Abstract
Purpose
Identify standard self-report questions about functioning suitable for measuring disability across integrated health and social services.
Theory
Functional activities can be validly grouped according to the International Classification of Functioning, Disability and Health (ICF) chapters of mobility, self-care, and domestic life.
Methods
Cross-sectional analysis using information on 112,601 persons interviewed as part of the United States National Health Interview Survey on Disability. We combined related sets of questions and tested the appropriateness of their groupings through confirmatory factor analyses. Construct validity was addressed by seeking to confirm clinically logical relationships between the resulting functional scales and related health concepts, including number of physician contacts, number of bed days, perception of illness, and perception of disability.
Results
Internal consistency for the summed scales ranged from 0.78 to 0.92. Correlations between the functional scales and related concepts ranged from 0.12 to 0.52 in directions consistent with expectations.
Conclusions
Analyses supported the 3 ICF chapters.
Discussions
The routine collection of this core set of functions could enhance decision-making at the client, professional, organizational, and policy levels encouraging cooperation among the medical and social service sectors when caring for people with disabilities.
Keywords: disabled persons, integrated delivery system, computer communication health plan, computerized medical records systems, functional review of systems, international classification of functioning, disability and health (ICF)
Introduction
Health of the individual, or the population as a whole, is not just about the reduction of premature injury, morbidity or mortality [1]. It is also about human functioning and the capacity of the person to participate in society. Recognizing the need for a standard way to describe disability concepts in 2001 the World Health Organization established the International Classification of Functioning, Disability and Health, known as the ICF [2]. The ICF is intended to complement diagnostic information on aetiology, and morbidity included in its tenth revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) [3, 4]. The ICD-10 expresses patients' health conditions, while the ICF, through a separate coding taxonomy, describes the disabilities associated with them. To date there have been few empirical attempts to address how the complicated set of ICF codes might be applied in medical and social care. To be practical, it may be necessary to identify small sets of questions relating the most relevant information [5]. Our intent was to establish a core set of self-report measures of person-level functioning consistent with the ICF that would be sufficiently user friendly for routine collection by busy health care practitioners and social agencies.
Accepted by 191 countries, the ICF is fast becoming the international standard for describing health and disability. There are 2 broad classification categories—(1) Body Functions and Body Structures and (2) Activities and Participation—through which information is organized into chapters of related health concepts. All components within the ICF are quantified using the same generic scale which ranges from “no difficulty” through “complete difficulty.” This generic scale is presented as a means through which various assessment instruments can be calibrated [2]. Activity and Participation codes are organized into “Chapters” of related items. The ICF also includes environmental factors. These are known physical, social and attitudinal features surrounding the person that either hinder or facilitate potential for activity and participation.
The ICF, developed through the consensus of seven international WHO collaborating centres, is considered to be a classification scheme not a measurement system. The collaborative centres call for the “development of assessment instruments for identification and measurement” (p. 251) consistent with ICF concepts. The proposed core set of functions is presented as such an assessment instrument. The series of psychometric analyses to be presented here were necessary to provide evidence for validity of the proposed set of functional measures, and for the key ICF chapters they represent. Our method involves a confirmatory factor analysis applied to empirically test theoretically based constructs established through clinical logic and review of the literature.
Theoretical basis
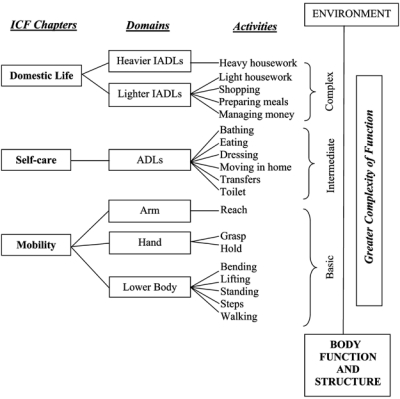
The body function and structure components of the ICF reflect the types of information collected during routine medical review of systems. The core functions are being proposed as an analogous “functional” review of systems that are reflective of the Activity and Participation components. Mobility, self-care, and domestic life echo distinct well-established functional domains documented in the literature and were selected as the ICF chapters most fundamental to clinical objectives. Mobility includes motor functions (such as standing or reaching, etc.). These motor functions have been referred to as “functional limitations” and form the building blocks of more complex activities such as those included in the self-care and domestic life chapters [6]. Self-care describes basic “activities of daily living or ADLs”, such as dressing or toileting, [7] and domestic life captures the more complex “instrumental activities of daily living”, such as shopping or heavy housework [8].
Within our conceptual framework these domains are partly hierarchical. Problems with mobility (the most basic functions) are primarily attributable to impairments in body function or structure, while difficulties with self-care or domestic life activities (the most complex) depend on interactions between those impairments and environmental barriers [9]. Figure 1 illustrates this conceptual framework with the core functions arranged by chapter as supported by the analyses described below. Widespread collection of responses to this core set of functions could aid clinicians and policy makers to make health care more responsive to the needs of individuals. It could improve the support of populations of people with disabilities by encouraging better linkage of health to social care services.
