Ingrown toenails are a common problem that cause inconvenience and pain and limit daily functioning. Ingrown toenails usually occur on the big toe but might also affect the lesser toes. Ingrown toenails are most frequently seen in adolescents and young adults, but are a common problem for people of all ages.
Ingrown toenails can have three stages. During stage 1, there is erythema, trace edema, and pain at the lateral nail fold. During stage 2, there is increased pain, discharge from the edge of the nail, and signs of bacterial paronychia. In stage 3, hypertrophic granulation tissue forms on the lateral wall.1
Causes
The etiology of ingrown toenails includes direct trauma to the toe that forces the nail corners into the surrounding nail fold, genetic predisposition, improper nail trimming, poorly fitting shoes, and constant and repetitive microtrauma from normal day-to-day activities.
Treatment
Treatment options range from conservative measures to surgery. Conservative approaches, including soaking the foot in warm water, use of topical or oral antibiotics, teaching proper nail-trimming technique, and elevation of the corner of the nail, are often used for patients with mild stage 1 disease.1 Patients can be prescribed antibiotics that cover Gram-positive organisms; diabetic and immunocompromised patients might need broader-spectrum antibiotics. Family physicians can pack the nail border with antibiotic-impregnated gauze to relieve the pressure and to aid the nail to grow out from the surrounding skin.
Surgical options include resection of the affected nail border back to the nail matrix or avulsion of the entire nail plate. Either surgical option can be followed with a matrixectomy (removal of the nail matrix), which prevents future growth of the nail. Matrixectomy can be accomplished through chemical application, surgical dissection, or electrocautery.2-4
For most cases, conservative treatment in the form of basic foot care and advice about footwear is adequate to relieve symptoms. When the problem is recurrent, health professionals often view surgery as the best treatment to remove permanently either the whole nail or just the troublesome portion of the nail. Current conventional surgical treatments are unsatisfactory, however, because ingrown nails have a high recurrence rate.2,5,6 Local infection seems to be a predisposing factor for recurrence after surgery.6
In this paper, we describe a new method for treating stage 2 and 3 infected ingrown toenails. We believe that all the problems mentioned above (especially recurrence) could be solved by the longitudinal band removal method.
Main steps in the longitudinal band removal method
Disinfect the ingrown nail and surrounding area with an appropriate chemical antiseptic.
Apply local anesthesia with ethyl chloride spray (for some patients we injected a mixture of lidocaine and epinephrine 1:100 000).
Draw two parallel longitudinal lines on the centre of the nail with a surgical knife to use as a guide for the rest of the procedure (distance between lines should be 4 to 5 mm).
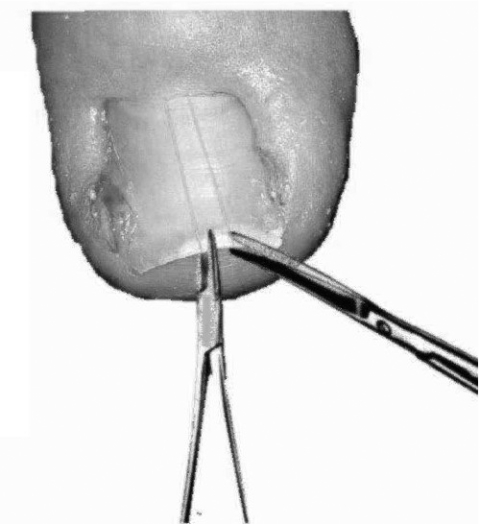
Using an appropriate suture holder and surgical scissors, remove the piece of nail between the two lines (we have used a surgical knife instead of scissors, but it seemed to cause more bleeding) (Figure 1).
Excise all the nail between two lines, but not the part under the skin at the base.
Drain the abscess with an appropriate lancet or surgical knife.
Dress the toenail with antiseptic dressing and local antibiotic cream. Keep the dressing on for 3 days. Replace it daily.
Figure 1. Longitudinal band removal.
After drawing two parallel lines on the nail, remove the nail between the lines using surgical scissors and a holder.
Postoperative care
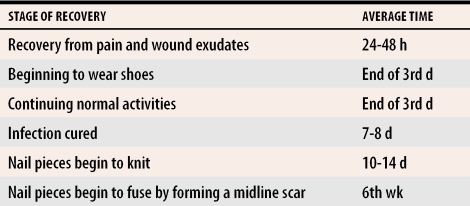
We ask patients not to wear shoes for 3 days and recommend systemic broad-spectrum antibiotics and nonsteroidal anti-inflamatory drugs for 10 days. We do not recommend any particular drugs. We evaluated the method in more than 50 patients for about 10 months. Responses to a survey of patients after treatment are shown in Table 1.
Table 1.
Recovery time after treatment
Only one patient had a recurrence of the condition during the follow-up period. Because that patient had a fungal infection, we now use this method only after appropriate treatment for fungal infections. We believe recurrence was related to the anomalous shape of the nail that resulted from the fungal infection.
Conclusion
We used the longitudinal band removal method for all cases of stage 2 and 3 ingrown nails after patients’ approval. Major advantages of the method revealed by our study were that the surgical procedure is easy to perform and does not require specialized equipment, that the operation can be performed despite concomitant infection, that the recurrence rate is low, and that postoperative pain and limitation of daily functioning is minimal.
Acknowledgments
We thank Dr Ogur’s uncle for this idea.
Biography
Drs Ogur, Tekbas, and Hasde are Public Health Specialists in the Department of Public Health at Gulhane Military Medical Academy in Ankara, Turkey.
References
- 1.Zuber TJ, Pfenninger JL. Management of ingrown toenails. Am Fam Physician. 1995;52(1):181–190. [PubMed] [Google Scholar]
- 2.Abby NS, Roni P, Amnon B, Yan P. Modified sleeve method treatment of ingrown toenail. Dermatol Surg. 2002;28(9):852–855. doi: 10.1046/j.1524-4725.2002.02040.x. [DOI] [PubMed] [Google Scholar]
- 3.Lin YC, Su HY. A surgical approach to ingrown nail: partial matricectomy using CO2 laser. Dermatol Surg. 2002;28(7):578–580. doi: 10.1046/j.1524-4725.2002.22028.x. [DOI] [PubMed] [Google Scholar]
- 4.Zuber TJ. Ingrown toenail removal. Am Fam Physician. 2002;65(12):2547. 2547-52, 2554. [PubMed] [Google Scholar]
- 5.Gerritsma-Bleeker CL, Klaase JM, Geelkerken RH, Hermans J, van Det RJ. Partial matrix excision or segmental phenolization for ingrowing toenails. Arch Surg. 2002;137(3):320–325. doi: 10.1001/archsurg.137.3.320. [DOI] [PubMed] [Google Scholar]
- 6.Rounding C, Hulm S. Surgical treatments for ingrowing toenails. Cochrane Database Syst Rev. 2000. CD001541. [DOI] [PubMed]