Abstract
OBJECTIVE
To investigate whether Canadian family practitioners routinely teach breast self-examination (BSE) after publication of the 2001 Canadian Preventive Health Task Force guideline advising them to exclude teaching BSE from periodic health examinations.
DESIGN
Self-administered cross-sectional mailed survey.
SETTING
Canada.
PARTICIPANTS
A random sample of English-speaking general practitioners and physicians certified by the College of Family Physicians of Canada.
MAIN OUTCOME MEASURES
Current and past BSE practices and opinions on the value of BSE.
RESULTS
Response rate was 47.4%. Most respondents (88%) were aware of the new recommendations, yet only 16% had changed their usual practice of routinely teaching BSE. Most physicians agreed that before the recommendation they almost always taught BSE (74.3%). Only 9.5% agreed that physicians should follow the recommendation and not routinely teach BSE. A few also agreed that they now spend less time discussing BSE (25.7%) and that the recommendation has influenced them to stop teaching (12.4%) and encouraging (12.9%) women to practise BSE. Physicians who had changed their BSE practices were less likely to agree that BSE increases early detection of breast cancer and more likely to agree that BSE increases benign breast biopsies. They were also more likely to agree that screening mammography in women older than 50 decreases mortality from breast cancer.
CONCLUSION
This survey, which assessed routine teaching of BSE, revealed poor adherence by Canadian family physicians to a well publicized evidence-based guideline update. Resistance to change could in part be attributed to a lack of knowledge of the supporting evidence, a lack of confidence in the evidence to date, and personal experiences with patients within their practices.
Abstract
OBJECTIF
Déterminer si les médecins de famille canadiens ont continué d’enseigner l’auto-examen des seins de façon routinière après la publication en 2001 d’une directive du Groupe de Travail en médecine préventive recommandant d’exclure l’AES de l’examen médical périodique.
TYPE D’ÉTUDE
Enquête postale transversale auto-administrée.
CONTEXTE
Canada
PARTICIPANTS
Un échantillon aléatoire d’omnipraticiens anglophones et de diplômés du Collège des médecins de famille du Canada
PRINCIPAUX PARAMÈTRES ÉTUDIÉS
Pratiques actuelles et passées à propos de l’AES et opinions sur la valeur de cet examen.
RÉSULTATS
Le taux de réponse était de 47,4%. Même si la plupart (88%) des répondants connaissaient la nouvelle recommandation, seulement 16 % d’entre eux avaient changé leur habitude d’enseigner l’AES de façon routinière. La plupart (74,3%) reconnaissaient qu’ils enseignaient presque toujours l’AES avant cette recommandation. Seulement 9,5% étaient d’avis que les médecins devraient accepter de cesser d’enseigner l’AES de façon routinière. Quelques-uns (25,7 %) déclaraient qu’ils passaient moins de temps à discuter de l’AES et que depuis la recommandation, ils enseignaient moins l’AES (12,4%) et encourageaient moins les femmes à pratiquer cet examen. Les médecins qui avaient changé leurs habitudes concernant l’AES avaient moins tendance à croire que cet examen améliore la détection précoce du cancer du sein et étaient plus susceptibles de penser qu’il augmente les biopsies bénignes du sein. Ils étaient également plus susceptibles de croire que la mammographie de dépistage chez les femmes de plus de 50 ans diminue la mortalité par cancer du sein.
CONCLUSION
Cette enquête évaluant l’enseignement systématique de l’AES a révélé que les médecins de famille canadiens suivent peu cette directive révisée, malgré une bonne publicité et des preuves adéquates. Cette résistance au changement pourrait être attribuable en partie à une connaissance insuffisante des données à l’appui, à un manque de confiance dans les données actuelles et à l’expérience des médecins dans leur pratique.
EDITOR’S KEY POINTS.
In 2001, the Canadian Task Force on Preventive Health Care advised that teaching breast self-examination (BSE) be excluded from routine periodic health examinations (grade D recommendation).
In this Canadian survey, although 88% of family doctors were aware of these guidelines, only 16% had changed their practice of routinely teaching BSE.