Figure 1.
Structure of Core Functions: The domains of function are seen as in-part hierarchical. Mobility (here represented by body part movements) is most closely related to impairment. As activities become more complex, they are increasingly modulated by environmental factors.
Methods
Data
The core set of functions was developed from questions on the 1994–1995 disability supplement of the National Health Interview Survey on Disability (NHIS-D) [10, 11], originally intended to reflect the World Health Organization's International Classification of Impairment, Disabilities and Handicaps [12] that preceded the ICF. The NHIS-D is a cross-sectional, stratified, random, multi-staged probability sample representative of the United States (US) non-institutionalized population. We selected respondents 18 years of age and older (n=143,007). A random selection of 80% of the data was used (n=116,005). The remaining data were held back for cross validation of multivariate statistical models applying the core set of functions in subsequent analyses not presented here.
NHIS-D questions
The NHIS-D questionnaire obtained information about all members of households selected at random to be representative of the non-institutionalized population. It included questions about abilities to perform 20 routine activities rated as: (1) “no difficulty”, (2) “some difficulty”, (3) “a lot of difficulty”, and (4) “completely unable”. Related questions were grouped according to the content of known measures into mobility, self-care and domestic life scales [6–8], the mobility chapter was anticipated to have 2 domains [13] expressing primarily lower body and upper body functions.
Factor analysis
We applied confirmatory factor analyses in order to empirically test the validity of the theoretical constructs described above. The factor analysis was to be considered successful in validating the hypothesized theoretical model if there was a clear clinical interpretation consistent with expectation for each identified latent factor. Sample weights were used to account for the multistage sampling design. Analyses began assessing the number of underlying latent dimensions necessary to adequately explain correlations among observed item scores. This was done by constructing a Scree plot of the incremental magnitudes of the eigenvalues determined from the correlation matrix versus their rank order. The cumulative sum of eigenvalues divided by the number of items reflects the total variance explained by that number of latent dimensions among the multiple items. The point where the incremental addition of another factor does not appreciably increase this variance indicates that the data do not support further increase in latent dimensionality. We hypothesized that the 20 NHIS-D questions arose from the 4 latent domains expressed above. We further hypothesized correlations between the self-care and domestic life domains to be at least moderate. Therefore, the factor analytic model was determined after promax oblique factor rotation which allows for inter correlation among the factors. In general, the quality of a factor analytic solution is judged on the simplicity of the factor pattern matrix. The factor pattern matrix summarizes the magnitude of the associations between observed measures and underlying latent traits. A simple solution is one in which items tend to be highly associated with only one latent dimension. The objective of factor rotations is to select among the optimal factor pattern matrices, the one that has the simplest structure according to some criterion for ‘simplicity’. Dimension-specific indices were constructed as sum scores from items with factor loading that were greater than 0.40. Factor solutions were obtained using SAS software version 8 [14].
Summed scale analysis and item-total correlations
Cronbach's alpha [15] was used to measure the internal consistency of the constructed sum score scales [16] and to study the effect of deleting the item with the lowest item-total correlations. If removal significantly increased alpha, the item was excluded because its presence detracted from the internal consistency of the constructed sum score index.
Establishing population norms for the scales
The United States population is used to illustrate the process of establishing norms. The number of individuals per 10,000 in the United States who had at least some difficulty with one or more activities in each domain was determined using population weighted data. To calculate confidence limits, the standard error of estimated prevalence values were computed, taking into account the multi-stage sampling design through SUDAAN [17]. As a last step in scale development we translated mean index scores estimated from the 4-level NHIS-D items into 5-category ordinal scales consistent with the 5-level ICF paradigm. This 5-level scale reflects the ICF qualifiers of: no difficulty in any of the items (all scores by definition, were 1), mild difficulty (mean item score ranged from 1 to ≤1.5), moderate difficulty (mean item score ranged from 1.5 to ≤2.5), severe difficulty (mean item score ranged from 2.5 to ≤3.5), and complete difficulty (mean item score ranged from 3.5 to ≤4.0).
Validity
Construct validity of the scales was determined by testing for expected associations with other NHIS-D questions [10, 11] using Spearman rank correlations. The largest associations of the functional scores were expected with perception of disability. Smaller associations were expected with the numbers of physician contacts and the number of days the individual remained in bed at least half the day over the last year.
Results
There were 112, 601 subjects whose data were complete in all 20 activities used to form the scales. Over half (53.4%) were women, 56.4% were between the ages of 18 and 44 years, and 6.2% were over 75 years of age. Just under 2/3 of respondents were described as white. Table 1 characterizes the actual respondents included in this study, and shows the proportion of the population represented by each characteristic.
