Abstract
Various organic and aqueous extracts of leaves of Indigofera suffruticosa Mill (Fabaceae) obtained by infusion and maceration were screened for their antibacterial and antifungal activities. The extracts were tested against 5 different species of human pathogenic bacteria and 17 fungal strains by the agar-solid diffusion method. Most of the extracts were devoid of antifungal and antibacterial activities, except the aqueous extract of leaves of I. suffruticosa obtained by infusion, which showed strong inhibitory activity against the Gram-positive bacteria Staphylococcus aureus with a minimal inhibitory concentration (MIC) of 5000 µg ml−1. The MIC values to dermatophyte strains were 2500 µg ml−1 against Trichophyton rubrum (LM-09, LM-13) and Microsporum canis. This study suggests that aqueous extracts of leaves of I. suffruticosa obtained by infusion can be used in the treatment of skin diseases caused by dermatophytes.
Keywords: antibacterial activity, antifungal activity, aqueous extract, Indigofera suffruticosa
Introduction
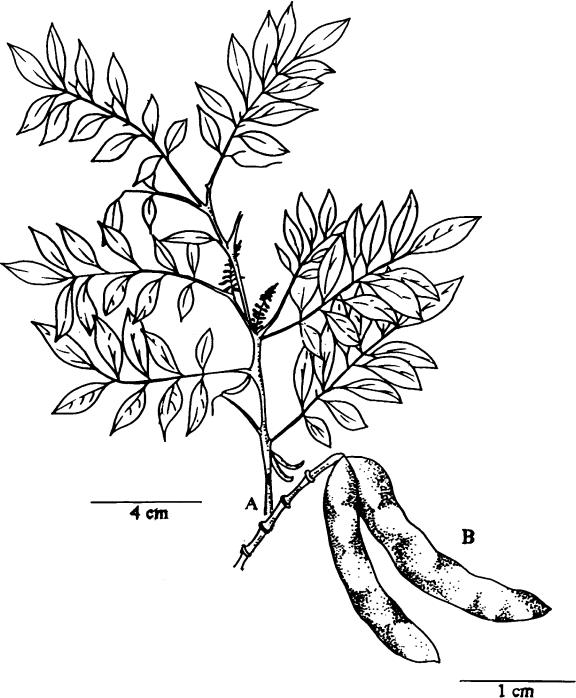
Plants are invaluable sources of pharmaceutical products (1) and Brazil, in particular, has yielded an incredible array of plant and animal products (2,3) that have drawn the attention of ethnopharmacologists from around the world. Many products, such as the one described in this paper, have traditional uses that are now being investigated to create an evidence base that will facilitate their inclusion in general medical practice. Belonging to the Fabaceae species, the I. suffruticosa Mill (Fig. 1) has been used as an infusion or decoction (flavor extract by boiling 1 l of hot water per 5 g of leaves) (4). This plant is found in tropical and subtropical areas and is well adapted to growth in semi-arid regions and soils of low fertility (5–7). It occurs in the northeast countryside of Brazil and has intensive popular use in the treatment of inflammations (8,9) and other diseases such as epilepsy in humans (10) and in animal models (11–13). Recently, embryotoxic effects have been reported (14). A chemical investigation of extracts of leaves of I. suffruticosa in Natural Products Alert (NAPRALERT) (15) and Chemical Abstracts databases has revealed the presence of alkaloids, flavanoids, steroids, proteins, carbohydrates and indigo. Herbal folk medicines provide an interesting and still largely unexplored source for drug development with potential chemotherapeutic benefits.
Figure 1.
Indigofera suffruticosa Mill. (A) Aspect of blossomed branch. (B) Aspect of branch with seeds. (Erilze da Silvas).
However, up to date, little research has been done to investigate this traditionally used plant. Although numerous studies have been carried out using natural extract products for screening antimicrobial activity (16,17), no attention was given to I. suffruticosa antimicrobial activity.
We report here our findings on some antibacterial and antifungal effects of various organic and aqueous extracts from leaves of I. suffruticosa obtained by infusion and maceration against a wide range of pathogenic bacteria and dermatophyte strains.
