Abstract
Background: Rapid reperfusion improves survival for patients with acute ST-segment elevation myocardial infarction (STEMI). We sought to analyze recent trends in door-to-reperfusion time and identify hospital characteristics associated with improved performance.
Methods: In this retrospective observational study from the National Registry of Myocardial Infarction 3 and 4 between 1999 and 2002, we analyzed door-to-needle and door-to-balloon times in patients admitted with STEMI and receiving fibrinolytic therapy (n=68,439 patients in 1,015 hospitals) or percutaneous coronary intervention (n=33,647 patients in 421 hospitals) within 6 hours of hospital arrival.
Results: In 1999, only 46% of the patients in the fibrinolytic therapy cohort were treated within the recommended 30-minute door-to-needle time; only 35% of the patients in the percutaneous coronary intervention cohort were treated within the recommended 90-minute door-to-balloon time. Improvement in these times to reperfusion over the 4-year study period was not statistically significant (door-to-needle: -0.01 min/yr, CI -0.24, +0.23, p > 0.9; door-to-balloon: -0.57 min/yr, CI -1.24, +0.10, p=0.09). Only 33% (337/1,015) of hospitals improved door-to-needle time by more than 1 minute per year, and 26% (110/421) improved door-to-balloon time by more than 3 minutes per year. No hospital characteristic was significantly associated with improvement in door-to-needle time. Only high annual percutaneous coronary intervention volume and location in New England were significantly associated with greater improvement in door-to-balloon time.
Conclusions: Fewer than half of patients with STEMI receive reperfusion in the recommended door-to-needle or door-to-balloon time, and mean time to reperfusion has not decreased significantly in recent years. Relatively few hospitals have shown substantial improvement.
Condensed Abstract
We analyzed door-to-needle and door-to-balloon times in patients admitted with ST-segment elevation myocardial infarction and receiving fibrinolytic therapy (n=68,439 patients in 1,015 hospitals) or percutaneous coronary intervention (n=33,647 patients in 421 hospitals) within 6 hours of hospital arrival in the National Registry of Myocardial Infarction 3 and 4. Despite national initiatives to measure and reduce these times, guideline recommendations were met less than half of the time, with no substantial trend toward improvement. Nevertheless, some individual hospitals experienced substantial improvement while others worsened. Structural features of hospitals did not adequately predict change in performance. Other factors need to be identified and used by hospitals for performance improvement programs.
Introduction
Shorter time to reperfusion is associated with better survival for patients with ST-segment elevation myocardial infarction (STEMI), whether they receive fibrinolytic therapy1, 2 or percutaneous coronary intervention (PCI).3-5 Recently published guidelines recommend goals of 30 minutes for presentation at the hospital to the administration of fibrinolytic therapy (door-to-needle time) and 90 minutes for presentation at the hospital to the inflation of an angioplasty balloon (door-to-balloon time).6 The Centers for Medicare and Medicaid Services and the Joint Commission on Accreditation of Healthcare Organizations have identified time to reperfusion as important quality indicators for acute myocardial infarction (AMI).
No contemporary information exists about hospital performance in achieving national benchmarks for time to reperfusion. Previous investigators determined that the average door-to-needle time decreased from 62 minutes in 1990 to 38 minutes in 1999.7 However, this average time in 1999 was still longer than the guideline recommendations, and no information was provided on door-to-balloon time. Moreover, studies of time to reperfusion did not evaluate hospital-level performance.
Several related questions remain. First, at the hospital level, has time to fibrinolytic therapy decreased in more recent years and are hospitals reaching the guideline recommendations? Second, has the time to PCI improved? Third, what is the variation in individual hospital improvement in time to reperfusion? Finally, are there hospital characteristics associated with improvement? To address these questions, we used detailed patient-level and hospital-level longitudinal data from a national sample of patients with STEMI admitted from 1999 to 2002 from the National Registry of Myocardial Infarction (NRMI) 3 and 4.8
Methods
Study design and sample
We used NRMI, a voluntary AMI registry sponsored by Genentech, Inc. (South San Francisco, CA), to obtain a cohort of patients with STEMI who received acute reperfusion therapy with either fibrinolytic therapy or primary PCI. The NRMI criteria9, 10 include a diagnosis of AMI according to the International Classification of Diseases, Ninth Revision, Clinical Modification (code 410.X1) and any one of the following criteria: total creatine kinase or creatine kinase MB that was 2 or more times the upper limit of the normal range or elevations in alternative cardiac markers; electrocardiographic evidence of AMI; or nuclear medicine testing, echocardiography, or autopsy evidence of AMI. During our study period of January 1, 1999 to December 31, 2002, there were 830,473 AMI admissions in NRMI. We excluded patients who had neither ST elevation (2+leads) nor left bundle branch block on the first electrocardiogram (ECG) (n=535,993); who were transferred from another acute care institution (n=72,756); whose AMI symptom onset was after the admit date and time (n=5,088); without chest pain in whom symptom onset time was not known (n=20,415); whose first ECG obtained was not the diagnostic ECG (the ECG with ST elevation or left bundle branch block; n=17,066); and those with time from symptom onset to diagnostic ECG that was negative, more than 6 hours, or missing (n=6,335).
