the data are hierarchical.10 The sum score of the Nijmegen Expectation Questionnaire was set as the dependent variable. In the multilevel analysis, raw scores were changed into standard scores expressing standard deviation units (z-scores) to allow for direct comparison of 1987 and 2001. At the level of the patient, sociodemographic variables and health indicators known to influence help-seeking behaviour were entered into the model as independent variables. At the level of the GPs, sex, age, duration of residency and length of working week were entered into the model as proxies for possible different ways of managing clinical activities. Practice variables in the model included type of practice, practice size and urbanisation type of the practice location. The independent variables were centred by the overall mean (of 1987 and 2001 combined) to correct for differences in sample characteristics and thereby allow for direct comparison between 1987 and 2001. Two steps of the analysis are shown: first, without explanatory variables (Model 1). We evaluated the percentage of variance at two levels: patient and practice. Multilevel analysis allows the separation of the variance over the levels: in part due to differences in patients and in part due to differences in practices. Initially, three levels were defined in the analysis: patient, GP and practice. When it became clear that in 2001 no variance existed at the level of the GP, we decided to use two levels: patients and practices. In a following step we added patient, GP and practice characteristics to the model (Model 2). The MLwiN software package was used to carry out the multilevel analysis.
RESULTS
Responders
Table 1 shows the characteristics of the responders in the health interview, and GPs and practices attended in 1987 and 2001. In 2001, the mean age of the responders was higher than in 1987 and fewer responders reported good health. In both 1987 and 2001 the majority of GPs were male, and about 50% of the practices were group practices. In the first survey a greater number of GPs were under 40 years. In 2001 more practices were located in an urban area than in 1987.
Table 1.
Characteristics of responders, GPs and practices attended in 1987 and 2001.
| 1987 | 2001 | |
|---|---|---|
| Mean NEQ sum score (SD), not standardised (range = 12–60) | 35.4 (8.9) | 30.8 (7.7) |
| Responders | n = 9579 | n = 8405 |
| Age range (years) | 18–97 | 18–96 |
| Mean (SD) | 43.0 (16.8) | 48.5 (16.8) |
| >65 years (%) | 13.8 | 19.4 |
| Female (%) | 51.1 | 55.7 |
| Cultural background (%) | ||
| Western | 75.2 | 86.2 |
| Non-Western | 1.2 | 2.7 |
| Missing data | 23.6 | 11.1 |
| Educational level (%) | ||
| No/low (elementary school or no school) | 19.4 | 13.9 |
| Medium | 66.4 | 64.3 |
| High (academic level education) | 14.2 | 21.8 |
| One or more chronic disease (%) | 56.7 | 65.0 |
| Acute ailment(s) in the last 14 days (%) | 80.4 | 90.6 |
| Self-reported health, in general (%) | ||
| Very good | 82.4 | 67.3 |
| Moderate to poor | 169 | 18.6 |
| Missing data | 0.7 | 14.1 |
| Consulted GP in past 2 months (%) | 39.2 | 58.2 |
| GPs | n = 175 | n = 159 |
| Female (%) | 17.7 | 20.5 |
| Age range (years) | 28–62 | 34–62 |
| Mean (SD) | 41.4 (7.8) | 47.7 (6.2) |
| <40 years (%) | 47 | 18 |
| Practices | n = 103 | n = 104 |
| Solo practice (%) | 50.5 | 53.8 |
| Location (%) | ||
| Most urban (inner city) | 14.6 | 21.2 |
| Urban (small town) | 15.5 | 23.1 |
| Suburban | 19.4 | 19.2 |
| Mixed urban/rural | 26.2 | 19.2 |
| Rural | 24.3 | 17.3 |
NEQ = Nijmegen Expectation Questionnaire. SD = standard deviation.
Changes in patients' attitudes between 1987 and 2001
Table 1 shows the mean raw sum scores of the Nijmegen Expectation Questionnaire (range = 12–60) in both 1987 and 2001. In 2001, patients' beliefs about the benefits of a GP's care as compared to self-care for minor ailments are significantly less strong than in 1987 (−4.6; 95% confidence interval [CI] = 4.3 to 4.8; P<0.001). In Table 2, the standardised scores for 1987 and 2001 are shown, corrected for differences in sample characteristics. These standardised scores also show a significant decline in patients' beliefs about GPs' care.
Table 2.
Practice and patient level variance in attitude scores, and association between characteristics of patients, GPs and practices against patients' attitudes: standardised scores (standard errors).
