Abstract
Despite dramatic and recently accelerated advances in the reduction of morbidity linked to radical prostatectomies, significant short- and long-term morbidity is still associated with this surgical procedure. Currently both surgical and nonsurgical minimally invasive options are available for men with clinically localized prostate cancer, including laparoscopic and robotic radical prostatectomy, brachytherapy, and cryosurgical ablation of the prostate, with others, such as high intensity focused ultrasound, under investigation. In continued efforts to improve patient outcomes and to tailor treatment options to individual patient circumstances, nomograms have been developed and are increasingly being used by physicians and patients, alike, to guide therapeutic choices at each stage of disease. This tool predicts the possibility of successful treatment for the patient based on factors such as prostate-specific antigen levels, clinical stage of disease, and biopsy results. The current and future development, design, availability, and use of nomograms is described along with the historic and newer minimally invasive treatment options for prostate cancer.
Key words: Localized prostate cancer, Minimally invasive therapy, Minimally invasive surgery, Brachytherapy, Cryotherapy, Robotic surgery, Nomograms, Prediction tools
Even with the dramatic reduction in morbidity of radical prostatectomy, beginning in 1982 with the development of the anatomic nerve-sparing technique by Patrick Walsh1 and accelerated in the past decade by contributions from many others, significant short- and long-term morbidity continues to be associated with this surgical procedure. While moderate to severe incontinence is an uncommon consequence of radical prostatectomy, more subtle reductions in overall urinary quality of life often persist throughout the first year after surgery.2,3 Furthermore, erectile dysfunction remains a difficult problem for patients who have undergone a radical prostatectomy. Even under the best of circumstances, erectile function may not fully return for 12 to 24 months. Generalized surveys of erectile function in the free-living community suggest that as few as 30% of men regain potency after surgery.3,4 In the short-term, radical prostatectomy typically requires a 2- to 3-day hospital stay. Blood loss, although seldom requiring transfusion, causes most patients to leave the hospital with a hemoglobin level under 10 g/dL, a level associated with a decreased quality of life.5 A 7- to 14-day period of catheterization is required, and patients do not return to a normal work schedule for 3 to 6 weeks.
External beam radiation therapy (EBRT) does not offer much better results in terms of patient morbidity and inconvenience. Although advances associated with intensive modulated radiation therapy (IMRT) continue to be made, patients are inconvenienced by 7 weeks of daily therapy. The higher doses (≥ 81.0 Gy) now recommended for the primary treatment of clinically localized prostate cancer are associated with moderate short- and long-term morbidities. Patients are unlikely to experience significant urinary incontinence, although, long-term urinary quality of life is adversely affected by irritative symptoms2 and erectile dysfunction becomes an increasing problem posttherapy. More serious long-term complications such as radiation cystitis, while uncommon, are devastating problems to those few patients severely affected.
The continuing desire to improve these outcomes has led to the development of numerous minimally invasive treatment options for men with clinically localized prostate cancer, including laparoscopic and robotic radical prostatectomy, brachytherapy, and cryosurgical ablation of the prostate, with others, such as high intensity focused ultrasound (HIFU), under intensive investigation. Both patients and physicians have demonstrated a strong and growing interest in these minimally invasive treatment options. However, it is increasingly difficult for patients to obtain unbiased data on which to base their selection of therapy. It is well known that a patient’s treatment options are strongly influenced by the treating physician, ie, urologists typically recommend surgery and radiation oncologists typically recommend EBRT.6 This bias is likely to extend to the minimally invasive therapies as well, with the choices offered likely to be influenced to a large extent by the personal experience of the urologist. In addition to these biases, the lack of data from head-to-head clinical trials comparing various therapies has severely limited our ability to provide reliable comparative data on cancer control and quality-of-life outcomes. Published reports often provide only average outcomes for large groups of patients thought to be in similar risk categories, but in actuality patients within the same risk category often remain widely heterogeneous. Other impediments to decision-making based on “evidence-based medicine” are; 1) the difficulty most physicians experience in translating general knowledge and concepts into daily medical decision-making, 2) the excessive influence of anecdotal experience (the “last case” syndrome), and 3) the eroding trust within the patient-physician relationship associated with the influence of third parties, eg, insurers, the government.
