Abstract
Recent developments in imaging science and treatment-planning software allow for accurate postimplant dosimetric assessment in all patients after prostate brachytherapy. This article reviews the available data correlating cancer control and morbidity with dosimetric quantifiers obtained from postimplant dosimetric assessment after prostate brachytherapy. Continued collection of dosimetric data in patients treated with prostate brachytherapy will allow for further refinements in the technique, leading to continued high rates of cure with increasingly lower rates of morbidity.
Key words: Prostate brachytherapy, Dosimetry, Iodine-125, Palladium-103, Morbidity, Biochemical relapse-free survival
Prostate brachytherapy (PB) has been performed for nearly a century. The early methods were, in retrospect, crude, and the assessment of implant quality was nonexistent. Whitmore and Carlton popularized PB in the 1960s and 1970s using a retropubic approach. Despite initial enthusiasm for this technique, long-term results were disappointing.1 Careful examination of the dosimetric results with the retropubic method indicated that in many cases the desired source placement was not optimal. In fact, using data from the retropubic era, Fuks and colleagues2 have established a relationship between the “adequacy” of PB and the eventual local control.
Holm and coworkers3 were the first investigators to combine ultrasoundbased source placement and a perineal template. The closed perineal method was further developed by Ragde and colleagues.4 The present widespread use of permanent PB is the result of prostate screening and improved technology that currently allows for an outpatient procedure that generally can be accomplished in 1 to 2 hours.
The modern technique of PB includes three components: treatment planning, placement of the sources, and an evaluation of the implant quality. In the early work of Ragde and colleagues,4 the three components were separated in time, but advances in imaging and treatmentplanning software have led to these components being compressed. In some centers, all three components are completed in the operating room at the same sitting.5
Two radioisotopes are in common use with PB: Iodine-125 (I-125) and Palladium-103 (Pd-103). Each of these isotopes possesses a low-dose rate and low energy relative to other isotopes used for brachytherapy in other clinical scenarios. The prescribed radiation dose differs according to isotope and whether brachytherapy is used alone (monotherapy) or combined with external beam radiation therapy (EBRT) (combined modality therapy). The low energy of the sources simplifies radiation protection precautions, and patients can be discharged from the hospital immediately after the implant procedure is completed. Sources can be “loose” or “stranded” (embedded in polyglactin 910 suture).
The radioactive sources are usually placed transperineally with some form of perineal template and ultrasound guidance. Two techniques of source deposition are commonly used. In the preloaded technique, brachytherapy needles with sources and spacers are prepared beforehand, and multiple sources are deposited with each needle placement. In the afterloading approach, a specially designed brachytherapy “gun” is used to deposit one source at a time. In either case, the needle or gun can be visualized and placed in the desired location. Close monitoring of the source deposition process allows the operator to recognize and adjust for changes that might occur intraoperatively (prostate gland movement, prostate gland swelling, source movement). Either method is amenable to the use of loose or stranded sources.
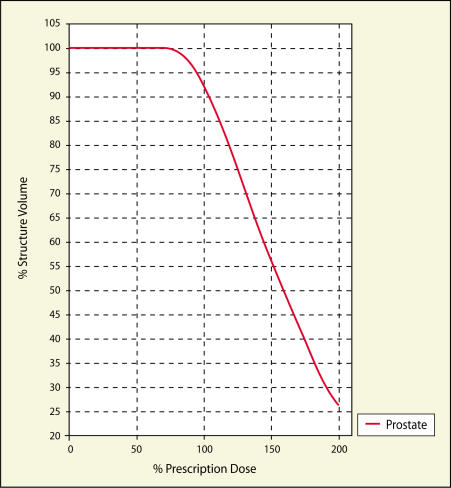
Some form of postimplant dosimetric assessment (PDA) is mandatory.6 In general, PDA involves importing images (computed tomography [CT], magnetic resonance, or ultrasound) into treatment-planning software and outlining the prostate gland and nearby structures (eg, urethra, rectum, penile bulb). On the basis of the delineation of the prostate and nearby structures and the location of the sources, isodose distributions can be calculated and dose-volume histograms (DVH) created (Figures 1 and 2). The most commonly used DVHs are cumulative DVHs, which graphically show the total volume (or percentage of total volume) of the target organ (eg, prostate) that receives a given radiation dose or greater.
