Abstract
OBJECTIVE
To determine the prevalence of neuroleptic use in long-term care institutions in the greater Montreal, Que, area and to estimate the extent of use of atypical neuroleptics.
DESIGN
Cross-sectional study in which single-day chart reviews were conducted to evaluate the prevalence of use of conventional and atypical neuroleptics.
SETTING
Ten long-term care institutions in the greater Montreal area.
PARTICIPANTS
Two thousand, four hundred sixty residents aged 65 years or older living in 10 long-term care institutions in and around Montreal.
MAIN OUTCOME MEASURES
Single-day medication profiles compiled by institutions’ pharmacists.
RESULTS
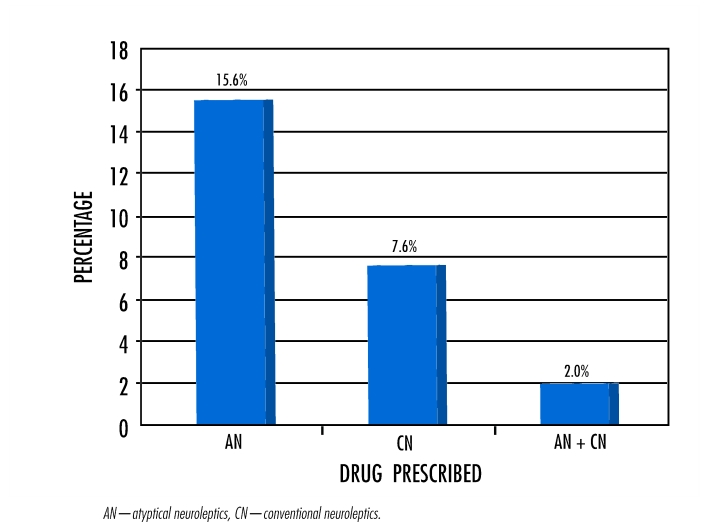
Among patients in the 10 participating institutions, use of neuroleptics ranged from 15% to 37% with a mean of 25.2% (620/2460). Atypical neuroleptics were prescribed to 15.6%, conventional neuroleptics to 7.6%, and a combination of both to 2.0% of the 2460 patients.
CONCLUSION
Use of neuroleptics was relatively prevalent, and there was wide use of atypical neuroleptics in Montreal-area long-term care institutions. There is little information on the safety and efficacy of these medications for institutionalized elderly people.
Abstract
OBJECTIF
Déterminer la prévalence d’utilisation des neuroleptiques dans certains centres d’hébergement à long terme du grand Montréal et estimer celle des neuroleptiques atypiques.
TYPE D’ÉTUDE
Étude transversale dans laquelle on a consulté les dossiers d’une seule journée pour évaluer la prévalence d’utilisation des neuroleptiques classiques et atypiques.
CONTEXTE
Dix centres d’hébergement à long terme du grand Montréal.
PARTICIPANTS
Deux mille quatre cent soixante personnes de 65 ans et plus vivant dans 10 centres de soins de longue durée de Montréal ou des environs.
PRINCIPAUX PARAMÈTRES ÉTUDIÉS
Les profils médicamenteux d’une seule journée établis par le pharmacien du centre.
RÉSULTATS
L’utilisation des neuroleptiques chez les patients des 10 institutions participantes variait de 15 à 37%, avec une moyenne de 25,2% ( 620 sur 2460). Sur les 2460 patients, 15,6% avaient reçu des neuroleptiques atypiques, 7,6% des neuroleptiques classiques et 2% une combinaison des deux.
CONCLUSION
Dans ces centres de soins de longue durée du grand Montréal, la prévalence d’utilisation des neuroleptiques était relativement élevée, notamment pour les neuroleptiques atypiques. On possède peu de données sur la sécurité et l’efficacité de ces médicaments chez les personnes âgées hébergées dans ces institutions.
EDITOR’S KEY POINTS.
Family doctors frequently use neuroleptics to treat institutionalized elderly patients’ behavioural problems despite the risk of extrapyramidal symptoms.
This study in Montreal found that, overall, 26% of residents were prescribed neuroleptics: 16% atypical neuroleptics, 8% conventional neuroleptics, and 2% a combination of both.
The most commonly prescribed neuroleptics were risperidone (52%), haloperidol (36%), and olanzapine (13%).
Newer atypical neuroleptics appear to be widely prescribed, even though there is limited evidence of their efficacy. They might be chosen, however, because of a lower incidence of extrapyramidal symptoms.
POINTS DE REPÈRE DU RÉDACTEUR.
Le médecin de famille prescrit souvent des neuroleptiques aux patients âgés des centres d’hébergement qui présentent des troubles du comportement et ce, malgré les risques d’effets extrapyramidaux.
