CAN YOU IDENTIFY THIS CONDITION?
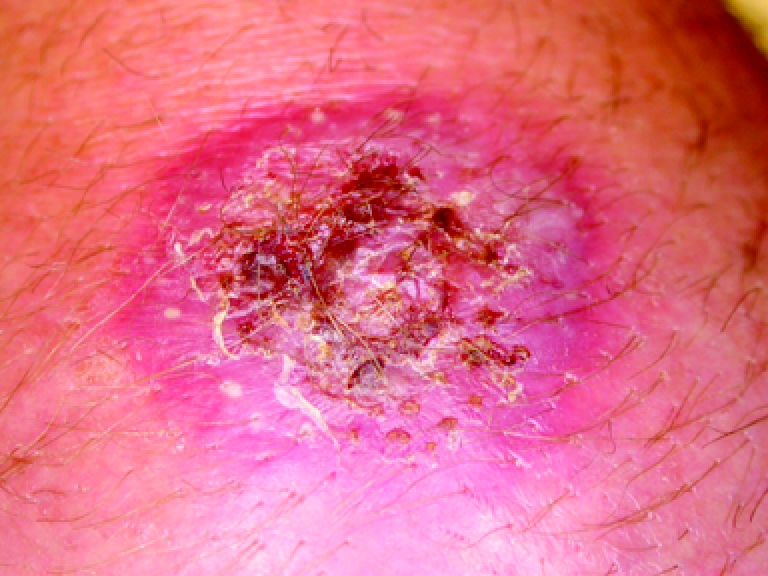
A 57-year-old farmer presents with edema, erythema, and a cutaneous lesion on the back of his right hand. The lesion first appeared 10 days before as a small, erythematous, pruritic macule and disappeared shortly thereafter. It reappeared 8 days later and became bigger. The farmer was otherwise healthy and was taking no medication. He had no known drug allergies. On examination, his right hand appeared erythematous, swollen, and warm, and it had a 3-cm erythematous scaly plaque on the back. Results of his examination were otherwise normal.
The most likely diagnosis is:
Spider-bite reaction
Psoriasis with inflammation secondary to bacterial infection
Dermatophyte infection (tinea)
Rickettsial infection (tick-bite eschar)
Granuloma annulare
3. Dermatophyte infection (tinea)
The dermatophytes are a group of fungi that invade the superficial layer of the epidermis and survive on the keratin of skin, hair, and nails. A dermatophyte infection results in increased skin proliferation, scaling, and epidermal thickening.1 Cutaneous dermatophyte infections are common in the general population; up to 20% of people are infected at any time.2 Most of these infections are not life threatening, but they can cause morbidity in immunocompromised and diabetic patients. It is important, therefore, for primary care physicians to recognize and treat these infections appropriately.
Dermatophyte infections involving the skin are called epidermal dermatophytoses. These infections are the most common dermatophytic infections2 and can involve the feet, hands, groin, face, trunk, and extremities (Table 1). Infection can last from months to years. Patients might have no symptoms or seek help for pruritus.1 Tinea pedis affects up to 70% of adults worldwide.2
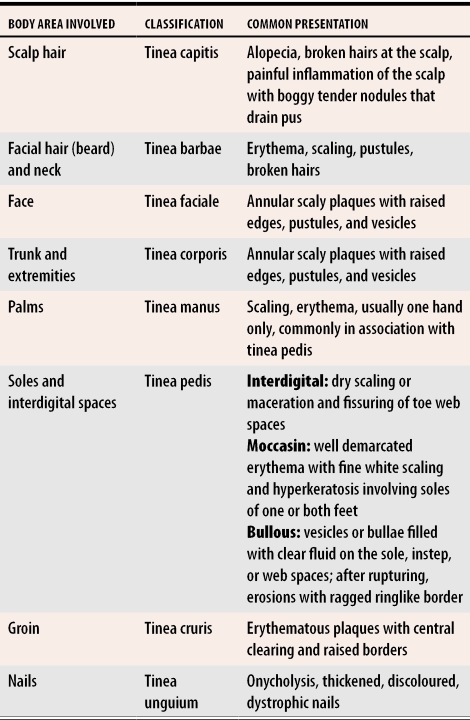
Table 1.
Clinical classification of cutaneous dermatophyte infections according to body area involved
Adapted from Martin et al.1
Dermatophyte infections involving the nails are called onychomycoses or tinea unguium. Adults are most commonly affected; children are rarely affected. About 40% of those older than 70 years are affected.2 Infection does not usually remit spontaneously.
