Abstract
OBJECTIVE
To identify patients with deep vein thrombosis (DVT) for whom in-hospital treatment should be considered.
QUALITY OF EVIDENCE
The literature was searched for studies on outpatient treatment of DVT. Seventeen studies were assessed: seven were randomized controlled trials (level I evidence), and 10 were non-randomized trials (level II evidence).
MAIN MESSAGE
Four criteria can be used to identify patients with DVT for whom outpatient treatment might not be appropriate: presence of massive DVT, presence of symptomatic pulmonary embolism, high risk of bleeding with anticoagulant therapy, and presence of comorbid conditions or other factors that warrant in-hospital care.
CONCLUSION
Four criteria can be used to identify patients with DVT for whom in-hospital treatment should be considered.
Abstract
OBJECTIF
Identifier les cas de thrombose veineuse profonde (TVP) pour lesquels un traitement à l’hôpital devrait être envisagé.
QUALITÉ DES PREUVES
On a fouillé la littérature à la recherche d’études sur le traitement extra-hospitalier de la TVP. Dix-sept études ont été évaluées, dont 7 essais randomisés (preuves de niveau I) et 10 essais non randomisés (preuves de niveau II).
PRINCIPAL MESSAGE
On peut déterminer les cas de TVP pour lesquels un traitement extra-hospitalier risque d’être inapproprié en utilisant quatre critères : la présence d’une TVP massive, une embolie pulmonaire symptomatique, un haut risque d’hémorragie en cas de traitement anticoagulant et la présence d’un état de comorbidité ou d’autres facteurs requérant des soins hospitaliers.
CONCLUSION
Quatre critères peuvent être utilisés pour déterminer les cas de TVP pour lesquels un traitement à l’hôpital devrait être envisagé.
EDITOR’S KEY POINTS.
For patients with newly diagnosed deep vein thrombosis (DVT), good evidence indicates that outpatient treatment is safe and effective using low-molecular-weight heparin and an oral anticoagulant until the international normalized ratio (INR) is in therapeutic range.
Hospitalization is recommended for patients with massive DVT, with symptomatic pulmonary embolism, at high risk of anticoagulant bleeding, or with major comorbidity.
POINTS DE REPÈRE DU RÉDACTEUR.
Des preuves de bonne qualité indiquent que les patients présentant une thrombose veineuse profonde (TVP) nouvellement diagnostiquéé peuvent être traités en externe de façon sûre et efficace avec une héparine de faible poids moléculaire et un anticoagulant oral jusqu’à ce que l’INR (International Normalized Ratio) soit dans la zone thérapeutique.
On recommande l’hospitalisation lorsqu’il y a une TVP massive, une embolie pulmonaire symptomatique, un risque élevé d’hémorragie liée à l’anti-coagulation ou un état de comorbidité sérieux.
Venous thromboembolism, which includes deep vein thrombosis (DVT) and pulmonary embolism, is the third most common vascular disease after coronary artery disease and stroke.1,2 An estimated 45 000 patients each year in Canada have DVT. Since the late 1990s, the standard of care for initial treatment of DVT has been at least 5 days’ treatment with a heparin preparation coadministered with an oral anticoagulant that, in North America, is usually warfarin. Heparin is given until warfarin attains a therapeutic effect, as defined by a target international normalized ratio (INR) of 2.0 to 3.0 for 2 consecutive days.3
The most common agent used for initiation of anticoagulant therapy is low-molecular-weight heparin (LMWH), which can be administered once or twice daily subcutaneously as a fixed dose, without laboratory monitoring.4,5 Because LMWH can be administered subcutaneously either by a visiting nurse or by patients themselves, in-hospital treatment is not required.
Well designed randomized trials have demonstrated that outpatient treatment of DVT with LMWH is comparable in efficacy and safety to in-hospital treatment with intravenous heparin and more economical than in-hospital treatment.6,7 Concerns remain, however, about the safety of treating all patients with DVT as outpatients. These concerns are, in part, due to the fact that outpatient DVT treatment was studied in closely monitored and structured clinical trials and that these studies excluded patients with more complicated disease, such as those with major comorbidity. With the increasing trend toward outpatient treatment of DVT, we still need to identify patients for whom outpatient treatment might be inadvisable.