Cette étude montréalaise révèle que dans l’ensemble, 26% des patients hébergés recevaient des neuroleptiques: 16% des neuroleptiques atypiques, 8% des neuroleptiques classiques et 2% un combinaison des deux.
Les neuroleptiques les plus souvent prescrits étaient la rispéridone (52%), l’halopéridol (36%) et l’olanzapine (13%).
Les nouveaux neuroleptiques atypiques sont apparemment prescrits de façon judicieuse, malgré le peu de preuve de leur efficacité. Leur choix pourrait toutefois dépendre du fait qu’ils entraînent moins d’effets extrapyramidaux.
In Canada, 50% of elderly people with dementia are institutionalized.1,2 More than 90% of them have behavioural disorders, particularly when they are at moderate-to-severe stages of dementia.3 Although the efficacy of neuroleptics for treating behavioural disorders in dementia has been shown to be modest,4 these medications are still widely used for this indication.5,6
Some studies comparing neuroleptics with placebo show improvement in hallucinations, agitation, and resistance to care among patients treated with neuroleptics.7 According to studies completed in the United States in the 1980s and early 1990s, one quarter to one third of residents in nursing homes were prescribed conventional neuroleptics (CNs).7-9
Haloperidol is the most commonly used CN. Serious adverse effects have been seen with use of CNs, particularly in frail institutionalized elderly patients. These medications can induce sedation; hypotension; anticholinergic effects; cardiovascular, gastrointestinal, and endocrinologic problems; hypersensitivity reactions; and extrapyramidal signs.10 Extrapyramidal signs are attributable to the antidopaminergic properties of neuroleptics. They include parkinsonism, akathisia, dystonia, and dyskinesia. According to population studied, methodology, and type of neuroleptics used, various studies report a prevalence of extrapyramidal signs ranging from 5% to 67% among elderly patients prescribed CNs.11 These side effects can come on suddenly or appear insidiously, generally within the first 30 days of use.
Atypical neuroleptics (ANs) (risperidone, olanzapine, quetiapine, and clozapine) were introduced in the 1990s. They show less affinity for dopaminergic receptors and greater affinity for serotonergic receptors.11,12 These pharmacodynamic properties could result in greater efficacy and fewer side effects for young schizophrenic patients.11,13-17
Quality of evidence
We searched PubMed, Ovid Citations, and Current Contents for randomized controlled trials carried out among elderly patients that evaluated the efficacy and safety of ANs. We identified only three studies using the key words dementia, Alzheimer’s disease, Lewy body disease, psychotic disorders, behavior disorders, pharmacotherapy, drugs, antipsychotic agents, atypical antipsychotics, randomized controlled trial, placebo, and double-blind method.18-20 These three trials suggested that ANs were superior to placebo but had modest efficacy. The only trial comparing a CN with an AN showed that haloperidol, risperidone, and placebo had similar efficacy.18
De Deyn et al18 and Katz et al19 reported a prevalence of extrapyramidal signs ranging from 7% to 22%, depending on type of neuroleptic used and dose given. Street et al20 found no significant differences in prevalence of extrapyramidal signs among elderly subjects taking placebo, and 5 mg, 10 mg, and 15 mg of olanzapine. Results reported in these three trials are insufficient to prove there is a real difference in prevalence of extrapyramidal signs among elderly patients prescribed ANs or CNs.
Objectives of study
The objectives of this study were to describe neuroleptic use and to estimate the extent of use of ANs in long-term care institutions in Montreal, Que. Greater knowledge of actual patterns of neuroleptic prescribing in long-term care institutions could help identify areas of continuing medical education for physicians and could be used as a starting point for development of Canadian guidelines on use of neuroleptics.
METHODS
Ten long-term care institutions in the greater Montreal, Que, area were randomly selected from among the Collaborative Research Network in long-term care, which consists of 17 institutions. This was a convenience sample, but it represented one third of Montreal’s long-term care institutions. The survey was conducted between October 2000 and April 2001. All residents aged 65 and older living in the participating institutions were included in the study. This study was approved by the research ethics committee of l’Institut universitaire de gériatrie de Montréal and by the research ethics committee or the committee of physicians, dentists, and pharmacists of each participating institution.
For each institution, the pharmacist was asked to provide data from a single-day medication profile for each neuroleptic user. These profiles included the date of the profile corresponding to the date of data extraction by the pharmacist; characteristics of patients, including date of birth, sex, and date of admission to the institution; and data on neuroleptic prescriptions, including generic name, date of prescription, dose, frequency, and route of administration. Use of the following medications were also recorded, as they can influence presence of extrapyramidal signs: antiparkinsonian agents, such as levodopa; antidepressants; benzodiazepines; sedatives; cholinesterase inhibitors; anticonvulsants; lithium; and anticholinergic agents, such as procyclidine.