From the 172,820 remaining patients, we analyzed fibrinolytic therapy and PCI separately. We assigned patients who received both therapies to the group based on the therapy they received first. From the patients who received fibrinolytic therapy (n=73,422), we excluded those with door-to-needle time that was negative, more than 6 hours, or missing (n=512); those who received fibrinolytic therapy after PCI (n=13); those in hospitals with fewer than 20 total patients (n=4,436); and those from the single NRMI hospital outside of the 50 states (n=22), leaving a final fibrinolytic therapy cohort of 68,439 patients from 1,015 hospitals. From the patients who received PCI (n=36,763), we excluded those with door-to-balloon time that was negative, more than 6 hours, or missing (n=891), those who received PCI after fibrinolytic therapy (n=507), and those in hospitals with fewer than 20 total patients (n=1,718), leaving a final PCI cohort of 33,647 patients from 421 hospitals.
Because NRMI is a voluntary registry, many hospitals did not participate consistently over the entire time period. Some hospitals started submitting data later than 1999, some stopped submitting data during the study period, and some intermittently submitted data. We repeated analyses using hospitals that reported at least 5 cases for each year of the study period (as opposed to the original cohort with hospitals that reported an average of at least 5 cases per year). The results from these smaller cohorts (for both fibrinolytic therapy and PCI) were not substantially different from those of the more inclusive cohorts. Thus, we present only the analyses using the larger cohort.
Data collection and measures
Our principal outcome was the time in minutes between hospital arrival and the delivery of reperfusion therapy, as noted in the medical record and recorded in the NRMI case report form. Calendar time was measured in elapsed time from the beginning of the study period.
Hospital characteristics included U.S. Census division; ownership (government, nonprofit, for-profit); cardiac facilities (open heart surgery, cardiac catheterization laboratory only, other); annual reperfusion volume (<20, 20-40, >40 for fibrinolytic therapy and <15, 15-50, >50 for PCI); and reperfusion specialization (percent of all reperfused STEMI patients in the hospital who received the given strategy). We classified hospitals based on urban (residence in a county with a population of at least 50,000) versus rural location and teaching status (i.e., participation in a residency or fellowship training program accredited by the Liaison Committee on Medical Education). Data for hospital characteristics were obtained from the American Hospital Association Annual Survey of Hospitals11 and the SMG data set (SMG Marketing Group, Inc., Chicago, IL).
Patient demographic and clinical covariates included sociodemographic variables (sex, age, race/ethnicity, and payer type); medical history (smoker, chronic renal insufficiency, previous AMI, hypertension, family history of coronary artery disease, hypercholesterolemia, congestive heart failure, previous percutaneous transluminal coronary angioplasty, previous coronary artery bypass graft surgery, chronic obstructive pulmonary disease, stroke, angina, diabetes); presentation characteristics (whether a pre-hospital ECG was performed, chest pain at presentation, systolic blood pressure, pulse, heart failure); the results of the diagnostic ECG (number of leads with ST-elevation, AMI location, ST depression, nonspecific ST/T-wave changes, Q-wave); the admission time of day (day, evening, or night); and admission day of week (weekday or weekend).
Statistical analysis
We reported the number of patients who were administered fibrinolytic therapy or PCI within the recommended time frame for each year of the study. We then examined differences in hospital performance (geometric mean time to reperfusion) and improvement (change over calendar time in geometric mean time to reperfusion) using multivariable hierarchical models.12 Hierarchical models were used to account for the non-independence of observations in this sample, in which patients were clustered within participating NRMI hospitals. In addition, hierarchical models allowed us to estimate variation in performance and improvement across hospitals by modeling both the intercept and calendar time as random effects. We identified hospital characteristics that were associated with greater improvement using cross-level interactions between calendar time and hospital characteristics.
To account for potential floor and ceiling effects (hospitals starting with very high or low treatment times having more or less opportunity to improve over time) and for regression to the mean,13 each model also included terms representing the interaction of calendar time with hospital baseline performance. Baseline performance was calculated as the median time to reperfusion of the first 10 cases reported in the study period for a given hospital. Time to reperfusion was treated as a continuous variable, and log transformation was used to correct for skewness.14 For easier interpretation, we transformed coefficients back into natural units using geometric means or simulation methods.15 Statistical analyses were performed using SAS versions 6.12 and 8.2 (SAS Inc., Cary, NC), Stata version 8.0 (Stata Corp., College Station, TX), and HLM version 5 (SSI, Lincolnwood, IL). The authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Results
Sample characteristics
The characteristics of the patients included in the fibrinolytic therapy cohort (n=68,439) and the PCI cohort (n=33,647) are displayed in Table 1. The cohorts were predominantly male and white, with a significant proportion of patients having a prior diagnosis of coronary artery disease and/or traditional cardiac risk factors. Over 93% had chest pain, 11% were in overt heart failure, and about 2% had left bundle branch block. The characteristics of the hospitals in the study are shown in Table 2. A greater proportion of hospitals in the fibrinolytic therapy cohort were rural teaching hospitals, whereas the PCI cohort included a greater proportion of urban teaching hospitals.
Table 1.