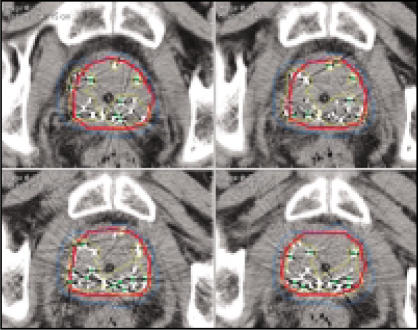
Figure 1.
Computed tomography (CT) images through the middle of the prostate gland. CT performed 2 hours after prostate brachytherapy. The red contour is the prostate outline. The blue line represents the 100% prescription isodose volume. The yellow line represents the 150% prescription isodose volume. Note how the 150% isodose line resides within the peripheral zone and does not include the entire urethra (Foley catheter in place).
Figure 2.
Cumulative dose-volume histogram for the case shown in Figure 1. Note that the volume of the prostate receiving 100% of prescription dose is approximately 92%, approximately 55% of the prostate receives 150% of the prescription dose, and approximately 25% of the prostate receives 200% of the prescription dose.
PDA Defined
For the purposes of this review, PDA based on CT images will be emphasized. A number of dosimetric quantifiers have been described.6 The most commonly reported include D90 and V100 (Table 1). D90 is the dose (usually reported in grays [Gy], but which can also be reported as a percentage of the prescription dose) that covers 90% of the prostate volume outlined on the postimplant CT images. V100 is the fractional volume of the prostate (usually reported as a percentage) that receives 100% of the prescription dose. It is also possible to report the dose received by the urethra, rectum, penile bulb, and other organs with a similar methodology. A number of dose uniformity and conformity parameters (target-volume ratio, dose-homogeneity index) have been calculated, but these will not be discussed further.
Table 1.
Definitions of Commonly Used Dosimetric Quantifiers Obtained from Postimplant Dosimetric Assessment
| Dosimetric Quantifier | Definition |
|---|---|
| D90 | Radiation dose delivered to 90% of the prostate |
| V100 | Volume of the prostate receiving 100% of the prescription dose |
| TVR | Target-volume ratio. Ratio of the prescription isodose volume to prostate volume |
| DHI | Dose-homogeneity index. Volume within the prostate that receives 100% to 150% of the prescription dose, divided by the volume of the prostate |
Before discussing the results of PDA, a few comments on the timing of PDA are warranted. CT-based PDA has been performed at numerous times after PB.6 Some reports include PDA performed early, at day 0 (same day as PB) or day 1 (1 day after PB), whereas other reports describe PDA performed 14 to 30 days after PB. Advocates of early PDA argue that it is impractical to have patients return for PDA 30 days after PB if they must travel from a long distance and that the early assessment provides timely feedback so that additional therapy (reimplantation or supplemental EBRT) can be added if the prostate is underdosed. The argument for PDA performed 14 to 30 days after PB is that the results are more reliable and consistent, because most prostate swelling has diminished by that time. Time-averaged weighting factors and computer modeling have determined that the best interval for PDA is approximately 14 days for Pd-103 implants and 30 days for I-125 implants.7,8 It is important to note when PDA was performed, because the results are predictably different depending on the timing of PDA. Specifically, PDA obtained early (day 0 or 1) will underestimate prostate coverage by approximately 10% compared with PDA obtained 30 days after PB.7,8
The Relationship of Dosimetry to Cancer Control
Given the observation that the dosimetric adequacy of retropubic implants was associated with the likelihood of local control, there was every expectation that the same relationship would be observed in patients treated with the closed retropubic approach. The available literature that examines this relationship is summarized below.
Stock and collegues9 from the Mount Sinai Hospital in New York, NY were the first to report a doseresponse relationship in men treated with I-125 and the transperineal approach. They studied 134 patients treated with I-125 alone without supplemental EBRT or androgen deprivation therapy. The median followup was 32 months (range 12–74 mo), and the authors examined the relationship between biochemical relapse-free survival (BRFS) and D90, calculated from PDA performed 1 month after PB. Biochemical recurrence was defined as two consecutive rises in serum prostate-specific antigen (PSA) or a PSA nadir greater than 1.0 ng/mL. The calculated D90 values had a very wide range (26.8–256.3 Gy), with a median of 140.8 Gy. The authors observed improved BRFS as the calculated D90 increased. Specifically, the authors reported 4-year BRFS of 92% in patients with D90 of at least 140 Gy, compared with a 4-year BRFS of 68% in patients with a D90 of less than 140 Gy (P = .02). When patients were grouped according to pretreatment PSA levels, the improved BRFS with higher doses was observed only in patients with a pretreatment PSA level greater than 10 ng/mL (4-year BRFS of 51% vs 100% for D90 < 140 Gy vs D90 ≥ 140 Gy, P = .009). In patients with pretreatment PSA of less than or equal to 10 ng/mL, no dose effect was observed (4-year BRFS of 82% vs 88% for D90 < 140 Gy vs D90 ≥ 140 Gy, P = .29).