The prevalence of neuroleptic use by those 65 or older was determined for each institution first, and then the mean prevalence was calculated for the 10 institutions. With this approach, each institution had equal weight, regardless of size. We also calculated the mean prevalence of neuroleptic users, using the total number of residents in the 10 institutions as a denominator. These two approaches were used to evaluate whether size of institution influenced estimates of prevalence. The prevalence of use of CNs, ANs, or a combination of both types (CN+AN) was estimated for each institution and for the 10 institutions overall. Use of medications that can influence presence of extrapyramidal signs was also analyzed. For comparing our results with those of previous studies, dose and duration of treatment were estimated only for neuroleptics prescribed on a regular basis and administered orally.
In the context of this study, we could not verify whether neuroleptics prescribed only as needed (PRN) were administered or not. Only neuroleptics prescribed on a regular basis were considered in the analysis. Mean daily doses of neuroleptics used on a regular basis were calculated and compared with maximum geriatric daily doses recommended by the United States Omnibus Budget Reconciliation Act (OBRA-87) legislation: 4 mg for haloperidol, 2 mg for risperidone, 10 mg for olanzapine, and 200 mg for quetiapine.21 We compared our results with American guidelines since no Canadian guidelines on neuroleptic prescribing in long-term care were available. Duration of treatment was analyzed according to a binary method; 180 days or more was considered a long duration of treatment.
The association between type of neuroleptic prescribed and characteristics of residents (age, sex, length of stay, and use of other medications) was analyzed using multinomial logistic regressions to determine which factors were related to use of CNS, ANs, or CN+AN. The association between medications that can influence presence of extrapyramidal signs and characteristics of residents were analyzed using logistic regression. Logistic regressions were also used to analyze the association between high doses of neuroleptics and characteristics of residents and the association between duration of treatment and characteristics of residents. All analyses were adjusted considering the institutions as fixed factors.22
RESULTS
Our sample was composed of eight public institutions and two private institutions caring for a total of 2460 residents. Three institutions had fewer than 150 beds, four had between 150 and 300, and the other three had more than 300 beds. Four institutions were affiliated with universities.
Prevalence of neuroleptic use
The mean prevalence of neuroleptic use calculated from the prevalence in each of the 10 institutions was 25.8% ± 6.3% (range 15% to 37%). The mean prevalence of neuroleptic use among all 2460 residents was 25.2% (620/2460). These results show that the size of the institution had little influence on the mean prevalence of neuroleptic use. Therefore, for the rest of the analysis, mean prevalence was based on the 620 neuroleptic users. Mean age of neuroleptic users was 84 years (range 65 to 102 years); more women (75%) than men were prescribed neuroleptics. Mean length of stay in an institution was 2.5 years (range 6 days to 23 years).
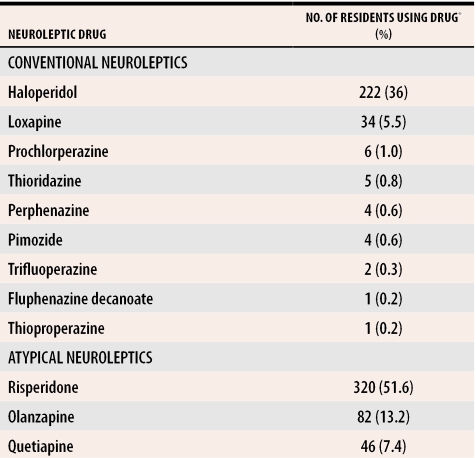
For the 620 neuroleptic users, 757 prescriptions were identified for an average of 1.22 prescriptions per resident. Figure 1 shows the proportion of residents receiving ANs, CNs, or AN+CN. Table 1 shows the number of residents prescribed each type of neuroleptic. No resident in our sample was prescribed clozapine.
Figure 1. Prevalence of neuroleptic use according to type.
N = 2460
Table 1. Relative frequencies of use of conventional and atypical neuroleptics.
N =620.
*Some patients were taking more than one drug.
Risperidone was most frequently prescribed (52%), followed by haloperidol (36%), olanzapine (13%), and quetiapine (7%). The most common combinations (n = 46) were one of the three ANs prescribed on a regular basis with haloperidol PRN. Risperidone appeared in 41% of these combinations, olanzapine in 26%, and quetiapine in 13%.