Those who had changed their practice were more likely to agree that BSE does not increase early detection of breast cancer and does increase benign breast biopsies.
Personal and previous experience appears to count more than evidence when considering how this guideline was or was not adopted.
POINTS DE REPÈRE DU RÉDACTEUR.
En 2001, le Groupe de Travail canadien en médecine préventive conseillait d’exclure l’enseignement de l’auto-examen des seins (AES) de l’examen médical périodique (recommandation de catégorie D).
La présente enquête révèle que même si les médecins canadiens connaissaient cette directive dans une proportion de 88%, seulement 16% d’entre eux avaient modifié leur habitude d’enseigner l’AES de façon routinière.
Ceux qui avaient changé leurs habitudes étaient plus susceptibles de croire que l’AES n’améliore pas la détection précoce du cancer du sein, alors qu’il augmente le nombre de biopsies bénignes du sein.
L’expérience personnelle et antérieure semble avoir plus de poids que les données probantes dans la décision d’adhérer ou non à cette directive.
Until recently, both Canadian and American preventive health task forces concluded that evidence to either include or exclude routine teaching of breast self-examination (BSE) in periodic health examinations for women was insufficient.1,2 Widespread support for BSE had been based mostly upon weak scientific evidence and an assumption that early detection of breast cancer through BSE would improve prognosis. Potential adverse consequences of BSE had not been studied thoroughly.
Before 2001, 85% of Canadian women aged 50 to 69 years reported that they had been taught how to perform BSE.3 Sixty percent were taught by their family physicians.3 Moreover, 75% to 96% of North American physicians reported that they routinely taught BSE to their patients.4-11
In June 2001, the Canadian Task Force on Preventive Health Care (CTFPHC) published an evidence-based appraisal and recommendations regarding routine teaching of BSE.12 The evidence was based on more recent studies that included two large randomized controlled trials, a quasi-randomized trial, a large cohort study, and several case-control studies.13-26 Overall, this evidence failed to show a survival benefit from regular BSE or BSE education.12 Good evidence of harm from BSE instruction, including substantial increases in the number of physician visits for evaluation of benign breast lesions and higher rates of benign breast biopsies, were also observed. Based on this evidence, the CTFPHC recommended that routine teaching of BSE be excluded from the periodic health examination.12
Despite scientific evidence suggesting an overall harmful outcome from teaching BSE, the recommendations were immediately criticized by breast cancer advocacy groups and by many physicians.27-29 Our study was designed to determine the effect of these recommendations on family physicians’ practices regarding BSE.
METHODS
Study design
A modified Dillman’s method was used for this mailed self-administered cross-sectional survey of Canadian family physicians.30 The survey was first sent out in March 2002, 9 months after the Task Force recommendations were published.
Study population and sampling procedure
A random sample of English-speaking Canadian family physicians was obtained from the College of Family Physicians of Canada (CFPC). To obtain responses from non-CFPC members, a similar random sample of general practitioners was obtained from Cornerstone List Managers. The geographic proportions of the physician samples intentionally reflected the total provincial proportions of English-speaking physicians across Canada. Physicians were considered eligible to complete the survey if their practices included preventive care of women.
Survey instrument
The survey instrument was designed specifically for this study. Portions of existing questionnaires were incorporated.3-11 Clarity and face validity were pilot-tested among 15 academic and community family physicians affiliated with Mount Sinai Hospital’s Family Medicine Centre in Toronto, Ont. Statistically significant Spearman rank correlations between comparable questions ensured good internal reliability of the instrument.
Physicians were asked, “are you aware of the recent Canadian BSE recommendations,” and “as a result of the CTFPHC 2001 BSE recommendations, have you changed your usual practice regarding routine teaching of BSE?” Open-ended, Likert, and multiple-choice questions were used to further assess practices and opinions regarding BSE.
Statistical analysis
Descriptive statistics for all variables were generated. Logistic regression modeling was used to determine variables that predict which physicians have changed their routine BSE teaching practices.