The Mount Sinai group10 has recently updated its results examining the dose-response relationship. In this study, 243 men treated with PB alone (I-125 and Pd-103) between 1990 and 1996 were followed for a median of 75 months. The majority of tumors (78%) were graded as Gleason score 6 or less. Nearly 90% of men had pretreatment PSA levels less than 20 ng/mL. Sixty percent of these men received androgen deprivation therapy for 6 months in addition to PB, but none received supplemental EBRT. The American Society for Therapeutic Radiology and Oncology (ASTRO) consensus definition was used to define biochemical recurrence. The previously observed dose-response relationship was observed when all patients were included in the analysis. The estimated 8-year BRFS was 82% in those patients (n = 145) with D90 ≥ 140 Gy, compared with 68% in those patients (n = 98) with D90 < 140 Gy (P = .007). In patients with favorable features (stage < T2b, PSA < 10 ng/mL, and Gleason score < 7), the estimated 8-year BRFS was 94% in the optimaldose group, compared with 75% in the suboptimal-dose group (P = .02).
Potters and coworkers11 examined 719 men treated between 1995 and 1999 with PB with I-125 and Pd-103, with or without supplemental EBRT. Of these men, 60% had nonpalpable disease, and more than 90% had a Gleason score of less than 8. The median PSA level was 8.0 ng/mL. Two hundred and fifty men (34.8%) were treated with neoadjuvant androgen deprivation therapy. Biochemical recurrence was defined according to the ASTRO consensus definition, and the investigators examined the relationship between BRFS and dosimetric quantifiers (D90, V100) obtained from CT scans performed 2 to 3 weeks after PB. The median follow-up was 30 months (range 7–71 mo). The only dose-response relationship observed was at greater than or equal to a D90 of 90% of the prescription dose. In those patients with D90 < 90% of the prescription dose, the 4-year BRFS was 80.4%, compared with a 4-year BRFS of 92.4% (P = .001) in those men with D90 ≥ 90% of the prescription dose. No statistically significant cutpoints for V100 were observed. The importance of dose was independent of isotope and the use of androgen deprivation therapy. In patients treated with supplemental EBRT, however, there was no statistically significant evidence for a dose effect.
Potters and colleagues12 recently updated their series. In 883 men treated with PB between 1992 and 1998, the dose-response relationship was again analyzed. All patients had PDA performed 2 to 6 weeks after PB, and D90 was calculated. The median follow-up had increased to 55 months (range 3-125 mo). The 10-year estimate of BRFS was 79.1% according to the ASTRO consensus definition. After multivariate analysis, the most important predictor of BRFS was D90. The authors did not provide any cutpoints for D90, thus making it difficult to interpret the doseresponse relationship. Specifically, this updated information supports a positive linear relationship between D90 and BRFS, but it is impossible to know whether a threshold value exists.
One of the most recent reports of a dose-response relationship concerned men enrolled in a yet-to-be completed randomized trial comparing the efficacy of I-125 and Pd-103 in patients with favorable-risk prostate cancer.13 Wallner and colleagues13 reported the preliminary BRFS of 115 patients in whom isotope selection was determined by a random process. PDA was performed within 2 to 4 hours of PB, much earlier than in the studies outlined above. The dosimetric quantifiers analyzed included D90 and V100. Biochemical recurrence was defined according to a nadir definition (whereby the PSA level must be < 0.5 ng/mL for the patient to be considered disease-free). The median follow-up was 2.9 years (range 2–4 y). Three-year BRFS was not different according to isotope. Significant dose-response relationships, however, were observed. In patients with a D90 ≥ 100% of the prescription dose, the estimated 3-year BRFS was 97%, compared with 82% if the D90 was < 100% (P = .01). Similarly, if the V100 was ≥ 90% of the prescription dose, the 3-year estimate of BRFS was 97%, compared with 87% if the V100 was < 90% of the prescription dose (P = .01). The dose effect was observed with both isotopes.