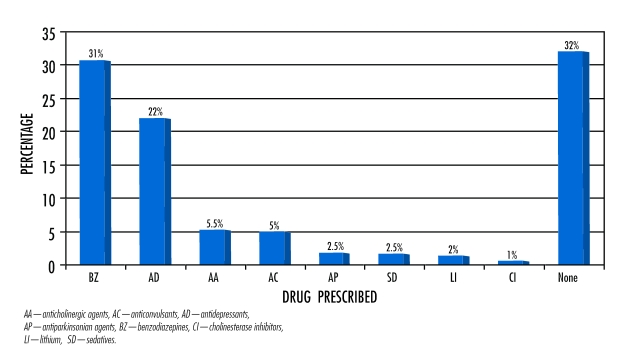
Figure 2 shows the distribution of other psychotropic drugs among neuroleptic users. Benzodiazepines were the most frequently prescribed (31%), followed by antidepressants (22%). Only 32% of neuroleptic users were not using these medications. Overall, 79% of neuroleptics were prescribed on a regular basis and 21% PRN. Almost half (46%) the haloperidol prescriptions, but only 13% of the risperidone prescriptions, were PRN.
Figure 2. Distribution of other psychotropic drugs among neuroleptic users.
N = 620
Doses
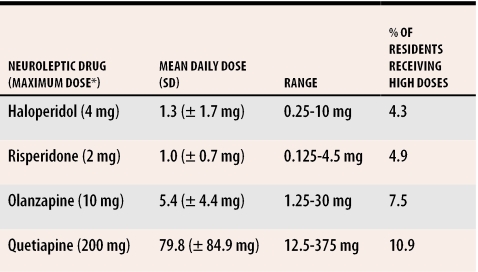
Daily doses of risperidone, haloperidol, olanzapine, and quetiapine were evaluated, since they were the most frequently prescribed (543 prescriptions, 92% of our sample). Table 221 shows the mean daily dose, standard deviation, range of dose given, and proportion of residents receiving high doses. High dose was defined as above the maximum daily dose recommended in OBRA-87. Quetiapine was most likely to be prescribed at a dose exceeding the maximum recommended geriatric daily dose (10.9%), followed by olanzapine (7.5%), risperidone (4.9%), and haloperidol (4.3%). Duration of treatment was also estimated for all oral neuroleptics prescribed on a regular basis (n = 590). Results show that 19% of neuroleptic prescriptions had been initiated within 30 days preceding the study, 39% were active in a range of 30 days to 180 days, and 42% had been ongoing for 180 days and more.
Table 2. Daily neuroleptic dose prescribed.
N = 543 prescriptions.
*Maximum daily dose according to the OBRA-87 (Omnibus Budget Reconciliation Act).21
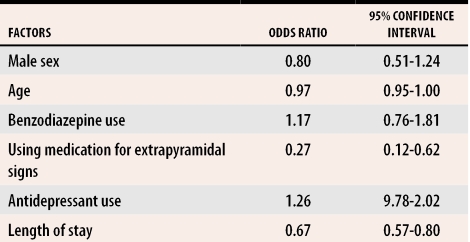
Results were adjusted considering the institutions as fixed factors. For comparisons between types of neuroleptics, CN users were considered the reference group. Compared with CN users, AN users were more likely to have a shorter length of stay in an institution (odds ratio [OR] 0.67, 95% confidence interval [CI] 0.57 to 0.80), were less likely to be prescribed medications used to treat extrapyramidal signs (OR 0.27, 95% CI 0.12 to 0.62), and were relatively younger (OR 0.97, 95% CI 0.95 to 1.00) (Table 3). We created various multiple logistic regression models to identify characteristics that would make patients more likely to be taking psychotropic drugs other than neuroleptics. Increasing age was the only factor associated with decreased risk of receiving antidepressants (OR 0.97, 95% CI 0.94 to 0.99), benzodiazepines (OR 0.74, 95% CI 0.95 to 99), and medications used to treat extrapyramidal signs (OR 0.90, 95% CI 0.86 to 0.95).
Table 3. Multiple logistic regression model comparing atypical neuroleptic users with conventional neuroleptic users.
Conventional neuroleptic users were the reference group.
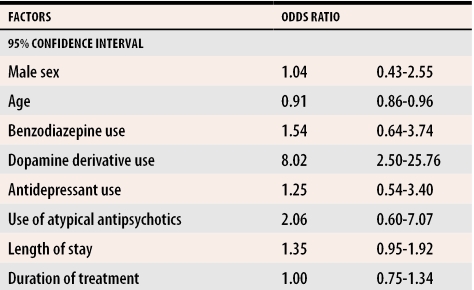
Likelihood of receiving high doses of neuroleptics was inversely related to age (OR 0.91, 95% CI 0.86 to 0.96) (Table 4). Patients prescribed high doses were eight times more likely to receive medications used to treat extrapyramidal signs (OR 8.02, 95% CI 2.50 to 25.76).