Sample size calculation
A sample size of 256 was calculated based on assumptions that at least 10% of physicians have changed their BSE practices, that 60% of women are taught how to perform BSE by their family doctors,3 and that the likelihood of a type II error was .05 and of a type I error was .9. Expecting a response rate of 40% to 50% and that 5% of surveys would be undeliverable, we contacted 600 family physicians.
Ethics
The study was approved by the Mount Sinai Hospital Research Ethics Board.
RESULTS
Response rate
Of the 600 surveys mailed, 329 were returned: 244 completed surveys from eligible physicians, 80 incomplete surveys from ineligible physicians, and five undeliverable at the address we had. Overall, we had a 47.4% response rate of potentially eligible respondents.
Demographics
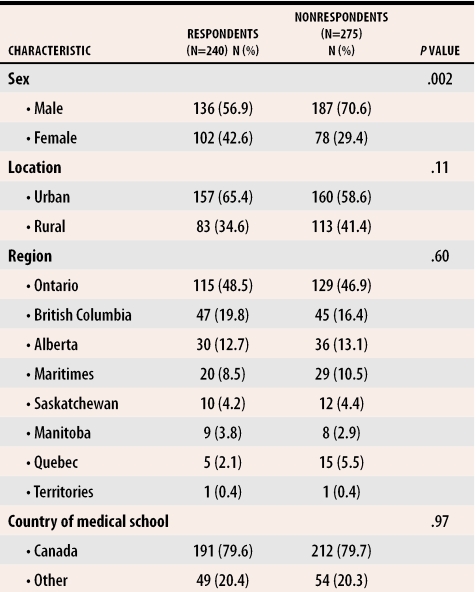
Demographic characteristics of study respondents and nonrespondents are presented in Table 1. On average, nonrespondents had been in practice significantly longer (19.7 ± 10.4 years) than respondents (16.5 ± 9.9 years). Approximately 28% of respondents had university appointments. Seventy-nine percent of respondents reported that they usually or always follow clinical practice guidelines.
Table 1.
Demographics of physician respondents and nonrespondents
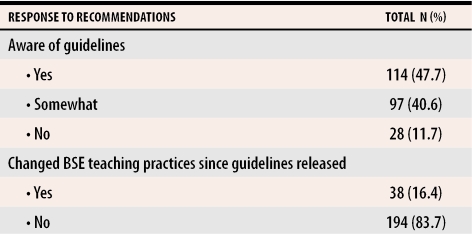
Awareness and change in practice after recommendations
Eighty-eight percent of respondents were at least somewhat aware of the new Task Force recommendations regarding BSE. Sixteen percent changed their usual practice of teaching BSE as a result of the guidelines (Table 2).
Table 2.
Awareness and change in practice after 2001 BSE recommendations released by the Canadian Task Force on Preventive Health Care
BSE—breast self-examination.
In two separate questions, the frequency 1 year before and the current frequency of routinely teaching BSE were also assessed. When current practices among those who reported not having changed their usual practice as a result of the guidelines (n=194) were compared with practices 1 year earlier, two respondents increased their frequency of routinely teaching BSE while eight decreased their frequency. When current practices among those who reported changing their usual practice (n=38) were compared with practices 1 year before, 15 (39%) did not change their frequency of routinely teaching BSE. Of the remaining respondents who reported changing their practice, all but two decreased their frequency of routinely teaching BSE.
Among physicians at least somewhat aware of the Task Force recommendations, only 9.5% agreed that physicians should follow the recommendations and not routinely teach BSE. A few also agreed that they now spend less time discussing BSE (25.7%) and that the recommendations have influenced them to stop teaching (12.4%) and encouraging (12.9%) women to practise BSE. Most physicians agreed that before the recommendations they almost always taught BSE (74.3%).
Advice to patients
When respondents were asked to indicate what they were currently advising their patients regarding BSE, 79% were advising women to use a systematic approach to examine their breasts for lumps regularly, 21% advised women to be aware of their breasts generally for changes or new lumps, and 0.5% gave no advice regarding self-detection of breast lumps.