The objective of this review is, therefore, to identify patients with DVT for whom in-hospital treatment should be considered. This article also describes the medications available for outpatient treatment of DVT.
Quality of evidence
MEDLINE (1994 to March 2004), HEALTHSTAR (1994 to March 2004), and the Cochrane Controlled Trials Register (1994 to March 2004) databases were searched for clinical trials (randomized and non-randomized) of outpatient treatment of DVT using the key words “deep vein thrombosis,” “venous thromboembolism,” “treatment,” “outpatient,” and “randomized controlled trial.” English and other-language articles were searched to avoid language-related selection bias, but only articles with English abstracts were reviewed.
The search strategy identified 17 trials in which patients with acute symptomatic DVT received treatment, either completely or in part, as outpatients.8-25 These studies were reviewed to find criteria for identifying patients for whom outpatient management might not be appropriate and for whom in-hospital treatment would be warranted. Seven randomized controlled trials (RCTs) providing level I evidence, and 10 non-randomized clinical trials providing level II evidence, were assessed.
When is outpatient treatment of DVT appropriate?
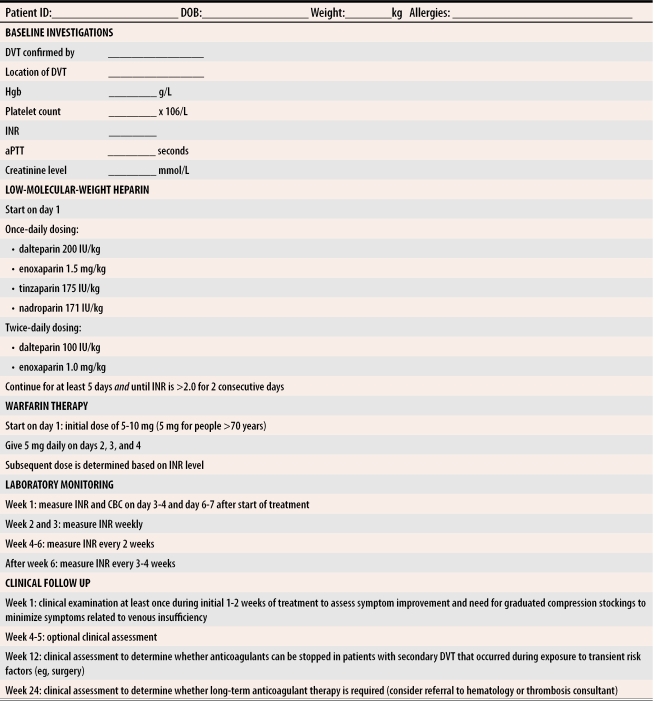
For patients presenting with DVT, level I and II evidence from well designed clinical trials indicates that outpatient treatment is effective and safe.8-25 Many hospitals and outpatient clinics currently have care paths to facilitate and standardize outpatient treatment (Figure 1). Outpatient treatment of DVT can be justified because, in general, the prognosis of such patients is good.
Figure 1.
Care path for outpatient treatment of deep vein thrombosis
aPTT—activated partial thromboplastin time, CBC—complete blood cell count, DOB—date of birth, DVT—deep vein thrombosis, Hgb—hemoglobin, ID—identification number, INR—international normalized ratio.
Among patients who receive appropriate anticoagulant therapy, 3% to 5% develop recurrent thromboembolism, and 3% to 5% develop major bleeding during the first 3 months of treatment.26 The case-fatality rate of recurrent venous thromboembolism is 5%; one in 400 patients who develop recurrent disease dies.27
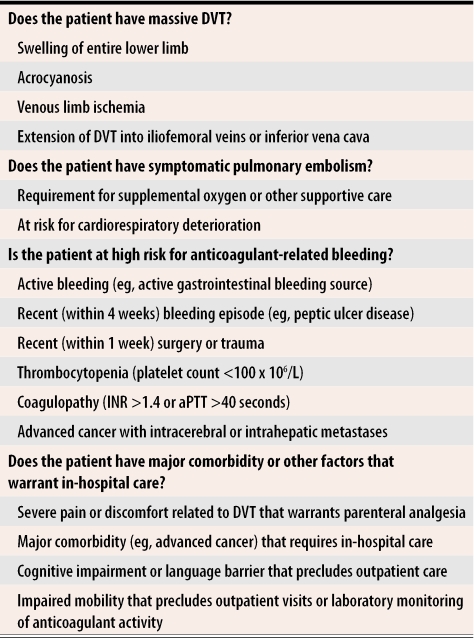
Four criteria can be used to identify patients for whom outpatient treatment might be inadvisable (Table 1). First, does the patient have massive DVT? Second, does the patient have objectively confirmed symptomatic pulmonary embolism? Third, is the patient at high risk of anticoagulant-related bleeding complications? Fourth, does the patient have major comorbidity or other factors that might warrant in-hospital care? If the answer to any of these questions is yes, in-hospital treatment should be considered.
