Abstract
The treatment of men with symptomatic benign prostatic hyperplasia (BPH) has shifted dramatically from surgery to drug therapy over the past decade. The revolution in BPH treatment began with the discovery of congenital 5α-reductase (5AR) deficiency, leading to the appreciation of 2 different androgenic hormones: testosterone, which mediates overt masculinization in the adult male, and dihydrotestosterone (DHT), which mediates prostatic growth, acne, facial beard, and male pattern baldness. Inhibition of DHT in adults results in prostatic shrinkage and symptomatic relief in many men, without the side effects seen with conventional androgen-deprivation therapy. The 5AR inhibitor drugs (finasteride and the dual inhibitor, dutasteride) are able to ablate the accumulation of intraprostatic DHT, the mechanism most responsible for prostate growth and maintenance. Not only may these drugs relieve symptoms, but they may also alter the natural history of the BPH process. Future indications for the 5ARI drugs could include chemoprevention of prostate cancer, prophylaxis of BPH-related complications, and treatment of BPH-associated hematuria.
Key words: Benign prostatic hyperplasia, Guevedoces, Dihydrotestosterone, 5α-reductase, Finasteride, Dutasteride
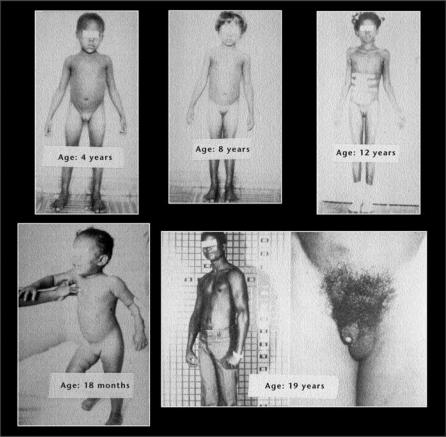
No one could have anticipated the revolution in prostate treatments that followed the discovery of pseudohermaphrodites in the Dominican Republic more than 30 years ago.1–4 Yet, the discovery of the Dominican “guevedoces”—literally “penis at 12” (years of age) (Figure 1)—helped lead the transformation of urology from a purely surgical specialty into a discipline centered on effective drug therapy and minimally invasive treatments. The chief legacy of the guevedoces is a class of drugs known as 5α-reductase inhibitors (5ARIs), the first of the “prostate pills.” Finasteride, the original 5ARI was approved in 1992.5 Other drugs followed, and the treatment approach to prostatic obstruction dramatically changed.
Figure 1.
Two classes of drugs now serve as the initial treatments of choice for most men with lower urinary tract symptoms (LUTS) and prostatic obstruction: 1) 5ARIs and 2) α-adrenergic receptor blocking agents. Whereas the latter (eg, alfuzosin, doxazosin, tamsulosin, and terazosin) offer quick relief of LUTS, only the former (finasteride or dutasteride) can alter the natural history of the disease, slow symptomatic progression, and prevent complications.6 Moreover, as the 5ARIs exert an atrophic effect on the prostate,7,8 without the deleterious systemic effects of conventional androgen deprivation, their potential utility may extend beyond relief of LUTS to prevention of prostatic diseases, both malignant9 and benign.10 What a natural mutation did to the guevedoces, pharmacologic intervention has extended to the mature prostate without effect on the external genitalia.
The safety record of the 5ARIs deserves special mention, as these drugs are intended for long-term use. Aside from a relatively low incidence of sexual dysfunction—difficult to differentiate from the usual effects of the aging process—the 5ARIs are among the most benign treatments for any chronic condition. Thus, finasteride and dutasteride deprive the prostate of androgenic stimulation without causing major sexual dysfunction, osteoporosis, anemia, muscular atrophy, or hot flashes—all expected consequences of conventional androgen deprivation (ie, medical or surgical castration). This advantage is conferred on the 5ARIs because inhibition of the enzyme results only in lowering the prostatic concentration of dihydrotestosterone (DHT), the principle androgenic stimulus within the gland, while leaving serum testosterone levels normal or even slightly elevated by about 10% to 20% as a result of the enzymatic block. DHT, not testosterone, is the major intraprostatic androgen, and only DHT is suppressed by 5ARIs11–13 (Figure 2). Hence, intervention with a 5ARI is a method that safely deprives the prostate of one of its primary growth stimuli, shrinks the gland, relieves symptoms, and lowers the risk of disease progression and complications.5,14,15 The different functions of testosterone and DHT are shown in Table 1.
Figure 2.
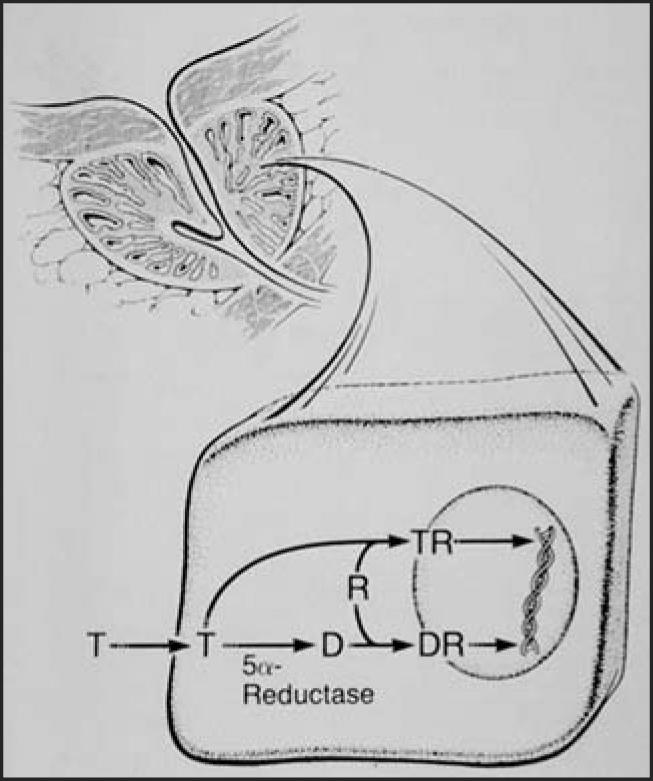
Within prostate cells, testosterone (T) is converted to dihydrotestosterone (D or DHT), which is the major intraprostatic androgen, binding preferentially to androgen receptors (R) to effect DNA synthesis. In the prostate, tissue DHT levels are some 10 times higher than T levels, just the opposite of serum levels.