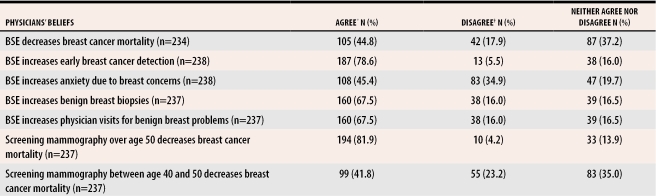
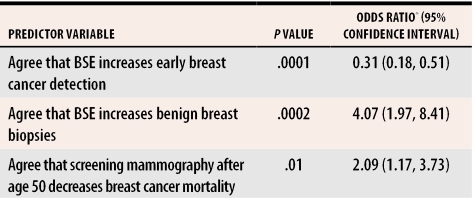
Physicians’ beliefs regarding breast cancer screening
Physicians’ beliefs regarding the benefits and risks associated with BSE and mammography are summarized in Table 3. In general, physicians believed that BSE increases early breast cancer detection, benign breast biopsies, and physician visits for benign breast problems. Several factors predict which physicians are more likely to change their usual practice of teaching BSE (Table 4).
Table 3.
Beliefs about BSE and mammography
BSE—breast self-examination.
*Strongly agree and agree have been combined.
†Strongly disagree and disagree have been combined.
Table 4.
Final multivariate regression model of factors predicting which physicians have changed their usual practice regarding routine teaching of BSE after the 2001 Task Force guidelines
BSE—breast self-examination.
*An odds ratio below 1 indicates the predictor variable is associated with a reduced likelihood of changing BSE practices; an odds ratio above 1 indicates the predictor variable is associated with an increased likelihood of changing BSE practices.
Among physicians who routinely teach BSE (88% of total), 90% (n=181) begin routine teaching of BSE before patients reach the age of 40. The remaining 10% (n=20) begin teaching BSE to women between the ages of 40 and 49 years.
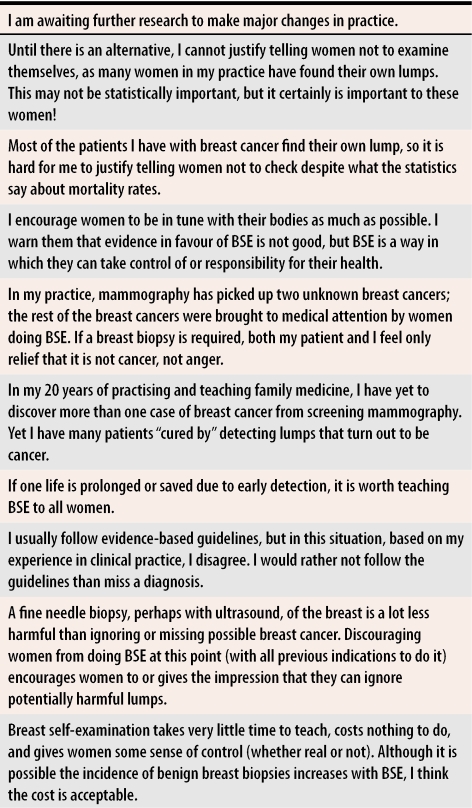
Sample comments provided by respondents are listed in Table 5.
Table 5.
Respondent comments regarding BSE and the current Canadian guidelines
BSE—breast self-examination.
DISCUSSION
Most Canadian family physicians are aware of the recent guidelines on BSE from the Canadian Task Force. Although 77% of physicians in this survey reported that they usually follow clinical practice guidelines, only 16% reported that they had changed their usual BSE teaching practices as a result of the recommendations. These results are consistent with a recent survey in which 80% of Canadian family physicians reported that they continue to teach BSE.31
Discordances between Canadian Task Force cancer screening recommendations and physicians’ practices have been reported. One survey concluded that family physicians often do not adopt cancer screening guidelines backed by good evidence but will perform nonrecommended screening procedures.32 Evidence from our survey shows that most respondents continue to teach BSE. Physicians begin teaching BSE to most women before they reach 40 even though BSE in this age group has not been adequately studied and even though benign breast lumps are more likely to be detected. As a result, health care resources are potentially being spent on inappropriate maneuvers. Evidence suggests these resources would be better spent on interventions that have been proven effective.