Description of the patient samples
| Fibrinolytic Therapy Cohort | PCI Cohort | |
|---|---|---|
| N | 68,439 | 33,647 |
| Mean(sd) or %(n) | Mean(sd) or %(n) | |
| Demographics | ||
| Age | 61.7 (13.0) | 61.8 (13.2) |
| Female | 30.5% (20,867) | 29.8% (10,027) |
| Race | ||
| White | 85.9% (58,790) | 85.4% (28,718) |
| Black | 4.9% (3,376) | 5.1% (1,703) |
| Hispanic | 3.5% (2,423) | 3.5% (1,178) |
| Other/Unknown | 5.6% (3,850) | 6.1% (2,048) |
| Medical history | ||
| Congestive heart failure | 4.0% (2,707) | 3.3% (1,103) |
| Hypertension | 47.8% (32,680) | 49.1% (16,525) |
| Diabetes | 19.5% (13,340) | 19.2% (6,464) |
| Smoker | 39.1% (26,753) | 38.2% (12,854) |
| Stroke | 3.4% (2,336) | 4.8% (1,610) |
| Percutaneous transluminal coronary angioplasty | 9.8% (6,696) | 14.5% (4,872) |
| Coronary artery bypass graft surgery | 6.5% (4,418) | 5.9% (1,991) |
| Chronic obstructive pulmonary disease | 8.2% (5,600) | 7.9% (2,671) |
| Hypercholesterolemia | 33.6% (22,978) | 37.5% (12,603) |
| Hormone replacement therapy | 2.8% (1,941) | 3.1% (1,037) |
| Chronic renal insufficiency | 2.1% (1,416) | 2.5% (847) |
| Coronary artery disease | 30.9% (21,140) | 28.7% (9,658) |
| Angina | 7.1% (4,861) | 8.0% (2,682) |
| Previous myocardial infarction | 16.3% (11,128) | 16.5% (5,535) |
| Presentation | ||
| Chest pressure | 95.0% (65,017) | 93.5% (31,473) |
| Heart failure | ||
| None | 89.2% (61,043) | 88.1% (29,636) |
| Rales/jugular venous distension | 7.4% (5,095) | 6.7% (2,251) |
| Pulmonary edema | 2.2% (1,512) | 2.0% (680) |
| Shock | 1.2% (789) | 3.2% (1,080) |
| ST elevation | ||
| Left bundle branch block | 2.0% (1,338) | 2.1% (696) |
| 2 leads | 10.6% (7,221) | 11.2% (3,777) |
| 3-4 leads | 67.2% (45,959) | 67.0% (22,554) |
| >4 leads | 18.8% (12,893) | 18.6% (6,274) |
| Anterior location | 32.6% (22,286) | 36.4% (12,237) |
PCI= percutaneous coronary intervention
Table 2.
Description of the hospital samples and time to reperfusion
| Fibrinolytic Therapy Hospitals | PCI Hospitals | |||||||
|---|---|---|---|---|---|---|---|---|
| Door-to-Needle Time |
Door-to-Balloon Time |
|||||||
| Characteristics | N=1,015 | Crude | Adjusted* | p | N=421 | Crude | Adjusted* | p |
| % | minutes | minutes | % | minutes | minutes | |||
| Geographic location | 0.060 | 0.001 | ||||||
| New England | 6.4 | 33.9 | 34.6 | 2.9 | 99.5 | 101.9 | ||
| Middle Atlantic | 12.2 | 35.2 | 35.4 | 5.2 | 106.8 | 107.9 | ||
| South Atlantic | 16.8 | 34.5 | 35.1 | 12.4 | 107.3 | 115.6 | ||
| East North Central | 18.1 | 32.7 | 33.6 | 20.2 | 105.8 | 106.0 | ||
| East South Central | 6.5 | 32.3 | 33.1 | 5.9 | 108.6 | 107.1 | ||
| West North Central | 6.9 | 31.9 | 32.9 | 11.6 | 96.1 | 101.7 | ||
| West South Central | 7.5 | 35.1 | 34.5 | 10.5 | 111.1 | 113.3 | ||
