Abstract
OBJECTIVE
One distressing health problem facing breast cancer patients is breast cancer-related lymphedema (BCRL). This incurable condition can occur many years after treatment is completed and often causes pain and disability and interferes with work and activities of daily living. Patients at risk of BCRL are those who have received radiation therapy or axillary node dissection; higher incidence is reported among patients who have had both radiation and dissection. Our objective was to explore New Brunswick women’s experiences of BCRL and its treatment.
DESIGN
A focus group and 15 individual in-depth interviews.
SETTING
Province of New Brunswick.
PARTICIPANTS
A diverse sample of 22 women with BCRL was obtained using age, location, time after breast cancer diagnosis, and onset of BCRL symptoms as selection criteria.
METHOD
The focus group discussion guided development of a semistructured interview guide that was used for 15 individual interviews exploring women’s experiences with BCRL.
MAIN FINDINGS
Four themes emerged from the interviews. First, participants thought they were poorly informed about the possibility of developing BCRL. Eleven women reported receiving very little or no information about BCRL. Second, triggers and symptoms varied. Participants used words such as numb, heavy, tingling, aching, seeping fluid, hard, tight, limited mobility, and burning to describe symptoms. They reported a variety of both aggravating and alleviating factors for their symptoms. Some actions, such as applying heat, were thought to both exacerbate and reduce symptoms. Third, in New Brunswick, access to treatment is poor, compression garments are costly, and accessing physiotherapists is difficult. Last, the effect of BCRL on daily life is profound: 12 of the 15 women reported that it interfered with work and day-to-day activities.
CONCLUSION
Participants were unaware of the risk factors and treatment options for BCRL. Family physicians should discuss BCRL with their breast cancer patients routinely. They should be vigilant for the possible onset of BCRL and, if it is diagnosed, should manage it aggressively to minimize the severe effect it has on the lives of breast cancer patients.
Abstract
OBJECTIF
Le lymphœdème lié au cancer du sein (LLCS) est une complication pénible à laquelle font face plusieurs patientes atteintes de cancer du sein. Cette condition incurable, qui peut survenir plusieurs années après la fin du traitement, cause de la douleur et de l’incapacité, en plus de gêner le travail et les activités de la vie quotidienne. Les patientes à risque de LLCS sont celles qui ont eu de la radiothérapie ou un curage des ganglions axillaires. Dans cette étude, on a voulu savoir comment les femmes du Nouveau-Brunswick vivent ce problème et comment on le traite.
TYPE D’ÉTUDE
Un groupe de discussion et 15 entrevues en profondeur.
CONTEXTE
Le Nouveau-Brunswick.
PARTICIPANTES
Un échantillon diversifié de 22 femmes souffrant de LLCS a été formé en utilisant comme critères de sélection l’âge, le lieu de résidence, le temps écoulé depuis le diagnostic de cancer du sein et le moment d’apparition des symptômes de LLCS.
MÉTHODE
Les rencontres du groupe de discussion ont permis de développer un guide d’entrevue semi-structurée qui a ensuite été utilisé dans 15 entrevues individuelles explorant la façon dont les femmes vivent le LLCS.
PRINCIPALES OBSERVATIONS
Les entrevues ont permis d’identifier quatre thèmes principaux: premièrement, les participantes se disaient mal informées de la possibilité de développer le LLCS. Onze d’entre elles déclaraient avoir reçu très peu ou aucune information à ce sujet. Deuxièmement, les facteurs déclencheurs et les symptômes variaient. Les termes utilisés pour décrire les symptômes étaient engourdissement, lourdeur, picotement, douleur sourde, suintement, durcissement, constriction, mobilité réduite et brûlure. Divers facteurs susceptibles d’aggraver ou de soulager les symptômes étaient mentionnés. On croyait que certaines mesures, comme l’application de chaleur, pouvaient à la fois exacerber et soulager les symptômes. Troisièmement, au Nouveau-Brunswick, le traitement n’est pas facilement disponible, les vêtements compressifs coûtent cher et les physiothérapeutes sont difficiles d’accès. Enfin, le LLCS a des effets profonds sur le vécu quotidien: 12 des 15 femmes disaient que cela les gênait au travail et dans les activités de la vie quotidienne.
CONCLUSION
Les participantes ignoraient les facteurs de risque du LLCS et ne connaissaient pas les possibilités de traitement. Le médecin de famille devrait prendre l’habitude de discuter du LLCS avec ses patientes souffrant de cancer du sein. Il devrait être attentif à l’apparition éventuelle du LLCS et, le cas échéant, intervenir de façon agressive pour minimiser ses graves conséquences sur la vie des patientes.