Table 1.
Characteristics of the sample with weighted crude proportion of cases used to establish the core set of functions
| Percent |
|||
|---|---|---|---|
| Variables | Number* | Actual | Weighted |
| Gender | |||
| Female | 60111 | 53.4 | 52.0 |
| Male | 52490 | 46.6 | 48.0 |
| Race | |||
| White | 79602 | 71.0 | 75.0 |
| Black | 13145 | 11.7 | 10.9 |
| Hispanic | 14630 | 13.0 | 9.5 |
| Other | 4724 | 4.2 | 4.6 |
| Age | |||
| 18–44 | 63453 | 56.4 | 57.8 |
| 45–64 | 31009 | 27.5 | 26.7 |
| 65–69 | 5897 | 5.2 | 5.0 |
| 70–74 | 5211 | 4.6 | 4.4 |
| 75 and older | 7031 | 6.2 | 6.1 |
Numbers of actual respondents used in building the functional indices are shown for each characteristic. Note: Race was missing from 500 cases.
Item level analyses
Eating was the activity in which the fewest reported problems and walking 1/4 mile was the activity in which the largest number reported problems. At least some individuals were coded as functioning at each level in each of the 20 items.
Factor analysis
The Scree plot of eigenvalues identified a 4-factor solution as optimum. These first 4 eigenvalues summed to 70% of the total sum of the eigenvalues. The rotated factor pattern is shown in Table 2, supporting the 3 ICF chapters of mobility (factors 1 and 4), self care (factor 2) and domestic life (factor 3), with the mobility chapter further sub-divided into lower (factor 2) and upper body scales (factor 4), as expected. Review of the factor loadings of items associated with each factor shows all expected items met the minimum 0.40 criterion for belonging to their expected latent dimension. For example, loadings for the first factor ranged from 0.65 to 0.87. In contrast, factor loadings for those items identified as associated with factor 1 were close to zero with one exception. The factor 3 loading for “heavy house work” was 0.39, although still below the 0.40 criteria. This implies that this activity is multidimensionally associated with factor 3 as well as with factor 1. This activity hypothesized to be associated with items in the domestic life chapter (factor 3), was associated more strongly with lower body functions (factor 1). The “reaching” activity in upper body functions loaded weakly compared to the other activities in the upper body function (factor 4) domain. All other items loaded on the factors expected.
Table 2.
Rotated factor matrix—describes how each item loads on the underlying dimensions as named—and summary of item total correlations and Cronbach alphas after deletion of each variable
| Factors |
Correlation with Total | Alpha after item removal | ||||
|---|---|---|---|---|---|---|
| Activity | 1 | 2 | 3 | 4 | ||
| Factor 1 | ||||||
| Walking a quarter mile | 0.869 | −0.023 | −0.024 | −0.003 | 0.767 | 0.858 |
| Walking up 10 steps | 0.821 | 0.070 | −0.040 | 0.013 | 0.766 | 0.860 |
| Standing 20 minutes | 0.809 | 0.064 | −0.065 | 0.031 | 0.737 | 0.863 |
| Bending from standing | 0.758 | 0.096 | −0.109 | 0.100 | 0.701 | 0.869 |
| Lifting 10 pounds | 0.703 | 0.001 | 0.040 | 0.121 | 0.670 | 0.873 |
| Doing heavy housework* | 0.649 | −0.171 | 0.389 | −0.025 | 0.623 | 0.885 |
| Factor 2 | ||||||
| Getting in and out of bed or chairs | 0.020 | 0.923 | −0.032 | −0.045 | 0.847 | 0.889 |
| Using toilet | 0.060 | 0.920 | −0.063 | −0.012 | 0.827 | 0.892 |
| Getting around home | 0.085 | 0.890 | −0.052 | −0.052 | 0.809 | 0.893 |
| Dressing | 0.017 | 0.782 | 0.013 | 0.029 | 0.826 | 0.891 |
| Eating | −0.236 | 0.629 | 0.199 | 0.246 | 0.619 | 0.922 |
| Bathing | 0.171 | 0.626 | 0.205 | −0.049 | 0.755 | 0.911 |
| Factor 3 | ||||||
| Managing money | −0.078 | −0.059 | 0.909 | 0.026 | 0.682 | 0.840 |
| Using telephone | −0.229 | 0.110 | 0.767 | 0.133 | 0.587 | 0.869 |
| Preparing meals | 0.086 | 0.186 | 0.734 | −0.045 | 0.815 | 0.807 |
| Shopping | 0.330 | −0.012 | 0.703 | −0.081 | 0.765 | 0.828 |
| Doing light housework | 0.332 | 0.196 | 0.502 | −0.071 | 0.705 | 0.834 |
| Factor 4 | ||||||
| Using fingers for grasping | 0.115 | −0.033 | −0.004 | 0.845 | 0.589 | 0.498 |
| Holding pen/pencil | 0.028 | 0.029 | 0.051 | 0.835 | 0.581 | 0.540 |
| Reaching* | 0.373 | 0.014 | −0.045 | 0.457 | 0.405 | 0.780 |
Item removed from factor to create final scale.