Table 1. Criteria for assessing appropriateness of outpatient treatment of deep vein thrombosis.
Presence of one or more criteria suggests need for in-hospital care
aPTT—activated partial thromboplastin time, DVT—deep vein thrombosis, INR—international normalized ratio.
Does the patient have massive DVT?
About 5% of patients presenting with symptomatic lower-limb DVT have massive DVT that is characterized by severe pain, swelling of the entire limb, acrocyanosis, and in the most severe cases, limb ischemia. Seen on venous ultrasound, massive DVT involves the iliofemoral vein segment and can extend into the inferior vena cava. Hospitalization is recommended for these patients to administer parenteral analgesia and to consider alternative modes of treatment with thrombolytic agents, or extended-duration LWMH, or unfractionated heparin therapy for 10 to 14 days. One study assessed the prognosis of patients with iliofemoral DVT who received conventional anticoagulant therapy28 and showed that such patients were more than twice as likely to develop thrombosis than patients with less extensive DVT (11.2% vs 5.3%).
Does the patient have symptomatic pulmonary embolism?
About 10% of patients presenting with symptomatic lower-limb DVT also have symptomatic pulmonary embolism.26 For such patients, cardiorespiratory symptoms or the need for oxygen and other supportive therapy might preclude outpatient treatment. Some emerging evidence indicates that certain patients with symptomatic pulmonary embolism can be safely treated as outpatients, at least for part of their initial treatment.10,29 Patients in these studies were hemodynamically stable, had an oxygen saturation >95% while breathing room air, and did not require parenteral analgesia. Until there are more studies investigating outpatient treatment of pulmonary embolism in diverse clinical settings, however, patients with DVT and symptomatic pulmonary embolism should receive in-hospital anticoagulant therapy, at least for the initial 2 to 3 days’ treatment or until they have no ongoing requirement for supplemental oxygen or other supportive care.
Is the patient at high risk for anticoagulant-related bleeding?
Between 5% and 10% of patients with newly diagnosed DVT have conditions that preclude anticoagulation therapy or make administration of anticoagulants problematic. Certain conditions confer a high risk of bleeding complications after initiation of anticoagulant therapy.30-32 Patients with actively bleeding lesions, such as colonic neoplasms, will likely experience increased bleeding after anticoagulation commences. If the bleeding is severe or the lesion cannot be removed, placing an inferior vena cava filter (eg, Greenfield filter) could be warranted until anticoagulation can be safely administered.
Patients with recent (within 4 weeks) bleeding (eg, peptic ulcer disease) can receive anticoagulant therapy, but must be closely monitored to detect recurrent bleeding. Patients who have had recent surgery or trauma are also at increased risk of bleeding, particularly if they have extensive wound- or trauma-related injury that could begin to bleed again. Patients with thrombocytopenia (platelet count <100 x 106/L) or coagulopathy (INR >1.4; activated partial thromboplastin time [aPTT] >40 seconds) could be at increased risk of bleeding because of impaired hemostatic reserve. Finally, patients with advanced cancer who have intracerebral or intrahepatic metastases are at increased risk of bleeding because metastases to these sites tend to be highly vascular. Hospitalization is recommended for patients with these conditions because, if bleeding does occur, it can be detected and treated promptly.
Does the patient have major comorbidity or other factors that could warrant in-hospital care?