EDITOR’S KEY POINTS.
Breast cancer-related lymphedema (BCRL) is an under-recognized complication of breast cancer treatment that can occur years after initial care. It strongly affects the lives of the women who have it. This qualitative study from New Brunswick explored their experiences.
A major finding was the lack of information provided to the women, either by their initial treating surgeons or oncologists or by their family physicians.
Triggers for the condition appeared to be activities that were unusual in their daily lives and activities associated with hot weather. The women described symptoms of swelling, tingling, heaviness, tightness, reduced mobility, and burning.
POINTS DE REPÈRE DU RÉDACTEUR.
Le lymphœdème lié au cancer du sein (LLCS) est une complication trop peu connue du traitement du cancer du sein, qui peut survenir plusieurs années après l’intervention initiale et qui a des effets profonds sur la vie des femmes. Dans cette étude menée au Nouveau-Brunswick, on a voulu connaître l’expérience des femmes confrontées à ce problème.
Une observation importante est que les femmes reçoivent peu d’information à ce sujet, que ce soit du chirurgien initial, de l’oncologiste ou du médecin de famille.
Les activités inhabituelles ou effectuées par temps chaud semblaient être des facteurs déclencheurs. Les symptômes mentionnés étaient des gonflements, picotements, lourdeurs, constrictions, brûlures et perte de mobilité.
One of the most distressing of the long-term health problems facing breast cancer patients is breast cancer-related lymphedema (BCRL). This incurable condition can occur many years after breast cancer treatment has been completed.1 The condition arises from an accumulation of fluid in the arm or trunk due to an impaired lymphatic system; it can result from axillary lymph node dissection, radiation therapy, or advanced cancer.2 Breast cancer-related lymphedema is a serious condition that often causes pain and disability and can predispose patients to life-threatening complications, such as cellulitis and, very rarely, lymphangiosarcoma.1,3,4
Although BCRL has emerged as an area for research fairly recently, many aspects of this condition remain poorly understood. There is little research on breast cancer patients’ experiences of BCRL, on what information they receive from physicians about BCRL, and on their access to treatment.3,5,6,7
Sentinel node dissection, a technique that replaces axillary lymph node dissection, might decrease risk of BCRL in the future, but this procedure is not yet accepted as the standard of care.3Given that an estimated 21100 Canadian women will be newly diagnosed with breast cancer this year and that survival rates have increased while mortality rates have decreased, it seems likely that an increasing number of breast cancer survivors will suffer from BCRL. In 2001, Petrek et al3 very conservatively estimated that 200000 American women would have BCRL, using an incidence rate of only 10%.
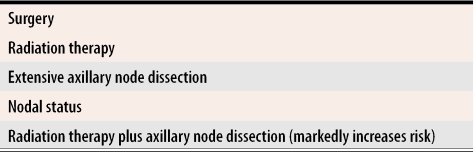
Estimating incidence has been difficult because the etiology of BCRL is complex, and we are not aware of all the factors that contribute to its development. Patients at risk of BCRL are those who have received radiation therapy or axillary node dissection; higher incidence is reported among patients who have received both radiation and dissection, particularly if either treatment was extensive8,9 (Table 19). Some additional risk factors for BCRL include poor nutritional status, obesity, delayed wound closure, and postoperative infections.1,3,8,10
Table 1.
Treatment-related risk factors for breast cancer-related lymphadenopathy
Data from Kwan et al.9
Diagnosis
Diagnostic criteria for BCRL vary, as do recommended treatments and their efficacy.1,3,11 The lack of consensus on the diagnostic criteria and appearance of BCRL, even 30 years after cancer treatment, have led to an estimated incidence of 6% to 70%.4A review of the literature suggests that prevalence rates of 15% to 30% are reasonable.9 When diagnosing new cases of BCRL, it is important to rule out axillary vein thrombosis and cancer recurrence.