Table 1.
Functions of the 2 Androgenic Hormones
| Testosterone |
|
| Dihydrotestosterone |
|
Widespread adoption of 5ARI treatment has been somewhat hindered because treatment benefit is not uniformly overt or immediate in all men. Two factors have recently emerged to mitigate that hindrance. First is the advent of dutasteride, a drug, which, in comparison with the original 5ARI finasteride, is more powerful via dual inhibition of both 5α-reductase (5AR) isoenzymes while being equally safe.14,15 Second is the increasing appreciation for disease prevention.9,10 A comparison with the protective effects of statins for cardiovascular disease, where benefits are also not immediately obvious, can be drawn. In both heart and prostate diseases, treatment decisions are often driven by risk factors—cholesterol levels in the former, prostate-specific antigen (PSA) levels in the latter—not only by symptoms. Ultimately, prevention of disease and relief of symptoms will together provide momentum for the clinical application of the guevedoces’ legacy.
Androgen Dependence of Prostate Gland
History
Testicular androgens are responsible for normal growth, development, and maintenance of the prostate.11–13 Important precursors to establishing the testicular-prostatic relationship include: 1) Berthold’s discovery in 1849 that a blood-borne substance from the testes can act on distant organs (cock’s comb) (http://www.usrf.org) and 2) the Nobel Prize-winning isolation and synthesis of testosterone by Ruzicka in Switzerland and Butenandt in Germany during the 1930s.16
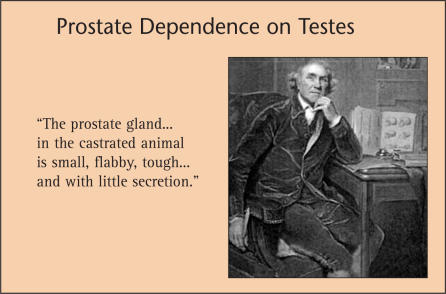
Perhaps the first to study and document findings on the relationship between the prostate and testis was John Hunter, the Scotsman who became known as the “Father of Scientific Surgery” (Figure 3). In a publication in 1786, Hunter described his observations regarding the effect of castration on the prostate gland of bulls:
Figure 3.
The Scotsman, John Hunter, who became known as the “Father of Scientific Surgery,” described more than 200 years ago the androgen dependence of the prostate, which he observed in castrated bulls.
The prostate gland, Cowper’s glands, and the glands along the urethra in the perfect male are large and pulpy, secreting a considerable quantity of a slimy mucus, which is salty to the taste, is most probably for the purpose of lubricating those parts, and is only thrown out when in vigour for copulation: while in the castrated animal they are small, flabby, tough and ligamentous, and have little secretion.
From this account a considerable difference in appearance is distinguishable between the parts connected with generation of the perfect male, and those which remain in one that has been castrated, more especially if that operation had been performed while the animal was young.17
Hunter’s note—that the effect of castration was most pronounced if performed “while the animal was young”—proved prescient. In 1960, a group of 26 Chinese eunuchs ages 59 to 83 years, who had all been castrated early in life to serve the last emperor of the Qing Dynasty, underwent prostate examinations. The average interval between castration and prostate examination was 54 years. In 21 eunuchs, no prostate tissue was palpable, and in the other 5, the gland was only a rudiment. The authors reported that “testicular hormone is essential for the development and preservation of the prostate.”18 This brief report appears to be the only documentation, aside from an autopsy study of older men with congenital panhypopituitarism or gonadotropic deficiency,19 to confirm that the prostate does not develop without testicular androgens. Another well-known group of men castrated early in life were the Castrati singers of Italy, but prostate studies on them are not available.
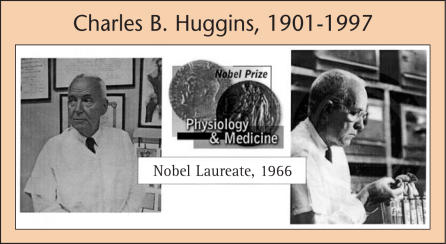
Urologist Charles B. Huggins (1901–1997) first applied the scientific method to the study of androgen-prostate relationships, earning him the Nobel Prize in 1966.20,21 The work Huggins performed in the late 1930s and early 1940s, along with his urological colleagues WW Scott and CV Hodges, has been deemed the most important body of urological research in history (Figure 4). When Huggins was awarded his Prize, the Nobel committee said:
FIgure 4.
Charles B. Huggins, working in the 1930s and early 1940s at the Ben May Laboratory at the University of Chicago, was the first to apply scientific method to a study of the relationship of prostate growth and testosterone. He observed that men with advanced prostate cancer could be markedly relieved by castration or estrogen therapy. He also noted that the glandular epithelium underwent marked involution in men with benign prostatic hyperplasia who were similarly treated. For his work, he received the Nobel Prize in Physiology and Medicine in 1966.