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| 1987 | 2001 | 1987 | 2001 | |
| Variation | ||||
| Practice level variance | 0.063 | 0.061 | 0.029 | 0.035 |
| Patient level variance | 0.939 | 0.948 | 0.788 | 0.756 |
| Patient characteristics | ||||
| Intercepta (mean NEQ score, standardised) | −0.006 (0.028) | 0.019 (0.028) | 0.072 (0.028) | −0.111 (0.031) |
| Medical need variables | ||||
| Self-reported healtha (0 = [very] good, 1 = moderate/poor) | 0.047 (0.034) | 0.141b (0.028) | ||
| One or more health complaintsa (1 = yes) | −0.053 (0.032) | 0.050 (0.038) | ||
| Chronic illness (1 = yes) | −0.033 (0.026) | 0.009 (0.024) | ||
| Visit to GP last 2 months (1 = yes) | 0.089c (0.025) | 0.123b (0.022) | ||
| Enabling factors | ||||
| Socioeconomic status (1 = low, 2 = medium, 3 = high) | −0.103c (0.023) | −0.087b (0.018) | ||
| Public insurance (1 = yes) | 0.150c (0.028) | 0.107b (0.025) | ||
| Factors independent of illness | ||||
| Sexa (1 = male) | 0.190b (0.024) | 0.324b (0.022) | ||
| Educational level (1 = no/low, 3 = high) | −0.238b (0.029) | −0.196b (0.023) | ||
| Age (continuous)c | 0.023b (0.002) | 0.027b (0.002) | ||
| Non-Western background (1 = yes) | 0.337b (0.103) | <0.570b (0.070) | ||
| GP attributes | ||||
| Duration of residency (continuous) | 0.002 (0.002) | −0.006 (0.005) | ||
| Age (continuous) | 0.004 (0.002) | 0.010 (0.007) | ||
| Sex (1 = male) | 0.010 (0.052) | −0.011 (0.043) | ||
| Hours working (continuous) | 0.117 (0.110) | 0.226 (0.132) | ||
| Practice attributes | ||||
| Type of practice (0 = single-handed, 1 = group) | 0.031 (0.057) | 0.008 (0.064) | ||
| Urbanicity (1 = most urban to 5 = rural) | 0.013 (0.016) | 0.005 (0.017) | ||
| Total GPs in practice (continuous) | −0.066 (0.034) | 0.018 (0.037) | ||
| Total listed patients (continuous) | <0.001 (0.000) | <−0.001 (0.000) | ||
Significant effect between both samples: the difference in standardised mean score was significant at the level of P<0.001; the difference in effect of male sex between the two studies was significant at the level of P<0.01, whereas the difference in effects of self-reported bad health and reporting more health complaints were significant at the level of P<0.05.
In order to capture a possible non-linear relationship between age and patients' attitudes, age was modelled as a separate polynomial effect.
Significant effect of independent variable on patients' scores as measured with the Nijmegen Expectation Questionnaire (NEQ).
Variation in patients' attitudes
The bulk of the variation in patients' attitudes can be ascribed to differences between patients (see Table 2). In 1987, 6.3% of the variance in expectation scores could be ascribed to differences between practices, and most of the variance was found at the level of the patients (93.7%).
In a three level model in 1987, 3.7% of the variance clustered at the level of practices and 3.5% of the variance could be ascribed to differences between GPs. In 2001, 6% of the variance could be ascribed to differences between practices and 94% to differences between patients, but no variance was found at the level of the GP. With all the variables included in the model, we were able to explain 41.3% (1987) and 41% (2001) of the variance at the level of the practices, and 16.1% (1987) and 20.1% (2001) at the patients' level.
Relationships
Table 2 also shows the relationship the combination of patient characteristics, GP and practice has with patients' attitudes towards the management of minor ailments in 1987 and 2001. From Table 2 it can be seen that at the patient level, in both 1987 and 2001, a visit to the GP 2 months prior to the interview, public health-insurance, being male, older in age, and of a non-Western cultural background are associated with stronger beliefs about the benefits of a GP's care. A higher educational level and socioeconomic status are associated with weaker beliefs about the benefits of care. In 2001 (but not 1987), self-reported poor health is significantly associated with beliefs about the benefits of a GP's care. The included characteristics of the GPs and practices were not significantly associated with patients' attitudes towards the management of minor ailments.