Materials and Methods
Plant Material
Leaves of I. suffruticosa were collected in June 2000 in São Caetano, State of Pernambuco, Brazil and authenticated by biologist Marlene Barbosa from the Department of Botany, Universidade Federal de Pernambuco (UFPE). A voucher specimen number 32 859 has been deposited at the herbarium of the above-cited department.
Preparation of Extracts
Two extracts were obtained by infusion and maceration from 150 g of the plant material. The material was weighed; chopped and extracted with solvents and water. The infusion was prepared with 75 g of fresh leaves in 2 × 200 ml of increasing polarity solvents (hexane, ethyl acetate and methanol) at 40°C for 10 min and removing solid matter by filtration. After this preliminary step, the same plant material was extracted in boiling distilled water at the same conditions, and the maceration was obtained following the aforementioned process at room temperature (28°C) overnight. The solvents were removed by rotary evaporation. The yields (w/w) of the infusion and the maceration were, respectively, hexane (0.67 and 0.74%), ethyl acetate (0.39 and 0.34%) and methanol (3.90 and 1.88%) in terms of newly collected plant material. After lyophilization the aqueous extract yielded 4.20 and 1.75% and the dried material was stored at −20°C (18,19).
Preliminary Phytochemical Analysis
The aqueous, methanolic, hexane and ethyl acetate extracts of leaves of I. suffruticosa obtained by infusion were analyzed by qualitative method (thin layer chromatography on silica gel/UV detection at 365 nm) for presence of alkaloids, iridoids, saponins, carbohydrates, coumarins, flavonoids, phenol, terpenoides, indigo and sterol (20–22). Lectin activity was obtained from aqueous extracts of leaves of I. suffruticosa by infusion (23).
Antimicrobial Assays
Microorganisms Tested
Strains of human pathogen microorganisms used in this study were as follows. Three Gram-negative bacteria, Klebsiella pneumoniae (LM-49), Pseudomonas aeruginosa (LM-B6) and Escherichia coli (LM-209); two Gram-positive bacteria, Staphylococcus aureus (ATTCC-6538) and Staphylococcus epidermidis (ATCC-12228); 17 yeasts of fungi including 9 potentially pathogenic yeasts, Candida albicans (ATCC-76615, ICB-12, FCF-243), Cryptococcus neoformans (FFCF-19), Cryptococcus guillermondii (LM-1), Cryptococcus krusei (FCF-1161), Cryptococcus stellatoidea (LM-19), Cryptococcus parapsilosis (CM-1), Trichosporon inkin (LM-267), and 8 filamentous fungi, Trichophyton rubrum (M-09, LM-13), Trichophyton mentagrophytes (LM-16), Microsporum canis (LM-828), Aspergillus flavus (LM-127), Penicillium sp (LM-131), Geotrichum candidum (LM-23) and Fusarium sp (LM-135). The microorganisms were originally obtained from the Mycology Laboratory of the Department of Pharmaceutical Science at Universidade de São Paulo (USP), Universidade Federal da Paraíba (UFPB) and Adolfo Lutz Institute in São Paulo, Brazil.
Antimicrobial Testing
Antimicrobial activity of the various organic and aqueous extracts from leaves of I. suffruticosa obtained by infusion and maceration was determined by the agar-solid diffusion method (24–28). Bacteria strains were cultured overnight at 37°C in Müller–Hinton agar, the filamentous and leveduriform yeasts in Sabouraud dextrose agar at 25°C overnight and at room temperature for a period of 14 days. The agar-solid diffusion method was used to determine antibacterial and antifungal activities. The extracts, in concentrations of 10 000 and 625 ug ml−1, were dissolved in dimethylsulfoxide (DMSO) for a final concentration of 4%.