Considering the data outlined above, a few summary statements are in order. It is clear that a dose-response relationship exists after treatment with PB; in other words, dosimetry matters. Most, but not all, series observe that D90 correlates better with BRFS than V100. The specifics of this relationship are more problematic. The cutpoints that authors have reported differ slightly between reports: D90 ≥ 140 Gy for I-125, or D90 ≥ 90% of prescription dose, or D90 ≥ 100% of prescription dose. This lack of consistency precludes any definitive statements about what constitutes a “good” versus a “bad” implant. Further prospective data from multicenter trials are required.
The Relationship Between Dosimetry and Morbidity
Just as authors have attempted to correlate dosimetric quantifiers with cancer control outcome, there is tremendous interest in examining the relationship between radiation dose delivered to nearby normal tissues and the development of morbidity. Morbidity after PB is typically manifest in three systems: urinary, bowel, and sexual. The next few paragraphs will focus on dosimetric quantifiers that have been reported to affect brachytherapy-related morbidity.
Urinary Morbidity
Urinary morbidity is the most commonly reported toxicity after PB. Most patients will have some degree of urinary symptoms (nocturia, dysuria, urgency, or hesitancy) for several weeks after PB. The published rates of acute urinary retention range from 2% to 35%, with most series reporting rates of approximately 10%.14
The relationship between urethral dose and acute urinary morbidity is of great interest. An early report concluded that increased D90 doses were associated with increased acute urinary morbidity (measured by International Prostate Symptom Score [IPSS]).15 In more recent reports, no relationship between urethral dose and urinary morbidity has been observed.14,16 Modern treatment-planning and operative techniques allow practitioners to keep the urethral dose well below this threshold (< 150% in most cases), and this might be why a stronger relationship between acute urinary morbidity and urethral dose has not been observed. Multiple confounding variables, including different philosophies regarding the use of intermittent self-catheterization and inconsistent use of α-blockers, likely muddle any association.
The most commonly reported late genitourinary morbidity after PB is urethral stricture. The reported incidence ranges from 5% to 12%. Essentially all reported strictures have occurred in the bulbomembranous urethra. The number of reports is few, but at least one report suggests that stricture formation might be related to urethral dose. In the report by Merrick and colleagues,17 factors predicting the development of urethral stricture included the magnitude and extent of high-dose regions within the prostate, the mean membranous urethral dose, and the dose delivered 20 mm distal to the prostate apex on CT-based PDA. In a very early study, Wallner and coworkers18 found an association between late urinary morbidity and urethral dose but only at very high urethral doses (< 250% of the matched peripheral dose). In a more recent study, Stock and Stone19 examined the relationship between prostate dose and the development of late urinary morbidity. This study included 276 patients treated with I-125 and followed for a median of 34 months (range 18–108 mo). Chronic urinary morbidity was measured by comparing pretreatment IPSS with the last available IPSS. The authors reported worsening IPSSs in those men whose D90 was greater than 180 Gy and encouraged practitioners to attempt to keep the D90 below this level.
Rectal Morbidity
Rectal morbidity is less common than urinary morbidity after PB. The rate of self-limited rectal bleeding or proctitis is generally less than 10%. The development of rectal fistula is rare. No patient- or tumor-related variables have been consistently associated with rectal morbidity. Rectal morbidity seems to be correlated with one treatment-related variable, namely, radiation dose to the rectal wall.
Three articles have identified a dose-volume effect for rectal morbidity after PB. In the earliest report, Wallner and colleagues18 calculated anterior rectal wall surface area doses and found a positive relationship between increasing surface area dose and rectal morbidity. Specifically, the average area of the rectal wall irradiated to greater than 100 Gy was greater (17 mm2 vs 11 mm2) in those men that developed Radiation Therapy Oncology Group grade 1 to 2 complications compared with those patients without complications. Merrick and colleagues20 performed rigorous rectal dosimetry on 45 men treated with I-125 or Pd-103 with or without supplemental EBRT. They found that the incidence of self-limited proctitis was low (9%), and no patient developed fistula. The number of events was small, thus limiting the power of the study, but the authors concluded that the length of rectal mucosa receiving 100% and 120% of the prescription dose should be kept to 10 mm and 5 mm, respectively. The Mount Sinai groupB21 has also reported that grade 2 rectal morbidity after PB is associated with increased rectal volume receiving the prescription radiation dose. In their experience, the proctitis rate rose from 0% if the rectal volume receiving the prescription dose was ≤ 0.8 cm3 to 25.5% if the rectal volume receiving prescription dose was > 2.3 cm3.
