Abstract
OBJECTIVE
Personal digital assistants (PDAs) are popular with physicians: in 2003, 33% of Canadian doctors reported using them in their practices. We do not know, however, whether using a PDA changes the behaviour of practising physicians. We studied the effectiveness of a PDA software application to help family physicians diagnose angina among patients with chest pain.
DESIGN
Prospective randomized controlled pilot trial using a cluster design.
SETTING
Primary care practices in the Toronto area.
PARTICIPANTS
Eighteen family physicians belonging to the North Toronto Primary Care Research Network (Nortren) or recruited from a local hospital.
INTERVENTIONS
We randomized physicians to receive a Palm PDA (which included the angina diagnosis software) or to continue conventional care. Physicians prospectively recorded the process of care for patients aged 30 to 75 presenting with suspected angina, over 7 months.
MAIN OUTCOME MEASURES
Did the process of care for patients with suspected angina improve when their physicians had PDAs and software? The primary outcomes we looked at were frequency of cardiac stress test orders for suspected angina, and the appropriateness of referral for cardiac stress testing at presentation and for nuclear cardiology testing after cardiac stress testing. Secondary outcome was referrals to cardiologists.
RESULTS
The software led to more overall use of cardiac stress testing (81% vs 50%). The absolute increase was 31% (P =.007, 95% confidence interval [CI] 8% to 58%). There was a trend toward more appropriate use of stress testing (48.6% with the PDA vs 28.6% control), an increase of 20% (P =.284, 95% CI -11.54% to 51.4%). There was also a trend toward more appropriate use of nuclear cardiology following cardiac stress testing (63.0% vs 45.5%), an absolute increase of 17.5% (P =.400, 95% CI -13.9% to 48.9%). Referrals to cardiologists did not increase (38.2% with the PDA vs 40.9%, P =.869).
CONCLUSION
A PDA-based software application can lead to improved care for patients with suspected angina seen in family practices; this finding requires confirmation in a larger study.
Abstract
OBJECTIF
Les assistants numériques personnels (ANP) sont de plus en plus utilisés par les médecins: en 2003, 33% des médecins canadiens déclaraient s’en servir dans leur pratique. On ignore toutefois si cela modifie leur façon de faire. Les auteurs ont voulu vérifier l’efficacité d’un logiciel ANP aider le médecin de famille à diagnostiquer l’angine en présence de douleurs thoraciques.
TYPE D’ÉTUDE
Essai randomisé prospectif pilote selon un mode en grappes.
CONTEXTE
Établissements de soins primaires du grand Toronto.
PARTICIPANTS
Dix-huit médecins de famille appartenant au North Toronto Primary Care Research Network (Nortren) ou recrutés dans un hôpital local.
INTERVENTIONS
Les médecins ont été assignés au hasard à recevoir un ANP Palm (incluant le logiciel de diagnostic pour l’angine) ou à poursuivre leur pratique habituelle. Ils ont ensuite noté de façon prospective et pendant 7 mois leur façon de traiter les patients de 30 à 75 ans soupçonnés d’angine.
PRINCIPALES QUESTIONS À L’ÉTUDE
La possession du logiciel a-t-elle amélioré la façon de traiter les patients soupçonnés d’angine? Les paramètres principaux étaient la fréquence de prescription des épreuves d’effort en cas d’angine possible et l’à-propos des prescriptions d’épreuves d’effort lors des premières manifestations et des demandes d’examens nucléaires cardiaques à la suite des épreuves d’effort. Secondairement, on a mesuré les demandes de consultation en cardiologie.
RÉSULTATS
L’utilisation du logiciel a entraîné une augmentation globale de l’utilisation des tests d’effort (81% vs 50%). En valeur absolue, il s’agit d’une augmentation de 31% (P =.007, intervalle de confiance [IC] à 95%, 8% à 58%). Il y avait une tendance à utiliser les épreuves d’effort de façon plus appropriée (48,6% avec l’ANP vs 28,6% chez les témoins), une augmentation de 20% (P =.284, IC à 95% -11,54% à 51,4%). On notait aussi une tendance à un usage plus approprié des tests cardiaques nucléaires à la suite des tests d’effort (63,0% vs 45,5%), une augmentation absolue de 17,5% (P =.400, IC à 95% -13,9 à 48,9%). Les demandes de consultation en cardiologie n’ont pas augmenté (38,2% avec l’ANP vs 40,9%, P =.869).
CONCLUSION
L’utilisation par le médecin de famille d’un logiciel ANP peut améliorer le traitement des patients soupçonnés d’angine; ces observations devront être confirmées par une étude plus large.
EDITOR’S KEY POINTS.
This pilot study is the first randomized controlled trial comparing referral for testing for angina with family doctors’ use of a personal digital assistant (PDA) and software to calculate risk.
Users of PDAs referred patients for cardiac testing more often than control subjects did (81% versus 50%). There were trends toward more appropriate referrals for stress tests and nuclear cardiology among PDA users.
POINTS DE REPÈRE DU RÉDACTEUR.