Agar-solid Diffusion Method
Suspension of microorganisms (1 ml) with an optical density of McFarland 0.5 was prepared in physiological saline solution (0.9%) and it was adjusted to 90% of transmittance (530 nm) in a spectrophotometer. The antimicrobial spectrum of the extracts was determined qualitatively for the bacterial and fungal species in terms of zone sizes around wheels, cut in plates of agar Sabouraud and Müller–Hilton (supplemented as necessary) surface-inoculate with approximately 106 CFU of various microbial species containing 50 µl of the tested material dissolved in DMSO (equivalent to 5 mg of the dried extracts). The agar was melted (50°C) and the microorganism cultures were then added aseptically to the agar medium at 45°C in plates and poured into sterile Petri dishes to give a solid plate. All these experiments were performed in duplicate. The plates were incubated for 24–48 h, at 37°C for bacteria, and 10–14 days, at 30°C for filamentous fungi.
The inhibition zones produced by the plant extracts were compared with the inhibition zones produced by commercial standard antibiotics: chloramphenicol (30 µg) for bacteria, and ketoconazole (1000 µg) for fungi. They were used as positive control and the solvent DMSO as negative control.
The minimal inhibitory concentration (MIC) was applied to the aqueous extract that had proved to be highly effective against microorganisms by the agar- diffusion method. The aqueous extract of I. suffruticosa obtained by infusion (50 µl) was diluted in DMSO with decreasing concentrations (from 10 000 to 625 µg ml−1). The strains were designated arbitrarily as sensitive or resistant and the zones were measured at the end of the incubation time. An inhibition zone of 10 mm or greater was considered to indicate good antibacterial and antifungal activities.
Results
Preliminary Phytochemical Analysis
The results of our assay on the aqueous, methanolic, hexane and ethyl acetate extracts of leaves of I. suffruticosa obtained by infusion are shown in Table 1. The aqueous extract showed the presence of carbohydrates, glycoproteins, cinnamic derivatives, iridoids, leococyanidines and lectin activity but it was negative for alkaloids, flavanoids and coumarins. Alkaloids, sterols, triterpenes, indigo, flavanoids, carbohydrates, coumarins were detected in methanolic extract and it did not show the presence of iridoids and saponins. The hexane and ethyl acetate extracts showed the presence of β sitosterol, β amilina, triterpenes, sterols and azulene derivatives and they were negative for alkaloids, polar flavonoids, cinnamic derivatives, coumarins and phenylpropanoid glycosides.
Table 1.
Phytochemical screening of extract of leaves of I. suffruticosa by infusion
| Tested material | Yield (%) | Positive tests for | Negative tests for |
|---|---|---|---|
| Aqueous extract | 4.20 | Lectin, carbohydrates, glycoproteins, cinnamic derivatives, iridoids and leococyanidines | Alkaloids, flavanoids and coumarins |
| Methanolic extract | 3.90 | Alkaloids, sterols, triterpenes, indigo, flavanoids, carbohydrates and coumarins | Iridoids and saponins |
| Hexane extract | 0.67 | β sitosterol, β amilina, triterpenes, sterols and azulene derivatives | Alkaloids, polar flavanoids, cinnamic derivatives, coumarins and phenylpropanoid glycosides |
| Ethyl acetate extract | 0.39 | β sitosterol, β amilina, triterpenes, sterols and azulene derivatives | Alkaloids, polar flavonoids, cinnamic derivatives coumarins and phenylpropanoid glycosides |
Antimicrobial Activity of Extracts of I. suffruticosa Leaves
The aqueous, methanolic, hexane and ethyl acetate extracts of I. suffruticosa leaves obtained by infusion and maceration in a concentration of 10 000 µg ml−1 were tested against 22 microorganisms (bacterial and fungal) by means of agar-solid diffusion method. From those extracts, only the aqueous obtained by infusion showed variable degrees of antibacterial and antifungal activities against one or more of the tested organisms. The aqueous extract of leaves of I. suffruticosa obtained by infusion exhibited results against S. aureus, T. rubrum (LM-09, LM-13) and M. canis, whereas the organic extracts showed no activity. An inhibition zone of 10 or greater was considered as good antimicrobial activity. The aqueous and the organic extracts by maceration did not show any effect against both Gram-negative and Gram-positive bacteria and fungi. The solvents used, as control exerted no effect against the microorganisms in broth medium.