Sexual Function
The rates of erectile dysfunction after PB range from 6% to 90%. This wide range is likely a consequence of patient selection, length of follow-up, and methods of defining erectile dysfunction (physician reports vs selfadministered questionnaires). Despite initial optimistic reports, the largest series indicate that approximately 40% to 50% of men will develop erectile dysfunction within 5 years of PB.22,23
The physiologic mechanism for PB-induced erectile dysfunction has yet to be completely understood. Two anatomic structures have produced the most interest: the neurovascular bundles (NVB) and the penile bulb. Two studies examining the dose to the NVB failed to show a relationship between dose to the NVB and the development of erectile dysfunction.24,25 The available data on dose to the penile bulb are conflicting. In one report by Merrick and collegues,25 patients who developed erectile dysfunction had higher doses to the penile bulb and the crura. The authors recommend limiting the dose to the penile bulb such that less than 50% of the penile bulb receives no more than 40% of the prescription dose. Kiteley and investigators24 at Wake Forest University, Winston-Salem, NC were not able to reproduce the findings of Merrick’s group.
Methods to Improve Dosimetry
Given the observation that dosimetric quantifiers predict treatment success, it should come as no surprise that clinicians would be interested in methods to ensure that quality postimplant dosimetry can be achieved on a consistent basis. Perhaps the most important predictor of quality dosimetry is experience with the PB technique. Lee and collegues26 found evidence for a learning curve with PB and observed that consistently good postimplant dosimetry could be achieved within approximately 30 implant procedures.
Specific technical methods to improve dosimetry have run the gamut from the simple to the complex. Baird and coworkers27 observed that placing two marker seeds before placement of sources resulted in better D90 values. Stock and collegues28 observed that the use of a dualphase ultrasound probe resulted in fewer patients with low D90 values compared with the use of a mechanical sector probe. Zelefsky and others29 have reported that intraoperative computer-optimized treatment planning was associated with improved dosimetric outcomes.
Another approach to improving dosimetry is to use a unique radiation delivery device, namely sources embedded in polyglactin 910 suture (RAPID Strand™, Oncura, Inc., Plymouth Meeting, PA). RAPID Strand consists of 10 Model 6711 OncoSeeds (Oncura), spaced at a fixed distance of 1 cm, embedded within polyglactin 910 absorbable suture (Figure 3). The stiffened suture material holds the sources in place to minimize source movement and optimize the intended radiation dose distribution. Studies of intramuscular implantation in rats show that non-stiffened suture material containing I-125 sources are minimally absorbed until about the 40th postoperative day, but absorption is essentially complete between 60 and 90 days postoperatively.
Figure 3.

RAPID Strand™ (Oncura, Inc., Plymouth Meeting, PA) radiation delivery device, consisting of 10 I-125 sources, spaced at a fixed distance of 1 cm, embedded within polyglactin 910 absorbable suture.
There is at least a theoretical argument that the fixed relationship of the sources embedded in suture (SES) will result in a reduction in spacing errors, thus leading to improved postimplant dosimetry.30 In a large study examining the spatial distribution of dose within the prostate gland, the region of the prostate reported most likely to be underdosed was the anterior base.31 Anecdotal and recently published experience indicates that the sources most likely to migrate are those placed on the periphery of the prostate or those placed anteriorly (near the dorsal venous plexus).32 Given that the use of stranded sources results in 1) lower rates of source migration; and 2) more consistent source placement by decreasing spacing errors, it is plausible that the use of stranded sources might be associated with improved postimplant dosimetry.
