Abstract
OBJECTIVE
To describe errors Canadian family physicians found in their practices and reported to study investigators. To compare errors reported by Canadian family physicians with those reported by physicians in five other countries.
DESIGN
Analytical study of reports of errors. The Linnaeus Collaboration was formed to study medical errors in primary care. General practitioners in six countries, including a new Canadian family practice research network (Nortren), anonymously reported errors in their practices between June and December 2001. An evolving taxonomy was used to describe the types of errors reported.
SETTING
Practices in Canada, Australia, England, the Netherlands, New Zealand, and the United States.
PARTICIPANTS
Family physicians in the six countries.
MAIN OUTCOME MEASURES
Types of errors reported. Differences in errors reported in different countries.
RESULTS
In Canada, 15 family doctors reported 95 errors. In the other five countries, 64 doctors reported 413 errors. Although the absence of a denominator made it impossible to calculate rates of errors, Canadian doctors and doctors from the other countries reported similar proportions of errors arising from health system dysfunction and gaps in knowledge or skills. All countries reported similar proportions of laboratory and prescribing errors. Canadian doctors reported harm to patients from 39.3% of errors; other countries reported harm from 29.3% of errors. Canadian physicians considered errors “very serious” in 5.8% of instances; other countries thought them very serious in 7.1% of instances. Hospital admissions and death were among the consequences of errors reported in other countries, but these consequences were not reported in Canada.
CONCLUSION
Serious errors occur in family practice and affect patients in similar ways in Canada and other countries. Validated studies that analyze errors and record error rates are needed to better understand ways of improving patient safety in family practice.
Abstract
OBJECTIF
Décrire les erreurs que les médecins de famille (MF) canadiens ont identifiées dans leur pratique et qu’ils ont rapportées aux auteurs de l’étude. Comparer ces erreurs à celles rapportées par les médecins de cinq autres pays.
TYPE D’ÉTUDE
Étude analytique des rapports d’erreurs. Le projet Linnaeus Collaboration a été créé pour étudier les erreurs médicales dans les soins primaires. Les omnipraticiens de six pays, incluant ceux d’un nouveau réseau de recherche sur la médecine familiale au Canada (Nortren), ont rapporté de façon anonyme leurs erreurs de pratique entre juin et décembre 2001. Une taxonomie en développement a été utilisée pour décrire les types d’erreurs.
CONTEXTE
Milieux de pratique du Canada, de l’Australie, de l’Angleterre, de la Hollande, de la Nouvelle-Zélande et des États-Unis.
PARTICIPANTS
Médecins de famille de ces six pays.
PRINCIPAUX PARAMÈTRES MESURÉS
Types d’erreurs rapportées. Différences entre les erreurs rapportées par differents pays.
RÉSULTATS
Au Canada, 15 MF ont rapporté 95 erreurs. Dans les cinq autres pays, 64 médecins on rapporté 413 erreurs. Même si l’absence de dénominateur commun ne permet pas de calculer les taux d’erreurs, les médecins canadiens et ceux des autres pays ont rapporté une proportion semblable d’erreurs attribuables à un dysfonctionnement du système de santé et à des connaissances ou habilités insuffisantes. Les taux d’erreurs de laboratoire et de prescription étaient semblables dans tous les pays. Les médecins canadiens ont déclaré que 39,3% de leurs erreurs avaient causé préjudice aux patients, contre 29,3% dans les autres pays. Les médecins canadiens jugeaient les erreurs «très graves» dans 5,8% des cas; ceux des autres pays, dans 7,1% des cas. Parmi les conséquences rapportées dans les autres pays, il y avait des hospitalisations et des décès, ce qui n’était pas le cas au Canada.
CONCLUSION
Les erreurs graves qui surviennent en pratique familiale et les préjudices qu’elles causent aux patients sont semblables au Canada et dans les autres pays. Des études validées permettant d’analyser les erreurs et d’enregistrer leurs taux devront être entreprises pour connaître la façon de mieux assurer la sécurité des patients en pratique familiale.
EDITOR’S KEY POINTS.
