Abstract
Millimeter wave therapy (MWT), a non-invasive complementary therapeutic technique is claimed to possess analgesic properties. We reviewed the clinical studies describing the pain-relief effect of MWT. Medline-based search according to review criteria and evaluation of methodological quality of the retrieved studies was performed. Of 13 studies, 9 of them were randomized controlled trials (RCTs), only three studies yielded more than 3 points on the Oxford scale of methodological quality of RCTs. MWT was reported to be effective in the treatment of headache, arthritic, neuropathic and acute postoperative pain. The rapid onset of pain relief during MWT lasting hours to days after, remote to the site of exposure (acupuncture points), was the most characteristic feature in MWT application for pain relief. The most commonly used parameters of MWT were the MW frequencies between 30 and 70 GHz and power density up to 10 mW cm−2. The promising results from pilot case series studies and small-size RCTs for analgesic/hypoalgesic effects of MWT should be verified in large-scale RCTs on the effectiveness of this treatment method.
Keywords: analgesia, millimeter waves, pain therapy, review
Introduction
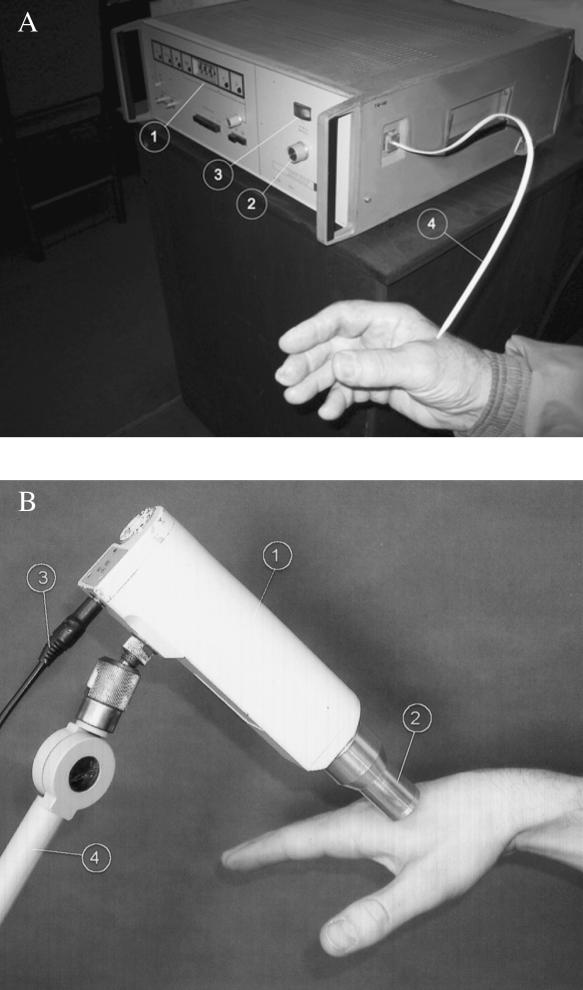
Inadequate pain therapy increases both morbidity and health care costs (1,2). The dominant method of pain control in modern medicine, pharmacotherapy, can cause numerous side effects (3–5). In order to increase the quality of pain management, various complementary non-pharmacological analgesic techniques, including millimeter wave therapy (MWT), have been tested (6). MWT is a non-invasive technique, consisting of the exposure of parts of the human body to electromagnetic radiation with frequencies 30–300 GHz (extremely high frequency electromagnetic field) and corresponding wavelengths from 10 to 1 mm (7). The discovery of resonance-like frequency dependence of biological effects of millimeter waves (MW) provided the theoretical background for their clinical application (8,9). Industrial continuous-wave generators (e.g. G4-142) using the backward-wave oscillator or Gunn diode-based generators are used for MWT (Fig. 1). Low intensity (<10 mW cm−2) electromagnetic radiation produced by MW generators causes no direct physical damage, ionization nor heating (<0.5°C) of exposed surface (10). More than 50 diseases and conditions have been claimed to be treated successfully with MW alone, or in combination with other treatment modalities, in over 3 million patients of the former USSR (11,12). One of the most common therapeutic effects of MW reported during the treatment of different diseases was the relief of concomitant pain (6,10,11). On the other hand, there are numerous experimental studies demonstrating the potential analgesic effects of MW in different parts of the nociceptive system (13–18). Distinguishing analgesia among the other therapeutic effects of MWT, the National Center for Complementary and Alternative Medicine (NCCAM) classified this form of treatment as one of the major areas of complementary and alternative medicine (19).
Figure 1.
Generators of electromagnetic millimeter waves. (A) Industrial continuous-wave generator G4-142 (Russia) using the backward-wave oscillator. 1-frequency out selector; 2-output power regulator; 3-output power indicator; 4-waveguide, applied to acupuncture point LI4. (B) Gunn diode-based generator DD 21-10 (Ukraine), over the LI4 point. 1-generator; 2-waveguide; 3-cable for DC supply; 4-extension arm (reproduced with permission, references 27,28).