Your fundamental discoveries concerning the hormone dependence of normal and neoplastic cells in experimental animals and their immediate practical application to the treatment of human prostatic and breast cancer have already given many years of an active and useful life to patients with advanced cancer over the entire civilized world, patients who would have been lost to all other forms of therapy (http://www.nobelprize.org/medicine/laureates/1966/press.html).
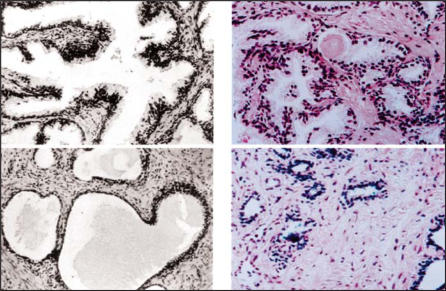
Huggins’ most important discovery was that cancers are not always autonomous, but may be under the control of signals, such as hormones, to grow and survive. Blocking those signals, by orchiectomy or estrogen administration, could restore health to patients even with widespread metastases. Huggins also showed that benign prostatic hyperplasia (BPH) tissue was under control of testicular androgens (Figure 5), thus providing a scientific basis for the use of castration therapy for advanced BPH, which was used before the turn of the last century. Video clips of Huggins explaining his work are available online (http://www.usrf.org).
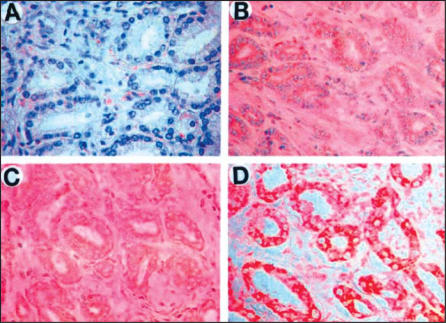
Figure 5.
Photomicrographs of prostatic epithelium from men with benign prostatic hyperplasia before (above) and after (below) treatments that deprive the prostate of androgenic stimuli. On the left (black/white) are sections from Huggins’ patients circa 1940; treatment was castration. On the right (color) are sections from a contemporary treatment circa 1999: finasteride. The prostate tissue effect from the 2 treatments is similar. Reprinted with permission from Marks LS et al.8
A summary of scientific events leading up to the discovery of the 5ARI drugs is shown in Table 2.
Table 2.
Scientific Events Leading to Advent of 5α-Reductase Inhibitors
| Investigator | Era | Discovery |
|---|---|---|
| J. Hunter (Scotland)17 | 1786 | Prostate dependence on testes |
| A. Berthold (Germany) | 1849 | Blood-borne nature of testosterone; first |
| (http ://www.usrf.org) | hormone | |
| L. Ruzicka (Switzerland) & | 1939 | Isolation, synthesis of testosterone; |
| A. Butenandt (Germany)16 | Nobel Prize, 1939 | |
| C.B. Huggins (US)20,21 | 1941 | Responsiveness of prostate diseases to |
| androgen deprivation therapy; | ||
| Nobel Prize, 1966 | ||
| J. Wilson (US)23 | 1969 | Biologic role of DHT |
| J. Imperato-McGinley (US)1 | 1974 | Effects of congenital deficiency of 5AR |
| P.C. Walsh (US)26 | 1975 | Co-discovery of 5AR syndrome |
| E. Stoner,28 | 1992 | Approval of finasteride |
| G. Gormley (US)29 | ||
| R. Rittmaster,30 | 2002 | Approval of dutasteride |
| C. Roehrborn (US)14 |
DHT, dihydrotestosterone; 5AR, 5α-reductase.
Current Understanding of Prostate Growth
Testosterone, the main circulating androgen, is not the primary nutrient for the prostate. That role belongs to DHT, which is derived from testosterone within prostate cells by the action of the enzyme 5AR.11–13 Testosterone in serum has approximately 10 times the concentration of DHT, but in the prostate gland, the ratio is more or less reversed. The biologic role of DHT was clarified by the work of Jean Wilson and co-workers at the University of Texas Southwestern Medical Center during the late 1960s.22,23 These investigators demonstrated that, within the prostate, DHT is present in higher concentration and also binds more tightly to the androgen receptor than does testosterone. Thus, DHT remains at high levels in the prostate throughout life, without the age-related decline seen in circulating testosterone. For this reason, DHT must exert at least a permissive role in the development of BPH.
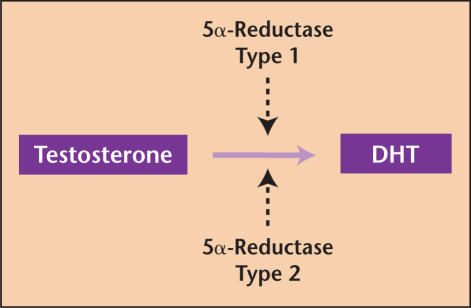
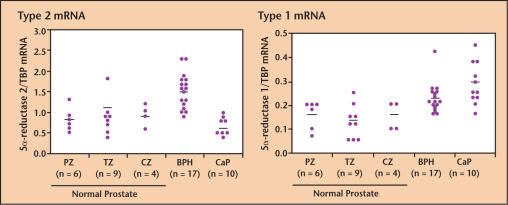
The enzyme 5AR, which catalyzes the conversion of testosterone to its 5α-reduced form DHT, is now known to exist in 2 isoenzymatic forms: Type 1 and Type 2 (Figure 6).12,13 Type 1 is most prevalent in extra-prostatic tissues, primarily liver and skin, and DHT derived from its conversion of testosterone reaches the prostate via systemic circulation. Type 2 is the major type in the prostate, and it is this type that is deficient in the Dominican pseudohermaphrodites.1–3 A separate gene encodes each type. Finasteride inhibits Type 2 5AR; dutasteride is a more potent inhibitor of Type 2 and also inhibits Type 1 (ie, it is a dual inhibitor). Dual inhibition of 5AR is believed to explain the greater suppression of serum DHT levels by dutasteride, and possible earlier onset of clinical effect than seen with the Type 2 inhibitor finasteride.14,15 Data regarding intraprostatic DHT levels on clinically used dosages of dutasteride are currently not available, however. Differential expression of messenger RNA (mRNA) for the 2 types of 5AR is shown in Figure 7.24 The mechanism by which DHT is formed, receptor binding occurs, and DNA synthesis is effected in the prostate is shown in a published video clip in an article by Carson and Rittmaster.25
Figure 6.