The inhibitory bacterial and fungal growth by extract, indicated by their MIC values, is summarized in Table 2. The aqueous extract of leaves of I. suffruticosa obtained by infusion provided activity against S. aureus in a concentration of 5000 µg ml−1 with an inhibition zone of 10 mm. The T. rubrum (LM-13, LM-9) showed an activity more significant in a concentration of 2500 µg ml−1 with an inhibition zone from 12 to 14 mm, respectively, and M. canis at the same concentration with an inhibition zone of 12 mm.
Table 2.
Values of inhibition zone in (mm) by MIC evaluation of aqueous extracts of leaves of I. suffruticosa obtained by infusion against bacterial and fungal activities
| Microorganisms | Aqueous extract (µg ml−1) | Microorganism growth without antimicrobians | Controls | |||||
|---|---|---|---|---|---|---|---|---|
| 10 000 | 5000 | 2500 | 1250 | 625 | Chloramphenicol (30 µg) | ketoconazol (1000 µg) | ||
| Staphylococcus aureus | 12 | 10 | 7 | 0 | 0 | + | 20 | 0 |
| Trichophyton rubrum (LM-09) | 20 | 17 | 14 | 10 | 7 | + | 0 | 20 |
| T. rubrum (LM-13) | 18 | 15 | 12 | 8 | 0 | + | 0 | 20 |
| Microsporum canis | 17 | 15 | 12 | 8 | 0 | + | 0 | 20 |
Discussion and Conclusions
Recently, much attention has been directed toward extracts and biologically active compounds isolated from popular plant species. The use of medicinal plants plays a vital role in covering the basic health needs in developing countries, and these plants may offer a new source of antibacterial, antifungal and antiviral agents with significant activity against infective microorganisms (29,30).
Results from our phytochemical analysis in methanolic (alkaloids, sterols, triterpenes, indigo, flavanoids, carbohydrates and coumarins), hexane and ethyl acetate extracts (β sitosterol, β amilina, triterpenes, sterols and azulene derivatives) obtained by infusion revealed no antimicrobial effects. However, the aqueous extract obtained by infusion (lectin, carbohydrates, glycoproteins, cinnamic derivatives, iridoids and leococyanidines) showed the presence of biologically active compounds, correlated to known substance that possess antimicrobial properties (31–34). Studies done with I. linnaei identified the amino acid indospicine as a natural toxic product (35). This observation provides strong circumstantial evidence that small protein/peptide plays an important role in a plant's antimicrobial defense system (36). The protein or peptide fractions from leaves of I. oblongifolia were reported (33). Biologically, activity detected in the aqueous extract of leaves of I. suffruticosa by infusion could be linked to lectins (23).
The aqueous and organic extracts of leaves of I. suffruticosa showed different activities against 22 microorganisms (bacterial and fungal). The aqueous extract of I. suffruticosa leaves by infusion showed an activity more significant on dermatophyte T. rubrum (LM-09, LM-13) and M. canis. The aqueous extract of I. suffruticosa obtained by infusion provided a zone of inhibition of 10 mm diameter (mm d−1) for S. aureus and a zone of inhibition of 14 mm d−1 and 12 mm d−1 for T. rubrum (LM-09, LM-13) and of 12 mm d−1 for M. canis (filamentous fungal).
Our results concerning the aqueous extract of I. suffruticosa obtained by infusion corroborate those of Dahot (33) who showed that the aqueous extract of I. oblongifolia leaves has significant antimicrobial activity against both Gram-positive and Gram-negative bacteria and fungal species. Ethanolic extracts of the same species have been mentioned in the literature for their antibacterial activity on S. aureus and P. aeruginosa and antifungal activity on Enterococcus faecalis, E. coli (37).
Reports showed that the aqueous extract of I. dendroides has significant antimicrobial activity against the Gram-positive bacterial (S. aureus, Bacillus subtilis), Gram-negative bacterial (K. Pneumoniae, E. coli) and fungal species (Aspergillus niger, C. albicans). (32).
The literature indicates that the antibacterial activity is due to different chemical agents in the extract, including essential oils (especially thymol), flavonoids and triterpenoids and other nature phenolic compounds or free hydroxyl groups. These are classified as active antimicrobial compounds (38).