As anticipated, the largest inter-factor correlation was between self-care and domestic life, at 0.54. The next largest were between lower body and self-care and lower body and domestic life, 0.46 and 0.42, respectively. The remaining inter-factor correlations were less than 0.33.
Excluding shared variance, the percentages of variance explained by the lower body, self-care, domestic life, and upper body domains were 14.9%, 12.6%, 10.0%, and 7.7%, respectively. Including shared variance, the percentages of variance explained by these same factors were 32.4%, 34.4%, 29.1%, and 18.8%, respectively. The final communality estimates of items ranged from 44% for reaching to 83% for getting in and out of beds and chairs. The communality of a variable is the percentage of variance in an observed variable explained by the latent factors.
Internal consistency of constructed scales
Cronbach's alpha (internal consistency) was 0.89, 0.92, 0.69, and 0.97, for the lower body, self-care, upper body, and domestic life scales, respectively. As noted above, a single item, heavy housework, did not appear to fit its anticipated construct. Expected to load most heavily on domestic life, it loaded slightly more heavily on lower body functions. Tested with both constructs, heavy housework had the lowest item-total correlations of all items. It was removed after documenting that its inclusion reduced internal consistency of the domestic life and failed to improve internal consistency of the lower body scale. This is important because it suggests that heavy housework, although occupationally related to light housework, is different from the other items currently included in either scale.
Although difficulty reaching met the 0.40 loading criterion necessary for inclusion in the hand and arm use scale, it had the lowest item-total correlation. Internal consistency of items in the upper body use scale increased from 0.69 to 0.78 after it was excluded. Although unexpected, this improvement in internal consistency with the removal of reaching makes sense clinically. Certainly hand and arm function are physiologically and anatomically distinct. The reaching and heavy housework variables were removed from the scales but included in subsequent analyses as separate indicators of arm use and heavier domestic life activities, respectively. Alphas were stable for the other scales when the lowest correlating item was removed. Consequently, the core set of functions yields 3 chapters expressing mobility, self-care, and domestic life activities. Mobility sub-divides into lower body, hand use, and arm use. Self-care includes a single ADL scale. Domestic life divides into lighter and heavier instrumental activities of daily living. The final alphas were 0.89, 0.78, 0.92, and 0.87 for the lower body functional limitation, the upper body functional limitation, self care scales, and domestic life scales, respectively. These findings support the conceptual framework of measurement as diagrammed in Figure 1.
These concepts are organized by ICF Chapter into a simple self-report checklist that can be applied in the clinic (Table 3).
Table 3.
The ICF core functions
| 1. No difficulty | 2. Some difficulty | 3. A lot of difficulty | 4. Completely unable | 5. Do not know | |
|---|---|---|---|---|---|
| Mobility: Lower body | |||||
| Walking one quarter-mile | ○ | ○ | ○ | ○ | ○ |
| Walking up 10 steps | ○ | ○ | ○ | ○ | ○ |
| Standing 20 minutes | ○ | ○ | ○ | ○ | ○ |
| Lifting 10 pounds | ○ | ○ | ○ | ○ | ○ |
| Bending down from a standing position to pick up an object from the floor | ○ | ○ | ○ | ○ | ○ |
| Mobility: Hand use | |||||
| Grasp handle | ○ | ○ | ○ | ○ | ○ |
| Hold pen | ○ | ○ | ○ | ○ | ○ |
| Mobility: Arm use | |||||
| Reaching | ○ | ○ | ○ | ○ | ○ |
| Self-care | |||||
| Getting to and using toilet | ○ | ○ | ○ | ○ | ○ |
| Getting in and out of chairs/bed | ○ | ○ | ○ | ○ | ○ |
| Moving inside home | ○ | ○ | ○ | ○ | ○ |
| Dressing | ○ | ○ | ○ | ○ | ○ |
| Eating | ○ | ○ | ○ | ○ | ○ |
| Bathing or showering | ○ | ○ | ○ | ○ | ○ |
| Domestic life—Light | |||||
| Managing money | ○ | ○ | ○ | ○ | ○ |
| Preparing meals | ○ | ○ | ○ | ○ | ○ |
| Shopping | ○ | ○ | ○ | ○ | ○ |
| Light housework | ○ | ○ | ○ | ○ | ○ |
| Domestic life—Heavy | |||||
| Heavy housework | ○ | ○ | ○ | ○ | ○ |
Validity
Construct validity was supported by Spearman rank correlations between the functional limitation scores and perceived disability, ranging from 0.27 to 0.52; for bed days, from 0.10 to 0.20; for number of physician contacts, from 0.12 to 0.20; and for perceived health status, from 0.15 to 0.35. The generally larger correlations with the perceived disability construct were taken as evidence for construct validity.