Minimally Invasive Treatment: Options Currently Available
Minimally invasive treatments for patients with clinically localized prostate cancer include laparoscopic and robotic radical prostatectomy, brachytherapy, and cryosurgical ablation of the prostate. Of the surgical options, laparoscopic removal of the prostate gland offers the potential benefits of a minimally invasive approach to surgery. These benefits generally include reduced pain, shorter hospital stays, and a faster recovery, although a short-term benefit for prostatectomy patients over the standard open approach has not been clearly demonstrated. The advent of robotic technology has dramatically enhanced a surgeon’s abilities to perform minimally invasive surgery with precision and speed.7 With the da Vinci™ Surgical (robotic) System (Intuitive Surgical, Inc., Sunnyvale, CA), the surgeon is seated comfortably a few feet away from the patient at a control console, while an assistant stands by the operative table. Surgery is performed through tiny incisions, as in standard laparoscopic surgery. However, the robotic instruments, about the diameter of a pencil, have wrist-like maneuverability, allowing the surgeon to move them like his own hand, as opposed to standard laparoscopic instruments, which have a much more limited range of motion. Unlike visualization provided by standard laparoscopic surgery, the advanced optics of the robotic procedure allow the surgeon to view the operative field at high magnification, while maintaining a three-dimensional perspective. Finally, the dexterity of the surgeon’s hand is enhanced by the robotic system scaling motion to allow microsurgical movements unequaled with either open or standard laparoscopic surgical approaches. Results with robotic-assisted laparoscopic prostatectomy demonstrate a more rapid development of proficiency, even in surgeons not skilled in standard laparoscopy,8 and excellent cancer control and quality-of-life outcomes.9
Nonsurgical Approaches: Brachytherapy and Cryosurgical Ablation of the Prostate
The two nonsurgical, minimally invasive options for clinically localized prostate cancer are brachytherapy and cryotherapy. Brachytherapy, as with cryotherapy, suffered through an early period in which the technology of the therapy was insufficiently developed to allow high-quality cancer control and quality-of-life outcomes. Beginning in the 1970s, brachytherapy, initially using iodine-125 seeds implanted without imaging guidance through an open, retropubic approach, led to poor outcomes. Currently, however, better imaging, dosimetry planning, and seed technology have led to marked improvement in both cancer control and quality-of-life outcomes, leading to a resurgence in this therapeutic modality. Similarly, early results with cryotherapy were inadequate mostly because of underdeveloped technology. Third-generation cryotherapy has also now evolved into a standard, safe, and effective option for many patients requiring therapy.10
Published data have shaped perceptions regarding the selection of candidates for treatment with these novel modalities and the outcomes to be expected. Despite the controversy regarding equivalence with surgery, patients treated with brachytherapy for smaller volume, moderate or lower Gleason Score-disease have demonstrated excellent cancer control rates in studies including large numbers of treated patients.11 Brachytherapy as monotherapy, however, is not necessarily appropriate for higher grade (Gleason Score ≥ 7) disease because studies have shown cancer control rates inferior to those achieved with surgery or EBRT.12 Similarly, cryosurgical ablation of the prostate has been gaining acceptance as newer, “third-generation” technology has decreased the morbidity and increased the ease of use and effectiveness of therapy.10 Because cryosurgical ablation is more like surgery in that physical destruction of the tumor is the goal of therapy, patients with higher grade disease may in fact have better outcomes with cryosurgical ablation than with brachytherapy. Furthermore, both of these therapies are potential secondary salvage therapies for patients failing ERBT or primary brachytherapy.
Nomograms: Personalized Prediction of Treatment Outcomes
Given the disparity in physician opinions and the increase in the number of treatment options, validated tools that can predict the cancer control and quality-of-life outcomes for any therapeutic option for individual patients, taking into account a multitude of factors, would allow both patients and physicians to better tailor treatment decisions to individual circumstances. Nomograms are excellent tools for this purpose. A nomogram is a device or model that uses an algorithm or mathematical formula to predict the probability of an outcome, optimized for predictive accuracy.