Many plant extracts have been used as a source of medicinal agents to cure urinary tract infections, cervicitis vaginitis, gastrointestinal disorders, respiratory diseases, cutaneous affections, helmintic infections, parasitic protozoan diseases and inflammatory process (9,39–43). Elisabetsky has recently stressed that alstonine, a unique indole alkaloid is an example of richness of medicinal plants and traditional medical systems in the discovery of new prototypic drug (44).
From this study we can conclude that the traditional use of this plant for the treatment of infectious diseases is promising, mainly against bacteria and fungi. Purification of the bioactive component(s) from the extracts is underway and further investigations may improve our understanding of possible antimicrobial and antifungal activities.
Acknowledgments
We wish to express our appreciation and thanks to Dr Edeltrudes de Oliveira Lima (UFPB, Brazil) for providing us with the microorganisms and Dr Haroudo Satiro Xavier (UFPE, Brazil) for the partial support of this work. We are also grateful to CNPq for its financial support.
References
- 1.Olalde Rangel JA. The systemic theory of living systems and relevance to CAM. Part I: the theory. Evid Based Complement Alternat Med. 2005;2:13–18. doi: 10.1093/ecam/neh068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Teixeira EW, Negri G, Meira RM, Message D, Salatino A. Plant origin of green propolis: bee behavior, plant anatomy and chemistry. Evid Based Complement Alternat Med. 2005;2:85–92. doi: 10.1093/ecam/neh055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salatino A, Teixeira EW, Negri G, Message D. Origin and chemical variation of Brazilian Propolis. Evid Based Complement Alternat Med. 2005;2:33–38. doi: 10.1093/ecam/neh060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matos FJA. Plantas da Medicina Popular do Nordeste: Propriedades Atribuídas e Confirmadas. Editora UFC: Fortaleza, Brazil; 1999. [Google Scholar]
- 5.Pio Correia M. Dicionário de Plantas Úteis no Brasil e das Exóticas Cultivadas. Vol.1. Imprensa Nacional: Rio de Janeiro, Brazil; 1926. [Google Scholar]
- 6.Braga R. Plantas do Nordeste Especialmente do Ceara, 3a edição, Escola Superior de Agricultura. Rio Grande do Norte: Mossoró, Brazil; 1976. [Google Scholar]
- 7.Paiva MAS, Barbosa ACD, Alves HLJ. Indigofera suffruticosa Mill (Leguminosae) com potencial forrageiro em uma região de Caatinga no Semi-árido de Pernambuco. (Alagoinha). Proceedings of the XXXVIII Congresso Nacional de Botânica; São Paulo, Brazil: Sociedade Nacional de Botânica; 1987. p. 422. [Google Scholar]
- 8.Bhaskar AE, Ganga N, Arivudaimbi R, Santhanum G. Anti-inflammatory, analgesic activities of Indigofera aspalthoides. Indian J Med. 1982;76:115–16. [PubMed] [Google Scholar]
- 9.Leite SP, Silva LLS, Catanho MTJA, Lima EO, Lima VLM. Anti-inflammatory activity of Indigofera suffruticosa extract. REBRASA. 2003;7:47–52. [Google Scholar]
- 10.Roig T, Mesa JT. Plantas Medicinales Arómaticas y Venenosas de Cuba. La Habana Cuba: Editorial Ciencia y Técnica Instituto del Libro; 1974. pp. 315–16. [Google Scholar]
- 11.Wong BM, Rodríguez SN, Alejo PLJ, Perez FM. Actividad de la Indigofera suffruticosa Mill en la epilepsia crónica experimental y su relación con aminoácidos neurotransmissores. Rev Cubana Plant Med. 1999;1:18–21. [Google Scholar]
- 12.Pérez de Alejo J, Miranda R, Rodrigues G. Actividad Anticonvulsivante (Antiepileptica) del extracto fluido de Indigofera suffruticosa (Anil Cimarrón) Ver Cubana Plant Méd. 1996;1:7–10. [Google Scholar]
- 13.Mc Namara JO. Role of neurotransmitter in seizure mechanism in the kindled model of epilepsy. Fed Proc. 1984;43:2516–20. [PubMed] [Google Scholar]
- 14.Leite SP, Lys PM, Silva EC, Maia MBS, Lima VLM, Saul DE. Embryotoxicity in vitro with extract of Indigofera suffruticosa leaves. Reproductive Toxicol. 2004;18:701–5. doi: 10.1016/j.reprotox.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 15. NAPRALERT—Natural Products Alert, Illinois University, Chicago. 2003. Accessed at http://www.uic.edu/phamacy/depts/PCRPS/NAPRALERT.htm.