The conversion of testosterone to dihydrotestosterone is catalyzed by the enzyme 5α-reductase (5AR), which exists in 2 forms: Type 1 and Type 2, both of which are found in the prostate. Type 1 is produced primarily in liver and skin and is carried to the prostate via the systemic circulation. Type 2 is the major form in the prostate. Finasteride inhibits Type 2 5AR. Dutasteride inhibits both Type 1 and 2 5AR (dual inhibitor). DHT, dihydrotestosterone.
Figure 7.
Distribution of messenger RNA (mRNA) for Type 2 (left) and Type 1 (right) 5α-reductase (5AR) in human prostate tissues: normal, BPH, and CaP. In BPH tissue, both types of 5AR are over-expressed; in CaP tissue, only Type 1 is over-expressed. Note difference in vertical axis scale. BPH, benign prostatic hyperplasia; CaP, cancer of the prostate; TBP, TATA-binding protein; PZ, peripheral zone; TZ, transition zone; CZ, central zone. Reprinted from Iehle C et al.24 with permission from Elsevier.
Pseudohermaphrodites (“Guevedoces”) of the Dominican Republic
The pseudohermaphrodites of the Dominican Republic, having a congenital deficiency of 5AR Type 2, provided a model to confirm the DHT theory of prostate growth.1–4 In the isolated village where the mutation was discovered, approximately 2% of live births were males (46 XY karyotype), with apparent female genitalia at birth. These children were raised as girls until puberty, at which time the microphallus developed into a functional penis (hence the name “guevedoce” or penis at 12), the normal testes descended into a developed scrotum, the body became muscular, the voice deepened, and a male psychosexual orientation evolved (Figure 8). Throughout life thereafter, the guevedoces are in most ways like the other males of the village except beard growth remains scanty, no acne occurs, the temporal hair line does not recede, and the prostate remains small.1 At about the same time, Walsh and colleagues26 co-discovered the syndrome in 2 siblings in Dallas. Later studies of the guevedoces as adults revealed that the prostate was rudimentary by MRI evaluation; biopsy of the gland showed only stromal tissue, no epithelium, and serum PSA level was undetectable.4
Figure 8.
“Guevedoces” (literally, penis at 12) of Dominican Republic are biological males (46XY) with female-appearing external genitalia from birth until puberty; at puberty, they develop a penis, the testes descend, muscles and a male psychosexual orientation develop. Throughout life, the prostate remains small, because the congenital deficiency of 5α-reductase leaves affected individuals with markedly suppressed levels of dihydrotestosterone (DHT). DHT is the major androgenic stimulus for the prostate. Reprinted from Peterson RE et al.2 with permission from Elsevier.
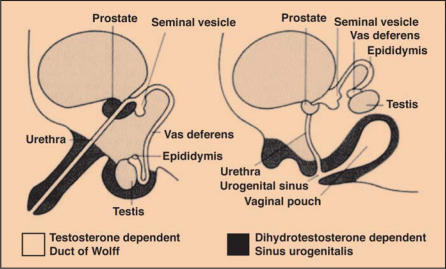
The unusual features of the guevedoces are explained by differential functions of testosterone (Table 1), which in these individuals is normal, and DHT, which is markedly suppressed. In utero, testosterone is responsible for differentiation of the Wolffian duct derivatives (ie, seminal vesicles, vasa, epididymis, and ejaculatory ducts); after puberty testosterone causes masculinization (ie, muscle mass, voice change, libido, growth of external genitalia, and spermatogenesis) (Figure 9). In utero, DHT is responsible for normal differentiation of the male external genitalia; after puberty, however, DHT may be considered a “bad” hormone, as it is responsible for facial hair, acne, male pattern baldness, and prostate growth.1,12
Figure 9.
Differences in testosterone-dependent (Wolffian duct) and DHT-dependent (urogenital sinus) structures in embryogenesis of male genitalia. The “guevedoces” are congenitally deficient in DHT, resulting in failure of the urogenital sinus derivatives to differentiate properly. At puberty, the outpouring of testosterone causes these biologic males to experience descent of testes, phallic enlargement, and development of a male body habitus. DHT, dihydrotestosterone. Reprinted from Bartsch G et al.12 with permission from Springer-Verlag.
Drugs to Inhibit 5AR Enzymes
Scientists in the pharmaceutical industry reasoned that if 5AR could be targeted for inhibition after the external genitalia were fully formed and mature, then a safe drug to shrink the prostate, relieve LUTS, and ameliorate baldness and acne might be developed. Eighteen years after Imperato-McGinley’s first publication,1 the “prostate pill” arrived; the US Food and Drug Administration (FDA) approved finasteride June 19, 1992 for the treatment of men with symptomatic BPH. FDA approval for male pattern hair loss (in men only) followed, and in October 2002, the dual 5ARI dutasteride was approved. Both drugs currently claim to improve symptoms, reduce the risk of acute urinary retention (AUR), and reduce the risk of the need for BPH-related surgery. A comparison of finasteride and dutasteride is shown in Table 3. In recognition of data from the Medical Therapy of Prostatic Symptoms study,6 an additional indication for finasteride is: “in combination with the α-blocker doxazosin, to reduce the risk of symptomatic progression of BPH.”