| Mountain | 6.3 | 31.2 | 32.5 | 9.0 | 107.5 | 108.7 | ||
| Pacific | 19.2 | 34.7 | 34.9 | 22.3 | 103.1 | 107.1 | ||
| Ownership | >.500 | >.500 | ||||||
| Public | 12.2 | 33.4 | 34.3 | 9.0 | 106.6 | 108.2 | ||
| Not-for-profit | 78.5 | 33.7 | 34.3 | 81.9 | 104.1 | 107.9 | ||
| Private | 9.3 | 33.9 | 34.1 | 9.0 | 109.5 | 108.0 | ||
| Teaching | <0.001 | 0.118 | ||||||
| Urban/teaching | 20.5 | 35.7 | 37.0 | 47.0 | 105.0 | 108.9 | ||
| Urban/nonteaching | 51.7 | 33.7 | 34.3 | 46.1 | 105.0 | 107.6 | ||
| Rural/teaching | 1.9 | 32.6 | 34.1 | 2.1 | 103.3 | 100.6 | ||
| Rural/nonteaching | 25.9 | 31.9 | 33.3 | 4.8 | 96.7 | 101.8 | ||
| Facilities | 0.362 | 0.040 | ||||||
| Open-heart surgery program | 31.8 | 35.0 | 35.0 | 91.9 | 105.2 | 108.4 | ||
| Cardiac catheterization lab only | 35.1 | 32.9 | 34.2 | 8.1 | 98.7 | 102.4 | ||
| Other | 33.1 | 33.2 | 33.6 | - | - | - | ||
| Annual volume | 0.004 | <0.001 | ||||||
| <20 LYS or <15 PCI | 25.9 | 34.9 | 35.9 | 15.4 | 114.2 | 112.6 | ||
| 20-40 LYS or 15-50 PCI | 44.9 | 33.7 | 34.8 | 72.2 | 107.2 | 110.4 | ||
| >40 LYS or >50 PCI | 29.2 | 33.3 | 33.4 | 12.4 | 97.2 | 101.6 | ||
| Reperfusion specialization † | 0.005 | 0.018 | ||||||
| %LYS or %PCI <20 | 0.3 | 52.9 | 49.3 | 3.1 | 120.1 | 110.0 | ||
| %LYS or %PCI 20-90 | 31.6 | 35.0 | 35.7 | 74.1 | 107.2 | 108.7 | ||
| %LYS or %PCI >90 | 68.1 | 33.0 | 33.6 | 22.8 | 98.6 | 99.3 | ||
Hierarchical model adjusted for both patient and hospital characteristics, and calendar time
Percent of total reperfused patients who had the reperfusion strategy (i.e., # PCI patients / total # reperfused)
LYS=fibrinolytic therapy; PCI=percutaneous coronary intervention
Guideline adherence
In 1999, 46% (11,107/24,024) of patients in the fibrinolytic therapy cohort were treated within 30 minutes, and 35% (3,104/8,798) of the patients in the PCI cohort were treated within 90 minutes, the recommended times16, 17 (Figures 1a and 1b). These proportions increased by 1% and 2%, respectively, over the next 3 years. In addition, the proportion of patients receiving fibrinolytic therapy after 40 minutes or PCI after 120 minutes did not change substantially.
Figures 1a and 1b:
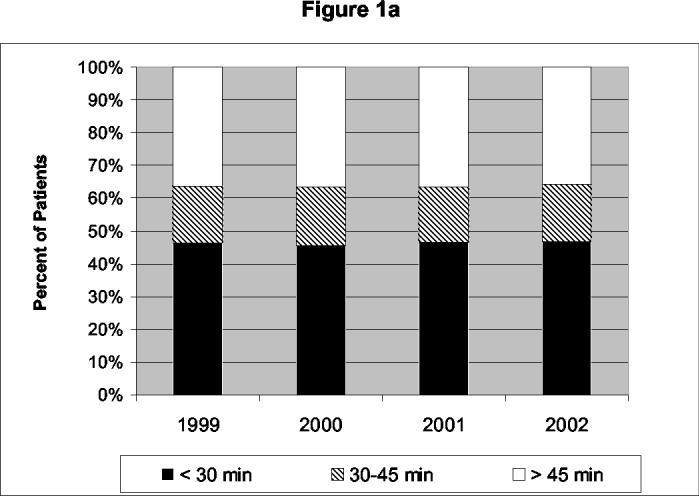
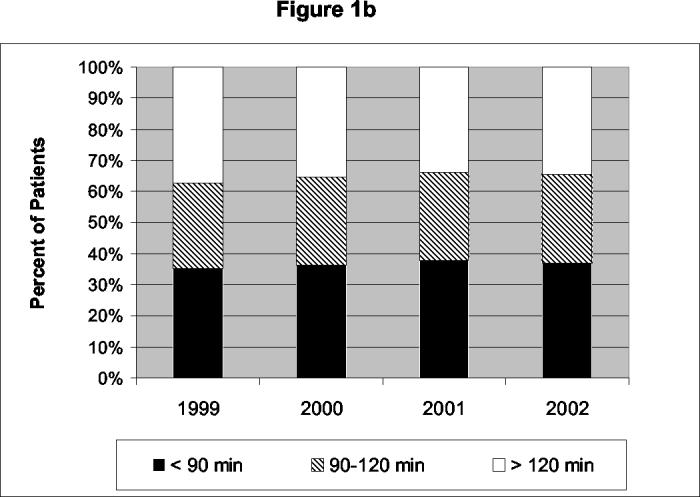
Guideline Adherence - Proportions of patients receiving either fibrinolytic therapy (Figure 1a) or PCI (Figure 1b) within the ACC/AHA recommended times17 are indicated in black. The proportions of additional patients receiving late reperfusion, defined as the recommended time plus one third (40 minutes for fibrinolytic therapy and 120 minutes for PCI) are indicated in white. The proportions of patients receiving reperfusion between these times are indicated in the diagonal pattern.