Most patients with DVT require simple supplementary measures that can be administered at home: rest, elevation of the symptomatic leg, and use of oral analgesics for relief of symptoms. Some ambulation should be encouraged because complete bed rest can promote thrombus progression. Symptoms typically take 7 to 14 days to resolve and usually do not start to improve until the third or fourth day of treatment. In-hospital care might be warranted, however, if patients have concomitant comorbidity (eg, advanced cancer) or if patients are unable to care for themselves.
Anticoagulation therapy for outpatient treatment of DVT
Low-molecular-weight heparin.
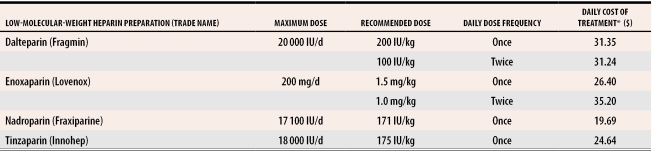
Level I evidence from RCTs has established the efficacy and safety of outpatient treatment of DVT with LMWH.8-10 Several LMWH preparations, administered once or twice daily by subcutaneous injection, are currently approved for the initial treatment of DVT (Table 2). Although there are no head-to-head RCTs comparing different LMWH preparations for treatment of DVT, the preparations likely have comparable antithrombotic efficacy and safety.33
Table 2.
Low-molecular-weight heparin for outpatient treatment of deep vein thrombosis
*Based on treatment with prefilled syringes for an 80-kg patient.
Low-molecular-weight heparin preparations have several advantages over unfractionated heparin for treatment of DVT. First, LMWH preparations have stable pharmacokinetics and, therefore, when administered using a weight-based dosing regimen, have stable and predictable antithrombotic activity. This eliminates the need for laboratory monitoring of the anticoagulant effect. Second, LMWH preparations can be administered in a once-daily injection, which might be easier for patients to administer themselves and might be less costly, particularly if visiting health care providers are required to administer the injections. Third, compared with unfractionated heparin, LMWH preparations are associated with a lower risk of heparin-induced thrombocytopenia, an immune-mediated condition that, paradoxically, is associated with increased risk of venous and arterial thromboembolism.3
Unfractionated heparin.
Outpatient treatment of DVT with twice-daily subcutaneous unfractionated heparin injections is efficacious and safe, based on level I evidence.34 Laboratory monitoring is required, however, with aPTT testing 6 hours after each daily morning dose. As with intravenous heparin therapy, subcutaneous heparin doses are adjusted to achieve a target aPTT of 1.5 to 2.0 times the control aPTT. One advantage of unfractionated heparin is that it is less expensive than LMWH.
Anti–factor Xa inhibitors.
Fondaparinux is a novel synthetically derived agent that exerts its antithrombotic activity by selective inhibition of factor Xa.35 Fondaparinux is currently available for prevention of DVT after orthopedic surgery and soon will be available for the initial treatment of DVT. Fondaparinux is administered in a once-daily, fixed-dose, subcutaneous injection of 7.5 mg (10 mg for patients >100 kg; 5 mg for patients <45 kg). A recently completed RCT showed that fondaparinux was as effective and as safe as enoxaparin for initial treatment of DVT.23
Oral anticoagulants.
Whether LMWH or unfractionated heparin is used, oral anticoagulant therapy (usually warfarin in North America) is started on the first or second day of treatment.3 Based on level I and II evidence, the usual dose of warfarin is 5 to 10 mg on the first day and 5 mg daily thereafter.25,36 The INR should be tested at least twice during the first week of treatment, weekly during the next 2 to 3 weeks, every 2 weeks during the next 4 weeks, and every 3 to 4 weeks thereafter.37
Whatever warfarin dose regimen is used, treatment with LMWH or unfractionated heparin should be continued for at least 5 days and until the INR has been >2.0 for 2 consecutive days. Warfarin should be administered, with a target INR of 2.0 to 3.0, for 3 months to patients with DVT following exposure to a transient risk factor (eg, surgery, trauma, immobility) and for at least 6 months to patients with unprovoked (or idiopathic) DVT.3 The optimal duration of anticoagulation for this last group is unknown, but long-term treatment should be considered for patients with recurrent venous thromboembolism and for patients with inherited thrombophilia (eg, factor V Leiden mutation) or acquired thrombophilia (eg, antiphospholipid antibody syndrome). For patients with DVT and cancer, recent evidence indicates that long-term treatment with LMWH is superior to oral anticoagulant therapy for preventing recurrent venous thromboembolism.24
Conclusion
For patients with newly diagnosed DVT, good-quality evidence demonstrates the efficacy and safety of outpatient anticoagulant therapy. Outpatient treatment, however, might not be appropriate for all patients. In-hospital treatment should be considered for patients with massive DVT, with symptomatic pulmonary embolism, at high risk of anticoagulant-related bleeding, and with major comorbidity or other factors that warrant in-hospital care.