Treatment
Treatment of BCRL is controversial, and various treatment options have been proposed including manual and sequential pneumatic lymph drainage, compression garments, prescribed exercises, ultrasound therapy, and more recently, use of coumarin, intra-arterial injections of autologous lymphocytes, liposuction, selenium, and laser treatment.1,4Most currently used treatments, however, involve some form of lymphatic drainage. Outcomes of this treatment vary greatly.1,15,16,17 More specifically, treatment involves physical decongestion therapy, use of compression garments, and exercise under the supervision of trained physiotherapists.14
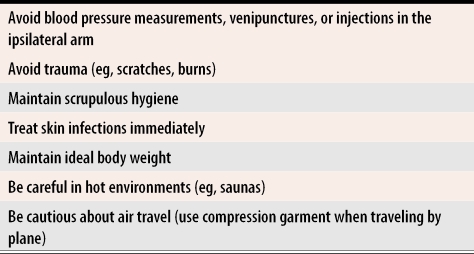
Some evidence indicates that instructing patients on precautions for limb and skin care following surgery and radiation therapy reduces the incidence and complications associated with BCRL.5Early identification of risk of developing BCRL and preventive counseling and monitoring are vital to prevent development of BCRL19 (Table 21). Risk-reduction guidelines advocating scrupulous hygiene and avoidance of trauma to the affected limb have been developed, but they do not appear to have been communicated to breast cancer patients, suggesting that family physicians can play a greater role in patient education. Symptoms can emerge long after completion of acute treatment when patients no longer have contact with the specialists who treated them.20 A recent literature review yielded only one study that examined knowledge of lymphedema in a primary care setting. The authors found that primary health care professionals were not aware of important issues associated with prevention and management of this condition.21
Table 2. Advice for patients at risk of breast cancer-related lymphedema.
Recommendations are based largely on anecdotal evidence, but are a representative summary of clinical practice guidelines.
Data from Harris et al.1
While complications of BCRL are important to consider, psychosocial effects can disrupt women’s lives even more.19,22,23 Women in rural areas might be more seriously affected because there are fewer support services outside cities. Consequently, rural family physicians might have to play a more active role in BCRL management than urban physicians.24
Our research team became interested in BCRL concerns and management possibilities as a result of our Cancer Follow-up Care Study of patients’ satisfaction with follow-up cancer care.25 Many breast cancer patients in that study indicated that they wore compression garments and described their daily struggle with lymphedema. Our study was designed to document, from the perspective of BCRL patients, the effect of BCRL on New Brunswick women’s lives in terms of physical and psychosocial health and patients’ perspectives on availability of information and access to treatment. Although our findings are specific to New Brunswick, we believe they would be similar to findings in other largely rural areas with limited medical resources across the country.
Setting
New Brunswick, a largely rural province with limited economic resources, has a population of approximately 750000 people. There are three urban areas with populations ranging from 50000 to 100000. Provision of health care services varies, depending on hospital region. Within the largest of seven hospital regions in the province, there is only one regional hospital. This hospital provides most health services, but because it does not provide therapeutic radiation, patients sometimes have to travel long distances for both acute and follow-up cancer care. An estimated 500 New Brunswick women were diagnosed with breast cancer in 2003.26
Data collection
Following ethics approval by the Research Ethics Committee of the Dr Everett Chalmers Regional Hospital, we recruited 22 women to take part in the study. Participants were recruited from across the province with the aid of breast cancer support groups, advertisements in local newspapers, and using the snowball technique. Thirty-one women indicated interest during the 2 months the study was advertised. Inclusion criteria were age 19 years or older, active breast cancer treatment completed, ability to provide informed consent, residence in New Brunswick, and a clinical history of BCRL. Women with recurrent disease were excluded.
A focus group with seven participants was facilitated by two of the authors to gather ideas for developing a guide for the in-depth interviews. Focus groups are a useful exploratory method of research when little is known about the topic at hand, particularly from the perspective of those affected by a particular phenomenon.27 The discussion lasted about 2 hours. Participants were asked to respond to open-ended questions about breast cancer diagnosis and treatment, BCRL symptoms and treatment, and sources of information on BCRL.
Fifteen individual interviews were then conducted using the guide along with specific probes developed from the focus group discussion to verify or elaborate upon the initial response. For instance, participants were asked whether they had received BCRL treatment, and then asked about specific treatment programs if they had not been mentioned. Saturation was reached by the 12th interview, but three more interviews were conducted to ensure a diverse sample had been interviewed.