Lee and others33 at Wake Forest University have examined a small group of patients to determine whether the use of SES is associated with improved postimplant dosimetry when compared with the use of loose sources. These clinicians had been performing prostate implants for approximately 3 years using exclusively loose sources. In May 2000, the use of SES was incorporated into the treatment procedure. In this study, the investigators compared postimplant dosimetric quantifiers of the first 20 patients treated with SES to those of the last 20 patients treated with loose sources. The patient and treatment characteristics of the two groups were not different, with the exception that the mean prostate volume of the patients treated with SES was slightly smaller (33.74 vs 39.55 cm3, P = .0474). The dosimetric quantifiers for each group are listed in Table 2. It is clear that the V100 and D90 are superior in the group treated with SES. Given the retrospective nature of the comparisons, the result can only be considered hypothesis-generating, and definitive statements require a randomized trial. Randomized trials of loose seeds compared with SES are ongoing.
Table 2.
Dosimetric Quantifiers for 40 Patients, Stratified by Source Type
| Variable | LS (n = 20) | SES (n = 20) | P* |
|---|---|---|---|
| V100 | 86.5 (3.7) | 94.1 (2.9) | <.0001 |
| V90 | 90.4 (3.2) | 96.6 (2.2) | <.0001 |
| V80 | 94.1 (2.6) | 98.5 (1.3) | <.0001 |
| D90 | 132 (11) Gy | 164 (17) Gy | <.0001 |
| No. (%) with D90 >140 Gy | 7/20 (35%) | 20/20 (100%) | <.0001 |
Data are presented as mean (standard deviation), unless otherwise specified LS, loose sources; SES, sources embedded in suture; V100, V90, V80, volumes of the prostate receiving 100%, 90%, and 80%, respectively, of the prescription dose; D90, radiation dose delivered to 90% of the prostate.
Data from Lee et al.33.
Two-sided, LS vs SES.
Future Directions
The long-term efficacy of PB is no longer in doubt. For the next several years, clinical focus will be on techniques that reduce morbidity without compromising cancer control. Analogous to the development of the anatomical prostatectomy described by Walsh, radiation oncologists and urologists owe it to their patients to better understand the relationships between radiation dose delivery and PB-related morbidity. As more information on the dose-morbidity relationship is collected, further refinements of PB should lead to better patient outcomes.
Main Points.
In prostate brachytherapy (PB), some form of postimplant dosimetric assessment (PDA) is mandatory.
The most commonly reported dosimetric quantifiers include D90 (the dose that covers 90% of the prostate volume outlined on postimplant computed tomography images) and V100 (the fractional volume of the prostate that receives 100% of the prescription dose).
Results from several studies seeking to correlate dosimetric quantifiers with cancer control outcomes make it clear that a doseresponse relationship exists after treatment with PB; in other words, dosimetry matters.
One approach to improving dosimetry is the use of a unique radiation delivery device, namely sources embedded in polyglactin 910 suture (RAPID Strand); the stiffened suture material holds the sources in place to minimize source movement and optimize the intended radiation dose distribution.
In a retrospective study that compared postimplant dosimetric quantifiers of 20 patients treated with sources embedded in suture (SES) with those of 20 patients treated with loose sources, V100 and D90 were superior in the group treated with SES. Randomized trials of loose seeds compared with SES are ongoing.
References
- 1.Zelefsky MJ, Whitmore WF., Jr. Long-term results of retropubic permanent 125iodine implantation of the prostate for clinically localized prostatic cancer. J Urol. 1997;158:23–29. doi: 10.1097/00005392-199707000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Fuks Z, Leibel SA, Wallner KE, et al. The effect of local control on metastatic dissemination in carcinoma of the prostate: long-term results in patients treated with 125I implantation. Int J Radiat Oncol Biol Phys. 1991;21:537–547. doi: 10.1016/0360-3016(91)90668-t. [DOI] [PubMed] [Google Scholar]