Table 4.
Multiple logistic regression model to identify patient characteristics associated with use of high-dose neuroleptics
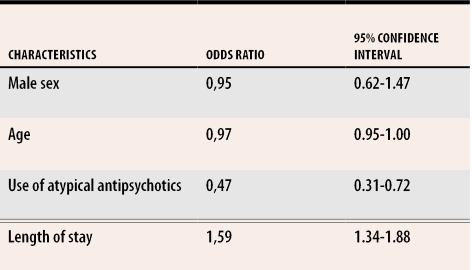
Duration of treatment
Another multiple logistic regression model was used to predict factors associated with treatment exceeding 180 days. Results are shown in Table 5. Relatively younger users were less likely to receive neuroleptics for a long period (OR 0.97, 95% CI 0.95 to 1.00), and AN users were less likely to have a long duration of treatment (OR 0.47, 95% CI 0.31 to 0.72). Longer stay in an institution (OR 1.60, 95% CI 1.34 to 1.88) was related to a higher probability of having a long duration of treatment with neuroleptics.
Table 5.
Multiple logistic regression model to identify patient characteristics associated with duration of treatment with neuroleptics exceeding 180 days
DISCUSSION
In this cross-sectional study, the mean prevalence of neuroleptic use among institutionalized elderly people was 25.2%. Our sample was a convenience sample and does not necessarily represent all Montreal’s institutionalized elderly residents. Nevertheless, it represents one third of all residents. Use of PRN prescriptions was almost exclusively for haloperidol and risperidone. This is likely due to their pharmacokinetic properties (both medications reach their peak concentration rapidly) and to the fact that they are both available in small and variable doses. Conn et al,5 in an Ontario study, reported a prevalence of neuroleptic prescriptions of 29.8% among 436 nursing home residents and of 20.3% among 442 residents of a veterans’ institution, but of only 14.8% among 1405 residents living in homes for the aged.
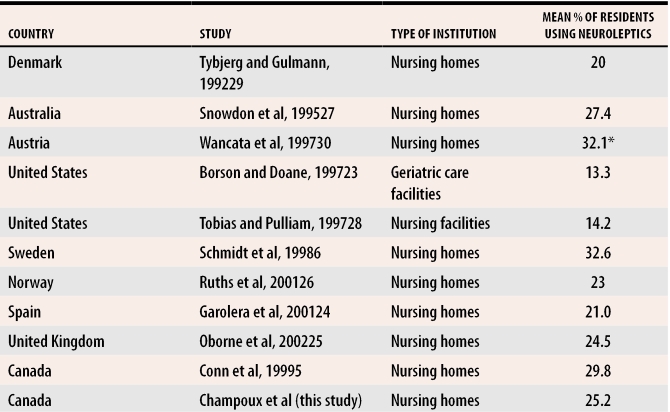
Overall, neuroleptic use in Canada is comparable to use in other countries,5,6,23-30 but is somewhat higher than in the United States since implementation of OBRA-87. Table 65,6,23-30 shows neuroleptic use among nursing home residents in various countries. Only studies published after 1990 were considered because use of neuroleptics has changed markedly in the United States since implementation of OBRA-87.
Table 6.
Prevalence of neuroleptic use among nursing home residents in various countries since 1989
*Newly admitted patients only.
Use despite modest efficacy
Our study shows wide use of neuroleptics despite their modest efficacy. This finding might reflect the lack of more effective treatment. The distress experienced by demented residents with behavioural disorders and their caregivers can partly explain this high use. According to our clinical experience, once physicians initiate neuroleptic treatment, the drugs are prescribed for very long periods, often until patients die, without considering trying to reduce or stop the medication.
We also found physicians were prescribing ANs despite the lack of scientific evidence to support this practice. The frailty of institutionalized patients could explain why physicians switch to ANs; they are safer.
Among the three trials we found in our literature search,18-20 only one compared a CN (haloperidol) to an AN (risperidone).18 The efficacy of the two drugs appeared to be similar, but presence of extrapyramidal signs was lower with risperidone (15% of patients) than haloperidol (22%) (P <.05).
In our study, the proportion of residents receiving high doses of neuroleptics was relatively low. Perhaps physicians practising in long-term care institutions are aware of the increased risks of side effects when prescribing for this frail population. About 42% of neuroleptic users, however, had active prescriptions for 180 days or more. This rather long duration of treatment raises concern since neuroleptics’ long-term efficacy in this population has not been evaluated. Moreover, clinical trials conducted over short periods report that CNs have only modest effects on elderly people’s behavioural disorders31-33 and that prolonged exposure to neuroleptics could increase risk of developing extrapyramidal signs, especially tardive dyskinesia.34-37
The newer ANs were prescribed relatively more frequently (62.1%) despite a lack of information on use of these medications for institutionalized elderly patients and their relatively high cost compared with CNs.