Hospital characteristics associated with performance
Using multivariable hierarchical modeling, the mean door-to-needle time over the study period, adjusted for both patient and hospital characteristics, was 34.3 minutes (95% Confidence Interval (CI) 33.9, 34.7). Several hospital characteristics were significantly associated with performance (Table 2). Door-to-needle times differed by geographic location, with best times in the West North Central (Minnesota, Iowa, Missouri, North Dakota, South Dakota, Nebraska, and Kansas) and Mountain (Montana, Idaho, Wyoming, Nevada, Utah, Colorado, Arizona, and New Mexico) divisions. Urban teaching hospitals had longer times than nonteaching hospitals or rural teaching hospitals. Hospitals with higher volumes and those with higher proportions of fibrinolytic therapy to total reperfusion therapy (reperfusion specialization) had modestly shorter times.
The adjusted mean door-to-balloon time over the study period was 108.0 minutes (95% CI 106.5 to 109.4). Volume and reperfusion specialization were associated with shorter door-to-balloon times. Hospitals in the West North Central and New England (Maine, New Hampshire, Vermont, Massachusetts, Rhode Island, and Connecticut) divisions averaged the best times for the PCI cohort. Teaching and rural/urban status were not significantly associated with door-to-balloon time. Hospitals without cardiac surgery facilities had shorter times than those with cardiac surgery facilities (108.4 minutes vs. 102.4 minutes). Hospital ownership status did not affect performance for either the fibrinolytic therapy or PCI cohort.
Improvement
The mean door-to-needle times for the fibrinolytic therapy cohort were stable over the 4-year time period, with a non-significant yearly improvement of 0.01 minutes (P>0.9). The decrease in door-to-balloon time for the PCI cohort also was not statistically significant (-0.57 minutes per year; p=0.09) (Figure 2).
Figure 2:
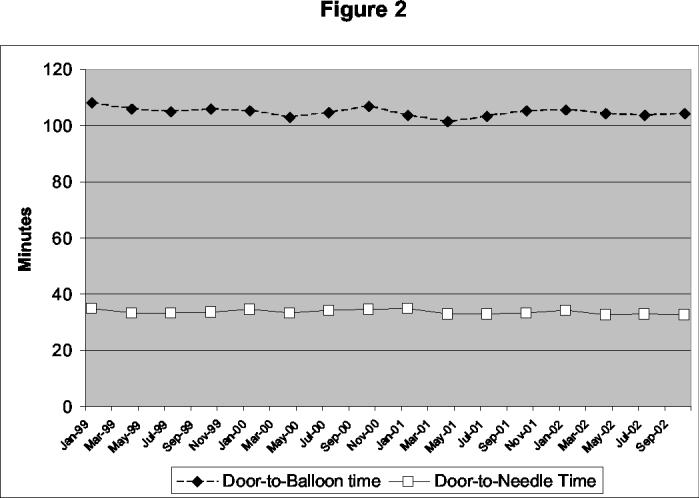
Calendar Time Trend - The geometric mean door-to-needle times for 68,439 patients (white squares) and geometric mean door-to-balloon times for 33,647 patients (black diamonds) for each month from January 1999 to December 2002. There was no significant trend for either door-to-needle times (p=0.956) or door-to-balloon times (p=0.094).
The change in mean time to reperfusion by hospital showed a wide distribution nearly centered on 0 for both cohorts (Figures 3a and 3b), with ranges of -5.7 minutes to +7.4 minutes for door-to-needle times and -12.9 minutes to +10.1 minutes for door-to-balloon times. Only 33% (337/1,015) of hospitals in the fibrinolytic therapy cohort improved more than 1 minute per year, and 26% (110/421) of PCI hospitals improved more than 3 minutes per year. Average door-to-needle and door-to-balloon times worsened by these amounts in 32% (325/1,015) and 18% (74/421) of hospitals, respectively.
Figures 3a and 3b:
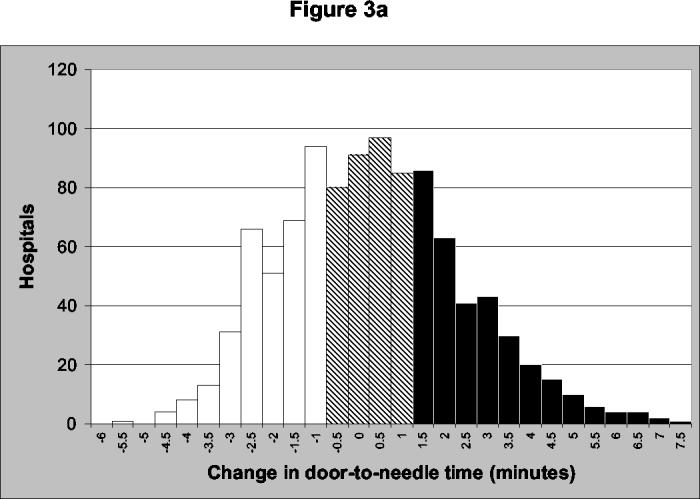
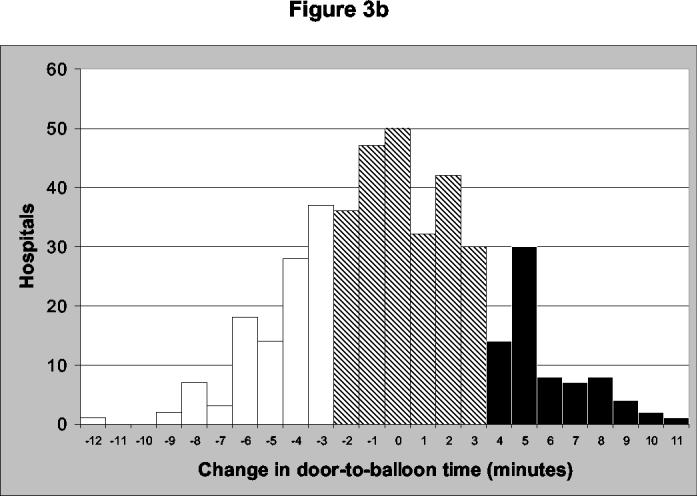
Distribution of Improvement - Improvement over the study period for each of the 1,015 hospitals reporting for fibrinolytic therapy (Figure 3a) and for each of the 421 hospitals reporting for PCI (Figure 3b). For illustration purposes, those hospitals that improved by an average of 1 minute for fibrinolytic therapy and 3 minutes for PCI are indicated in white; those hospitals that worsened by an average of 1 minute for fibrinolytic therapy and 3 minutes for PCI are indicated in black; and those hospitals in between these times are indicated in the diagonal pattern.