Table 4 estimates the United States population prevalence (per 10,000 persons) expected to have at least some difficulty performing one or more of the activities in each domain or chapter based on population weighted data. Problems with lower body functioning appear by far the most prevalent and self-care limitations the least.
Table 4.
Applying the core functions to show patterns of disability in a population
| Scale | Prevalence estimate | 95% Confidence Interval |
|---|---|---|
| Lower body functional limitation | 1025 | 999–1051 |
| Reaching over head or out | 215 | 204–225 |
| Hand use | 229 | 218–240 |
| Self-care (ADL) | 135 | 127–143 |
| Domestic life (IADL) | 216 | 205–227 |
| Heavy housework | 394 | 377–412 |
Discussion
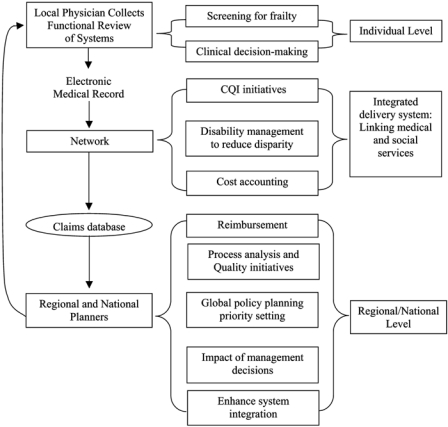
Results of our factor analyses support the core set of functional measures organized into the mobility, self-care, and domestic life chapters bridging population level NHIS variables from the US with ICF concepts. By facilitating standard comparisons for clinical practice and program evaluation, we propose that this standard set of core functions can help link and coordinate care across general practitioners, rehabilitation professionals, and social services as well as acute and long term care sectors. The component scales appear to reflect distinct clinically relevant concepts that correlate expectedly with perceived disability, perceived illness, greater numbers of bed days, and increased physician utilization in the US supporting construct validity. The core set of functions are sufficiently parsimonious for acquisition during routine clinical encounters through patient self-report or proxy. Appropriate use could express the effects of illnesses, injuries and interventions on life participation in ways that are meaningful to patients [18] and facilitate communication among the many professionals and organizations necessary in providing care to patients with disabilities and multiple needs. Once collected, the core functions could be disseminated through electronic formats across settings [19] and applied in multi-level analyses (Figure 2). Uploads from the medical clinic to administrative databases with linkage to diagnostic information could enable population surveillance at the health plan, regional, and national levels. Such an “information highway” for centralizing medical and functional status information [20] has already been proposed by the Canadian government. All public, private, or voluntary health and social service organizations in an area could agree to participate in an umbrella system in efforts to enhance the coordination and efficiency of care for patients with multiple needs, while maintaining their own structures [21].
Figure 2.
The proposed functional information infrastructure.
The core set of functions might serve as a functional review of systems and routine screen for frailty. Physicians typically overlook the disabilities perceived by their patients [21]. Disability is associated with reduced use of preventive services, such as mammograms [22, 23], the tendency to diagnose cancer at later stages [24], and elevated risks of institutionalization and mortality [5, 25–28]. Specific interventions to help older people maintain independent functioning have shown benefits across multiple health, function, and quality of life domains [29–31].
Program evaluators and clinicians in integrated settings have long struggled with applicability of normative data across populations. The routine collection of these core functions during patient encounters could prove important to both program evaluators and clinicians. It could provide a meaningful first step towards obtaining normative data about disabilities across populations for integrated service planning purposes. Although people with disabilities comprise only about 1/6 of the population in the US, they account for almost half of all medical spending [32]. Measures of function are used in determining national payment rates for long-term care [33], rehabilitation [34], and home care services [35, 36]; in addressing best practices among large health systems [37, 38]; and in monitoring population health goals regionally and nationally [39]. Each application uses different measures, hindering integration of objectives, blocking the integration of health and social services and potentially leading to duplication of efforts across venues or programs of care. Seeing this as problematic, the Benefits Improvement Act of 2001, supported by the U.S. Medicare Payment Advisory Commission [40], mandated development of standard scales for assessing the health and functioning of patients across all post-acute settings [41]. Additionally, a joint report by the U.S. Department of Health and Human Services and the Centres for Disease Control [42] called for projects to demonstrate the inclusion of functional status data in standardized electronic patient records, claims forms, and encounter forms, acclaiming the ICF as the most promising approach to standard measurement. The heterogeneity of patients served across care venues makes the identification of a parsimonious set of questions challenging.