Other drugs prescribed to neuroleptic users
Benzodiazepines were prescribed to 31% of neuroleptic users. Considering that both medications can affect mobility and increase risk of falls in frail elderly people, this relatively frequent combination raises concern. Among the antidepressants prescribed to 22% of patients, 60% were selective serotonin reuptake inhibitors, such as sertraline and paroxetine, both of which can cause extrapyramidal signs. We also found concurrent use of antiparkinsonian and anticholinergic agents in neuroleptic users; high-dose neuroleptic users were more likely to receive anticholinergic agents. It was impossible to determine whether these residents suffered from Parkinson disease or had side effects from neuroleptics. Such confusion could result in addition of dopaminergic drugs.38
Reducing doses or discontinuing neuroleptics
Whenever possible, reducing the dose or discontinuing the neuroleptic should be considered.38 Use of CNs is strongly related to use of anticholinergic agents, but use of AN+CN is not. This difference could be explained by the fact that CNs in combination were prescribed only PRN.
Older residents seem protected against long duration of treatment with neuroleptics, high doses of neuroleptics, and use of medications that can affect presence of extrapyramidal signs. Nevertheless, a prolonged stay in a long-term care institution increases the probability of receiving CNs and of using neuroleptics for more than 180 days. This could be because CN users were probably initially treated with CNs and were never switched to newer neuroleptics.
Limitations
It was impossible to ascertain how often PRN medications were actually administered without an extensive, time-consuming review of each resident’s chart because the information was collected through institutions’ computerized pharmacy databases. Second, it was impossible to determine whether residents using neuroleptics were suffering from dementia or any other psychiatric disorders, such as schizophrenia. We hope that other studies will address the many unanswered questions about institutionalized seniors’ use of neuroleptics.
Conclusion
Results of our study have shed light on use of neuroleptics in Montreal long-term care institutions and on use of medications that can affect the presence of extrapyramidal signs. Prevalence of use of neuroleptics continues to be relatively high (25.2%) among institutionalized elderly people; use of ANs is extensive (62.1%) even though little information exists about the safety and efficacy of these medications in this population.
Biographies
Dr Champoux is an Associate Professor in the Department of Family Medicine at the University of Montreal in Quebec.
Dr Monette is an Assistant Professor in the Department of Medicine at McGill University in Montreal.
Ms Monette is an Occupational Therapist practising in Montreal.
Dr Galbaud du Fort is an Assistant Professor in the Department of Psychiatry at McGill University.
Dr Wolfson is a Professor in the Department of Epidemiology and Biostatistics at McGill University.
Mr Le Cruguel is a statistician in Montreal.
Footnotes
Competing interests: None declared
References
- 1.Beck C, Frank L, Chumbler NR, O’Sullivan P, Vogelpohl TS, Rasin J, et al. Correlates of disruptive behavior in severely cognitively impaired nursing home residents. Gerontologist. 1998;38(2):189–198. doi: 10.1093/geront/38.2.189. [DOI] [PubMed] [Google Scholar]
- 2.Canadian Medical Association. Canadian study of health and aging: study methods and prevalence of dementia. CMAJ. 1994;150(6):899–913. [PMC free article] [PubMed] [Google Scholar]
- 3.Goldberg RJ, Goldberg J. Risperidone for dementia-related disturbed behavior in nursing home residents: a clinical experience. Int Psychogeriatr. 1997;9(1):65–68. doi: 10.1017/s1041610297004213. [DOI] [PubMed] [Google Scholar]