- 16.Ngono Ngane A, Biyiti L, Amvam Zollo PH, Bouchet Ph. Evaluation of antifungal activity of extracts of two Cameroonian Rutaceae; Zanthoxylum leprierurii Guill. et Perr, and Zanthoxylum xantholoides Waterm. J Ethonopharmacol. 2000;70:335–42. doi: 10.1016/s0378-8741(99)00188-9. [DOI] [PubMed] [Google Scholar]
- 17.Ramesh N, Viswanathan MB, Saraswathy A, Balakrishna K, Brindha PL. Phytochemical and antimicrobial studies of Begonia malabarica. J Ethonopharmacol. 2002;79:129–32. doi: 10.1016/s0378-8741(01)00352-x. [DOI] [PubMed] [Google Scholar]
- 18.McCloud T, Nemec J, Muschik G, Sheffield H, Quesenberry P, Suffness M, et al. Extraction of bioactive molecules from plants. Proceedings of the International Congress on Natural Products Research; 1988. pp. 17–21. Park City, UT. [Google Scholar]
- 19.Leite PS. João Pessoa, Paraíba, Brazil: Tese de Doutorado da Universidade Federal da Paraíba; 2003. Indigofera suffruticosa Mill: Ensaio Fitoquímico e Ações Biológicas. [Google Scholar]
- 20.Markhan KR. London: Academic Press; 1982. Techniques of Flavonoid Identification; pp. 52–61. [Google Scholar]
- 21.Harborne JB. London: Chapman & Hall; 1998. Phytochemical Methods; pp. 1–302. [Google Scholar]
- 22.Wagner H, Bladt S, Zgainski EM. Berlin: Springer-Verlag; 1984. Drogenanalyse; p. 164. [Google Scholar]
- 23.Leite SP, Leite ACR, Paiva PMG, Coelho LCBB, Lima EO, Lima VLM. Atividade Lectínica em folhas de Indigofera suffruticosa VI Reunião Regional da SBBq, Nordeste, Fortaleza Ceará Resumo Completo. 2002 [Google Scholar]
- 24.Casals JB. Tablet sensitivity testing of pathogenic fungi. J Clin Pathol. 1979;32:719–22. doi: 10.1136/jcp.32.7.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mcginnis MR. Annu Rev Microbiol. Vol. 34. 1980. Recent taxonomic developments and changes in medical mycology; pp. 109–35. [DOI] [PubMed] [Google Scholar]
- 26.Shadomy S, Espinel-Ingrof A, Gebhar RJ. In vitro studies with sf 86-327, a new orally active allylamine derivatives. I Med Vet Mycologia. 1985;23:125–32. doi: 10.1080/00362178585380201. [DOI] [PubMed] [Google Scholar]
- 27.Odds FC. Antifungal activity of saperconazole (R. 66905) in vitro. J Antimicrobiol Chemother. 1989;24:533–7. doi: 10.1093/jac/24.4.533. [DOI] [PubMed] [Google Scholar]
- 28.Cleeland RS, Squires E. Evaluation of new antimicrobials in vitro and in experimental animal infection. In: Lorian VMD, editor. Antibiotics in Laboratory Medicine. Baltimore: Willians & Wikins; 1991. pp. 739–88. [Google Scholar]
- 29.Muñoz-Mingarro D, Acero N, Llinares F, Pozuelo JM, Galán de Mera A, Vicenten JA, et al. Biological activity of extracts from Catalpa bignonioides Walt. (Bignoniaceae) J Ethonopharmacol. 2003;87:163–7. doi: 10.1016/s0378-8741(03)00111-9. [DOI] [PubMed] [Google Scholar]
- 30.Coelho de Souza G, Haas APS, von Poser GL, Schapoval EES, Elisabetsky E. Ethnopharmacological studies of antimicrobial remedies in the south of Brazil. J Ethnopharmacol. 2004;90:135–43. doi: 10.1016/j.jep.2003.09.039. [DOI] [PubMed] [Google Scholar]