Table 3.
Major Diffferences in Dutasteride and Finasteride, the 2 Approved 5α-Reductase Inhibitors*
| Dutasteride | Finasteride | |
|---|---|---|
| Dosage, mg/d | 0.5 | 5.0 |
| Half-life (d) | 35 | 0.3 |
| 5α-reductase inhibition | Type 1 and 2 | Type 2 |
| DHT suppression (%) | 90 | 70 |
| Prostate volume reduction (y 2, %) | 27 | 20 |
| Symptom decrease, 2 y (IPSS points) | 3.8 | 3.1 |
| Uroflow increase, 2 y (Qmax, cc/sec) | 1.9 | 1.8 |
| Risk reduction (AUR, y 4, %) | 57 | 57 |
| Side effects (ED, libido, ejaculatory | 10–15 | 10–15 |
| disorders, breast; %)† | ||
| Cost (AWP, 1 m Rx, 2/03; $) | 75 | 80 |
These data reflect the author’s impression based on information published in the 2003 package inserts of both drugs.
Percent of patients reporting 1 or more of these side effects during first year of study.
DHT, dihydrotestosterone; IPSS, International Prostate Symptom Score; Qmax, maximum flow rate; AUR, acute urinary retention; ED, erectile dysfunction; AWP, average wholesale price.
Finasteride
Soon after the guevedoces’ story became known, and the implications of 5AR deficiency became clear, Merck began an ambitious development program in the research laboratories at Rahway, New Jersey. Following synthesis of many potential 4-aza steroid molecules that would inhibit 5AR, a drug known as MK-906 was selected as the best therapeutic molecule. After successful testing in experimental animals, where the drug was found to sharply reduce DHT levels and prostate volume, 27 MK-906 (later finasteride) went into human trials in 1986. A few years later, reports of phase I testing were reported by Stoner,28 Gormley and colleagues,29 Rittmaster and colleagues,30 and others. As expected, men treated with finasteride developed a marked suppression of DHT, no change or slight elevation in serum testosterone, and no change in all other serum components studied. In 1992, the phase III studies, demonstrating safety and efficacy over 1 year of treatment in men with symptomatic BPH, were published in the New England Journal of Medicine,5 concomitant with FDA approval.
Dutasteride
As finasteride was known to be a pure Type 2 inhibitor of 5AR, efforts soon began to develop a drug that would inhibit both Type 1 and 2, theoretically a more powerful inhibition. Merck went into phase II testing of such a molecule in the early 1990s (MK-434), but trials were quickly halted because of potential toxicity problems, and the drug was never developed. A dual inhibitor from GlaxoSmithKline, originally known as GG745 (dutasteride), was developed later in the decade, and in 1998, early-phase clinical trial results were published.31 The dual inhibitor was found to lower DHT serum levels significantly more than finasteride (∼ 90% with dutasteride vs 70% with finasteride), offering the potential for greater clinical efficacy of the new drug. Although direct, long-term comparisons of finasteride and dutasteride in a clinical trial are not available; the phase III dutasteride data published in 2002 showed that dutasteride yielded symptomatic improvement over placebo as early as 3 months and a prostate shrinkage exceeding 25%,14 both quicker and more profound than what had been seen in the finasteride trials.
Dutasteride Versus Finasteride
Differences between the 2 drugs are shown in Table 3. A few notable differences are that dutasteride inhibits both Type 1 and Type 2 5AR, whereas finasteride inhibits only Type 2 and dutasteride has a 5-week half-life, whereas finasteride has an 8-hour half-life. Although Type 2 is clearly the prominent type in the prostate (Figure 7),24 increasing evidence suggests an important role for Type 1, particularly in cancer (Figure 10).32
Figure 10.
Four different prostate cancers stained with a monoclonal antibody for Type 1 5AR (red color), showing that in some cancers (ie, section D above), the enzyme is highly expressed. Marginal expression of the enzyme is seen in cancer A, moderate expression in cancers B & C. 5AR, 5α-reductase. Reprinted with permission from Thomas LN et al.32
5ARI Drugs: Beyond Treatment of LUTS
Beyond the current approved indications of the 5ARI drugs, 3 additional applications are now on the horizon: chemoprevention of prostate cancer, prophylaxis of BPH complications, and treatment of prostatic bleeding. Treatment of prostatitis might be a fourth application, but the available literature is sparse.
Chemoprevention of Prostate Cancer
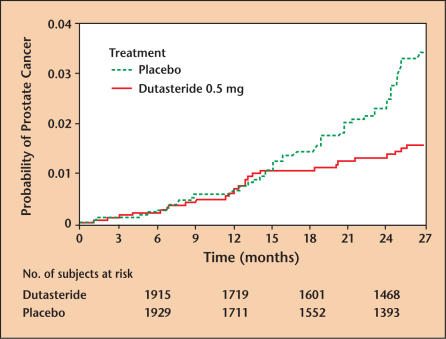
Results of the National Cancer Institute Prostate Cancer Prevention Trial, comparing finasteride with placebo in the prevention of prostate cancer, were published in June 2003.9 This trial included enrollment of more than 25,000 men, who were randomized to finasteride or placebo between 1993 and 2003. In finasteride-treated men, the 7-year period prevalence of cancer of the prostate (CaP) was reduced by 24% (P < .01). Increased numbers of high-grade tumors in the finasteride group have not yet been fully explained, and efforts to analyze the actual prostatectomy specimens of those men diagnosed with cancer in the course of the trial are underway.33 Nevertheless, the hypothesis was confirmed, and the conclusion is evident: a 5ARI can lower the risk of CaP. A lowered incidence of CaP in dutasteride-treated men compared with placebo-treated men was recently culled from the phase III BPH data (Figure 11),34 setting the stage for a major chemoprevention trial with dutasteride (Reduction by Dutasteride in Prostate Cancer Events trial) now in the second year of enrollment. The recent discovery that dutasteride promotes apoptosis in a LNCaP cell line, gives a basic science impetus for this study.35 Currently, neither drug has FDA approval for use in this manner.