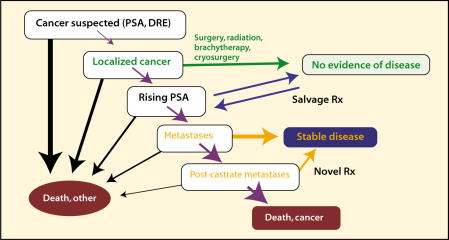
How can nomograms help a patient select a treatment optimized for his own circumstances? One can view prostate cancer as a succession of interconnected disease states, ranging from diagnosis to death (Figure 1). For each individual state, nomograms provide useful predictions that assist the patient in making decisions concerning his own illness. For instance, at the diagnosis stage, the patient must select a treatment that offers him both the highest possible chance of being cured, as well as a personally acceptable quality-of-life state. A nomogram considers the patient’s individualized clinical parameters and his selected treatment to predict the resulting chance of cancer control. Likewise, in the subsequent stage, patients who have undergone local definitive treatment can use the nomogram to predict the probability of avoiding disease progression. This allows the physician to identify patients at high risk for progression and therefore decide for or against adjuvant therapy, as well as to formulate a suitable follow-up schedule. Patients with a rising serum prostate-specific antigen (PSA) level after local definitive therapy can use nomograms to predict the results of salvage therapy. Because nomograms are able to provide standardized prognoses tailored to the patient’s specific clinical characteristics for each stage of his disease, they are a proven and valuable clinical tool for counseling patients.13
Figure 1.
Prostate cancer disease states. Diagram showing the clinical states in prostate cancer progressing from the suspected diagnosis of the disease based on evidence from prostate-specific antigen (PSA) levels or digital rectal examination (DRE) to death from either cancer or another cause, with the roles of salvage and novel therapies (Rx) indicated. Adapted with permission from Scher HI, Heller G. Clinical states in prostate cancer: toward a dynamic model of disease progression. Urology. 2000;55:323–327.
Quality of care in prostate cancer can be optimized only if clinicians are cognizant of the most recent methods for achieving an accurate prognosis. Because nomograms can be electronically based, they are easily updated to contain the most current information. They can be adapted for use on personal digital assistants and personal computers. These nomograms are available for free download and use by patients, physicians, or researchers in the home or office setting.14
Nomogram Development
Nomogram design incorporates a number of important considerations.15 First, a nomogram should discriminate between patients by predicting who will and who will not reach a particular endpoint (eg, prostate cancer progression after therapy). It also needs to produce predictions that will match results actually observed in general practice (calibration). Additionally, it must function consistently when applied to different cohorts and datasets (validation). The nomogram must base its prediction on a sufficient amount of data and specifically incorporate a sufficiently large proportion of cases that reach the relevant endpoint. It should also include variables that are statistically insignificant because a model containing only significant variables will produce narrowed, and thus inaccurate confidence intervals and make the nomogram appear to be more precise than it actually is. Simply counting risk factors/variables should likewise be avoided as this assumes that each separate variable holds the same amount of prognostic influence on the outcome, despite the fact that this is an unlikely representation of the realistic relationship between each variable and the final prognosis. Furthermore, this method requires the conversion of continuous variables into categorical variables, thereby removing information about the actual variable. Thus, the model becomes a risk-grouping system and decreases predictive accuracy.
Ideally, a predictive model should exhibit generalizability, or have the ability to repeatedly produce similarly accurate results when applied to a new, heterogeneous information matrix. Several factors can cause prognostic models to lose this ability, including using small datasets, using datasets that lack necessary information, incorrectly entering or removing missing records, and incorporating an unsuitable number of variables. For the greatest utility in a clinical setting, nomograms should employ parameters that are dependable, easy to use, and used on a consistent basis.
Brachytherapy Nomogram
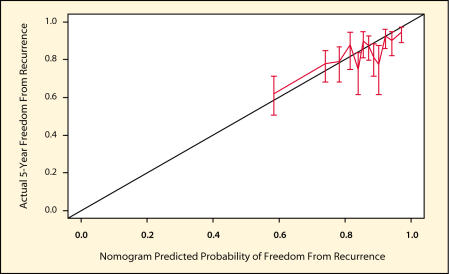
Using these principles, we have developed a number of prostate cancer-related nomograms to guide therapeutic choices at each stage of disease. For example, for patients with clinically localized prostate cancer, nomograms have been constructed and/or published in the peer-reviewed literature that predict outcomes with watchful waiting, radical prostatectomy,16–18 EBRT,19 and most recently, transperineal interstitial prostatic brachytherapy (TPIPB).20 We have developed a pretreatment nomogram that can predict the 5-year progression-free probability after TPIPB, without the use of adjuvant hormonal therapy (Figure 2). Predictor variables are pretreatment PSA level, clinical stage, biopsy Gleason sum, and the coadministration of EBRT. This model was based on 920 men, all of whom were treated for stage T1 and T2 prostate cancer at Memorial Sloan-Kettering Cancer Center in New York, NY with PSA failure defined by a modified version of the ASTRO (American Society for Therapeutic Radiology and Oncology) criteria. Patients with increasing PSA levels at last follow-up and in whom failure had not yet been documented were censored immediately before that PSA level but were not classified as failures. Also, the administration of adjuvant hormonal deprivation therapy, clinical evidence of disease progression (local, regional, or distant), or death from prostate cancer signaled treatment failure. External validation of 1827 men treated at the Seattle Prostate Institute demonstrated a c-index (probability of a correct prediction) of 0.61 (Figure 3), and further validation with 765 men treated at the Arizona Oncology Services yielded a c-index of 0.64.