“To err is human” and physicians are no different from other people in this respect. Despite their potential for harming patients, there is little information about medical errors in family practice.
The Linneas Collaboration was formed in 2001 to study medical errors in primary care. Family doctors from Canada and five other countries were asked to report errors they thought should not happen again.
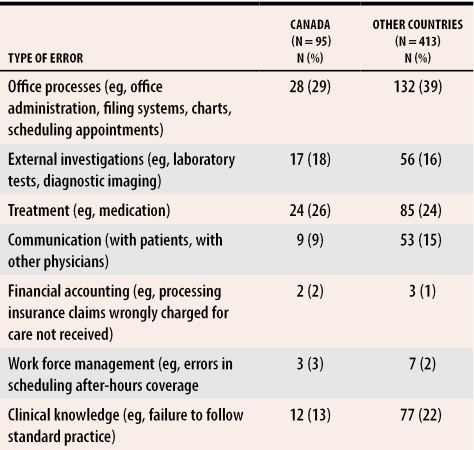
The three most common categories of errors reported in Canada were process errors (office administration, filing systems, chart problems), investigation errors, and treatment errors. Proportions of errors in Canada were similar to those in other countries. Most errors occurred in family physicians’ offices.
POINTS DE REPÈRE DU RÉDACTEUR.
«L’erreur est humaine» et les médecins ne font pas exception à cette règle. Malgré les préjudices que cela peut engendrer pour les patients, on possède peu d’information sur les erreurs médicales en pratique familiale.
Le projet Linneaus Collaboration a été créé en 2001 pour examiner les erreurs médicales dans les soins primaires. On a demandé à des médecins de famille du Canada et de cinq autres pays de rapporter les erreurs qui, selon eux, ne devraient jamais se reproduire.
Les trois catégories d’erreurs les plus fréquemment mentionnées au Canada étaient les erreurs méthodologiques (gestion du bureau, systèmes d’archivage, problèmes de dossiers), les erreurs d’investigation et les erreurs de traitement. Les proportions d’erreurs étaient les mêmes au Canada et dans les autres pays. La plupart des erreurs étaient survenues au cabinet des médecins de famille.
In 1999, the Institute of Medicine in the United States published their report To err is human describing the extent of medical error detected in US hospitals and institutions.1 Starfield subsequently published US hospital data that showed medical error was the third most common cause of death in the United States.2 Both these reports acknowledged the almost complete absence of data from community-based practices.
In early 2001, primary care researchers in Australia, Canada, England, the Netherlands, New Zealand, and the United States formed the Linnaeus Collaboration out of a perceived need to develop methods of measuring error in community-based primary care practice.3 One member of the group (S.D.) had developed and carried out preliminary evaluations of a taxonomy for classifying the types of errors reported in community practice.
The Linnaeus Collaboration aims to investigate ways primary care physicians could reduce threats to patient safety in family practice. Countries participating in the Linnaeus Collaboration have various organizational and policy frameworks. The collaboration was interested in how different countries’ delivery systems allow medical errors or protect patients from harm. In each participating country, most health care contacts occur in primary care, so this setting is important in understanding total patient risk. Australia, and more recently the United Kingdom, have conducted descriptive studies on medical errors in primary care.4,5,6,7 Results of these studies suggest that patient safety issues found in hospitals are unlikely to be the same as those found in primary care settings.
A major constraint on the study was that physicians reporting errors had to be completely anonymous. A test of anonymity was that, if an error report was legally demanded by a court action, there would be no possible way to trace it back to the reporting physician. A further constraint was the inability to determine a denominator from any participating practice. This constraint prevented calculation of error rates, limiting the study to simply describing errors committed. The only comparison possible between countries was the percentage of errors of a particular classification of error in each country.
Definition of error
The Linnaeus Collaboration chose to use a definition of medical error that made sense to participating doctors. This definition had been tested in a pilot study in 2000.
Errors are events in your practice that made you conclude, “That was a threat to patient well-being and should not have happened. I don’t want it to happen again.” Such an event affects or could affect the quality of the care you give your patients. Errors might be large or small, administrative or clinical, or actions taken or not taken. Errors might or might not have discernible effects. Errors in this study are anything you identify as something wrong, to be avoided in the future.