The reluctance of physicians to adopt new practice guidelines into their clinical practice could stem from ignorance of the evidence upon which the guidelines are based, lack of confidence in the evidence to date, personal experiences with patients within their practices, or personal beliefs.
Despite scientific evidence showing a substantial increase in the number of benign breast biopsies and no difference in breast cancer incidence, stage at diagnosis, and survival among women who are taught BSE,13-26 physicians in this survey who had not changed their practice were more likely to agree that BSE increases the incidence of early detection of breast cancer. Although physicians might be aware of the guidelines, they might not be aware of the specific underlying scientific evidence upon which the recommendations are based. Physicians who no longer teach BSE were more likely to agree that screening mammography in women older than 50 decreases breast cancer mortality. Perhaps they offer only a very well proven breast cancer screening method.
Some respondents in our survey commented on their lack of confidence in the current evidence regarding BSE and concern that future studies will show benefits. After this survey was completed, however, the existing evidence was further validated by an update of one of the large randomized trials on which the 2001 BSE recommendations were based, which reported that even after longer follow up, BSE did not reduce breast cancer mortality.33
For many physicians, practice guidelines conflict with personal experiences. Physicians commented on women in their practices who detected malignant breast lumps through BSE. Practice guidelines could also conflict with personal beliefs. A survey of Canadian family physicians concluded that, overall, some Task Force recommendations are inconsistent with physicians’ personal beliefs and those of their patients.34 Physicians often attribute high value to detection of insidious diseases, even in the absence of proof of the effectiveness of such activity. Similarly, in our survey, physicians indicated that it is easier to live with not adhering to guidelines than with having missed a diagnosis and that, even if only one life was prolonged or saved due to early detection, it was worth teaching BSE to all women in their practices.
Given that this study looked only at practice changes and opinions of the recent Canadian guidelines on teaching BSE, further research is needed to understand how physicians incorporate evidence-based recommendations into usual practice. Specifically the underlying reasons supporting physicians’ reluctance and the factors that would influence them to change their clinical practice should be assessed in more detail.
Limitations
The observed sample of 244 approached the target sample size of 256. Therefore, a low response rate of 47%, which was factored into the sample size calculation, would only minimally affect the generalizability of these results. Although our study did not show a difference between sexes observed in a comparable survey,31 we observed significantly more female respondents than nonrespondents, thereby potentially inflating our estimates.
Breast self-examination practices reported in this survey could differ from actual practice. In a 1994 Canadian survey, only 60% of women reported that they were taught BSE by their family doctors.3 In our 2002 survey, however, 78% of physicians reported that they had routinely taught BSE before the new guidelines were published. Further, given the criticisms of the guidelines after they were published, perhaps physicians influenced by social desirability were less likely to report that they no longer teach BSE.
Conclusion
Although most family physicians state that they usually follow clinical practice guidelines, this survey, which assessed routine teaching of BSE, revealed poor adherence by Canadian family physicians to a well publicized guideline update.
Acknowledgments
We acknowledge the financial assistance of the Marvelle Koffler Breast Centre Fund for Excellence.
Biography
Dr Del Giudice is an Assistant Professor and Dr Tannenbaum is an Associate Professor in the Department of Family and Community Medicine at the University of Toronto in Ontario. Dr Goodwin is a Professor in the Department of Medicine at the University of Toronto and is Director of the Marvelle Koffler Chair in Breast Research and of the Breast Centre at Mount Sinai Hospital.