Hospital characteristics associated with improvement
No hospital characteristic significantly predicted improvement in door-to-needle time for the fibrinolytic therapy cohort (Table 3). Improvement in hospitals with a higher proportion of patients receiving fibrinolytic therapy (reperfusion specialization) nearly reached statistical significance (p=0.09). Although total fibrinolytic therapy volume predicted overall door-to-needle times, fibrinolytic therapy volume did not predict improvement over the study period.
Table 3.
Hospital characteristics and improvement*
| Fibrinolytic Therapy Cohort |
PCI Cohort |
|||
|---|---|---|---|---|
| minutes/year | p | minutes/year | p | |
| Average | −0.01 | 0.956 | −0.58 | 0.094 |
| Geographic location | >.500 | 0.046 | ||
| New England | 0.2 | −7.5 | ||
| Middle Atlantic | 0.2 | 0.8 | ||
| South Atlantic | 0.3 | −0.5 | ||
| East North Central | −0.3 | −0.5 | ||
| East South Central | 0.1 | −0.7 | ||
| West North Central | −0.5 | −1.6 | ||
| West South Central | 0.3 | 0.4 | ||
| Mountain | −0.2 | 1.1 | ||
| Pacific | 0.0 | −0.6 | ||
| Ownership | 0.152 | 0.329 | ||
| Public | −0.2 | 0.8 | ||
| Not-for-profit | −0.1 | −0.6 | ||
| Private | 0.8 | −1.6 | ||
| Teaching | >.500 | >.500 | ||
| Urban/teaching | 0.1 | −0.6 | ||
| Urban/nonteaching | 0.2 | −0.3 | ||
| Rural/teaching | 0.2 | −1.7 | ||
| Rural/nonteaching | −0.1 | −3.1 | ||
| Facilities | >.500 | 0.271 | ||
| Open-heart surgery program | 0.3 | −0.5 | ||
| Cardiac catheterization lab only | −0.2 | −1.9 | ||
| Other | −0.1 | − | ||
| Annual volume | >.500 | 0.016 | ||
| <20 LYS or <15 PCI | 0.1 | 1.0 | ||
| 20-40 LYS or 15-50 PCI | 0.0 | −0.1 | ||
| >40 LYS or >50 PCI | 0.0 | −1.9 | ||
| Reperfusion specialization | 0.086 | 0.294 | ||
| %LYS or %PCI <20% | 6.0 | −2.3 | ||
| %LYS or %PCI 20%-90% | 0.6 | −0.4 | ||
| %LYS or %PCI > 90% | −0.3 | −1.9 | ||
Adjusted for patient characteristics (from Table 1)
LYS=fibrinolytic therapy; PCI=percutaneous coronary intervention
In the PCI cohort, PCI volume significantly predicted improvement, with high volume hospitals (>50 PCI’s per year) showing improvement in mean door-to-balloon time (-1.9 minutes per year), medium volume hospitals (15-50 PCI’s per year) showing nearly no change in mean time (-0.1 minutes per year), and low volume hospitals (<15 PCI’s per year) showing an increase in time (+1.0 minutes per year, p=0.033). Thus, in addition to being associated with overall performance, PCI volume predicted improvement over the study period. Hospitals in New England showed the most improvement (-7.5 minutes per year). Proportion of PCI’s to total reperfusion therapy (reperfusion specialization) did not predict improvement in door-to-balloon time.
Discussion
Despite strong evidence that decreased time to reperfusion for patients with STEMI is related to improved morbidity and mortality, we found that fewer than half of these patients received reperfusion therapy within the recommended time in any year from 1999-2002. Furthermore, we found little evidence of substantial improvement in time to reperfusion over these years. Although the entire cohorts did not improve, the analysis of the individual hospitals demonstrated a notable hospital-level variation in change from 1999 to 2002. Some hospitals showed substantial improvement while others’ performance worsened. Traditional hospital characteristics generally were not good predictors of improvement, indicating a need to identify other, perhaps more subtle, reasons why some hospitals improve.