Participating physicians reported events that fell under this definition. The definition is not based on known adverse reactions to medical interventions, but rather on process breakdowns that increase risk of harm. Only the errors that family physicians recognized and reported during daily clinical practice in ambulatory care clinics, hospitals, patients’ homes, nursing homes, or other sites were included.
Participants
Study participants were drawn from the North Toronto Primary Care Research Network (Nortren), a network of 17 volunteers who are community based and hospital- and university-appointed family physicians. This was not a representative sample of Canadian family physicians, but a test group upon which the data-collection methods could be evaluated. For this study, six physicians were also drawn from rural Ontario practices. Their descriptions of errors would determine whether serious errors were occurring in rural practice and whether the errors could be reported using descriptive methods. In each of the other participating countries, convenience samples of family physicians were recruited.
To be eligible for the study, doctors had to be family physicians who were providing direct patient care for at least 20 hours weekly and who expected to be absent from clinical work for no more than 2 weeks during the data-collection period.
Data and processes
A standard study protocol was used in all countries. Reports from Canada were made on printouts of the electronic forms used in the other countries. They were filled in by hand and mailed to the Canadian data-collection centre at Sunnybrook and Women’s College Health Sciences Centre in Toronto, Ont. They were then copied and posted to the project coordinating office at the Robert Graham Center in Washington, DC. Electronic reports from the other five countries were sent from participating doctors’ computers to a secure server until investigators from each country and the international investigator could access and download them. Each investigator’s access was limited to data from his or her own country; the international investigator had access to all data.
Full anonymity was maintained for all participating doctors. There was no way to trace the source of any report. This level of anonymity prevented validation of reports and discussion of serious errors with individual doctors. The ethical review panel in Canada requested that, if a serious error were reported, a notice be sent to all participating physicians asking them to ensure that appropriate steps be taken to notify the patient and prevent repetition of the error.
Data collected included information about the error and, if appropriate, non-identifying demographic data about the patient affected by the error, including age, sex, ethnicity, and the reporting doctor’s level of familiarity with the patient. The reporting doctor was asked to describe the error and was prompted to record what happened, known consequences, and what he or she thought might be contributing factors and effective prevention strategies. The seriousness of resulting harm (if any) and the frequency of the type of error were included in the report. The protocol was assessed and approved in Canada by the University of Toronto’s Health Sciences Research Ethics Board with considerable difficulty because of issues related to the anonymity of reporting physicians.8
Analysis
The preliminary taxonomy for errors, developed from an earlier study, was used to classify reported errors.9 General categories for classifying errors included practice management, investigation, treatment, payment, and work force organization. In developing the taxonomy, up to four more precise classifications were created under these main headings for each report of a distinctly different phenomenon. Some errors did not fit into any of these classifications, but were directly related to gaps in health care providers’ knowledge or skills.
Descriptive statistics were calculated for reported site of occurrence; patients’ age, sex, and ethnicity; reported consequences to patients; and familiarity of reporting physicians with affected patients. The proportion of reports attributed to each category was calculated for Canada and for all the other countries combined. The study design allowed only descriptive statistics to be calculated from the reports from each country. No statistical comparison was possible between countries.
Error category
Fifteen Canadian family physicians contributed 95 of the 508 reports during the 7-month data-collection period. Three reports from Canada (3.6%) and three reports from other countries (0.9%) were not included in the error categorization because they reported unpreventable adverse events rather than errors. Table 1 shows the taxonomy to the first three levels comparing Canadian reports of errors with reports from the other five countries. Errors are described as a percentage of the total number of errors reported in each country.
Table 1.
Errors reported in Canada and five other countries
Error context
Canadian physicians reported errors at 67 sites; doctors in the other countries reported errors at 406 sites. Most often, only one site was identified (Canada 85.2% of reports; other countries 83.6% of reports), and that site was usually a family physician’s office (Canada 69.1% of reports; other countries 62.9% of reports). Ten reports from Canada and 44 from other countries involved errors starting in hospitals. Three reports from Canada and 19 reports from the other countries involved errors in nursing homes.