- 31.Hasan A, Farman M, Ahmed I. Flavonoid glycosides from Indigofera hebepetala. Phytochemistry. 1994;35:275–6. [Google Scholar]
- 32.Esimone CO, Adikwu MU, Muko KN. Antimicrobial properties of Indigofera dendroides leaves. Fitoterapia. 1999;70:517–20. [Google Scholar]
- 33.Dahot MU. Antibacterial and antifungal activity of small protein of Indifogera oblongifolia leaves. J Ethnopharmacol. 1999;64:277–82. doi: 10.1016/s0378-8741(98)00136-6. [DOI] [PubMed] [Google Scholar]
- 34.Thangadurai D, Ramesh N, Viswanathan MB, Prasad DX. A novel xanthene from Indigofera longeracemosa stem. Fitoterapia. 2001;72:92–4. doi: 10.1016/s0367-326x(00)00236-7. [DOI] [PubMed] [Google Scholar]
- 35.Christie GS, Madsen NP, Hegarty MP. Acute biochemical changes in rat liver induced by the naturally occurring amino acid indospicine. Biochem Pharmacol. 1969;18:693–700. doi: 10.1016/0006-2952(69)90039-2. [DOI] [PubMed] [Google Scholar]
- 36.Terras FRG, Eggermont K, Kovaleva V. Small cysteine rich antifungal proteins from radish: their role in host defence. Plant Cell. 1995;7:573–88. doi: 10.1105/tpc.7.5.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ali AN, Attif OA, Mohammed MI. Herbal medicine in two Yemen provinces. Yemen Med J. 1999;3:13–20. [Google Scholar]
- 38.Rojas A, Hernandez L, Pereda-Miranda R, Mata R. Screening for antimicrobial activity of crude drug extracts and pure natural products from Mexican medicinal plants. J Ethonopharmacol. 1992;35:275–83. doi: 10.1016/0378-8741(92)90025-m. [DOI] [PubMed] [Google Scholar]
- 39.Brantner A, Grein E. Antibacterial activity of plant extract used externally in traditional medicine. J Ethnopharmacol. 1994;44:35–40. doi: 10.1016/0378-8741(94)90096-5. [DOI] [PubMed] [Google Scholar]
- 40.Somchit MN, Reezal I, Nur IE, Mutalib AR. In vitro antimicrobial activity of ethanol and water extracts of Cassia alata. J Ethonopharmacol. 2003;84:1–4. doi: 10.1016/s0378-8741(02)00146-0. [DOI] [PubMed] [Google Scholar]
- 41.Thangadurai D, Viswanathan MB, Ramesh N. Indigoferabietone, a novel abietane diterpenoid from Indigofera longeracemosa with potential antituberculous and antibacterial activity. Pharmazie. 2002;57:714–15. [PubMed] [Google Scholar]
- 42.Cáceres A, Cano O, Samayoa B, Aguilar L. Plants used in Guatemala for treatment of gastrointestinal disorders. I. Screening of 84 plant against Enterobacteria. J Ethnopharmacol. 1990;30:55–40. doi: 10.1016/0378-8741(90)90017-n. [DOI] [PubMed] [Google Scholar]
- 43.Meyer JJM, Afolayan AJ, Taylor MB, Engelbrecht L. Inhibition of herpes simplex virus type 1 by aqueous extracts from shoots of Helichrysum aureonitens (Asteraceae) J Ethnopharmacol. 1996;52:41–3. doi: 10.1016/0378-8741(96)01387-6. [DOI] [PubMed] [Google Scholar]
- 44.Elisabetsky E, Costa-Campos L. The alkaloid alstonine: a review of its pharmacological properties. Evid Based Complement Alternat Med. 2006;3:339–48. doi: 10.1093/ecam/nek011. [DOI] [PMC free article] [PubMed] [Google Scholar]