Biography
Dr Douketis teaches in the Department of Medicine at McMaster University and at St Joseph’s Hospital in Hamilton, Ont.
References
- 1.Tsai AW, Cushman M, Rosamund WD, Heckbert SR, Polak JF, Folsom AR. Cardiovascular risk factors and venous thromboembolism incidence: the longitudinal investigation of thromboembolism etiology. Arch Intern Med. 2002;162(10):1182–1189. doi: 10.1001/archinte.162.10.1182. [DOI] [PubMed] [Google Scholar]
- 2.Hanson PO, Welin L, Tibblin G, Eriksson H. Deep vein thrombosis and pulmonary embolism in the general population. “The Study of Men Born in 1913.”. Arch Intern Med. 1997;157(15):1665–1670. [PubMed] [Google Scholar]
- 3.Hyers TM, Agnelli G, Hull RD, Morris TA, Samama M, Tapson V, et al. Antithrombotic therapy for venous thromboembolic disease. Chest. 2001;119(Suppl 1):176–193. doi: 10.1378/chest.119.1_suppl.176s. [DOI] [PubMed] [Google Scholar]
- 4.Dolovich LR, Ginsberg JS, Douketis JD, Holbrook AM, Cheah G. A meta-analysis comparing low-molecular-weight heparins with unfractionated heparin in the treatment of venous thromboembolism: examining some unanswered questions regarding location of treatment, product type, and dosing frequency. Arch Intern Med. 2000;160(2):181–188. doi: 10.1001/archinte.160.2.181. [DOI] [PubMed] [Google Scholar]
- 5.Hirsh J, Warkentin TE, Shaughnessy SG, Anand SS, Halperin JL, Raschke R, et al. Heparin and low-molecular-weight heparin: mechanism of action, pharmacokinetics, dosing, monitoring, efficacy, and safety. Chest. 2001;119(Suppl 1):64–94. doi: 10.1378/chest.119.1_suppl.64s. [DOI] [PubMed] [Google Scholar]
- 6.O’Brien B, Levine M, Willan A, Goeree R, Haley S, Blackhouse G, et al. Economic evaluation of outpatient treatment with low-molecular-weight heparin for proximal vein thrombosis. Arch Intern Med. 1999;159(19):2298–2304. doi: 10.1001/archinte.159.19.2298. [DOI] [PubMed] [Google Scholar]
- 7.Rodger MA, Gagne-Rodger C, Howley HE, Carrier M, Coyle D, Wells PS. The outpatient treatment of deep vein thrombosis delivers cost savings to patients and their families, compared to inpatient therapy. Thromb Res. 2003;112(1-2):13–18. doi: 10.1016/j.thromres.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 8.Koopman MM, Prandoni P, Piovella F, Ockelford PA, Brandjes DP, van der Meer J, et al. Treatment of venous thrombosis with intravenous unfractionated heparin administered in the hospital as compared with subcutaneous low-molecular-weight heparin administered at home. N Engl J Med. 1996;334(11):682–687. doi: 10.1056/NEJM199603143341102. [DOI] [PubMed] [Google Scholar]
- 9.Levine M, Gent M, Hirsh J, Leclerc J, Anderson D, Weitz J, et al. A comparison of low-molecular-weight heparin administered primarily at home with unfractionated heparin administered in the hospital for proximal deep-vein thrombosis. N Engl J Med. 1996;334(11):677–681. doi: 10.1056/NEJM199603143341101. [DOI] [PubMed] [Google Scholar]