In most reports of errors, only a single patient was affected, but in six reports from Canada (7.4%) and 21 from other countries (6.1%), errors had a broader effect. In Canada, three errors were due to faulty laboratory processes, one to inadequate scheduling of after-hours coverage, one to receptionists’ systematic failure to deal appropriately with telephone calls from patients, and one to a doctor’s forgetting to give out patient information leaflets.
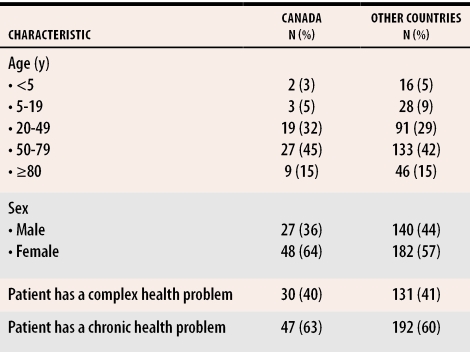
Demographic characteristics of affected patients are shown in Table 2. In most reports (73.3% from Canada and 59.7% from other countries) reporting physicians already knew the affected patients very or fairly well. In seven reports from Canada (9.3%) and 53 from other countries (16.3%), errors were reported after physicians’ first contacts with affected patients.
Table 2. Demographic characteristics of patients affected by medical errors.
Number of patients and percentage of patients in the sample affected by errors in Canada and other countries.
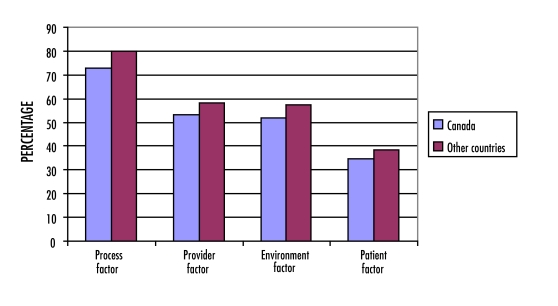
Regarding factors that might have contributed to errors, 132 different reasons were offered a total of 1491 times. In Figure 1, factors contributing to errors are broadly categorized as process factors, provider factors, environmental factors, and patient factors, and Canadian percentages are compared with percentages in the other countries.
Figure 1. Factors contributing to errors reported in Canada and the five other countries.
Percentage of error reports involving the contributing factor.
Consequences
When asked directly if patients were harmed by reported errors, Canadian doctors said yes in 39.3% of reports and physicians from the other countries said yes in 29.3% of reports. Harm was considered somewhat serious or very serious in nine reports from Canada (5.8%) and in 40 reports from other countries (7.1%). In 16 cases of errors reported in other countries (3.7%), patients had to be hospitalized, and in five cases (1.2%), patients died. No Canadian errors reported resulted in either hospitalization or death.
DISCUSSION
Despite very different primary care systems in the six countries, the general types of errors reported were similar. These results suggest that participating countries’ management practices (including management of medications) and administrative systems function less well than they should and that patients were harmed as a result. Even though Canada had the lowest use of computers in family practice of any of the participating countries, all countries experienced problems with information management and medication use. As Canada contemplates more widespread use of computers in health care, we need to design systems to avoid the problems reported by countries more advanced in computer use. We noted that Canadian reports focused more on the adverse effects of drugs and treatments rather than on actual errors.
Assessing risk
One idea that emerged from discussion of the results was the idea of assessing patients’ risk during office visits. Physicians should assess risk in three domains: risk due to physicians, risk due to systems, and risk due to patients themselves. Risk due to physicians would include how stressed, fatigued, or distracted they were at the time of visit. Risk due to systems would include how backed up, chaotic, or intrusive office systems were during the visit, including the effect of missing charts, missing test results, or other information not available during patients’ visits. Risk due to patients would include the number and severity of comorbid conditions, the number of drugs or treatments patients were receiving, and how cooperative patients were with physicians and caregivers. To avoid errors, physicians could mentally assess the risk of committing errors in the three domains and proceed with the appropriate degree of caution.