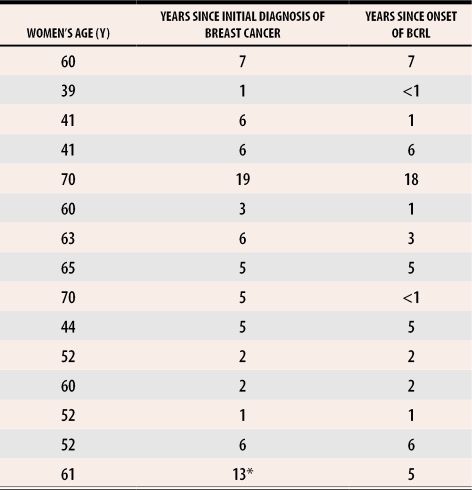
A diverse sample was obtained using age, location (urban or rural), time after breast cancer diagnosis, and time elapsed since onset of BCRL symptoms as selection criteria (Table 3). Ten of 15 interviewees were wearing visible compression garments during the interviews, one indicated she was no longer experiencing symptoms, and another said she was waiting to see her family physician about BCRL symptoms. The remaining three interviewees reported symptoms consistent with BCRL, but stated that they were not currently being treated for it.
Table 3. Age of women, years since diagnosis of breast cancer, and years since onset of breast cancer-related lymphedema (BCRL).
Eight women were from urban areas; seven were from rural regions.
*Participant had breast cancer twice; surveyed 6 years after second occurrence.
Analysis
Audiotapes were transcribed verbatim and analyzed using established guidelines for qualitative research.28,29 Transcripts were read in their entirety by all three authors independently. Important statements (ie, those that were repeated) were highlighted and put into thematic categories or clusters. Team discussions verified the emergence of these thematic categories, as well as agreement on their similarities and applicability. The categories then provided the basis for a coding structure within NVivo, a qualitative data analysis software package.
Similarities and differences were sought both within the transcripts and between them, which further developed the thematic categories. This level of coding resulted in more than 100 themes, which were then collapsed into the four major, substantive themes explored in this paper. To validate our analysis, we shared our findings with members of a breast cancer support group that included several women who suffered from BCRL. They confirmed that our analysis was consistent with their experiences.
FINDINGS
Four substantive themes captured women’s experiences with BCRL: lack of information, triggers and symptoms, access to treatment, and effect on daily life.
Lack of information
Most participants did not recall receiving information on BCRL, either during cancer treatment or afterward. Eleven of 15 participants reported receiving “very little” or no information about BCRL, and two reported receiving information at the time of treatment. Two other women received information after requesting it, and one woman, who experienced swelling before completion of chemotherapy, believed this was why she received information about BCRL. One of the women who requested information was a health care professional. She had been informed during acute cancer treatment that there was little chance of developing BCRL. Her surgeon stated that she need not worry about taking precautions.
When I asked the surgeon about the lymph dissection, the surgeon said, “Oh well, years ago we used to try to take every lymph gland we could because we thought we were making things better. Now we just take a sample” and I said, “Well, what about blood pressure and punctures and all that?” and he said “Well, they’ve done studies on that and it doesn’t matter.”
When asked about family physicians’ knowledge of BCRL, one participant responded, “She didn’t even talk to me about it when I had my surgery; … even my surgeon, or the oncology department [staff] that you go to once a year, they did not mention it. Really, nobody ever mentioned it to me, ever.” Eight other participants said that their family physicians knew very little about BCRL and that they did not discuss BCRL during follow-up care. The lack of information was also revealed as participants pointed to individual triggers for BCRL, rather than citing breast cancer treatment as the cause of their symptoms.
Triggers and symptoms
A few participants pointed to possible triggers to onset of BCRL. One woman said she had been at a driving range and thought the repetitive activity combined with heat resulted in onset of BCRL symptoms. Another noted that her arm started to swell upon her return from a camping trip. A third described how extreme physical exertion appeared to trigger onset of lymphedema. She said, “The doors were all frozen in the car … and I climbed in the backseat and got one door open, but the other door was frozen shut and I pounded it with my arm … it hurt at the time and it was shortly after that, I noticed the swelling.”
Participants described a variety of sensations and symptoms, and used such words as numb, heavy, tingling, aching, seeping fluid, hard, tight, limited mobility, and burning. One woman said:
Sometimes I can’t even see my knuckles, and [my arm] gets tight and painful up here (under the arm). It’s like an arthritis pain, you know; … when my arm is really swollen, my fingers will cramp and I have to take my fingers, rub them and try to get the cramp out.