Cette étude pilote est le premier essai randomisé qui évalue de quelle façon l’utilisation par le médecin de famille d’un assistant numérique personnel (ANP) et d’un logiciel de calcul de risque modifie la prescription d’épreuves pour l’angine.
Ceux qui utilisaient les ANP ont demandé des épreuves cardiaques plus souvent que les témoins (81% versus 50%). Ils avaient aussi tendance à prescrire des tests d’effort et des examens nucléaires cardiaques plus appropriés.
Hand-held computers are increasingly being used in health care: a recent Canadian survey found that 33% of physicians used personal digital assistants (PDAs) in their practices.1 No randomized controlled trial (RCT), however, has yet reported whether using a hand-held computer changes the behaviour of practising physicians. We report the results of the first pilot RCT on this subject to our knowledge.
We used a recent guideline on diagnosis and management of angina2 as the basis for a PDA software application. This application assesses patients’ risk of angina, using the Diamond-Forrester risk-stratification model,3 and suggests appropriate diagnostic management. Further management suggestions are derived using test results, such as the Duke prognostic score4 for electrocardiographic exercise stress testing.
The study’s aim was to explore whether this diagnostic software would improve care for suspected angina. Primary outcomes were:
frequency of ordering cardiac stress tests for diagnosis of suspected angina and
appropriateness of cardiac stress testing at presentation, and of nuclear cardiology after cardiac stress testing.
METHOD
We defined appropriate cardiac stress testing as referral for testing when there was an intermediate or high probability of angina, and no referral when there was a low probability of angina.2,3 Appropriate referral for nuclear cardiology was referral after a cardiac stress test indicated intermediate prognostic risk using the Duke score.2,4 Secondary outcomes included referrals to cardiologists.
We recruited 18 family physicians practising in Toronto, Ont. Eleven were members of the North Toronto Primary Care Research Network (Nortren), and seven were from a local hospital’s department of family medicine. Written informed consent was obtained from all participants. Participants were allocated randomly to study groups using a simple block design. Nine physicians received Palm OS-based hand-held computers loaded with the angina software, and nine were instructed to continue to manage patients presenting with chest pain in their normal manner. Physicians randomized to the PDA group received a brief introduction to the technology and a short manual on use of the angina software (the manual is posted at http://dfcm19.med.utoronto.ca/research/nortren/angina_manual.htm).
Eligibility criteria for patient enrolment were being between 30 and 75 years old and presenting at the office to see their family physicians with symptoms judged by the physicians to be possible new-onset angina. Physicians recorded the identities of all such patients prospectively over 7 months, from mid-November 2001 to mid-June 2002; monthly reminders were sent to all physicians to maximize patient recruitment and to minimize recall bias. The medical records of patients identified by their family physicians were audited at the end of the recording period.
Ethics approval for the study was received from the North York General Hospital’s Research Ethics Board.
Results were analyzed using SAS software (version 8.2). Nominal variables were compared using the chi-square test (or Fisher’s exact test when appropriate), and accounted for clustering. All reported P values are two tailed.
RESULTS
Both groups of physicians were similar in terms of personal and professional characteristics. One physician recruited to the control arm of the study withdrew, and was excluded from the analysis. Patients’ risk factors for cardiovascular disease were also found to be similar. Of the 76 patients enrolled over 7 months, 65 were eligible for inclusion in the analysis.
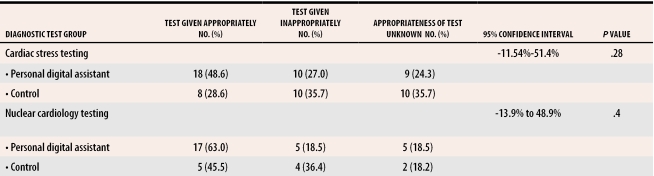
Fourteen of the 28 patients in the control arm (50%) and 30 of the 37 patients in the PDA arm (81%) were referred for cardiac stress tests (P =.007), an absolute difference of 31% (95% CI 8% to 58%). We also found a trend toward more appropriate referrals for cardiac stress tests among physicians using PDAs (Table 1), with an absolute increase of 20% (P =.284, 95% CI -11.54% to 51.4%).
Table 1.
Appropriate diagnostic tests
We did not find a calculated Duke prognostic risk score in any of the electrocardiographic exercise stress test reports in charts. Using the data available in the reports, a Duke score could be calculated for 31 of the 38 cardiac stress tests done (82%); six tests were ordered but not done. Referral for nuclear cardiology after cardiac stress testing was appropriate for 45.5% of the patients in the control arm and 63% of the patients in the PDA arm (Table 1), an absolute increase of 17.5% (P =.400, 95% CI -13.9% to 48.9%).
Referrals to cardiologists did not differ between the two groups. We could determine whether a referral was made for 56 patients (86%); referral rates were 41% in the control group, and 38% in the PDA group (P =.869). A referral was more likely to have been made if the final diagnosis was angina (likelihood ratio for referral 15.455, 95% CI 2.124 to 112.431); in other words, family physicians appeared to refer appropriately.