Figure 2.
Brachytherapy nomogram. Pretreatment nomogram predicting 5-year progression-free probability after transperineal interstitial prostatic brachytherapy using pretreatment (PreTx) prostate-specific antigen (PSA) levels, biopsy (Bx) Gleason sum, clinical stage, and the coadministration of external beam radiation therapy as predictor variables. Reprinted with permission from Kattan MW, et al.20
Figure 3.
Brachytherapy nomogram applied to Seattle Prostate Institute study population of 1827 treated men with prostate cancer. External validation of a prostate cancer-related nomogram predicted probability of freedom from recurrence with a c-index (probability of a correct prediction) of 0.61. Reprinted with permission from Kattan MW, et al.20
This nomogram, together with previously published nomograms that predict outcomes after surgery and EBRT, allows physicians and patients to obtain individualized outcome predictions for any combination of prediction parameters, including PSA, Gleason Score, and clinical stage. These nomograms allow a more evidence-based estimation of the outcomes to be expected for each of these therapies, and allow the comparison of newer minimally invasive options with older, more standard choices for therapy, without the need for head-to-head clinical trials.
Nomograms to predict outcomes after cryotherapy are under construction. It is hypothesized, for example, that nomogram predictions would demonstrate superior cancer control outcomes for patients with high-grade cancer treated with cryotherapy than for patients treated with brachytherapy. This hypothesis will be tested when the cryotherapy nomogram is completed. With time, a “set” of nomograms that can predict outcomes for all possible choices at each stage of disease should improve the ability of patients and physicians to make therapeutic choices that maximize outcomes for patients, physicians, and the healthcare system.
Main Points.
Significant short- and long-term morbidity and inconvenience are still associated with radical prostatectomy, even after major and continually increasing improvements in this surgical procedure.
Numerous minimally invasive treatment options are currently available for men with clinically localized prostate cancer, including laparoscopic and robotic radical prostatectomy, brachytherapy, and cryosurgical ablation of the prostate.
Third-generation cryotherapy and brachytherapy have led to improved cancer control and quality-of-life outcomes and resurgence in the use of these therapeutic modalities.
Nomograms predict the possibility of successful treatment for the individual patient based on factors such as prostate-specific antigen levels, clinical stage of disease, and biopsy results.
Nomograms are increasingly popular predictive tools for physicians and patients to tailor treatment decisions depending on individual circumstances at each stage of disease.
Nomograms allow a more evidence-based estimate of outcomes expected for each therapeutic modality and allow for a comparison of newer minimally invasive treatment options with older, more standard therapies, without the need for head-to-head clinical trials.