- 10.The Columbus Investigators. Low-molecular-weight heparin in the treatment of patients with venous thromboembolism. N Engl J Med. 1997;337(10):657–662. doi: 10.1056/NEJM199709043371001. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz T, Schmidt B, Hohlein U, Beyer J, Schroder HE, Schellong SM. Eligibility for home treatment of deep vein thrombosis: prospective study. BMJ. 2001;322(7296):1212–1213. doi: 10.1136/bmj.322.7296.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harrison L, McGinnis J, Crowther M, Ginsberg J, Hirsh J. Assessment of outpatient treatment of deep-vein thrombosis with low-molecular-weight heparin. Arch Intern Med. 1998;158(18):2001–2003. doi: 10.1001/archinte.158.18.2001. [DOI] [PubMed] [Google Scholar]
- 13.Wells PS, Kovacs MJ, Bormanis J, Forgie MA, Goudie D, Morrow B, et al. Expanding eligibility for outpatient treatment of deep venous thrombosis and pulmonary embolism with low-molecular-weight heparin: a comparison of patient self-injection with homecare injection. Arch Intern Med. 1998;158(16):1809–1812. doi: 10.1001/archinte.158.16.1809. [DOI] [PubMed] [Google Scholar]
- 14.O’Shaughnessy D, Miles J, Wimperis J. UK patients with deep-vein thrombosis can be safely treated as out-patients. Q J Med. 2000;93(10):663–667. doi: 10.1093/qjmed/93.10.663. [DOI] [PubMed] [Google Scholar]
- 15.Dunn AS, Schechter C, Gotlin A, Vomvolakis D, Jacobs E, Sacks HS, et al. Outpatient treatment of deep venous thrombosis in diverse inner-city patients. Am J Med. 2001;110(6):458–462. doi: 10.1016/s0002-9343(01)00648-9. [DOI] [PubMed] [Google Scholar]
- 16.Mattiasson I, Berntorp E, Bornhov S, Lagerstedt C, Lethagen S, Persson J, et al. Out-patient treatment of acute deep vein thrombosis. Int Angiol. 1998;17(3):146–150. [PubMed] [Google Scholar]
- 17.Ting SB, Zeigenbein RW, Gan TE, Catalono JV, Monagle P, Silvers J, et al. Dalteparin for deep venous thrombosis: a hospital-in-the-home program. Med J Aust. 1998;168(6):272–276. doi: 10.5694/j.1326-5377.1998.tb140160.x. [DOI] [PubMed] [Google Scholar]
- 18.Grau E, Real E, Pastor E, Viciano V, Aguilo J. Home treatment of deep vein thrombosis: a two-year experience of a single institution. Haematologica. 1998;83(5):438–441. [PubMed] [Google Scholar]
- 19.Groce JB. Patient outcomes and cost analysis associated with an outpatient deep venous thrombosis treatment program. Pharmacotherapy. 1998;18(6 Pt 3):175–180. [PubMed] [Google Scholar]
- 20.Mathieu G, Fafard J, Cormier M, Giguère R, Nguyen DT, Dominguez M, et al. Treatment of deep vein thrombosis 1995-2000 in a Montreal university teaching hospital: from in-patient to outpatient care. Ann R Coll Physicians Surg Can. 2001;34:505–508. [Google Scholar]
- 21.Lindmarker P, Holstrom M. Use of low molecular weight heparin (dalteparin), once daily, for the treatment of deep vein thrombosis. A feasibility and health economic study in an outpatient setting. Swedish Venous Thrombosis Dalteparin Trial Group. J Intern Med. 1996;240(6):395–401. doi: 10.1046/j.1365-2796.1996.81877000.x. [DOI] [PubMed] [Google Scholar]
- 22.Merli G, Spiro TE, Olsson GG, Abildgaard U, Davidson BL, Eldor A, et al. Subcutaneous enoxaparin once or twice daily compared with intravenous unfractionated heparin for treatment of venous thromboembolic disease. Ann Intern Med. 2001;134(3):191–202. doi: 10.7326/0003-4819-134-3-200102060-00009. [DOI] [PubMed] [Google Scholar]
- 23.The Matisse Investigators. Fondaparinux compared with low-molecular-weight heparin for the initial treatment of deep vein thrombosis [abstract]. Blood. 2002;100:83. [Google Scholar]