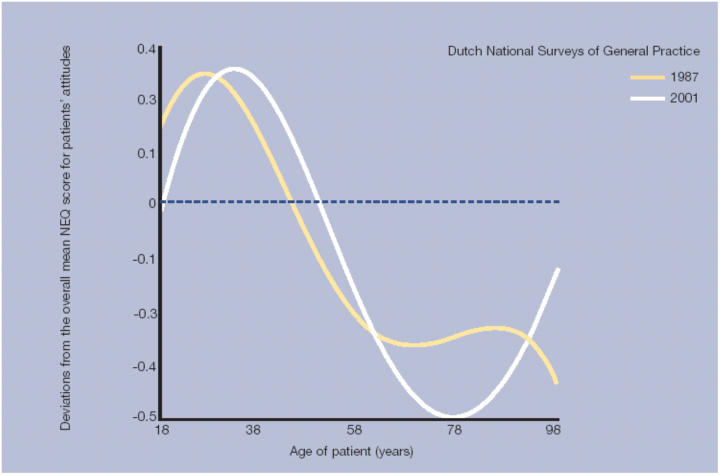
The magnitude of the association between belief in GPs' management of minor ailments and the factors being male, having self-reported poor health and the presence of acute health complaints was significantly greater in 2001 than in 1987 (Table 2). Additionally, we evaluated the relationship between attitudes and patients' ages in 1987 and 2001, as plotted in Figure 1. The graph shows that as compared to the overall mean, patients aged 30–40 years are more inclined to self-management for minor ailments, whereas elderly patients expect greater benefit from a GP's care. The main differences between 1987 and 2001 (P = 0.08) in the relationship between age and attitudes are seen in older patients. As compared to 1987, in 2001 older patients expect more benefit from a GP's care with regard to minor ailments.
Figure 1.
Relationship between patients' age and deviations from the overall mean Nijmegen Expectation Questionnaire (NEQ) score for patients' attitudes in 1987 and 2001.
DISCUSSION
Summary of main findings
As expected, in the past two decades, patients' attitudes towards the management of minor ailments have moved away from consulting GPs for minor ailments. Attitudes mainly vary between different categories of patient; they are uniform across different types of practice. It seems that the change in overall view is not one that is attributable to the actions of individual practices but rather to a more general effect, such as changes in the insurance package and information leaflets of the Dutch College of GPs (In Dutch: Nederland Huisartsen Genootschap). Strategic action by the profession and the government has affected the way the public uses primary care.
The different categories of patient (older age, less education and lower income) known to be associated with frequent attendance2,11 were also associated in our study with positive beliefs about the benefit of consulting a GP. In addition, we found that people with a non-Western background and those who visited a GP in the previous 2 months likewise expect more benefit from GPs' care in the case of minor ailments. Strikingly, in 2001 elderly patients expect greater benefit from GPs' care than in 1987. This could be because the information did not reach them; or it could have to do with an increased focus on health also among the elderly, as the relationship between health variables and patients' attitudes was significantly stronger in 2001 than in 1987. The answer cannot be elucidated on the basis of this study. What has become clear, however, is that further research is needed to find out why a marginal group of patients (elderly, non-Western and less educated) is more inclined than others to consult their GP for minor ailments.
Strengths and limitations of the study
Data collection in both 1987 and 2001 took place on a large scale and the samples are comparable. In the Netherlands, all non-institutionalised patients are registered in a general practice, which made it possible to include those patients in our study that rarely visit their GP; therefore the whole population at risk was included. Non-response of the health interview and the census showed not to be selective with regards to the age and sex of the responders. Responders with a cultural background other than Dutch were under-represented. The study was designed to provide robust data on the prevalence of disease and to shed a more up-to-date light on GPs' care. Attitudes towards minor ailments represented merely a small aspect of the extensive health interview. More detailed measures could be considered for future studies, and it would be interesting to compare intentions as described by the Nijmegen Expectation Questionnaire and consultation behaviour as recorded in the practices.
Implications for general practice
The question remains as to whether consulting a GP for a minor ailment always equals inappropriate behaviour. Taking into consideration differences in income, knowledge, comorbidity and the relative frequency of use of various medications in older age, the decision to consult a GP for common ailments can be a very adequate one. In a qualitative study, Kokko found that reasons for a consultation may be associated with seeking information or seeking support.12 Dowrick13 showed that frequent consulting may also be associated with a change in the healthcare team, and Williams et al14 found that most patients wanted an ‘explanation of the problem’ from their GP. Furthermore, from the GP's perspective, the definition of inappropriate help-seeking behaviour in out-of-hours services may be different from that during surgery hours.