- 3.Holm HH, Juul N, Pedersen JF, et al. Transperineal 125iodine seed implantation in prostatic cancer guided by transrectal ultrasonography. J Urol. 1983;130:283–286. doi: 10.1016/s0022-5347(17)51108-8. [DOI] [PubMed] [Google Scholar]
- 4.Ragde H, Blasko JC, Grimm PD, et al. Brachytherapy for clinically localized prostate cancer: results at 7- and 8-year follow-up. Semin Surg Oncol. 1997;13:438–443. doi: 10.1002/(sici)1098-2388(199711/12)13:6<438::aid-ssu8>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 5.Nag S, Ciezki JP, Cormack R, et al. Intraoperative planning and evaluation of permanent prostate brachytherapy: report of the American Brachytherapy Society. Int J Radiat Oncol Biol Phys. 2001;51:1422–1430. doi: 10.1016/s0360-3016(01)01616-9. [DOI] [PubMed] [Google Scholar]
- 6.Nag S, Bice W, DeWyngaert K, et al. The American Brachytherapy Society recommendations for permanent prostate brachytherapy postimplant dosimetric analysis. Int J Radiat Oncol Biol Phys. 2000;46:221–230. doi: 10.1016/s0360-3016(99)00351-x. [DOI] [PubMed] [Google Scholar]
- 7.Prestidge BR, Bice WS, Kiefer EJ, Prete JJ. Timing of computed tomography-based postimplant assessment following permanent transperineal prostate brachytherapy. Int J Radiat Oncol Biol Phys. 1998;40:1111–1115. doi: 10.1016/s0360-3016(97)00947-4. [DOI] [PubMed] [Google Scholar]
- 8.Yue N, Dicker AP, Nath R, Waterman FM. The impact of edema on planning 125I and 103Pd prostate implants. Med Phys. 1999;26:763–767. doi: 10.1118/1.598585. [DOI] [PubMed] [Google Scholar]
- 9.Stock RG, Stone NN, Tabert A, et al. A doseresponse study for I-125 prostate implants. Int J Radiat Oncol Biol Phys. 1998;41:101–108. doi: 10.1016/s0360-3016(98)00006-6. [DOI] [PubMed] [Google Scholar]
- 10.Kollmeier MA, Stock RG, Stone N. Biochemical outcomes after prostate brachytherapy with 5-year minimal follow-up: importance of patient selection and implant quality. Int J Radiat Oncol Biol Phys. 2003;57:645–653. doi: 10.1016/s0360-3016(03)00627-8. [DOI] [PubMed] [Google Scholar]
- 11.Potters L, Cao Y, Calugaru E, et al. A comprehensive review of CT-based dosimetry parameters and biochemical control in patients treated with permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2001;50:605–614. doi: 10.1016/s0360-3016(01)01473-0. [DOI] [PubMed] [Google Scholar]
- 12.Potters L, Huang D, Calugaru E, et al. Importance of implant dosimetry for patients undergoing prostate brachytherapy. Urology. 2003;62:1073–1077. doi: 10.1016/j.urology.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Wallner K, Merrick G, True L, et al. 125I versus 103Pd for low-risk prostate cancer: preliminary PSA outcomes from a prospective randomized multicenter trial. Int J Radiat Oncol Biol Phys. 2003;57:1297–1303. doi: 10.1016/s0360-3016(03)01448-2. [DOI] [PubMed] [Google Scholar]
- 14.Crook J, McLean M, Catton C, et al. Factors influencing risk of acute urinary retention after TRUS-guided permanent prostate seed implantation. Int J Radiat Oncol Biol Phys. 2002;52:453–460. doi: 10.1016/s0360-3016(01)02658-x. [DOI] [PubMed] [Google Scholar]
- 15.Desai J, Stock RG, Stone NN, et al. Acute urinary morbidity following I-125 interstitial implantation of the prostate gland. Radiat Oncol Investig. 1998;6:135–141. doi: 10.1002/(SICI)1520-6823(1998)6:3<135::AID-ROI4>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 16.Brown D, Colonias A, Miller R, et al. Urinary morbidity with a modified peripheral loading technique of transperineal (125)i prostate implantation. Int J Radiat Oncol Biol Phys. 2000;47:353–360. doi: 10.1016/s0360-3016(00)00433-8. [DOI] [PubMed] [Google Scholar]
- 17.Merrick GS, Butler WM, Tollenaar BG, et al. The dosimetry of prostate brachytherapy-induced urethral strictures. Int J Radiat Oncol Biol Phys. 2002;52:461–468. doi: 10.1016/s0360-3016(01)01811-9. [DOI] [PubMed] [Google Scholar]