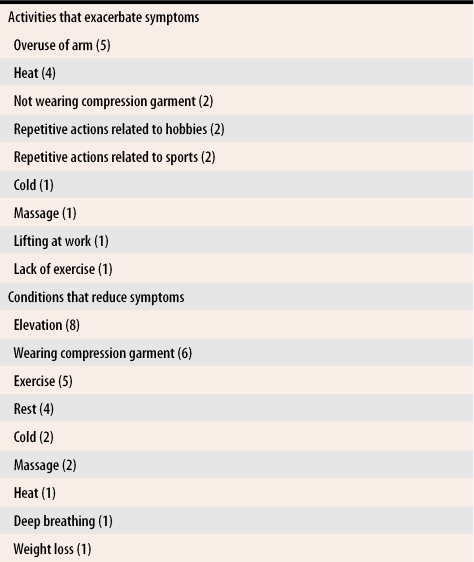
The women reported a variety of both aggravating and alleviating factors for BCRL symptoms (Table 4). Some conditions and actions, such as heat, were thought to both exacerbate and reduce BCRL symptoms in different women and sometimes at different times in the same women. Both cold and massage therapy were thought to both exacerbate and reduce symptoms.
Table 4. Reported exacerbating and alleviating factors for breast cancer-related lymphedema.
Numbers in parentheses indicate number of participants reporting the factor.
One participant who spoke of the importance of donning her compression sleeve first thing in the morning during the heat of the summer also said of a different source of heat: “I guess I’m not supposed to do this, but what I do sometimes, is put those heated bags under my arm, not really hot, but just warm, and it sort of makes my arm feel better while the bag is on there.” Participants reported a variety of symptoms and perceived triggers. Symptoms were exacerbated by poor access to treatment and the costs associated with managing the condition.
Access to treatment
In addition to difficulties associated with accessing physiotherapists was the barrier to proper management related to the cost of compression garments. One participant explained, “We have a private health plan, and it won’t cover my sleeve. It will cover my prosthesis, but I’ve called and they just won’t cover my sleeve. I said I had a prescription, I have to get measured, I have a prescription but that didn’t matter.” Six women reported using their sleeves beyond optimal elasticity because they had no health plans or had plans that limited coverage to a specific number of sleeves each year. Two participants reported further financial difficulties because they had to buy more than one compression garment in order to find one that was suitable.
Effect on daily life
The women in our study reported that BCRL had severe and disabling effects on their everyday lives. Twelve of 15 said it altered their ability to enjoy day-to-day activities, long-practised hobbies and sports, and leisure activities. They reported difficulty with finding clothing that would accommodate their swollen arms, needing support for the affected arm when driving long distances, and being unable to do household chores. One woman said:
I iron 15 minutes, and then I rest before I iron again. I’ll finish my [laundry] basket in the day, but it may take me all day to do it. Things around Christmas time, making cookies-you can stir, but not a lot … vacuuming, the same thing; you can vacuum one room but I can’t vacuum my whole house at the same time.
Another participant described disabling aspects of BCRL and their effect on everyday life:
I can’t really make a bed, like to throw the sheet or the blanket, I have to get my husband to help me. … I can’t vacuum. … I just do the lighter things around the house; my husband does the other things. … I can’t hold any sort of weight. … I don’t know what would be the limit of pounds that I could take but I would say 10. I don’t carry the groceries, if I do, I’ll carry the bread, the light things. I don’t grocery shop. It’s hard to reach sometimes, and although I do the exercises, I just find it hard to extend my arm.
DISCUSSION
Breast cancer incidence has not changed markedly in recent decades, yet survival rates have increased. This has led to a corresponding increase in the number of women with BCRL.30,31,32 The long-term effect of BCRL on women’s lives can be severe. Although BCRL might be avoidable, it is not curable; while effective management might not always be possible, it does depend on timely diagnosis.
Our study indicated a lack of awareness of BCRL among breast cancer patients and health care professionals, which supports the findings of two earlier studies on patient information and knowledge of BCRL in primary care.20,21 Many of the women in this study had had cancer diagnosed 5 or 6 years before; one participant had been diagnosed 19 years before. They probably received information on possible development of BCRL early in their treatment but were likely inundated with medical information at the time. It is both possible and even likely that their recollection of having received information was hampered by a combination of extreme distress, information overload, and the physical strain of breast cancer treatment. The findings of this study suggest that surgeons, oncologists, and family physicians need to explicitly, clearly, and most importantly, repeatedly inform patients about the possibility of developing BCRL. Onset of BCRL can occur months to years after acute treatment has been completed, and women with BCRL will likely present first to their family physicians rather than to the specialists who treated them originally. A variety of symptoms, such as numbness, tingling, aching, seepage, and burning, should alert physicians to the possibility of early presentation of BCRL.20
Family physicians should measure women’s arm circumference before and after treatment in order to make timely diagnoses of BCRL, although the optimal frequency of such measurements is unknown.1 Measurements are taken at metacarpal-phalangeal joints, wrists, 10 cm distal to the lateral epicondyles, and 15 cm proximal to the lateral epicondyles.1,33 Asking patients about physical changes, such as pain, tightness, and swelling, and their effect on activities of daily living might help detect early BCRL.1Patients should watch for such symptoms themselves also.