Footnotes
Competing interests: None declared
References
- 1.Canadian Task Force on the Periodic Health Examination. The Canadian guide to clinical preventive health care. Ottawa, Ont: Canada Communications Group; 1994. pp. 790–791. [Google Scholar]
- 2.Eastman P. Task force issues new screening guidelines [news]. J Natl Cancer Inst. 1996;88:74–76. doi: 10.1093/jnci/88.2.74. [DOI] [PubMed] [Google Scholar]
- 3.De Grasse CE, O’Connor AM, Perrault DJ, Aitken SE, Joanisse S. Changes in women’s breast cancer screening practices, knowledge and attitudes in Ottawa-Carleton since 1991. Can J Public Health. 1996;87:333–338. [PubMed] [Google Scholar]
- 4.Battista RN. Adult cancer prevention in primary care: patterns of practice in Quebec. Am J Public Health. 1983;73:1036–1039. doi: 10.2105/ajph.73.9.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Battista RN, Palmer CS, Marchand BM, Spitzer WO. Patterns of preventive practice in New Brunswick. CMAJ. 1985;132:1013–1015. [PMC free article] [PubMed] [Google Scholar]
- 6.Marin J, Howe HL. Physicians’ attitudes toward breast self-examination: a pilot study. Eval Health Prof. 1984;7:193–204. doi: 10.1177/016327878400700205. [DOI] [PubMed] [Google Scholar]
- 7.O’Malley MS, Fletcher SW, Bunce LA. Physicians and the teaching of breast self-examination: implications from a survey at a university teaching hospital. Am J Public Health. 1985;75:673–675. doi: 10.2105/ajph.75.6.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogle KS, Snellman LA, Henry RC. Breast and testicular self-examination in primary care. Am J Prev Med. 1988;4:11–13. [PubMed] [Google Scholar]
- 9.Warner SL, Worden JK, Solomon LJ, Wadland WC. Physician interest in breast cancer screening education. J Fam Pract. 1989;29:281–285. [PubMed] [Google Scholar]
- 10.Carney PA, Dietrich AJ, Freeman DH, Mott LA. The periodic health examination provided to asymptomatic older women: an assessment using standardized patients. Ann Intern Med. 1993;119:129–135. doi: 10.7326/0003-4819-119-2-199307150-00007. [DOI] [PubMed] [Google Scholar]
- 11.Mah Z, Bryant H. Age as a factor in breast cancer knowledge, attitudes and screening behaviour. CMAJ. 1992;146:2167–2174. [PMC free article] [PubMed] [Google Scholar]
- 12.Canadian Task Force on Preventive Health Care. Baxter N. Preventive health care, 2001 update: should women be routinely taught self-examination to screen for breast cancer? CMAJ. 2001;164:1837–1846. [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas DB, Gao DL, Self SG, Allison CJ, Tao Y, Mahloch J, et al. Randomized trial of breast self-examination in Shanghai: methodology and preliminary results. J Natl Cancer Inst. 1997;89:355–365. doi: 10.1093/jnci/89.5.355. [DOI] [PubMed] [Google Scholar]
- 14.Semiglazov VF, Moiseyenko VM. Breast self-examination for the early detection of breast cancer: a USSR/WHO controlled trial in Leningrad. Bull World Health Org. 1987;65:391–396. [PMC free article] [PubMed] [Google Scholar]
- 15.Koroltchouk V, Stanley K, Stjernsward J. The control of breast cancer: a World Health Organization perspective. Cancer. 1990;65:2803–2810. doi: 10.1002/1097-0142(19900615)65:12<2803::aid-cncr2820651233>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 16.Semiglazov VF, Moiseyenko VM, Bavli JL, Migmanova NS, Seleznyov NK, Popova RT, et al. The role of breast self-examination in early breast cancer detection (results of the 5-year USSR/WHO randomized study in Leningrad). Eur J Epidemiol. 1992;8:498–502. doi: 10.1007/BF00146366. [DOI] [PubMed] [Google Scholar]
- 17.Semiglazov VF, Sagaidak VN, Moiseyenko VM, Mikhailov EA. Study of the role of breast self-examination in the reduction of mortality from breast cancer. The Russian Federation/World Health Organization Study. Eur J Cancer. 1993;29A:2039–2046. [PubMed] [Google Scholar]