Our results extend the work on earlier trends in time to fibrinolytic therapy. In an earlier study of the NRMI database, the median door-to-needle time was shown to decrease from 62 minutes to 47 minutes from 1990 to 1994, with a subsequent decrease to 38 minutes by 1999.7 This slowing of improvement over time is consistent with the lack of change in door-to-needle times we found from 1999 to 2002. In a review of care given to Medicare beneficiaries, a state-by-state comparison found the door-to-needle time in the median state increased by 4 minutes between 1998-1999 and 2000-2001.18 In this same time period, the door-to-balloon time in the median state decreased by 19 minutes. However, the power of this study to address the specific question of time to reperfusion was limited; the median state contributed only 17 patients to the number of patients for the fibrinolytic therapy group and 6 to the PCI group.19 The size of the cohorts in our study and the focus only on time to reperfusion enabled us to determine more precise estimates and to investigate potential hospital-level predictors of improvement.
Previous studies demonstrated that hospital volume predicts lower door-to-needle1 and door-to-balloon times.20 In addition to confirming these results for performance, we further demonstrated the association of higher number of procedures with improvement in door-to-balloon times. Thus, hospitals performing greater than 50 PCI’s per year not only started out with better times but managed to improve even more over the 4 years. In comparison, higher volume fibrinolytic therapy hospitals did not improve more over the 4-year study period than lower volume hospitals. The difference in complexity between fibrinolytic therapy and PCI may account for these disparate results. The PCI strategy, with involvement of the interventional cardiologist and the cardiac catheterization laboratory in addition to the emergency department, is inherently a more complex process than the fibrinolytic strategy. A complex process such as PCI may benefit from more frequent use to identify more opportunities to improve. Also, in contrast to the greater than 2-decade experience with the fibrinolytic strategy, the PCI strategy has only recently been widely adopted.7 More improvement is likely seen early after introduction of a new strategy than after one has become established.
Hospitals that predominantly treated patients with one strategy (>90% of the time) had better performance for either fibrinolytic therapy or PCI than those hospitals that had a more balanced profile. One explanation could be that there is a time delay associated with the decision of whether to administer fibrinolytic therapy or perform PCI. Interestingly, improvement over the 4 years was not statistically greater in these hospitals with a predominant strategy compared with the balanced hospitals. More investigation into the relationship between the strategies may provide valuable insights.
Our findings suggest that factors other than traditional hospital characteristics are largely responsible for improvement in door-to-reperfusion times seen in some hospitals. These findings may not be surprising in that management of AMI involves many individuals, including nurses, physicians, technologists, and paramedics from different areas of the hospital, such as the emergency medical system, the emergency department, and cardiology. In this setting, achieving rapid reperfusion likely requires multifaceted, coordinated efforts at quality improvement specific to the institution. Qualitative approaches such as structured interviews and site visits may supplement quantitative outcome analysis by supplying in-depth insight into the complex processes of care.
One potential explanation for a lack of significant improvement in our analysis would be a “floor effect” - that no further improvement is possible. Although the low rates of guideline adherence would suggest ample potential room for improvement for most hospitals, we included the mean of the first 10 cases for each hospital as a baseline covariate in the model to account for this possibility and for potential regression to the mean. Even adjusting for baseline performance, many hospitals showed substantial improvement. Thus, a “floor effect” is not likely significantly limiting opportunities for improvement. In-depth qualitative investigation into hospitals with the best performance revealed valuable strategies common to many of them.21 These qualitative studies that identify optimal performance and disseminate those strategies that have proven positive outcomes complement the current analysis that identifies what is being done in actual practice.
While NRMI is a large database of more than 1 million patients with AMI, certain issues are important to consider in interpreting our results. First, the database is voluntary and may not be representative of all patients presenting with STEMI. Second, the membership of the cohort was not constant. Some hospitals started enrolling in NRMI during the study period, others stopped. However, the results from a smaller cohort of patients from the hospitals that consistently participated throughout the study period were similar. Third, the NRMI database may contain some patients for whom there were legitimate delays in time to reperfusion. In order to decrease the effect of extreme delays on our results, we only evaluated patients treated with reperfusion therapy within 6 hours and used geometric mean times. Finally, we evaluated the hospital characteristics most frequently shown to be associated with performance, but other unmeasured structural characteristics may exist that predict improvement.
In conclusion, the significant improvement in overall door-to-needle times seen in the 1990’s appears to have ended. Despite national initiatives to measure and reduce these times, guideline recommendations were met less than half of the time, with no substantial trend toward improvement. Nevertheless, some individual hospitals experienced substantial improvement while others worsened. Structural features of hospitals such as volume and teaching status do not adequately predict change in performance. Other factors that are related to improvement, such as organizational culture, physician leadership, interrelationship between cardiology and emergency physicians and staff, emergency medical systems, and administrative support need to be identified and used by hospitals for performance improvement programs to decrease door-to-needle and door-to-balloon times and decrease mortality from STEMI.
Acknowledgment
This research was supported by the National Heart, Lung, and Blood Institute (NHLBI), R01HS10407-01. The NHLBI did not play a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
This research was supported by the National Heart, Lung, and Blood Institute, R01HS10407-01. The authors do not have conflicts of interest to disclose in relation to this work.