Family physicians also play an important role in recognition of arm cellulitis, which might be the initial presentation of BCRL or might exacerbate it. Prompt recognition of BCRL could minimize acute morbidity (prevent hospitalization) and decrease the likelihood of permanent sequelae. Since BCRL might be the first presentation of a regional recurrence of breast cancer or axillary vein thrombosis, early recognition of symptoms could prompt urgent investigations.
Although there is debate over the usefulness or harm of exercise for women with BCRL, some research has indicated that exercise is beneficial for BCRL patients.34,35,36 Family physicians might want to encourage their patients to explore participation in a supervised exercise program, such as dragon boat racing.34,35,36
Since participants described difficulty finding appropriate compression garments, it is important that physicians refer patients to physiotherapists knowledgeable about BCRL for measurement and fitting of sleeves and gauntlets. Vendors of garments might lack the expertise of well-trained physiotherapists, and poorly fitting compression garments can exacerbate BCRL symptoms.3 Also, BCRL-trained physiotherapists can instruct women in self-care, including self-massage, which has been deemed helpful for some.37
There are only three physiotherapists in the entire province of New Brunswick who are trained in BCRL treatment, including proper measurement techniques for compression garments. These physiotherapists are located in two urban centres, which limits rural women’s access to them. Some women have to drive hours to receive appropriate BCRL-specific physiotherapy, which is particularly hazardous in the winter. It is apparent from this study that resources for appropriate BCRL treatment are inadequate for the needs of New Brunswick women. This situation is, however, not unique to this province. Prince Edward Island also lacks a lymphedema treatment centre, which puts the onus on family physicians to educate women regarding the possibility of developing BCRL, and to ensure early diagnosis of the condition.
Family physicians have, therefore, an important role in BCRL education of informing patients how to minimize complications in BCRL, such as keeping scrupulously clean and avoiding trauma.38 The actions that alleviated participants’ symptoms in our study are supported by the literature.4 Physicians might want to use the information in Table 4 for patient education. Table 2 summarizes some clinical practice guidelines.1 If patients live in areas where access to physiotherapists is difficult, physicians might want to increase their efforts at patient education.
Psychosocial effects of BCRL
Along with the trauma associated with a diagnosis of breast cancer and subsequent surgery and ancillary treatments, women with BCRL are further confronted with the psychosocial effects of BCRL. Our study has documented the severity of these effects on their daily lives. They affect women’s ability to engage in ordinary activities, including both paid and unpaid labour, household chores, sports, and leisure activities, all of which can seriously reduce their quality of life. Physicians should be aware of these psychosocial effects because even minimal symptoms can severely affect women’s lives.9 Family physicians are in a position to support and counsel their patients and might be able to reduce risk of the complications associated with BCRL and minimize disruption of daily living.
Limitations
For reasons of confidentiality, we did not seek to verify the diagnosis or severity of BCRL with participants’ physicians, although there is no reason to think that the women in the study did not suffer from BCRL. We acknowledge there might have been a self-selection bias because participants who had experienced difficulties might have been more likely to come forward. We believe this does not take away from the issues discussed.
Conclusion
Although additional research on BCRL is needed, family physicians are in a position to improve the care of women who have it. They should strive to provide more patient education and increase awareness of BCRL symptoms. They should also try to ensure that BCRL patients are referred to physiotherapists for rehabilitation and treatment and are provided with supportive counseling, if necessary. Resources for proper management of BCRL in New Brunswick are inadequate to serve the needs of breast cancer survivors. Our findings suggest that further research into primary care physicians’ knowledge of BCRL is warranted.
Acknowledgments
We thank the Canadian Breast Cancer Foundation (Atlantic Division) for their generous funding of this project. Sections of this paper were presented to the first Annual Canadian Lymphedema Conference in Montreal on May 28 to 31, 2003.
Biography
Dr Thomas-MacLean is an Assistant Professor in the Department of Sociology at the University of Saskatchewan in Saskatoon. Drs Tatemichi and Miedema work in the Dalhousie Family Medicine Teaching Unit at the Dr Everett Chalmers Regional Hospital in Fredericton, NB.