- 4.Carlyle W, Ancill RJ, Sheldon L. Aggression in the demented patient: a double-blind study of loxapine versus haloperidol. Int Clin Psychopharmacol. 1993;8(2):103–108. doi: 10.1097/00004850-199300820-00004. [DOI] [PubMed] [Google Scholar]
- 5.Conn DK, Ferguson I, Mandelman K, Ward C. Psychotropic drug utilization in long-term-care facilities for the elderly in Ontario, Canada. Int Psychogeriatr. 1999;11(3):223–233. doi: 10.1017/s1041610299005797. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt I, Claesson CB, Westerholm B, Nilsson LG, Svarstad BL. The impact of regular multidisciplinary team interventions on psychotropic prescribing in Swedish nursing homes. J Am Geriatr Soc. 1998;46(1):77–82. doi: 10.1111/j.1532-5415.1998.tb01017.x. [DOI] [PubMed] [Google Scholar]
- 7.Maletta GJ. Pharmacologic treatment and management of aggressive demented patients. Psychiatr Ann. 1990;20(8):446–455. [Google Scholar]
- 8.Arling G, Ryther BJ, Collins T, Zimmerman D. Mental illness and psychotropic medication use in the nursing home. J Aging Health. 1991;3(4):455–472. doi: 10.1177/089826439100300402. [DOI] [PubMed] [Google Scholar]
- 9.Avorn J, Dreyer P, Connelly K, Soumerai SB. Use of psychoactive medication and the quality of care in rest homes. Findings and policy implications of a statewide study. N Engl J Med. 1989;320(4):227–232. doi: 10.1056/NEJM198901263200406. [DOI] [PubMed] [Google Scholar]
- 10.Bezchlibnyk-Butler KZ. Clinical handbook of psychotropic drugs. 9th ed. Cambridge, Mass: Hogrefe and Huber Publishing; 1999. [Google Scholar]
- 11.Saltz BL, Woerner MG, Robinson DG, Kane JM. Side effects of antipsychotic drugs. Avoiding and minimizing their impact in elderly patients. Postgrad Med. 2000;107(2):169–178. doi: 10.3810/pgm.2000.02.891. [DOI] [PubMed] [Google Scholar]
- 12.Finkel SI. Psychotherapeutic agents in older adults. Antipsychotics: old and new. Clin Geriatr Med. 1998;14(1):87–100. [PubMed] [Google Scholar]
- 13.Chouinard G, Jones B, Remington G, Bloom D, Addington D, MacEwan GW, et al. A Canadian multicentre placebo-controlled study of fixed doses of risperidone and haloperidol in the treatment of chronic schizophrenic patients. J Clin Psychopharmacol. 1993;13(1):25–40. [PubMed] [Google Scholar]
- 14.Clozapine Study Group. The safety and efficacy of clozapine in severe treatment-resistant schizophrenic patients in the UK. Br J Psychiatry. 1993;163:150–154. doi: 10.1192/bjp.163.2.150. [DOI] [PubMed] [Google Scholar]
- 15.Geddes J, Freemantle N, Harrison P, Bebbington P. Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis. BMJ. 2000;321:1371–1376. doi: 10.1136/bmj.321.7273.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marder SR, Meibach RC. Risperidone in the treatment of schizophrenia. Am J Psychiatry. 1994;151(6):825–835. doi: 10.1176/ajp.151.6.825. [DOI] [PubMed] [Google Scholar]
- 17.Markowitz JS, Brown CS, Moore R. Atypical antipsychotics. Part I: pharmacology, pharmacokinetics, and efficacy. Ann Pharmacother. 1999;33(1):73–85. doi: 10.1345/aph.17215. [DOI] [PubMed] [Google Scholar]
- 18.De Deyn PP, Rabheru K, Rasmussen A, Bocksberger JP, Dautzenberg PF, Eriksson S, et al. A randomized trial of risperidone, placebo, and haloperidol for behavioral symptoms of dementia. Neurology. 1999;53(5):946–955. doi: 10.1212/wnl.53.5.946. [DOI] [PubMed] [Google Scholar]
- 19.Katz IR, Jeste DV, Mintzer JE, Clyde C, Napolitano J, Brecher M. Comparison of risperidone and placebo for psychosis and behavioral disturbances associated with dementia: a randomized, double-blind trial. Risperidone Study Group. J Clin Psychiatry. 1999;60(2):107–115. doi: 10.4088/jcp.v60n0207. [DOI] [PubMed] [Google Scholar]
- 20.Street JS, Clark WS, Gannon KS, Cummings JL, Bymaster FP, Tamura RN, et al. Olanzapine treatment of psychotic and behavioral symptoms in patients with Alzheimer disease in nursing care facilities: a double-blind, randomized, placebo-controlled trial. The HGEU Study Group. Arch Gen Psychiatry. 2000;57(10):968–976. doi: 10.1001/archpsyc.57.10.968. [DOI] [PubMed] [Google Scholar]
