Can you identify this condition?
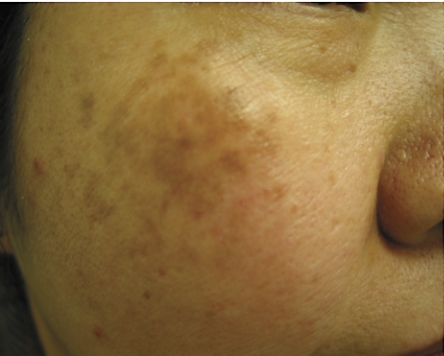
A 38-year-old Asian woman presented with brown macules on both cheeks that she had had for several years. She began to notice the macules with the birth of her first child 6 years ago. She currently takes no medications, and her medical history was unremarkable.
The most likely diagnosis is:
Melasma
Lentigines
Postinflammatory hypermelanotic macules
Addison’s disease
Discoid lupus erythematosus
1. Melasma
Melasma, the Greek term for “a brown spot,” is a common hypermelanosis that typically occurs on sun-exposed areas of the face. Chloasma, the Greek term for “a green spot,” is a synonymous term that describes melasma during pregnancy (the “mask of pregnancy”). Melasma is characterized by symmetrically distributed macules with irregular borders ranging from light brown to dark brown to gray-brown.1 Pigmentation can be guttate or confettilike, linear, or confluent. Three common clinically distinct distributions include centrofacial (ie, forehead, nose, chin, upper lip), malar (ie, cheeks), and mandibular (ie, lower jaw).2-4 Pigmentation usually evolves slowly over weeks or months.
Melasma is not exclusive to any sex, age, or race. Melasma is rarely reported before puberty and is more common in women of reproductive age. Men comprise only 10% of the affected population.5 The condition is more prevalent among people with darker complexions (skin types IV to VI), including those of Hispanic, Middle Eastern, Asian, and Indian descent who live in areas of the world that receive high-intensity ultraviolet radiation.2
Investigations
Wood’s light (wavelength 340 to 400 nm) examination is useful in diagnosis and can help classify melasma into epidermal, dermal, and mixed types.4 Epidermal pigmentation is the most common type of melasma; pigmentation is accentuated under Wood’s light examination. Dermal pigmentation disappears under Wood’s light examination, and mixed types show areas with increased (epidermal), absent, or decreased (dermal) pigmentation.4 On dark-brown skin (skin type VI), Wood’s light is unable to locate hyperpigmentation; hence, the classification is indeterminate.3,4 These classifications are valuable indicators of prognosis. While epidermal pigmentation tends to respond better and faster to hypopigmenting agents (eg, hydroquinone), dermal pigmentation responds variably and often unsatisfactorily.3
Histologic studies indicate an increase in the number and activity of melanocytes, which enhance formation and transfer of melanosomes (pigment-containing granules) to the layers of the epidermis and dermis.4 Epidermal and dermal classification of melasma is determined by the location of melanocyte deposition. Although epidermal melanin is usually found in keratinocytes of basal and suprabasal areas, dermal melanin is found in macrophages of the superficial and deep layers.3 Mixed types present with the histologic characteristics of both epidermal and dermal types. Melanocyte-stimulating hormone does not have a role in melasma.6
While most cases are idiopathic, melasma can also be associated with genetics, exposure to ultraviolet radiation, pregnancy, oral contraceptives, hormone replacement therapies, mild endocrine disturbances (ie, ovarian or thyroid dysfunction), cosmetics, antiepileptic medications, and other photosensitizing drugs.2,6,7 Melasma is commonly reported in women using estrogen-progesterone oral contraceptives, hormone replacement therapy for prevention of osteoporosis, and in men using an estrogen derivative for treatment of prostate cancer.3 An endocrinologic study of women with melasma who had never been pregnant nor used oral contraceptives reported increased serum concentrations of luteinizing hormone, which could implicate mild ovarian dysfunction as a possible cause of idiopathic cases of melasma.6 Sun exposure tends to be the most important causative factor in all patients, so management options for melasma must always include protection from the sun and avoidance of excessive exposure to sunlight.
Treatment
Melasma is a cosmetic problem that is difficult to treat. Current treatments include hypopigmenting compounds, exfoliative agents, and lasers.3,7,8 Hypopigmenting agents, such as hydroquinone (2% to 5%), tretinoin cream (0.1%), azelaic acid (15% to 20%), kojic acid (2% to 4%), mild cortisone, and combinations of these agents are effective at attenuating the formation, decreasing the stability, and promoting the destruction of melanocytes.3,8 Exfoliative agents, such as alpha-hydroxy and glycolic acid, used in superficial chemical peels are more commonly used to treat light-complexioned people. Complications of hypopigmentation are occasionally seen on darker complexions.7
In recent years, attempts have been made to use pigmented lesion dye, Q-switched Nd:YAG, Q-switched ruby, and argon and carbon dioxide lasers; however, studies using these instruments have achieved only moderate success.3,7,8 Lasers are typically used after hypopigmenting and exfoliative therapeutic options have been considered. In some cases, melasma spontaneously disappears several months postpartum or after cessation of oral contraceptives. If appropriate, discontinuation of causative medications is indicated. Treatment and prevention of melasma should always include avoiding excessive exposure to the sun and daily application of broad-spectrum sunscreens, preferably those containing opaque physical blockers, such as titanium dioxide and zinc oxide. Consultation with a dermatologist for therapeutic options is recommended.
Biographies
Ms Ting is a medical student at the University of Calgary in Alberta.
Dr Barankin is a dermatology resident at the University of Alberta in Edmonton.
References
- 1.Sams MW, Lynch PJ. Principles and practice of dermatology. 2nd ed. New York, NY: Churchill Livingstone Inc; 1996. [Google Scholar]
- 2.Pandya AG, Guevara IL. Disorders of hyperpigmentation. Dermatol Clin. 2000;18:91–98. doi: 10.1016/s0733-8635(05)70150-9. [DOI] [PubMed] [Google Scholar]
- 3.Perez-Bernal A, Munoz-Perez MA, Camacho F. Management of facial hyperpigmentation. Am J Clin Dermatol. 2000;1:261–268. doi: 10.2165/00128071-200001050-00001. [DOI] [PubMed] [Google Scholar]
- 4.Sanchez NP, Pathak MA, Sato S, Fitzpatrick TB, Sanchez JL, Mihm MC., Jr Melasma: a clinical, light microscopic, ultrastructural, and immunofluorescence study. J Am Acad Dermatol. 1981;4:698–710. doi: 10.1016/s0190-9622(81)70071-9. [DOI] [PubMed] [Google Scholar]
- 5.Vazquez M, Maldonado H, Benmaman C, Sanchez JL. Melasma in men. A clinical and histologic study. Int J Dermatol. 1988;27:25–27. doi: 10.1111/j.1365-4362.1988.tb02329.x. [DOI] [PubMed] [Google Scholar]
- 6.Perez M, Sanchez JL, Aguilo F. Endocrinologic profile of patients with idiopathic melasma. J Invest Dermatol. 1983;81:543–545. doi: 10.1111/1523-1747.ep12522896. [DOI] [PubMed] [Google Scholar]
- 7.Grimes PE. Melasma. Etiologic and therapeutic considerations. Arch Dermatol. 1995;131:1453–1457. doi: 10.1001/archderm.131.12.1453. [DOI] [PubMed] [Google Scholar]
- 8.Piamphongsant T. Treatment of melasma: a review with personal experience. Int J Dermatol. 1998;37:897–903. doi: 10.1046/j.1365-4362.1998.00585.x. [DOI] [PubMed] [Google Scholar]