References
- 1.Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol. 1982;128:492–497. doi: 10.1016/s0022-5347(17)53012-8. [DOI] [PubMed] [Google Scholar]
- 2.Penson DF, Litwin MS. Quality of life after treatment for prostate cancer. Curr Urol Rep. 2003;4:185–195. doi: 10.1007/s11934-003-0068-1. [DOI] [PubMed] [Google Scholar]
- 3.Litwin MS, Melmed GY, Nakazon T. Life after radical prostatectomy: a longitudinal study. J Urol. 2001;166:587–592. [see comment] [PubMed] [Google Scholar]
- 4.Stanford JL, Feng Z, Hamilton AS, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA. 2000;283:354–360. doi: 10.1001/jama.283.3.354. [see comment] [DOI] [PubMed] [Google Scholar]
- 5.Crawford J, Cella D, Cleeland CS, et al. Relationship between changes in hemoglobin level and quality of life during chemotherapy in anemic cancer patients receiving epoetin alfa therapy. Cancer. 2002;95:888–895. doi: 10.1002/cncr.10763. [see comment] [DOI] [PubMed] [Google Scholar]
- 6.Fowler FJ, Jr, McNaughton CM, Albertsen PC, et al. Comparison of recommendations by urologists and radiation oncologists for treatment of clinically localized prostate cancer. JAMA. 2000;283:3217–3222. doi: 10.1001/jama.283.24.3217. [see comment] [DOI] [PubMed] [Google Scholar]
- 7.Menon M, Shrivastava A, Tewari A, et al. Laparoscopic and robot assisted radical prostatectomy: establishment of a structured program and preliminary analysis of outcomes. J Urol. 2002;168:945–949. doi: 10.1016/S0022-5347(05)64548-X. [DOI] [PubMed] [Google Scholar]
- 8.Ahlering TE, Skarecky D, Lee D, Clayman RV. Successful transfer of open surgical skills to a laparoscopic environment using a robotic interface: initial experience with laparoscopic radical prostatectomy. J Urol. 2003;170:1738–1741. doi: 10.1097/01.ju.0000092881.24608.5e. [DOI] [PubMed] [Google Scholar]
- 9.Menon M, Tewari A, Baize B, et al. Prospective comparison of radical retropubic prostatectomy and robot-assisted anatomic prostatectomy: the Vattikuti Urology Institute experience. Urology. 2002;60:864–868. doi: 10.1016/s0090-4295(02)01881-2. [see comment] [DOI] [PubMed] [Google Scholar]
- 10.Han KR, Cohen JK, Miller RJ, et al. Treatment of organ confined prostate cancer with third generation cryosurgery: preliminary multicenter experience. J Urol. 2003;170(4 Pt 1):1126–1130. doi: 10.1097/01.ju.0000087860.52991.a8. [see comment] [DOI] [PubMed] [Google Scholar]
- 11.Ragde H, Korb L. Brachytherapy for clinically localized prostate cancer. Semin Surg Oncol. 2000;18:45–51. doi: 10.1002/(sici)1098-2388(200001/02)18:1<45::aid-ssu7>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 12.D’Amico AV, Whittington R, Malkowicz SB, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer [see comments] JAMA. 1998;280:969–974. doi: 10.1001/jama.280.11.969. [DOI] [PubMed] [Google Scholar]
- 13.Kattan MW. Nomograms are superior to staging and risk grouping systems for identifying highrisk patients: preoperative application in prostate cancer. Curr Opin Urol. 2003;13:111–116. doi: 10.1097/00042307-200303000-00005. [DOI] [PubMed] [Google Scholar]
- 14. [Accessed March 22, 2004];Prediction tools and prostatectomy nomogram predicting probability of prostate cancer recurrence. Available at: www.nomograms.org and at http://www.drslawin.com/nomogram.html.
- 15.Kattan MW. Comparison of Cox regression with other methods for determining prediction models and nomograms. J Urol. 2003;170(6 Pt 2):S6–S9. doi: 10.1097/01.ju.0000094764.56269.2d. discussion S10. [DOI] [PubMed] [Google Scholar]
- 16.Kattan MW, Eastham JA, Stapleton AM, et al. A preoperative nomogram for disease recurrence following radical prostatectomy for prostate cancer. J Natl Cancer Inst. 1998;90:766–771. doi: 10.1093/jnci/90.10.766. [DOI] [PubMed] [Google Scholar]
- 17.Kattan MW, Wheeler TM, Scardino PT. Postoperative nomogram for disease recurrence after radical prostatectomy for prostate cancer. J Clin Oncol. 1999;17:1499–1507. doi: 10.1200/JCO.1999.17.5.1499. [DOI] [PubMed] [Google Scholar]
- 18.Kattan MW, Shariat SF, Andrews B, et al. The addition of interleukin-6 soluble receptor and transforming growth factor beta1 improves a preoperative nomogram for predicting biochemical progression in patients with clinically localized prostate cancer. J Clin Oncol. 2003;21:3573–3579. doi: 10.1200/JCO.2003.12.037. [see comment] [DOI] [PubMed] [Google Scholar]
- 19.Kattan MW, Zelefsky MJ, Kupelian PA, et al. Pretreatment nomogram for predicting the outcome of three-dimensional conformal radiotherapy in prostate cancer. J Clin Oncol. 2000;18:3352–3359. doi: 10.1200/JCO.2000.18.19.3352. [DOI] [PubMed] [Google Scholar]
- 20.Kattan MW, Potters L, Blasko JC, et al. Pretreatment nomogram for predicting freedom from recurrence after permanent prostate brachytherapy in prostate cancer. Urology. 2001;58:393–399. doi: 10.1016/s0090-4295(01)01233-x. [DOI] [PubMed] [Google Scholar]