- 18.Semiglazov VF, Moiseyenko VM, Protsenko SA, Bavli JL, Orlov AA, Ivanova OA, et al. [Preliminary results of the Russia (St. Petersburg)/WHO program for the evaluation of the effectiveness of breast self-examination]. Vopr Onkol. 1996;42:49–55. [PubMed] [Google Scholar]
- 19.Semiglazov VF, Moiseyenko VM, Manikhas AG, Protsenko SA, Kharikova RS, Popova RT, et al. [Interim results of a prospective randomized study of self-examination for early detection of breast cancer (Russia/St. Petersburg/WHO)]. Vopr Onkol. 1999;45:265–271. [PubMed] [Google Scholar]
- 20.UK Trial of Early Detection of Breast Cancer Group. First results on mortality reduction in the UK trial of early detection of breast cancer. Lancet. 1988;2:411–416. [PubMed] [Google Scholar]
- 21.UK Trial of Early Detection of Breast Cancer Group. 16-year mortality from breast cancer in the UK trial of early detection of breast cancer. Lancet. 1999;353:1909–1914. [PubMed] [Google Scholar]
- 22.Holmberg L, Ekbom A, Calle E, Mokdad A, Byers T. Breast cancer mortality in relation to self-reported use of breast self-examination. A cohort study of 450 000 women. Breast Cancer Res Treat. 1997;43:137–140. doi: 10.1023/a:1005788729145. [DOI] [PubMed] [Google Scholar]
- 23.Gastrin G, Miller AB, To T, Aronson KJ, Wall C, Hakama M, et al. Incidence and mortality from breast cancer in the Mama program for breast screening in Finland, 1973-1986. Cancer. 1994;73:2168–2174. doi: 10.1002/1097-0142(19940415)73:8<2168::aid-cncr2820730822>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 24.Harvey BJ, Miller AB, Baines CJ, Corey PN. Effect of breast self-examination techniques on the risk of death from breast cancer. CMAJ. 1997;157:1205–1212. [PMC free article] [PubMed] [Google Scholar]
- 25.Muscat JE, Huncharek MS. Breast self-examination and extent of disease: a population-based study. Cancer Detect Prev. 1991;15:155–159. [PubMed] [Google Scholar]
- 26.Newcomb PA, Weiss NS, Storer BE, Scholes D, Young BE, Voigt LF. Breast self-examination in relation to the occurrence of advanced breast cancer. J Natl Cancer Inst. 1991;83:260–265. doi: 10.1093/jnci/83.4.260. [DOI] [PubMed] [Google Scholar]
- 27.Miller AB. [cited 2005 March 29];We disagree with Baxters criticism of previous studies. 2001 Sep 17 Available from http://www.cmaj.ca/cgi/eletters/164/13/1837#29.
- 28.Nekhlyudov L, Fletcher SW. Is it time to stop teaching breast self-examination? CMAJ. 2001;164:1851–1852. [PMC free article] [PubMed] [Google Scholar]
- 29.Lerner BH. When statistics provide unsatisfying answers: revisiting the breast self-examination controversy. CMAJ. 2002;166:199–201. [PMC free article] [PubMed] [Google Scholar]
- 30.Dillman DA. Mail and telephone surveys: the total design method. Toronto, Ont: John Wiley and Sons; 1978. [Google Scholar]
- 31.Tracy CS, Dantas GC, Moineddin R, Upshur RE. The nexus of evidence, context, and patient preferences in primary care: postal survey of Canadian family physicians. BMC Fam Pract. 2003;4:13. doi: 10.1186/1471-2296-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tudiver F, Herbert C, Goel V. Why don’t family physicians follow clinical practice guidelines for cancer screening? CMAJ. 1998;159:797–798. [PMC free article] [PubMed] [Google Scholar]
- 33.Thomas DB, Gao DL, Ray RM, Wang WW, Allison CJ, Chen FL, et al. Randomized trial of breast self-examination in Shanghai; final results. J Natl Cancer Inst. 2002;94:1445–1457. doi: 10.1093/jnci/94.19.1445. [DOI] [PubMed] [Google Scholar]
- 34.Beaulieu MD, Hudon E, Roberge D, Pineault R, Forte D, Legare J. Practice guidelines for clinical prevention: do patients, physicians and experts share common ground? CMAJ. 1999;161:519–523. [PMC free article] [PubMed] [Google Scholar]