- ACC/AHA
- American College of Cardiology/American Heart Association
- AMI
- acute myocardial infarction
- CI
- confidence interval
- ECG
- electrocardiogram
- LYS (used in Tables 2 and 3)
- fibrinolytic therapy
- NRMI
- National Registry of Myocardial Infarction
- PCI
- percutaneous coronary intervention
- STEMI
- ST-segment elevation myocardial infarction
References
- 1.Berger AK, Radford MJ, Krumholz HM. Factors associated with delay in reperfusion therapy in elderly patients with acute myocardial infarction: analysis of the Cooperative Cardiovascular Project. Am Heart J. 2000;139:985–992. doi: 10.1067/mhj.2000.105703. [DOI] [PubMed] [Google Scholar]
- 2.Cannon CP, Gibson CM, Lambrew C, et al. Longer thrombolysis door-to-needle times are associated with increased mortality in acute myocardial infarction: an analysis of 85,589 patients in the National Registry of Myocardial Infarction 2 + 3. J Am Coll Cardiol. 2000;35:376A. [Google Scholar]
- 3.Berger PB, Ellis SG, Holmes DR, Jr., et al. Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the Global Use of Strategies to Open Occluded Arteries in Acute Coronary Syndromes (GUSTO-IIb) trial. Circulation. 1999;100:14–20. doi: 10.1161/01.cir.100.1.14. [DOI] [PubMed] [Google Scholar]
- 4.Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–2947. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 5.DeLuca G, Suryapranata H, Ottervanger JP, et al. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 6.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) Circulation. 2004;110:e82–e92. [PubMed] [Google Scholar]
- 7.Rogers W, Canto J, Lambrew C, et al. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;36:2056–2063. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 8.French WJ.Trends in acute myocardial infarction management: use of the National Registry of Myocardial Infarction in quality improvement Am J Cardiol 2000855B–9B.discussion 10B-12B [DOI] [PubMed] [Google Scholar]
- 9.Every NR, Frederick PD, Robinson M, et al. A comparison of the National Registry of Myocardial Infarction 2 with the Cooperative Cardiovascular Project. J Am Coll Cardiol. 1999;33:1886–1894. doi: 10.1016/s0735-1097(99)00113-8. [DOI] [PubMed] [Google Scholar]
- 10.Rogers WJ, Bowlby LJ, Chandra NC, et al. Treatment of myocardial infarction in the United States (1990 to 1993). Observations from the National Registry of Myocardial Infarction. Circulation. 1994;90:2103–2114. doi: 10.1161/01.cir.90.4.2103. [DOI] [PubMed] [Google Scholar]
- 11.American Hospital Association . The annual survey of hospitals database: documentation for 1998 data. American Hospital Association; Chicago: 1998. [Google Scholar]
- 12.Goldstein H. Multilevel Statistical Models. Edward Arnold; Wiley; London: New York: 1995. [Google Scholar]
- 13.Mayer-Davis EJ, Kirkner GJ, Karter AJ, et al. Metabolic predictors of 5-year change in weight and waist circumference in a triethnic population: the insulin resistance atherosclerosis study. Am J Epidemiol. 2003;157:592–601. doi: 10.1093/aje/kwg022. [DOI] [PubMed] [Google Scholar]
- 14.Bland JM, Altman DG. Transformations, means, and confidence intervals. BMJ. 1996;312:1079. doi: 10.1136/bmj.312.7038.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.King G, Tomz M, Wittenberg J. Making the most of statistical analyses: improving interpretation and presentation. Am J Pol Sci. 1998;44:341–355. [Google Scholar]
- 16.Ryan TJ, Anderson JL, Antman EM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) J Am Coll Cardiol. 1996;28:1328–1428. doi: 10.1016/s0735-1097(96)00392-0. [DOI] [PubMed] [Google Scholar]
- 17.Ryan TJ, Antman EM, Brooks NH, et al. 1999 update: ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) J Am Coll Cardiol. 1999;34:890–911. doi: 10.1016/s0735-1097(99)00351-4. [DOI] [PubMed] [Google Scholar]
- 18.Jencks SF, Huff ED, Cuerdon T. Change in the quality of care delivered to Medicare beneficiaries, 1998-1999 to 2000-2001. JAMA. 2003;289:305–312. doi: 10.1001/jama.289.3.305. [DOI] [PubMed] [Google Scholar]
- 19.Jencks SF, Cuerdon T, Burwen DR, et al. Quality of medical care delivered to Medicare beneficiaries: a profile at state and national levels. JAMA. 2000;284:1670–1676. doi: 10.1001/jama.284.13.1670. [DOI] [PubMed] [Google Scholar]
- 20.Angeja BG, Gibson CM, Chin R, et al. Predictors of door-to-balloon delay in primary angioplasty. Am J Cardiol. 2002;89:1156–1161. doi: 10.1016/s0002-9149(02)02296-8. [DOI] [PubMed] [Google Scholar]
- 21.Bradley EH, Roumanis SA, Radford MJ, et al. Achieving door-to-balloon times that meet quality guidelines: how do successful hospitals do it? J Am Coll CardiolIn Press [DOI] [PubMed] [Google Scholar]