- 21.Gurvich T, Cunningham JA. Appropriate use of psychotropic drugs in nursing homes. Am Fam Physician. 2000;61(5):1437–1446. [PubMed] [Google Scholar]
- 22.Agresti A. Categorical data analysis. New York, NY: John Wiley and Sons; 1990. [Google Scholar]
- 23.Borson S, Doane K. The impact of OBRA-87 on psychotropic drug prescribing in skilled nursing facilities. Psychiatr Serv. 1997;48(10):1289–1296. doi: 10.1176/ps.48.10.1289. [DOI] [PubMed] [Google Scholar]
- 24.Garolera D, Bendahan G, Gras R, Benaque A, San Jose A, Vilardell M. [Psychoactive drug use in nursing homes]. Med Clin (Barc) 2001;117(16):615–616. doi: 10.1016/s0025-7753(01)72196-3. [DOI] [PubMed] [Google Scholar]
- 25.Oborne CA, Hooper R, Li KC, Swift CG, Jackson SH. An indicator of appropriate neuroleptic prescribing in nursing homes. Age Ageing. 2002;31(6):435–439. doi: 10.1093/ageing/31.6.435. [DOI] [PubMed] [Google Scholar]
- 26.Ruths S, Straand J, Nygaard HA. Psychotropic drug use in nursing homes—diagnostic indications and variations between institutions. Eur J Clin Pharmacol. 2001;57:523–528. doi: 10.1007/s002280100348. [DOI] [PubMed] [Google Scholar]
- 27.Snowdon J, Vaughan R, Miller R, Burgess EE, Tremlett P. Psychotropic drug use in Sydney nursing homes. Med J Aust. 1995;163(2):70–72. doi: 10.5694/j.1326-5377.1995.tb126117.x. [DOI] [PubMed] [Google Scholar]
- 28.Tobias DE, Pulliam CC. General and psychotherapeutic medication use in 878 nursing facilities: a 1997 national survey. Consultant Pharmacist. 1997;12(12):1401–1408. [Google Scholar]
- 29.Tybjerg J, Gulmann NC. [Use of psychopharmaceuticals in municipal nursing homes. A nationwide survey. ] Ugeskr Laeger. 1992;154:3126–3129. [PubMed] [Google Scholar]
- 30.Wancata J, Benda N, Meise U, Muller C. Psychotropic drug intake in residents newly admitted to nursing homes. Psychopharmacology (Berl) 1997;134(2):115–120. doi: 10.1007/s002130050432. [DOI] [PubMed] [Google Scholar]
- 31.Devanand DP, Marder K, Michaels KS, Sackeim HA, Bell K, Sullivan MA, et al. A randomized, placebo-controlled dose-comparison trial of haloperidol for psychosis and disruptive behaviors in Alzheimer’s disease. Am J Psychiatry. 1998;155(11):1512–1520. doi: 10.1176/ajp.155.11.1512. [DOI] [PubMed] [Google Scholar]
- 32.Finkel SI, Lyons JS, Anderson RL, Sherrell K, Davis J, Cohen-Mansfield J, et al. A randomized placebo-controlled trial of thiothixene in agitated, demented nursing home patients. Int J Geriatr Psychiatry. 1995;10:129–136. [Google Scholar]
- 33.Schneider LS, Pollock VE, Lyness SA. A meta-analysis of controlled trials of neuroleptic treatment in dementia. J Am Geriatr Soc. 1990;38(5):553–563. doi: 10.1111/j.1532-5415.1990.tb02407.x. [DOI] [PubMed] [Google Scholar]
- 34.Avorn J, Monane M, Everitt DE, Beers MH, Fields D. Clinical assessment of extrapyramidal signs in nursing home patients given antipsychotic medication. Arch Intern Med. 1994;154(10):1113–1117. [PubMed] [Google Scholar]
- 35.Caligiuri MR, Jeste DV, Lacro JP. Antipsychotic-induced movement disorders in the elderly: epidemiology and treatment recommendations. Drugs Aging. 2000;17(5):363–384. doi: 10.2165/00002512-200017050-00004. [DOI] [PubMed] [Google Scholar]
- 36.Jeste DV, Lacro JP, Palmer B, Rockwell E, Harris MJ, Caligiuri MP. Incidence of tardive dyskinesia in early stages of low-dose treatment with typical neuroleptics in older patients. Am J Psychiatry. 1999;156(2):309–311. doi: 10.1176/ajp.156.2.309. [DOI] [PubMed] [Google Scholar]
- 37.Woerner MG, Alvir JM, Saltz BL, Lieberman JA, Kane JM. Prospective study of tardive dyskinesia in the elderly: rates and risk factors. Am J Psychiatry. 1998;155(11):1521–1528. doi: 10.1176/ajp.155.11.1521. [DOI] [PubMed] [Google Scholar]
- 38.Avorn J, Bohn RL, Mogun H, Gurwitz JH, Monane M, Everitt D, et al. Neuroleptic drug exposure and treatment of parkinsonism in the elderly: a case-control study. Am J Med. 1995;99(1):48–54. doi: 10.1016/s0002-9343(99)80104-1. [DOI] [PubMed] [Google Scholar]