Footnotes
Competing interests: None declared
References
- 1.Steering Committee for Clinical Practice Guidelines for the Care and Treatment of Breast Cancer. Harris SR, Hugi MR, Olivotto IA, Levine M. Clinical practice guidelines for the care and treatment of breast cancer: II. Lymphedema. CMAJ. 2001;164(2):191–199. [PMC free article] [PubMed] [Google Scholar]
- 2.Smith RA. Introduction: American Cancer Society workshop on breast cancer treatment-related lymphedema. Cancer. 1998;83(12 Suppl):2775. [PubMed] [Google Scholar]
- 3.Petrek JA, Pressman PI, Smith RA. Lymphedema: current issues in research and management. CA Cancer J Clin. 2000;50(5):292–307. doi: 10.3322/canjclin.50.5.292. [DOI] [PubMed] [Google Scholar]
- 4.Marcks P. Lymphedema. Pathogenesis, prevention and treatment. Cancer Pract. 1997;5(1):32–38. [PubMed] [Google Scholar]
- 5.Glanz K, Lerman C. Psychosocial impact of breast cancer: a critical review. Ann Behav Med. 1992;14:202–212. [Google Scholar]
- 6.Ferrans CE. Quality of life through the eyes of survivors of breast cancer. Oncol Nurs Forum. 1994;21(10):1645–1651. [PubMed] [Google Scholar]
- 7.Thomas-MacLean R. Victims, patients, survivors, women: experiences of embodiment after breast cancer [PhD dissertation]. Fredericton, NB: University of New Brunswick; 2001. [Google Scholar]
- 8.Ververs JM, Roumen RM, Vingerhoets AJ, Vreugdenhil G, Coebergh JW, Crommelin MA, et al. Risk, severity and predictors of physical and psychological morbidity after axillary lymph node dissection for breast cancer. Eur J Cancer. 2001;37(8):991–999. doi: 10.1016/s0959-8049(01)00067-3. [DOI] [PubMed] [Google Scholar]
- 9.Kwan W, Jackson J, Weir LM, Dingee C, McGreggor G, Olivotto IA. Chronic arm morbidity after curative breast cancer treatment: prevalence and impact on quality of life. J Clin Oncol. 2002;20(20):4242–4248. doi: 10.1200/JCO.2002.09.018. [DOI] [PubMed] [Google Scholar]
- 10.Stanton AW, Svensson WE, Mellor RH, Peters AM, Levick JR, Mortimer PS. Differences in lymph drainage between swollen and non-swollen regions in arms with breast-cancer-related lymphedema. Clin Sci. 2001;101(2):131–140. [PubMed] [Google Scholar]
- 11.Kosir MA, Rymal C, Koppolu P, Hryniuk L, Darga L, Du W, et al. Surgical outcomes after breast cancer surgery: measuring acute lymphedema. J Surg Res. 2001;95(2):147–151. doi: 10.1006/jsre.2000.6021. [DOI] [PubMed] [Google Scholar]
- 12.Brennan MJ, DePompolo RW, Garden FH. Focused review: postmastectomy lymphedema. Arch Phys Med Rehabil. 1996;77(Suppl 3):74–80. doi: 10.1016/s0003-9993(96)90248-8. [DOI] [PubMed] [Google Scholar]
- 13.Brorson H. Liposuction gives complete reduction of chronic large arm lymphedema after breast cancer. Acta Oncol. 2000;39(3):407–420. doi: 10.1080/028418600750013195. [DOI] [PubMed] [Google Scholar]
- 14.Micke O, Bruns F, Mücke R, Schäfer U, Glatzel M, DeVries AF, et al. Selenium in the treatment of radiation-associated secondary lymphedema. Int J Radiat Oncol Biol Phys. 2003;56:40–49. doi: 10.1016/s0360-3016(02)04390-0. [DOI] [PubMed] [Google Scholar]
- 15.Brennan MJ, Miller LT. Overview of treatment options and review of the current role and use of compression garments, intermittent pumps, and exercise in the management of lymphedema. Cancer. 1998;83(12 Suppl):2821–2827. doi: 10.1002/(sici)1097-0142(19981215)83:12b+<2821::aid-cncr33>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 16.Chau N, Harris S. Practices and opinions of physiotherapists treating patients with breast cancer-related lymphedema. Physiotherapy Can. 2002;Summer:156–163. [Google Scholar]
- 17.Davis S. Lymphedema following breast cancer treatment. Radiol Technol. 1998;70(1):42–60. [PubMed] [Google Scholar]