The core functions were selected to be consistent with ICF concepts and to bridge content across measures typically applied in the acute [42, 43], rehabilitative [44], and long-term care settings [45]. Isolated difficulty with heavy housework and shopping will identify people with milder disabilities, while problems using the toilet and eating will identify those with more severe disabilities. Reliability of the core functional scales was consistent with commonly used health status instruments [46–50]. The core set is not intended to replace the more detailed setting- or condition-specific instruments but rather to offer global indicators appropriate to linking and transmitting information across venues.
We end with several cautionary notes. Specific to each health system and nation, demonstrations will be needed to determine appropriateness of these measures to the proposed applications. We caution that it may not be reasonable to hold health care systems responsible for the functional deterioration of individual patients. While the linking of individuals' self-report functional status information to administrative databases could provide a “powerful window” for showing the effectiveness of the health care system [51], use of such information has implications with regard to protecting individual privacy [52] and could be applied by payers to exclude populations of people whose disabilities (they believe) will likely cause high future expenditures. Ongoing debate is necessary on whether the value of collecting this type of information and enabling its reuse for administrative and policy purposes outweighs the potential economical and non-economical costs of collection.
Acknowledgments
This research was supported in part by NIH grant # R01-HD37234 from the National Institute of Child Health and Human Development of the United States of America. The opinions of the authors are not necessarily those of the sponsoring agency. Parts of this research were presented at the 49th Annual Meeting of the American Congress of Rehabilitation Medicine and the 9th Annual Meeting of the American Society of Neurorehabilitation, Philadelphia, PA, October 3–6, 2002.
Contributor Information
Margaret G. Stineman, Department of Physical Medicine and Rehabilitation, Senior Fellow, Leonard Davis Institute of Health Economics Associate Scholar, Clinical Epidemiology Unit, Center for Epidemiology and Biostatistics Senior Fellow, Institute on Aging, University of Pennsylvania, Philadelphia.
Richard N. Ross, Department of Physical Medicine and Rehabilitation, University of Pennsylvania, Philadelphia.
Greg Maislin, Department of Medicine, and Senior Fellow, School of Nursing, University of Pennsylvania, Philadelphia Principal Biostatistician, Biomedical Statistical Consulting, Wynnewood, Philadelphia.
Reviewers
Berrie Middel, Dr., Department of Health Sciences, University of Groningen, the Netherlands
Susanne M. Bruyère, PhD, CRC, NCC, Director Employment and Disability Institute, Professor of Disability Studies, Cornell University, School of Industrial and Labor Relations-Extension Division, Ithaca, New York, USA
Marianne C. Fahs, PhD, MPH, Professor of Urban Public Health, Research Director, Brookdale Center on Aging, Hunter College, City University of New York, USA
References
- 1.Brundtland GH. Speech before WHO conference on health and disability Trieste. 2002. Apr 18, [cited 2005 Jun 6]. Available from: URL http://www.who.int/director-general/speeches/2002/english/20020418_disabilitytrieste.html.
- 2.World Health Organization. International classification of functioning Disability and health: ICF. Geneva: WHO; 2001. [Google Scholar]
- 3.Üstün TB, Chatterji S, Kostansjek N, Bickenbach J. WHO's ICF and functional status information in health records. Health Care Financing Review. 2003;24(3):77–88. [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. The international statistical classification of diseases and related health problems. 10th rev. 1–3. Geneva: WHO; pp. 1992–1994. [Google Scholar]
- 5.Stuck AE, Egger M, Hammer A, Minder CE, Beck JC. Home visits to prevent nursing home admissions and functional decline in elderly people: systematic review and meta-regression analysis. Journal of the American Medical Association. 2002;287(8):1022–8. doi: 10.1001/jama.287.8.1022. [DOI] [PubMed] [Google Scholar]
- 6.Nagi SZ. Disability concepts revisted: implictions for prevention. In: Pope AM, Tarlov AR, editors. Disability in America: toward a national agenda for prevention. Washington, DC: National Academy Press; 1991. pp. 309–27. [Google Scholar]
- 7.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185(12):914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 8.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–86. [PubMed] [Google Scholar]