Figure 11.
Kaplan-Meier estimates of proportion of subjects experiencing a prostate cancer adverse event in the dutasteride phase III trial. Note that starting at approximately 15 months into the trial, the placebo and dutasteride groups begin to diverge. For the first 27 months, the cumulative incidence of CaP was 1.2% in the dutasteride group and 2.5% in the placebo group. The differences are highly significant (P = .002), suggesting a chemopreventive effect in the dutasteride group. CaP, cancer of the prostate. Reprinted with permission from Andriole GL et al.34
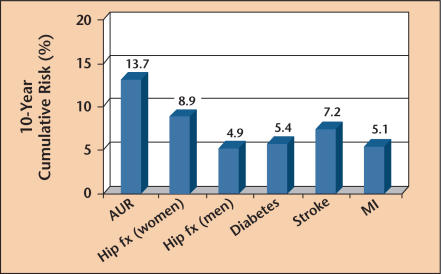
Prophylaxis of BPH Complications
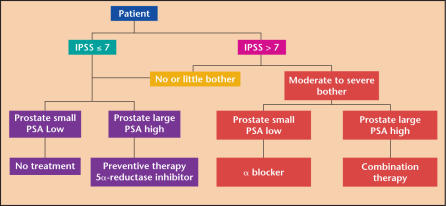
Development of complications from BPH is not necessarily related to antecedent symptoms. In the Olmstead County Study, a 60-year-old man with moderate symptoms had a 10-year risk of AUR of 13.7%36 (Figure 12). With substantial enlargement of the gland, the risk appears to be considerably greater. In that same community-based study, the AUR risk was several times greater than risk of a hip fracture, stroke, or heart attack.36 All of these conditions are regularly treated prophylactically with drugs. Although not life-threatening, the complications of BPH are dramatic and life-altering, usually resulting in surgery. Nowadays, a high-risk group can be identified by PSA level testing, and these men—perhaps those with a serum PSA level > 1.5 ng/mL—are candidates for 5ARI treatment.37,38 In such men, both 5ARI drugs have been shown to lower risk of AUR or need for surgery. In prior years, when prostatectomy was the only treatment, preventive surgery would have been unacceptable. Today however, the availability of well-tolerated preventive medications should encourage a reassessment of the former doctrine. Treatment of men with minimally symptomatic BPH was the subject of a recent “Point-Counterpoint” debate10 published in Urology. A BPH treatment algorithm, incorporating prophylactic use of a 5ARI in men with elevated PSA levels, is presented in Figure 13. Such usage of the 5ARI drugs is currently “off label.”
Figure 12.
10-year cumulative risk of a 60-year-old man developing one of the common conditions shown on the horizontal axis. Note that the risk of acute urinary retention (AUR) is several times greater than risk of hip fracture, stroke, or heart attack. fx, fracture; MI, myocardial infarction. Reprinted with permission from Jacobsen SJ et al.36
Figure 13.
PSA-based algorithm for treatment of men with BPH. In this schema, data from the MTOPS study6 is employed to suggest combination therapy with a 5ARI and an α-blocking agent for symptomatic men with high PSA levels (right side), whereas men with few symptoms and low PSA levels need only be observed (left side). Men with symptoms and low PSA levels would be treated with an α-blocker alone (right center, bottom). Men with few symptoms but elevated PSA levels would be offered preventive therapy with a 5ARI (left center, bottom), as discussed elsewhere.10 This schema is solely the author’s notion and does not reflect the package inserts. PSA, prostate-specific antigen; BPH, benign prostatic hyperplasia; MTOPS, Medical Therapy of Prostatic Symptoms; 5ARI, 5α-reductase inhibitor; IPSS, International Prostate Symptom Score.
Treatment of Prostatic Bleeding
A particularly vexing complication of BPH is bleeding from the surface of an enlarged gland into the urine. BPH bleeding is one of the most common causes of gross hematuria in older men. Finasteride was first reported to be effective against this condition in 1997, when 12 men at the Cleveland Clinic had their recurrent BPH bleeding arrested with the drug.39 Since the original, a number of additional reports have confirmed the value of the drug for this condition. Furthermore, some have recommended pretreatment of men scheduled for transurethral resection of the prostate to reduce perioperative bleeding, though this approach has not been widely adopted. The effectiveness of finasteride in BPH bleeding is thought to be via inhibition of angiogenesis with a reduction in microvessel density of the suburethral prostate tissue.40 This effect appears to be mediated via a finasteride-induced reduction in the tissue expression of vascular endothelial growth factor. An effective treatment for BPH bleeding is a welcome addition to the urologic armamentarium.
Main Points.
The discovery of the Dominican “guevedoces” helped lead the transformation of urology from a purely surgical specialty into a discipline centered around effective drug therapy and minimally invasive treatments.
Two classes of drugs serve as the initial treatment of choice for most men with benign prostatic hyperplasia (BPH): 5α-reductase inhibitors and α-adrenergic receptor blocking agents. Whereas the latter offer quick relief of lower urinary tract symptoms, only the former can alter the natural history of the disease, slow symptomatic progression, and prevent complications.
The enzyme 5α-reductase, which catalyzes the conversion of testosterone to its 5α-reduced form dihydrotestosterone (DHT), exists in 2 forms: Type 1 and Type 2. Finasteride inhibits Type 1 only, whereas dutasteride inhibits both Types 1 and 2.
