“No democracy has ever starved.”
— Amartya Sen, Nobel laureate economist
As rates of obesity continue to increase in the world's more affluent nations, it is difficult to comprehend that malnutrition affects over 800 million people worldwide. Six million children under the age of 5 die each year of malnutrition (www.unicef.org/sowc98), and 115 million remain malnourished.
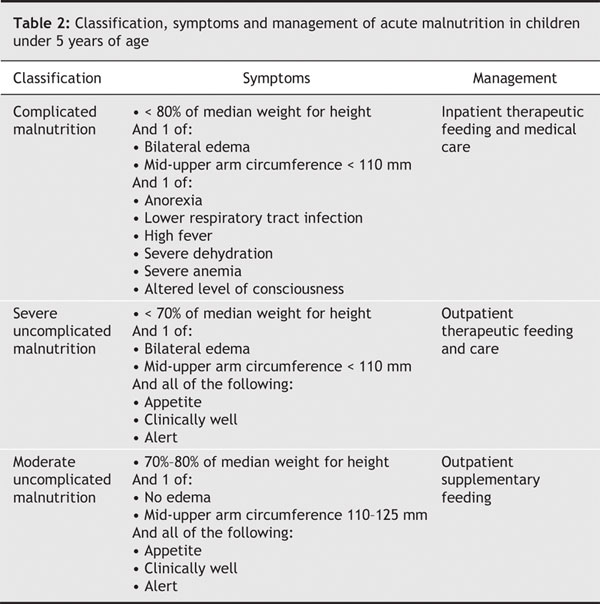
Varying types of malnutrition exist, including micronutrient deficiency (Table 1) and protein energy malnutrition (PEM). PEM consists of both kwashiorkor and marasmus and is further clinically subdivided into complicated, severe uncomplicated and moderate uncomplicated malnutrition (Table 2).2 Mortality from severe malnutrition is high, and recovery is complicated by coinfection, abnormal electrolyte levels, sepsis, hepatoinsufficiency and congestive heart failure.1,3
Table 1
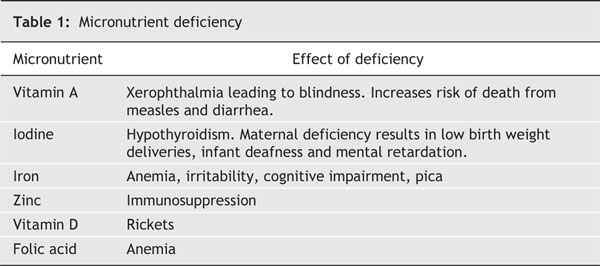
Table 2
Rates of malnutrition worldwide show no sign of decreasing. In fact, recent analysis predicts that an extra 100 million people will be starving by 2015 (www.aaas.org/news/releases/2006/0217poverty.shtml), a sobering projection considering the United Nation's millennium development goal to halve the worldwide rate of malnutrition by that year (www.un.org/millenniumgoals/index.asp).
The challenge of addressing malnutrition lies in its complicated causes and the complex interplay of individual, maternal, familial, societal, political and environmental forces that initiate and perpetuate malnutrition.
Endemic poverty is perhaps the one feature common to almost all causes of malnutrition. Over 2 billion people live on less than $2 a day, and many rely on small plots of land as their main source of food and income. Without savings, and when harvests fail from drought or deluge, malnutrition is inevitable. Political systems can also perpetuate malnutrition. Violent conflict disrupts food production and distribution, while despotic leadership, poor governance and widespread corruption undermine efforts to precipitate positive change.
Secondary contributors to malnutrition are also evident. Over a billion people cannot access clean water, and preventable and treatable infectious diseases weaken millions. Childhood immunization rates for common diseases such as measles and whooping cough are still alarmingly low in many poorer countries,3 while high prenatal and maternal morbidity and mortality from malnutrition perpetuate a generational cycle of poverty and hunger.3
Treating malnutrition once it has been recognized and when resources have been provided is relatively straightforward. Anthropometric surveys can be conducted rapidly, and therapeutic feeding centres constructed and put into operation. In addition to food supplementation, initiatives to combat vitamin A, iron and iodine deficiencies are required. Creative work by nongovernmental organizations has shown that large groups of children experiencing PEM can receive treatment in community-based therapeutic care programs with good outcomes (www.msf.org/msfinternational/invoke.cfm?component=article&objectid=CB803D87-94DC-423E-98E2485EAAAC0873&method=full_html). Simple and locally driven nutrition supplementation initiatives that focus on undernourished pregnant women have had positive effects on subsequent infant and childhood morbidity and mortality figures.3 The World Food Programme has been established to collect food from donor countries and oversee its distribution to international and local nongovernmental organizations in “Food for Life, Food for Growth, and Food for Work” programs (www.wfp.org/food_aid/introduction/index.asp?section=12&sub_section=1).
The prevention of malnutrition is a global collective problem. Providing food and medical care to malnourished populations is but a stopgap measure. Generating real change will only come after a united global community creates peaceful and imaginative solutions. A commitment to invest in and support universal education, health care initiatives and sustainable agricultural efforts, and to reduce trade barriers and offer debt relief is paramount (www.imf.org/external/np/exr/facts/hipc.htm).
The time to begin is now.
Simon Pulfrey Department of Emergency Medicine St. Paul's Hospital Vancouver, BC
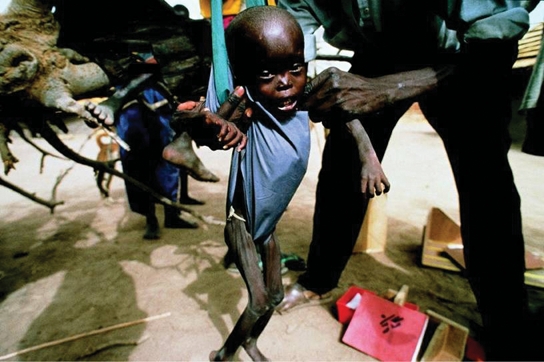
Figure. Weighing a child during a rapid nutritional assessment survey in Democratic Republic of Congo, 1997. Photo by: Rapid nutrition assessment survey DRC 1997 (MSF Archives)
Footnotes
Competing interests: None declared.
REFERENCES
- 1.Waterlow JC. Protein-energy malnutrition. London: Hodder & Stroughton; 1992.
- 2.Collins S, Yates R. The need to update the classification of acute malnutrition. Lancet 2003;362:249. [DOI] [PubMed]
- 3.Young H, Borrel A, Holland D, et al. Public nutrition in complex emergencies. Lancet 2004;365:1899-909. [DOI] [PubMed]