DISCUSSION
Guidelines recommend cardiac stress testing as the initial investigation for most cases of suspected angina.2,5,6 Previous studies of angina management in primary care found that only 34% and 6.4% of patients were referred for this test.7,8 A systematic review of personal computer-based diagnostic decision aids reported that these were unlikely to change practice, as only one in five trials was positive.9 We found a statistically significant increase in referrals for exercise stress tests with the PDA guideline. As well, results indicate a trend toward more appropriate referrals for cardiac stress testing, when appropriateness could be estimated. There was also a trend toward more appropriate referrals for nuclear cardiology testing.
Weaknesses of this study included the small physician sample size, the fact that many of the physicians belonged to a research network, and the fact that all physicians were located in the Toronto area. This will limit the findings’ generalizability. We are planning a larger trial in a variety of geographic locations, which will improve the external validity of the results.
In conclusion, results of this pilot trial indicate that providing family physicians with an interactive guideline on PDAs can improve care for patients presenting with suspected angina, particularly in relation to referral for exercise stress testing.
A full version of this article is available at http://individual.utoronto.ca/mgreiver/angina.pdf.
Acknowledgments
This study was funded by a Janus Research and Education Scholarship from the College of Family Physicians of Canada and a grant from the Bales Foundation at North York General Hospital. The project was awarded the North American Primary Care Research Group’s 2001 Pfizer Investigator-In-Practice Prize.
We thank Linda Deng, Shari Gruman, and Elfrieda Heiden for their help in this study. We also express our gratitude to the physicians who participated: Harvey Blankenstein, Risa Bordman, Branimir Brcic, Debra Butt, Paul Caulford, Kenneth Jaslkolka, Steve Kahane, Sonia Kurtz, Joanne Laine-Gossin, Naznin Lalani, Randall Lee, Ann Li, D’Arcy Little, Noel Rosen, Jim Ruderman, Brian Silver, Beverley Smith, and David Wheler.
Biographies
Dr Greiver is an Assistant Professor in the Department of Family and Community Medicine at the University of Toronto and is a Research Co-ordinator at North York General Hospital in Ontario.
Dr Drummond is an Associate Professor in the Departments of Family Medicine and Community Health Sciences at the University of Calgary in Alberta.
Dr White is an Associate Professor in the Department of Family and Community Medicine at the University of Toronto and is Chief of the Department of Family and Community Medicine at North York General Hospital.
Mr Weshler is an MBA candidate in the Michael G. Degroot School of Business at McMaster University in Hamilton, Ont.
Dr Moineddin is a biostatistician in the Department of Family and Community Medicine at the University of Toronto.
Footnotes
Competing interests: None declared
References
- 1.Canadian Medical Association. 2003 CMA Physician Resource Questionnaire. Ottawa, Ont: Canadian Medical Association; 2003. [cited 2005 January 18]. Available at: http://www.cmaj.ca/cgi/data/169/7/701/DC1/1. [Google Scholar]
- 2.Gibbons RJ, Chatterjee K, Daley J, Douglas JS, Fihn SD, Gardin JM, et al. ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on management of patients with chronic stable angina). Circulation. 1999;99:2829–2848. doi: 10.1161/01.cir.99.21.2829. [DOI] [PubMed] [Google Scholar]
- 3.Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979;300:1350–1358. doi: 10.1056/NEJM197906143002402. [DOI] [PubMed] [Google Scholar]
- 4.Mark DB, Shaw L, Harrell FE, Hlatky MA, Lee KL, Bengtson JR, et al. Prognostic value of a treadmill exercise score in outpatients with suspected coronary artery disease. N Engl J Med. 1991;325:849–853. doi: 10.1056/NEJM199109193251204. [DOI] [PubMed] [Google Scholar]
- 5.Scottish Intercollegiate Guideline Network. Management of stable angina: a national clinical guideline. April 2001. Edinburgh, Scotland: Royal College of Physicians; [cited 2003 December 30]. Available at: http://www.sign.ac.uk/pdf/sign51.pdf. [Google Scholar]
- 6.Institute for Clinical Systems Improvement. Stable coronary artery disease. November 2003. Bloomington, Minn: Institute for Clinical Systems Improvement; [cited 2005 January 18]. Available at: http://www.icsi.org/knowledge/detail.asp?.catID=29&itemID=192. [Google Scholar]
- 7.Gill D, Mayou R, Dawes M, Mant D. Presentation, management and course of angina and suspected angina in primary care. J Psychosom Res. 1999;46:349–358. doi: 10.1016/s0022-3999(98)00102-0. [DOI] [PubMed] [Google Scholar]
- 8.Eccles M, McColl E, Steen N, Rousseau N, Grimshaw J, Parkin D. Effect of computerised evidence based guidelines on management of asthma and angina in adults in primary care: cluster randomised controlled trial. BMJ. 2002;325:941–948. doi: 10.1136/bmj.325.7370.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes. JAMA. 1998;280:1339–1346. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]