Although direct comparisons of the 2 drugs in clinical trials have not been performed, available data show that dutasteride can lower DHT serum levels, yield more symptomatic improvement, and cause prostate shrinkage both quicker and more profoundly than finasteride.
5α-reductase inhibitors may prove to be useful in chemoprevention of prostate cancer, prophylaxis of BPH, and treatment of prostatic bleeding.
References
- 1.Imperato-McGinley J, Guerrero L, Gautier T, et al. Steroid 5α-reductase deficiency in man: an inherited form of male pseudohermaphroditism. Science. 1974;186:1213–1215. doi: 10.1126/science.186.4170.1213. [DOI] [PubMed] [Google Scholar]
- 2.Peterson RE, Imperato-McGinley J, Gautier T, et al. Male pseudohermaphroditism due to steroid 5α-reductase deficiency. Am J Med. 1977;62:170–191. doi: 10.1016/0002-9343(77)90313-8. [DOI] [PubMed] [Google Scholar]
- 3.Imperato-McGinley J, Peterson RE, Gautier T, et al. Androgens and the evolution of male-gender identity among male pseudohermaphrodites with 5α-reductase deficiency. N Engl J Med. 1979;300:1233–1237. doi: 10.1056/NEJM197905313002201. [DOI] [PubMed] [Google Scholar]
- 4.Imperato-McGinley J, Gautier T, Zirinsky TH, et al. Prostate visualization studies in male homozygous and heterozygous for 5α-reductase deficiency. J Clin Endocrinol Metab. 1992;75:1022–1026. doi: 10.1210/jcem.75.4.1400866. [DOI] [PubMed] [Google Scholar]
- 5.Gormley GJ, Stoner E, Bruskewitz RC, et al. The effect of finasteride in men with benign prostatic hyperplasia. The Finasteride Study Group. N Engl J Med. 1992;327:1185–1191. doi: 10.1056/NEJM199210223271701. [DOI] [PubMed] [Google Scholar]
- 6.McConnell JD, Roehrborn CG, Bautista OM, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349:2387–2398. doi: 10.1056/NEJMoa030656. [DOI] [PubMed] [Google Scholar]
- 7.Marks LS, Partin AW, Gormley GJ, et al. Prostate tissue composition and response to finasteride in men with symptomatic benign prostatic hyperplasia. J Urol. 1997;157:2171–2178. [PubMed] [Google Scholar]
- 8.Marks LS, Partin AW, Dorey FJ, et al. Long-term effects of finasteride on prostate tissue composition. Urology. 1999;53:574–580. [PubMed] [Google Scholar]
- 9.Thompson IM, Goodman PJ, Tangen CM, et al. The influence of finasteride on the development of prostate cancer. N Engl J Med. 2003;349:215–224. doi: 10.1056/NEJMoa030660. [DOI] [PubMed] [Google Scholar]
- 10.Marks LS. Treatment of men with minimally symptomatic benign prostatic hyperplasia-pro: the argument in favor. Urology. 2003;62:781–783. doi: 10.1016/s0090-4295(03)00779-9. [DOI] [PubMed] [Google Scholar]
- 11.McConnell JD. Prostatic growth: new insights into hormonal regulation. Br J Urol. 1995;76(suppl 1):5–10. [PubMed] [Google Scholar]
- 12.Bartsch G, Rittmaster RS, Klocker H. Dihydrotestosterone and the concept of 5α-reductase inhibition in human benign prostatic hyperplasia. World J Urol. 2002;19:413–425. doi: 10.1007/s00345-002-0248-5. [DOI] [PubMed] [Google Scholar]
- 13.Carson C, 3rd, Rittmaster R. The role of dihydrotestosterone in benign prostatic hyperplasia. Urology. 2003;61(suppl 1):2–7. doi: 10.1016/s0090-4295(03)00045-1. [DOI] [PubMed] [Google Scholar]
- 14.Roehrborn CG, Boyle P, Nickel JC, et al. Efficacy and safety of a dual inhibitor of 5α-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology. 2002;60:434–441. doi: 10.1016/s0090-4295(02)01905-2. [DOI] [PubMed] [Google Scholar]
- 15.Roehrborn CG, Marks LS, Fenter T, et al. Efficacy and safety of dutasteride in the four-year treatment of men with benign prostatic hyperplasia. Urology. 2004;63:709–715. doi: 10.1016/j.urology.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Ruzicka L. The artificial preparation of the male sex hormone. Current Science. 2001;80:616. [Google Scholar]
- 17.Hunter J. Observations on Certain Parts of the Animal Oeconomy. 1786:37–39. Sold at: 13 Castle-Street, Leicester-Square, London, England. [Google Scholar]
- 18.Wu CP, Gu FL. The prostate in eunuchs. Prog Clin Biol Res. 1991;370:249–255. [PubMed] [Google Scholar]
- 19.Oesterling JE, Epstein JI, Walsh PC. The inability of adrenal androgens to stimulate the adult human prostate: an autopsy evaluation of men with hypogonadotropic hypogonadism and panhypopituitarism. J Urol. 1986;136:1030–1034. doi: 10.1016/s0022-5347(17)45198-6. [DOI] [PubMed] [Google Scholar]
- 20.Huggins C, Steven R. The effect of castration on benign hypertrophy of the prostate in man. J Urol. 1940;43:705. doi: 10.1016/j.juro.2016.10.075. [DOI] [PubMed] [Google Scholar]
- 21.Huggins C, Hodges CV. Studies on prostatic cancer: I. the effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. Cancer Res. 1941;1:293. doi: 10.3322/canjclin.22.4.232. [DOI] [PubMed] [Google Scholar]