- 18.Wallner K, Roy J, Harrison L. Dosimetry guidelines to minimize urethral and rectal morbidity following transperineal I-125 prostate brachytherapy. Int J Radiat Oncol Biol Phys. 1995;32:465–471. doi: 10.1016/0360-3016(94)00599-G. [DOI] [PubMed] [Google Scholar]
- 19.Stock RG, Stone NN. Importance of postimplant dosimetry in permanent prostate brachytherapy. Eur Urol. 2002;41:434–439. doi: 10.1016/s0302-2838(02)00018-0. [DOI] [PubMed] [Google Scholar]
- 20.Merrick GS, Butler WM, Dorsey AT, et al. Rectal dosimetric analysis following prostate brachytherapy. Int J Radiat Oncol Biol Phys. 1999;43:1021–1027. doi: 10.1016/s0360-3016(98)00486-6. [DOI] [PubMed] [Google Scholar]
- 21.Snyder KM, Stock RG, Hong SM, et al. Defining the risk of developing grade 2 proctitis following 125I prostate brachytherapy using a rectal dose-volume histogram analysis. Int J Radiat Oncol Biol Phys. 2001;50:335–341. doi: 10.1016/s0360-3016(01)01442-0. [DOI] [PubMed] [Google Scholar]
- 22.Merrick GS, Butler WM, Galbreath RW, et al. Erectile function after permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2002;52:893–902. doi: 10.1016/s0360-3016(01)02675-x. [DOI] [PubMed] [Google Scholar]
- 23.Stock RG, Kao J, Stone NN. Penile erectile function after permanent radioactive seed implantation for treatment of prostate cancer. J Urol. 2001;165:436–439. doi: 10.1097/00005392-200102000-00020. [DOI] [PubMed] [Google Scholar]
- 24.Kiteley RA, Lee WR, de Guzman AF, et al. Radiation dose to the neurovascular bundles or penile bulb does not predict erectile dysfunction after prostate brachytherapy. Brachytherapy. 2002;1:90–94. doi: 10.1016/s1538-4721(02)00018-1. [DOI] [PubMed] [Google Scholar]
- 25.Merrick GS, Wallner KE, Butler WM. Management of sexual dysfunction after prostate brachytherapy. Oncology (Huntingt) 2003;17:52–62. [PubMed] [Google Scholar]
- 26.Lee WR, deGuzman AF, Bare RL, et al. Postimplant analysis of transperineal interstitial permanent prostate brachytherapy: evidence for a learning curve in the first year at a single institution. Int J Radiat Oncol Biol Phys. 2000;46:83–88. doi: 10.1016/s0360-3016(99)00359-4. [DOI] [PubMed] [Google Scholar]
- 27.Baird MC, Holt RW, Selby TL. Improvement of transperineal implant dosimetry by intraoperative cystoscopic confirmation of prostate anatomy. J Urol. 2000;164:406–410. [PubMed] [Google Scholar]
- 28.Stock RG, Stone NN, Kao J, et al. The effect of disease and treatment-related factors on biopsy results after prostate brachytherapy: implications for treatment optimization. Cancer. 2000;89:1829–1834. doi: 10.1002/1097-0142(20001015)89:8<1829::aid-cncr25>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 29.Zelefsky MJ, Yamada Y, Cohen G, et al. Postimplantation dosimetric analysis of permanent transperineal prostate implantation: improved dose distributions with an intraoperative computer-optimized conformal planning technique. Int J Radiat Oncol Biol Phys. 2000;48:601–608. doi: 10.1016/s0360-3016(00)00655-6. [DOI] [PubMed] [Google Scholar]
- 30.Roberson PL, Narayana V, McShan DL, et al. Source placement error for permanent implant of the prostate. Med Phys. 1997;24:251–257. doi: 10.1118/1.598058. [DOI] [PubMed] [Google Scholar]
- 31.Sidhu S, Morris WJ, Spadinger I, et al. Prostate brachytherapy postimplant dosimetry: a comparison of prostate quadrants. Int J Radiat Oncol Biol Phys. 2002;52:544–552. doi: 10.1016/s0360-3016(01)02672-4. [DOI] [PubMed] [Google Scholar]
- 32.Di Muzio N, Longobardi B, Losa A, et al. Seed migration in prostate brachytherapy: a re-implant case report. Br J Radiol. 2003;76:913–915. doi: 10.1259/bjr/14541259. [DOI] [PubMed] [Google Scholar]
- 33.Lee WR, deGuzman AF, Tomlinson SK, McCullough DL. Radioactive sources embedded in suture are associated with improved postimplant dosimetry in men treated with prostate brachytherapy. Radiother Oncol. 2002;65:123–127. doi: 10.1016/s0167-8140(02)00305-5. [DOI] [PubMed] [Google Scholar]