- 9.Stineman MG. A model of health environmental integration. Topics of Stroke Rehabilitation. 2001;8(2):34–45. doi: 10.1310/0L5G-NQHY-GH4K-HV58. [DOI] [PubMed] [Google Scholar]
- 10.National Center for Health Statistics. Data file documentation, National health interview survey on disability, Phase I, 1994 (machine readable data file and documentation) Hyattsville, MD: NCHS; 1996. [Google Scholar]
- 11.National Center for Health Statistics. Data file documentation, National health interview survey on disability, Phase II, Adult File 1995 (machine readable data file and documentation) Hyattsville, MD: NCHS; 1998. [Google Scholar]
- 12.World Health Organization. International classification of impairments, disabilities and handicaps. Geneva: WHO; 1980. [Google Scholar]
- 13.Gerety MB, Mulrow CD, Tuley MR, Hazuda HP, Lichtenstein MJ, Bohannon R, et al. Development and validation of a physical performance instrument for the functionally impaired elderly: the physical disability index (PDI) Gerontologist. 1993 Mar;48(2):M33–8. doi: 10.1093/geronj/48.2.m33. [DOI] [PubMed] [Google Scholar]
- 14.SAS Institute, Inc. SAS OnlineDoc®. Version 8. Cary, NC: SAS Inst; 2000. Feb, [Google Scholar]
- 15.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 16.Nunnally JC. Psychometric theory. 2nd edition. New York: McGraw-Hill; 1978. [Google Scholar]
- 17.Shah BV, Barnwell BG, Bieler GS. SUDAAN User's manual: software for the statistical analysis of correlated data. Research Triangle Park, NC: Research Triangle Institute; 1995. [Google Scholar]
- 18.National Committee on Vital and Health Statistics. NCVS 2000–2002. [DHHS Publication Number (PHS) 2003-1203. Washington, DC: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2003. [Google Scholar]
- 19.Harris MR, Ruggieri AP, Chute CG. From clinical records to regulatory reporting: formal terminologies as foundation. Health Care Financing Review. 2003;24(3):103–20. [PMC free article] [PubMed] [Google Scholar]
- 20.Bickenbach JE. Functional status and health information in Canada: proposals and prospects. Health Care Financing Review. 2003;24(3):89–102. [PMC free article] [PubMed] [Google Scholar]
- 21.Hebert R, Veil A. Monitoring the degree of implementation of an integrated delivery system. International Journal of Integrated Care [serial online] 2004 Sep 20;4 doi: 10.5334/ijic.106. Available from: URL: www.ijic.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Calkins DR, Rubenstein LV, Cleary PD, Davies AR, Jette AM, Fink A, et al. Failure of physicians to recognize functional disability in ambulatory patients. Annals of Internal Medicine. 1991;114(6):451–4. doi: 10.7326/0003-4819-114-6-451. [DOI] [PubMed] [Google Scholar]
- 23.Iezzoni LI, McCarthy EP, Davis RB, Harris-David L, O'Day B. Use of screening and preventive services among women with disabilities. American Journal of Medical Quality. 2001;16(4):135–44. doi: 10.1177/106286060101600405. [DOI] [PubMed] [Google Scholar]
- 24.Iezzoni LI, McCarthy E, Davis RB, Siebens H. Mobility impairments and use of screening and preventive services. American Journal of Public Health. 2000;90(6):955–61. doi: 10.2105/ajph.90.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roetzheim RG, Chirikos TN. Breast cancer detection and outcomes in a disability beneficiary population. Journal of Health Care for Poor and Underserved. 2002;13(4):461–76. doi: 10.1353/hpu.2010.0606. [DOI] [PubMed] [Google Scholar]
- 26.Inouye SK, Peduzzi PN, Robison JT, Hughes JS, Horwitz RI, Concato J. Importance of functional measures in predicting mortality among older hospitalized patients. Journal of the American Medical Association. 1998;279(15):1187–93. doi: 10.1001/jama.279.15.1187. [DOI] [PubMed] [Google Scholar]
- 27.Narain P, Rubenstein LZ, Wieland GD, Rosbrook B, Strome LS, Pietruszka F, et al. Predictors of immediate and 6-month outcomes in hospitalized elderly patients. The importance of functional status. Journal of the American Gerontological Society. 1988 Sep 9;36:775–83. doi: 10.1111/j.1532-5415.1988.tb04259.x. [DOI] [PubMed] [Google Scholar]
- 28.Nikolaus T, Bach M, Oster P, Schlierf G. Prospective value of self-report and performance-based tests of functional status for 18-month outcomes in elderly patients. Aging-Clinical and Experimental Research. 1996;8(4):271–6. doi: 10.1007/BF03339578. [DOI] [PubMed] [Google Scholar]
- 29.Wolinsky FD, Callahan CM, Fitzgerald JF, Johnson RJ. Changes in functional status and the risks of subsequent nursing home placement and death. Journal of Gerontology. 1993;48(3):S94–101. [PubMed] [Google Scholar]
- 30.Clark F, Azen SP, Zemke R, Jackson J, Carlson M, Mandel D, et al. Occupational therapy for independent living older adults. A randomized controlled trial. Journal of the American Medical Association. 1997;278:1321–6. [PubMed] [Google Scholar]