- 22.Bruchovsky N, Wilson JD. The intranuclear binding of testosterone 5α-androstan-17β-ol-3-one by rat prostate. J Biol Chem. 1968;243:5953–5960. [PubMed] [Google Scholar]
- 23.Wilson JD, Walker JD. The conversion of testosterone to 5α-androstan-17β-ol-3-one (dihydrotestosterone) by skin slices of man. J Clin Invest. 1969;48:371–379. doi: 10.1172/JCI105994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iehle C, Radvanyi F, Gil Diez de Medina S, et al. Differences in steroid 5α-reductace iso-enzymes expression between normal and pathological human prostate tissue. J Steroid Biochem Mol Biol. 1999;68:189–195. doi: 10.1016/s0960-0760(99)00030-8. [DOI] [PubMed] [Google Scholar]
- 25.Carson C, III, Rittmaster R. The role of dihydrotestosterone in benign prostatic hyperplasia. Urology. 2003;61(suppl 1):2–7. doi: 10.1016/s0090-4295(03)00045-1. [DOI] [PubMed] [Google Scholar]
- 26.Walsh PC, Madden JD, Harrod MJ, et al. Familial incomplete male pseudohermaphroditism, type 2 decreased dihydrotestosterone formation in pseudovaginal perineoscrotal hypospadias. N Engl J Med. 1975;291:944. doi: 10.1056/NEJM197410312911806. [DOI] [PubMed] [Google Scholar]
- 27.Brooks JR, Berman D, Glitzer MS, et al. Effect of a new 5α-reductase inhibitor on size, histologic characteristics, and androgen concentrations of the canine prostate. Prostate. 1982;3:35–44. doi: 10.1002/pros.2990030107. [DOI] [PubMed] [Google Scholar]
- 28.Stoner E. The clinical development of a 5α-reductase inhibitor, finasteride. J Steroid Biochem Mol Biol. 1990;37:375–378. doi: 10.1016/0960-0760(90)90487-6. [DOI] [PubMed] [Google Scholar]
- 29.Gormley GJ, Stoner E, Rittmaster RS, et al. Effects of finasteride (MK-906), a 5α-reductase inhibitor, on circulating androgens in male volunteers. J Clin Endocrinol Metab. 1990;70:1136–1141. doi: 10.1210/jcem-70-4-1136. [DOI] [PubMed] [Google Scholar]
- 30.Rittmaster RS, Stoner E, Thompson DL, et al. Effects of MK-906, a specific 5α-reductase inhibitor, on serum androgens and androgen conjugates in normal men. J Androl. 1989;10:259–262. doi: 10.1002/j.1939-4640.1989.tb00097.x. [DOI] [PubMed] [Google Scholar]
- 31.Gisleskog PO, Herman D, Hammarlund-Udenaes M, et al. A model for the turnover of dihydrotestosterone in the presence of the irreversible 5α-reductase inhibitors GI198745 and finasteride. Clin Pharmacol Ther. 1998;64:636–647. doi: 10.1016/S0009-9236(98)90054-6. [DOI] [PubMed] [Google Scholar]
- 32.Thomas LN, Douglas RC, Vessey JP, et al. 5α-reductase type 1 immunostaining is enhanced in some prostate cancers compared with benign prostatic hyperplasia epithelium. J Urol. 2003;170:2019–2025. doi: 10.1097/01.ju.0000091804.20183.81. [DOI] [PubMed] [Google Scholar]
- 33.Bostwick DG, Qian J, Civantros F, et al. Does finasteride alter the pathology of the prostate and cancer grading? Clin Prostate Cancer. 2004;2:228–235. doi: 10.3816/cgc.2004.n.004. [DOI] [PubMed] [Google Scholar]
- 34.Andriole GL, Roehrborn C, Schulman C, et al. Effect of dutasteride on the detection of prostate cancer in men with benign prostatic hyperplasia. Urology. 2004;64:537–543. doi: 10.1016/j.urology.2004.04.084. [DOI] [PubMed] [Google Scholar]
- 35.Lazier CB, Thomas LN, Douglas RC, et al. Dutasteride, the dual 5α-reductase inhibitor, inhibits androgen action and promotes cell death in the LNCaP prostate cancer cell line. Prostate. 2004;58:130–144. doi: 10.1002/pros.10340. [DOI] [PubMed] [Google Scholar]
- 36.Jacobsen SJ, Girman CJ, Lieber MM. Natural history of benign prostatic hyperplasia. Urology. 2001;58(suppl 1):5–16. doi: 10.1016/s0090-4295(01)01298-5. discussion 16. [DOI] [PubMed] [Google Scholar]
- 37.Roehrborn CG, Boyle P, Gould AL. Serum prostate specific antigen as a predictor of prostate volume in men with benign prostatic hyperplasia. Urology. 1999;53:581–589. doi: 10.1016/s0090-4295(98)00655-4. [DOI] [PubMed] [Google Scholar]
- 38.Roehrborn CG, McConnell JD, Lieber M, et al. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. PLESS Study Group. Urology. 1999;53:473–480. doi: 10.1016/s0090-4295(98)00654-2. [DOI] [PubMed] [Google Scholar]
- 39.Carlin BI, Bodner DR, Spirnak JP, et al. Role of finasteride in the treatment of recurrent hematuria secondary to benign prostatic hyperplasia. Prostate. 1997;31:180–182. doi: 10.1002/(sici)1097-0045(19970515)31:3<180::aid-pros6>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 40.Pareek G, Shevchuk M, Armenakas NA, et al. The effect of finasteride on the expression of vascular endothelial growth factor and microvessel density: a possible mechanism for decreased prostatic bleeding in treated patients. J Urol. 2003;169:20–23. doi: 10.1016/S0022-5347(05)64025-6. [DOI] [PubMed] [Google Scholar]