- 18.Pain SJ, Purushotham AD. Lymphoedema following surgery for breast cancer. Br J Surg. 2000;87(9):1128–1141. doi: 10.1046/j.1365-2168.2000.01569.x. [DOI] [PubMed] [Google Scholar]
- 19.Passick SD, McDonald MV. Psychosocial aspects of upper extremity lymphedema in women treated for breast carcinoma. Cancer. 1998;83(12 Suppl):2817–2820. doi: 10.1002/(sici)1097-0142(19981215)83:12b+<2817::aid-cncr32>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 20.Bosompra K, Ashikaga T, O’Brien PJ, Nelson L, Skelly J. Swelling, numbness, pain, and their relationship to arm function among breast cancer survivors: a disablement process model perspective. Breast J. 2002;8(6):338–348. doi: 10.1046/j.1524-4741.2002.08603.x. [DOI] [PubMed] [Google Scholar]
- 21.Logan V, Barclay S, Caan W, McCabe J, Reid M. Knowledge of lymphoedema among primary health care teams: a questionnaire survey. Br J Gen Pract. 1996;46(411):607–608. [PMC free article] [PubMed] [Google Scholar]
- 22.Martin SM, Hanson C. The differences in body image between patients with and without lymphedema following breast cancer treatment. Occup Ther Ment Health. 2000;15(2):49–69. [Google Scholar]
- 23.Hare M. The lived experience of breast cancer-related lymphoedema. Nurs Stand. 2000;15(7):35–39. doi: 10.7748/ns.15.7.35.s59. [DOI] [PubMed] [Google Scholar]
- 24.Carter BJ. Women’s experiences of lymphedema. Oncol Nurs Forum. 1997;24(5):875–882. [PubMed] [Google Scholar]
- 25.Miedema B, MacDonald I, Tatemichi S. Cancer follow-up care. Patients’ perspectives. Can Fam Physician. 2003;49:890–895. [PMC free article] [PubMed] [Google Scholar]
- 26.Canadian Cancer Society. Canadian Cancer Statistics 2003. Toronto, Ont: Canadian Cancer Society; 2003. [cited 2004 November 1]. Available at: http://www.cancer.ca/ccs/internet/standard/0,3182,3172_14291__langId-en,00.html. [Google Scholar]
- 27.Morgan DL. Focus groups as qualitative research. 2nd ed. Newbury Park, Calif: Sage Publications Inc; 1997. [Google Scholar]
- 28.Munhall PL, Oiler-Boyd C. Nursing research: a qualitative perspective. New York, NY: National League of Nursing; 1993. [Google Scholar]
- 29.Van Manen M. Modalities of body experience in illness and health. Qual Health Res. 1998;8(1):7–24. [Google Scholar]
- 30.Wyatt G, Kurtz ME, Liken M. Breast cancer survivors: an exploration of quality of life issues. Cancer Nurs. 1993;16(6):440–448. [PubMed] [Google Scholar]
- 31.Pelusi J. The lived experience of surviving breast cancer. Oncol Nurs Forum. 1997;24(8):1343–1353. [PubMed] [Google Scholar]
- 32.Beaulac SM, McNair LA, Scott TE, LaMorte WW, Kavanah MT. Lymphedema and quality of life in survivors of early-stage breast cancer. Arch Surg. 2002;137(11):1253–1257. doi: 10.1001/archsurg.137.11.1253. [DOI] [PubMed] [Google Scholar]
- 33.Gerber LH. A review of measures of lymphedema. Cancer. 1998. pp. 2803–2804. [DOI] [PubMed]
- 34.Harris SR, Niesen-Vertommen SL. Challenging the myth of exercise-induced lymphedema following breast cancer: a series of case reports. J Surg Oncol. 2000;74(2):95–99. doi: 10.1002/1096-9098(200006)74:2<95::AID-JSO3>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 35.McKenzie DC. Abreast in a boat-a race against breast cancer. CMAJ. 1998;159(4):376–378. [PMC free article] [PubMed] [Google Scholar]
- 36.Mitchell T, Nielsen E. Living life to the limits: dragon boaters and breast cancer. Can Womens Studies. 2002;21(3):50–57. [Google Scholar]
- 37.Mirolo BR, Bunce IH, Chapman M, Olsen T, Eliadis P, Hennessy JM, et al. Psychosocial benefits of postmastectomy lymphedema therapy. Cancer Nurs. 1995;18(3):197–205. [PubMed] [Google Scholar]
- 38.Ridner SH. Breast cancer lymphedema: pathophysiology and risk reduction guidelines. Oncol Nurs Forum. 2002;29(9):1285–1293. doi: 10.1188/02.ONF.1285-1293. [DOI] [PubMed] [Google Scholar]