This study shows that it is possible to collect data on medical errors in family practice in Canada and other countries in a relatively short time. Although protecting anonymity prohibited validation of the accuracy and completeness of our data, participating physicians reported that they were confident their anonymity was protected and that the data-collection methods worked smoothly. Results of this study set the stage for a more methodologically sophisticated study that could produce rates of errors so that comparisons could be made between geographic regions of Canada as well as between Canada and other countries. The evolution of a taxonomy able to classify all of the more than 500 errors reported in this study is a positive step toward a taxonomy for measuring error in primary care.
Limitations
The study has several limitations. The requirement for complete anonymity prevented validation of the accuracy and completeness of data collection. The fact that errors in such a sensitive area were self-reported might reduce confidence in the quality of results. The lack of denominator data from each practice prevents calculation of rates of errors. Types of errors can be described, and the percentages of various classifications of errors can be compared among the six countries. This limits results to descriptive comparisons only, and caution is required when making international comparisons. The evolving taxonomy requires further development and validation before it can be relied upon to capture accurately all errors committed in family practice. Because no attempt was made to use a representative sample of physicians in Canada or in the other countries, results of this descriptive study cannot be applied generally.
Conclusion
Descriptions emerging from this study of medical errors in family practice suggest that errors committed in Canada are similar to errors committed in the other five participating countries. Further studies capable of exploring these issues in rigorous and valid ways that will both protect participating physicians from the threat of litigation and generate error rates must be carried out to determine how to improve patient safety in primary care.
Biography
Dr Rosser is Head of the Department of Family Medicine at Queen’s University in Kingston, Ont, and was Chair of the Department of Family and Community Medicine at the University of Toronto while the study was conducted. Dr Dovey is Director of Research in the Dunedin Department of Family Medicine at Dunedin University in New Zealand. Dr Bordman is a family physician affiliated with the Scarborough General Hospital in Toronto. Dr White is Chief of Family Medicine at the North York General Hospital. Mr Crighton works in the Primary Care Research Unit, and Dr Drummond was Research Director for the Community Program when this paper was written, at Sunnybrook and Women’s College Health Sciences Centre.
References
- 1.Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 2.Starfield B. Is US health care really the best in the world? JAMA. 2000;284(4):483–485. doi: 10.1001/jama.284.4.483. [DOI] [PubMed] [Google Scholar]
- 3.Pennisi E. Taxonomy. Linnaeus’s last stand? Science. 2001;291:2304–2307. doi: 10.1126/science.291.5512.2304. [DOI] [PubMed] [Google Scholar]
- 4.Bhasale AL, Miller GC, Reid SE, Britt HC. Analysing potential harm in Australian general practice: an incident-monitoring study. Med J Aust. 1998;169:73–76. doi: 10.5694/j.1326-5377.1998.tb140186.x. [DOI] [PubMed] [Google Scholar]
- 5.Britt H, Miller GC, Steven ID, Howarth GC, Nicholson PA, Bhasale AL, et al. Collecting data on potentially harmful events: a method for monitoring incidents in general practice. Fam Pract. 1997;14:101–106. doi: 10.1093/fampra/14.2.101. [DOI] [PubMed] [Google Scholar]
- 6.Steven ID, Malpass A, Moller J, Runciman WB, Helps SC. Towards safer drug use in general practice. J Qual Clin Pract. 1999;1:47–50. doi: 10.1046/j.1440-1762.1999.00302.x. [DOI] [PubMed] [Google Scholar]
- 7.Rubin G, George A, Chinn DJ, Richardson C. Errors in general practice: development of an error classification and pilot study of a method of detecting errors. Qual Saf Health Care. 2003;12:443–447. doi: 10.1136/qhc.12.6.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall K, Rosser W, Makeham M, Dovey S, Esmail A, Kuzel A. What is research? An international study reveals a fundamental normative issue. J Clin Ethics. In press.
- 9.Dovey SM, Meyers DS, Phillips RL, Jr, Green LA, Fryer GE, Galliher JM, et al. A preliminary taxonomy of medical errors in famiily practice. Qual Saf Health Care. 2002;11:233–238. doi: 10.1136/qhc.11.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]