Risk factors for developing onychomycosis include atopy, diabetes mellitus, immunosuppression, occlusive footwear, nail trauma, and cutaneous diseases affecting the nails, such as psoriasis.2 Differential diagnosis can include psoriasis, lichen planus, traumatic injury, and congenital nail dystrophies.2 Clinical appearance can vary with site, fungal species involved, and host response. Appearance alters with inappropriate use of steroid creams. Zoophilic infections (fungi from animal sources) often have a more inflammatory presentation.2
Trichomycoses are dermatophyte infections involving the hair. Tinea capitis is most common in preschool-aged black children.2 Trichophyton tonsurans is a causative agent in most cases; it does not fluoresce on Wood’s lamp examination.2 Lesions usually last weeks to months. Tinea barbae is a dermatophytic trichomycosis involving the beard and moustache area. It resembles tinea capitis and invades the hair shaft. It occurs only in adult men and is more common among farmers.1
Diagnosis
Diagnosis of dermatophytosis relies on history and characteristic cutaneous findings, but can be confirmed by laboratory investigations that include potassium hydroxide (KOH) microscopy, fungal culture, and skin or nail biopsy.2 Wood’s lamp examination can be useful in confirming a hair infection with zoophilic dermatophytes (eg, Microsporum canis and Microsporum audouinii) that produce blue-green fluorescence.2 In general, this investigation is of limited diagnostic value because most dermatophytes in North America do not fluoresce.
Treatment
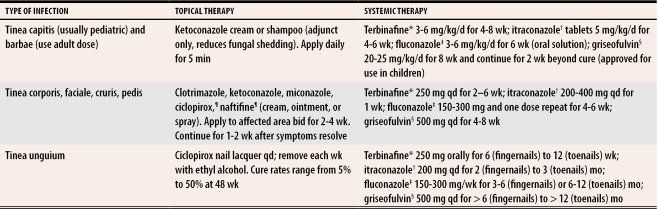
Dermatophyte infections can be treated with topical or systemic antifungal agents (Table 2). Topical therapy is seldom effective for treatment of onychomycosis and tinea capitis,3 but can be used for treatment of tinea corporis, faciale, cruris, and pedis. Aluminum chloride hexahydrate (20% to 25%) is a useful adjunct to topical antifungal therapy in chronic macerated interdigital tinea pedis.1 Keratolytic agents (eg, salicylic acid and lactic acid) can be useful in reducing hyperkeratosis in the moccasin type of tinea pedis. In this case, the patient was treated with oral fluconazole with no adverse effects, and had complete resolution of the dermatophytosis on his hand (tinea manus) within 2 months.
Table 2.
Topical and systemic antifungal treatment in management of dermatophytosis
bid—twice daily, qd—each day.
*Patients taking terbinafine should be followed up for hepatotoxicity; avoid in active or chronic liver disease.
†Itraconazole use has been associated with cardiac complications and neuropathy. Hypoglycemia might occur with sulfonylureas; rhabdomyolysis might occur with 3 hydroxy-3-methylglutaryl coenzyme A reductase inhibitors; absorption is impaired with administration of antacids. Use with caution in hepatic insufficiency.
‡Fluconazole might cause hepatic complications, especially with underlying AIDS and malignancy. Hydrochlorothiazide diuretics might increase fluconazole plasma levels.
§Griseofulvin could decrease warfarin activity, serum salicylate concentrations, and the effectiveness of oral contraceptives and cyclosporine. If therapy is prolonged, monitor complete blood count and renal and hepatic function. Photosensitivity is a possibility.
¶Apply to moist web spaces.
Diagnosis of dermatophytosis should be confirmed before initiating systemic therapy. Systemic antifungal medications can interact with other therapeutic agents,3-5 so consultation with a pharmacist or review of prescribing information is recommended if patients are taking more than one medication. Monitoring complete blood count with differential, creatinine, and liver function tests is advised. Patients should be told to discontinue their medication at the first sign of acute hepatitis symptoms, such as nausea, malaise, or fatigue.4 Consultation with a dermatologist might be beneficial for chronic disease and for consideration of systemic therapy.
Biography
Dr Turchin is a resident in the Department of Family Medicine at the University of Calgary in Alberta. Dr Barankin is a resident in the Department of Dermatology, Dr Alanen is a Dermatopathologist and Clinical Lecturer in the Departments of Dermatology and Pathology, and Dr Saxinger is an Assistant Professor in the Division of Infectious Diseases, all in the Faculty of Medicine at the University of Alberta in Edmonton.
References
- 1.Martin AG, Kobayashi GS. Superficial fungal infection: dermatophytosis, tinea nigra, piedra. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, et al, editors. Fitzpatrick’s dermatology in general medicine. 5th ed. New York, NY: McGraw-Hill; 1999. pp. 2337–2357. [Google Scholar]
- 2.Vander Straten MR, Hossain MA, Ghannoum MA. Cutaneous infections dermatophytosis, onychomycosis, and tinea versicolor. Infect Dis Clin North Am. 2003;17(1):87–112. doi: 10.1016/s0891-5520(02)00065-x. [DOI] [PubMed] [Google Scholar]
- 3.Gupta AK, Sauder DN, Shear NH. Antifungal agents: an overview. Part II. J Am Acad Dermatol. 1994;30(6):911–933. doi: 10.1016/s0190-9622(94)70112-1. [DOI] [PubMed] [Google Scholar]
- 4.Smith EB. The treatment of dermatophytosis: safety considerations. J Am Acad Dermatol. 2000;43(5 Suppl):113–119. doi: 10.1067/mjd.2000.110379. [DOI] [PubMed] [Google Scholar]
- 5.Gupta AK, Sauder DN, Shear NH. Antifungal agents: an overview. Part I. J Am Acad Dermatol. 1994;30(5 Pt 1):677–698. [PubMed] [Google Scholar]