It seems implausible that the decline in beliefs about the benefits of a GP's care correlates with a decline in overall confidence in health care or GPs. Over the past 5 years, levels of confidence in health care show only little variation, whereas in the same period there has been much debate about matters such as hospital waiting lists and organisational changes in general practice care.17
Finally, models on consultation behaviour take little account of the patient's social context, although several studies have shown the importance of considering the social context when evaluating help-seeking behaviour.16,17 In total, with all the variables included in the model we were able to explain about one fifth of the variance in attitude scores at the level of the patient. It is probably not only the context of the practice that accounts for this, but also the patients' direct social context: that is, patients' family or social circle may explain another part of the variance at the patients' level. In the past, several studies have shown that families share beliefs and behaviours with regard to illness and health, thereby influencing each other's beliefs about the benefits of health care and consequently the use of health care.13,18 Adding a family level to the analysis seems a logical avenue to pursue.
Conflicting interests
None.
REFERENCES
- 1.Morris CJ, Cantrill JA, Weiss MC. GPs' attitudes to minor ailments. Fam Pract. 2001;18:581–585. doi: 10.1093/fampra/18.6.581. [DOI] [PubMed] [Google Scholar]
- 2.Howe A, Parry G, Pickvance D, Hockley B. Defining frequent attendance: evidence for routine age and sex correction in studies from primary care settings. Br J Gen Pract. 2002;52:561–562. [PMC free article] [PubMed] [Google Scholar]
- 3.Andersen R, Newman JF. Societal and individual determinants of medical health care utilisation in the United States. Milbank Mem Fund Q. 1973;81:95–123. [PubMed] [Google Scholar]
- 4.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 5.Rogers A, Hassell K, Nicolaas G. Demanding patients? Analysing the use of primary care. Buckingham: Open University Press; 1999. [Google Scholar]
- 6.Rosenstock I. Why people use health services. Milbank Mem Fund Q. 1966;44:94–127. [PubMed] [Google Scholar]
- 7.Westert GP, Schellevis FG, de Bakker DH, et al. Monitoring health inequalities through general practice: the Second Dutch National Survey of General Practice. Eur J Public Health. 2005;15(1):59–65. doi: 10.1093/eurpub/cki116. [DOI] [PubMed] [Google Scholar]
- 8.Foets M, Van der Velden J. Een nationale studie naar ziekten en verrichtingen in de huisartspraktijk. Basisrapport: meetinstrumenten en procedures. Utrecht: NIVEL; 1990. [A national survey of morbidity and interventions in General Practice: methods and instruments] [Google Scholar]
- 9.Van de Lisdonk EH. Ervaren en aangeboden morbiditeit in de huisartspraktijk. Nijmegen: University of Nijmegen; 1985. [Morbidity in general practice] (Thesis) [Google Scholar]
- 10.Leyland AH, Groenewegen PP. Multilevel modeling and public health policy. Scand J Public Health. 2003;31:267–274. doi: 10.1080/14034940210165028. [DOI] [PubMed] [Google Scholar]
- 11.Weijden T van der, Velsen M van, Dinant GJ, et al. Unexplained complaints in general practice: prevalence, patients' expectations, and professionals test-ordering behaviour. Med Decis Making. 2003;23:226–231. doi: 10.1177/0272989X03023003004. [DOI] [PubMed] [Google Scholar]
- 12.Kokko SJ. Long-term patterns of general practice consulting behaviour: a qualitative 9-year analysis of general practice histories of a working-aged rural Finnish population. Soc Sci Med. 1990;30:509–515. doi: 10.1016/0277-9536(90)90354-u. [DOI] [PubMed] [Google Scholar]
- 13.Dowrick C. Why do the O'Sheas consult so often? An exploration of complex family behaviour. Soc Sci Med. 1992;34:491–497. doi: 10.1016/0277-9536(92)90204-4. [DOI] [PubMed] [Google Scholar]
- 14.Williams S, Weinman J, Dale J, Newman S. Patient expectations: what do primary care patients want from the GP and how far does meeting expectations affect patient satisfaction? Fam Pract. 1995;12:193–201. doi: 10.1093/fampra/12.2.193. [DOI] [PubMed] [Google Scholar]
- 15.Van der Schee E, Groenewegen PP, Friele R. Public trust in health care in The Netherlands. Eur J Public Health. 2002;12:104. [Google Scholar]
- 16.Tijhuis MA, Flap HD, Foets M, Groenwegen PP. Social support and stressful events in two dimensions: life events and illness as an event. Soc Sci Med. 1995;40:1513–1526. doi: 10.1016/0277-9536(94)00276-y. [DOI] [PubMed] [Google Scholar]
- 17.Pescosolido BA. Beyond rational choice: the social dynamics of how people seek help. Am J Sociol. 1992;97:1096–1138. [Google Scholar]
- 18.Wilcox-Gok VL. Sibling data and the family background influence on child health. Med Care. 1983;21:630–638. doi: 10.1097/00005650-198306000-00005. [DOI] [PubMed] [Google Scholar]