- 24.Lee AY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146–153. doi: 10.1056/NEJMoa025313. [DOI] [PubMed] [Google Scholar]
- 25.Kovacs MJ, Rodger M, Anderson DR, Morrow B, Kells G, Kovacs J, et al. Comparison of 10-mg and 5-mg warfarin initiation nomograms together with low-molecular-weight heparin for outpatient treatment of acute venous thromboembolism. A randomized, double-blind, controlled trial. Ann Intern Med. 2003;138(9):714–719. doi: 10.7326/0003-4819-138-9-200305060-00007. [DOI] [PubMed] [Google Scholar]
- 26.Douketis JD, Foster GA, Crowther MA, Prins MH, Ginsberg JS. Clinical risk factors and timing of recurrent venous thromboembolism during the initial 3 months of anticoagulant therapy. Arch Intern Med. 2000;160(22):3431–3436. doi: 10.1001/archinte.160.22.3431. [DOI] [PubMed] [Google Scholar]
- 27.Douketis JD, Kearon CB, Bates S, Duku EK, Ginsberg JS. The risk of fatal pulmonary embolism in patients with treated venous thromboembolism. JAMA. 1998;279(6):458–462. doi: 10.1001/jama.279.6.458. [DOI] [PubMed] [Google Scholar]
- 28.Douketis JD, Crowther MA, Foster GA, Ginsberg JS. Does the location of thrombosis determine the risk of disease recurrence in patients with proximal deep vein thrombosis? Am J Med. 2001;110(7):515–519. doi: 10.1016/s0002-9343(01)00661-1. [DOI] [PubMed] [Google Scholar]
- 29.Kovacs MJ, Anderson D, Morrow B, Gray L, Touchie D, Wells PS. Outpatient treatment of pulmonary embolism with dalteparin. Thromb Haemost. 2000;83(2):209–211. [PubMed] [Google Scholar]
- 30.Wester JP, de Valk HW, Nieuwenhuis HK, Brouwer CB, van der Graaf Y, Meuwissen OJ, et al. Risk factors for bleeding during treatment of acute venous thromboembolism. Thromb Haemost. 1996;76(5):682–688. [PubMed] [Google Scholar]
- 31.Kuijer PM, Hutten BA, Prins MH, Buller HR. Prediction of the risk of bleeding during anticoagulant treatment for venous thromboembolism. Arch Intern Med. 1999;159(5):457–460. doi: 10.1001/archinte.159.5.457. [DOI] [PubMed] [Google Scholar]
- 32.Bona RD, Hickey AD, Wallace DM. Efficacy and safety of oral anticoagulation in patients with cancer. Thromb Haemost. 1997;78(1):137–140. [PubMed] [Google Scholar]
- 33.Samama MM, Gerotziafas GT. Comparative pharmacokinetics of LMWHs. Semin Thromb Hemost. 2000;26(Suppl 1):31–38. doi: 10.1055/s-2000-9497. [DOI] [PubMed] [Google Scholar]
- 34.Prandoni P, Bagatella P, Bernardi E, Girolami B, Rossi L, Scarano L, et al. Use of an algorithm for administering subcutaneous heparin in the treatment of deep venous thrombosis. Ann Intern Med. 1998;129(4):299–302. doi: 10.7326/0003-4819-129-4-199808150-00006. [DOI] [PubMed] [Google Scholar]
- 35.Turpie AG, Bauer KA, Eriksson BI, Lassen MR. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch Intern Med. 2002;162(16):1833–1840. doi: 10.1001/archinte.162.16.1833. [DOI] [PubMed] [Google Scholar]
- 36.Harrison L, Johnston M, Massicotte MP, Crowther M, Moffat K, Hirsh J. Comparison of 5-mg and 10-mg loading doses in initiation of warfarin therapy. Ann Intern Med. 1997;126(2):133–136. doi: 10.7326/0003-4819-126-2-199701150-00006. [DOI] [PubMed] [Google Scholar]
- 37.Gage BF, Fihn SD, White RH. Management and dosing of warfarin therapy. Am J Med. 2000;109(6):481–488. doi: 10.1016/s0002-9343(00)00545-3. [DOI] [PubMed] [Google Scholar]