- 31.Cohen HJ, Feussner JR, Weinberger M, Carnes M, Hamdy RC, Hsieh F, et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. New England Journal of Medicine. 2002 Mar 21;346(12):905–12. doi: 10.1056/NEJMsa010285. [DOI] [PubMed] [Google Scholar]
- 32.Stuck AE, Aronow HU, Steiner A, Alessi CA, Bula CJ, Gold MN, et al. A trial of annual in-home comprehensive geriatric assessments for elderly people living in the community. New England Journal of Medicine. 1995 Nov 2;333(18):1184–9. doi: 10.1056/NEJM199511023331805. [DOI] [PubMed] [Google Scholar]
- 33.Max W, Rice DP, Trupin L. Medical expenditures for people with disabilities. [cited 2005 Jun 6];Disability statistics abstract. 1995 12:1–4. Available from: URL: http://dsc.ucsf.edu/pdf/abstract12.pdf. [Google Scholar]
- 34.Fries BE, Schneider DP, Foley WJ, Gavazzi M, Burke R, Cornelius E. Refining a case-mix measure for nursing homes: resource utilization groups (RUG-III) Medical Care. 1994;32(7):668–85. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Stineman MG, Tassoni CJ, Escarce JJ, Goin JE, Granger CV, Fiedler RC, et al. Development of function related groups version 2.0: a classification system for medical rehabilitation. Health Services Research. 1997 Oct;32(4):529–48. [PMC free article] [PubMed] [Google Scholar]
- 36.Grimaldi PL. Prospective rates for episodes of home health care. Journal of Health Care Financing Review. 2002;28(3):63–75. [PubMed] [Google Scholar]
- 37.Shaughnessy PW, Schlenke RE, Hittle DF. Case mix of home health patients under capitated and fee-for-service payment. Health Services Research. 1995;30(1):79–113. [PMC free article] [PubMed] [Google Scholar]
- 38.Allen H. Anticipating market demand: tracking enrollee satisfaction and health over time. International Journal of Quality Health Care. 1998;20(6):463–5. doi: 10.1093/intqhc/10.6.521. [DOI] [PubMed] [Google Scholar]
- 39.Selim AJ, Berlowitz DR, Finke G, Rosen AK, Ren XS, Christiansen CL, et al. Risk-adjusted mortality rates a potential outcome indicator for outpatient quality assessments. Medical Care. 2002 Mar;40(3):237–45. doi: 10.1097/00005650-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Department of Health and Human Services. Healthy people 2010: understanding and improving health. 2nd edition. Washington, DC: U.S. GPO; 2000. Nov, [Google Scholar]
- 41.Medicare Payment Advisory Commission. Prospective payment for post-acute care: current issues and long-term agenda. Report to the congress: Medicare payment policy. Washington, DC: MedPAC; 2001. Mar, pp. 87–95. [Google Scholar]
- 42.National Committee on Vital and Health Statistics. Classifying and reporting health status. Washington, DC: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2001. [Google Scholar]
- 43.McHorney CA, Ware JE. Construction and validation of an alternate form general mental health scale for the medical outcomes study short-form 36-item health survey. Medical Care. 1995;33:15–28. doi: 10.1097/00005650-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 44.Ware JE, Sherbourne CD. The MOS 36-item Short Form Health Survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 45.Hamilton BB, Granger CV, Sherwin FS, Zielezney M, Tashman JS. A uniform data system for medical rehabilitation. In: Fuhrer MJ, editor. Rehabilitation Outcomes: Analysis and Measurement. Baltimore, MD: Paul H. Brookes Publishing Co; 1987. pp. 137–48. [Google Scholar]
- 46.Morris JN, Murphy K, Nonemaker S. Long term care resident assessment user's manual, version 2.0. Health care financing administration. Baltimore, MD: U.S. GPO; 1995. Oct, [Google Scholar]
- 47.Bergner M, Bobbitt RA, Pollard WE, Martin DP, Gilson BS. The sickness impact profile: validation of a health status measure. Medical Care. 1976;14(1):57–67. doi: 10.1097/00005650-197601000-00006. [DOI] [PubMed] [Google Scholar]
- 48.Jette AM, Davies AR, Cleary PD, Calkins DR, Rubenstein LV, Fink A, et al. The functional status questionnaire: reliability and validity when used in primary care. Journal of General Internal Medicine. 1986 May;1:143–9. doi: 10.1007/BF02602324. [DOI] [PubMed] [Google Scholar]
- 49.McHorney CA, Ware JE, Lu JF, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care. 1994;32(1):40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 50.Stineman MG, Shea JA, Jette A, Tassoni CJ, Ottenbacher KJ, Fiedler R, et al. The functional independence measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Archives of Physical Medicine and Rehabilitation. 1996 Nov;77(11):1101–8. doi: 10.1016/s0003-9993(96)90130-6. [DOI] [PubMed] [Google Scholar]
- 51.Iezzoni LI, Greenberg MS. Capturing and classifying functional status information in administrative databases. Health Care Financing Review. 2003;24(3):61–76. [PMC free article] [PubMed] [Google Scholar]
- 52.U.S. Department of Health and Human Services, Office for civil rights. Summary of the HIPAA privacy rule. [cited 2005 Jun 6]. Available from: URL: http://www.hhs.gov/ocr/hipaa.