The aim of this literature review was to retrieve all clinical studies where the pain relief effect of MWT was described, to evaluate their methodology and to compare the essentials of research procedure and results of these studies in order to recommend the directions for future clinical research on MWT in pain therapy.
Methods
We performed a Medline-based search and analysis of clinical studies describing the analgesic effects of MWT. This procedure was completed by a search of the catalog in the Ukranian Scientific Medical Library according to the following criteria: MW with frequency range 30–300 GHz, applied closely to the surface of the body; key words: ‘millimeter waves’, ‘microwave resonance therapy’, ‘clinical study’, ‘pain relief’, ‘analgesic effects’ were used in our Medline search; only the original full articles were included; all papers were studied in full format. The methodological quality of the studies was evaluated using the 5-point Oxford scale (20).
Results
According to the search criteria 13 studies were identified and grouped according to the clinical indications (Table 1). Nine of them fulfilled the criteria of randomized controlled trials (RCTs). Only three RCTs yielded more than 3 points on the Oxford scale used to evaluate the methodological quality of the RCTs.
Table 1.
Main features of clinical studies on pain relief effect of MWT
| Pain syndrome | Disease/underlying condition | N | MW frequency (GHz) | Power density (mW cm−2) | Site of MW application | Design | Oxford scale | Source/year |
|---|---|---|---|---|---|---|---|---|
| Experimental pain | Immersion in cold water | 12 | 42.25 | 30 | Lower third of sternum | RCT crossover | 5 | (21)/1999 |
| Headache | Cerebral atherosclerosis | 204 | 54–78 | 0.003 | Carotid sinus, vertebral arteries | nRCT | 0 | (22)/1998 |
| Essential hypertension | 56 | 60–63 | Missed | AP | RCT | 1 | (23)/1992 | |
| Joint pain | Primary OA | 114 | 55–62 | 0.01 | AP | RCT | 1 | (25)/1998 |
| JRA | 138 | 53.5 | AP | RCT | 1 | (26)/1996 | ||
| DCTD | 12 | 54–78 | 2.5 | Periarticular tender points | Case series | 0 | (27)/2003 | |
| RA | 12 | 54–64 | 2.5 | AP | RCT | 5 | (28)/2003 | |
| Postoperative pain | Brain lesions | 42 | 42.25 & 53.5 | 10 | Hands and feet | Case series | 0 | (29)/1998 |
| Abdominal surgery | 141 | 37 | 1 | Wound area | RCT | 4 | (31)/1995 | |
| Oral mucous pain | Lichen planus | 30 | 42.25 | 10 | Perioral area | RCT | 3 | (32)/2001 |
| ‘Burning mouth’ | 80 | 42.25 | 10 | Perioral area | RCT | 3 | (33)/2003 | |
| Neuropathic pain | Trigeminal neuralgia | 52 | 42.25 | 10 | Branches of trigeminal nerve | RCT | 2 | (34)/1995 |
N, number of subjects in the study; MW, millimeter waves; nRCT, non-randomized controlled trial; AP, acupuncture points; JRA, juvenile rheumatoid arthritis; OA, osteoarthritis; DCTD, diffuse connective tissue disease; RA, rheumatoid arthritis.
Volunteer Study
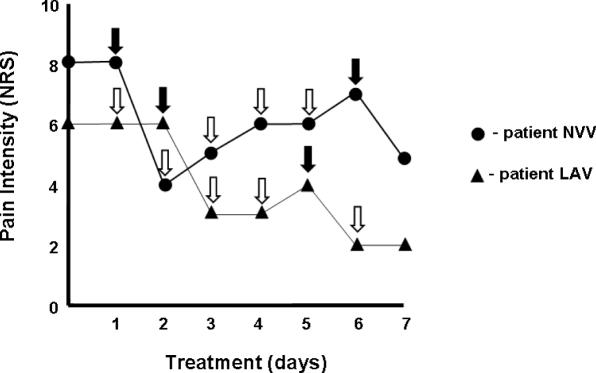
Radzievsky et al. performed the first classical physiological evaluation of hypoalgesic MW effect in a subject-evaluator blinded experimental study. The cold pressor test was used as a model of tonic aching pain, induced by immersing the hand of the volunteer in a cold water bath. Twelve healthy males were randomly exposed to an active medical MW generator for 30 min and the other time to a disabled sham generator with at least 24 h between exposures. Skin of the lower part of sternum of each volunteer was exposed to both true and sham generators in a random blinded manner. The characteristics of the active generator were frequency 42.25 GHz (corresponding wavelength 7.1 mm) and power density 30 mW cm−2. MW produced a suppression of pain sensation. Pain tolerance (measured as the time between the immersion of the hand in cold water and the onset of pain) increased by 38%. Pain sensitivity range (difference between pain tolerance and pain threshold values) increased by almost 50% (Fig. 2). Out of 12 volunteers, 7 reacted to the active MW generator with an increased pain tolerance. Heart rate, arterial blood pressure and palm temperature measured within the study remained unchanged (21).
Figure 2.
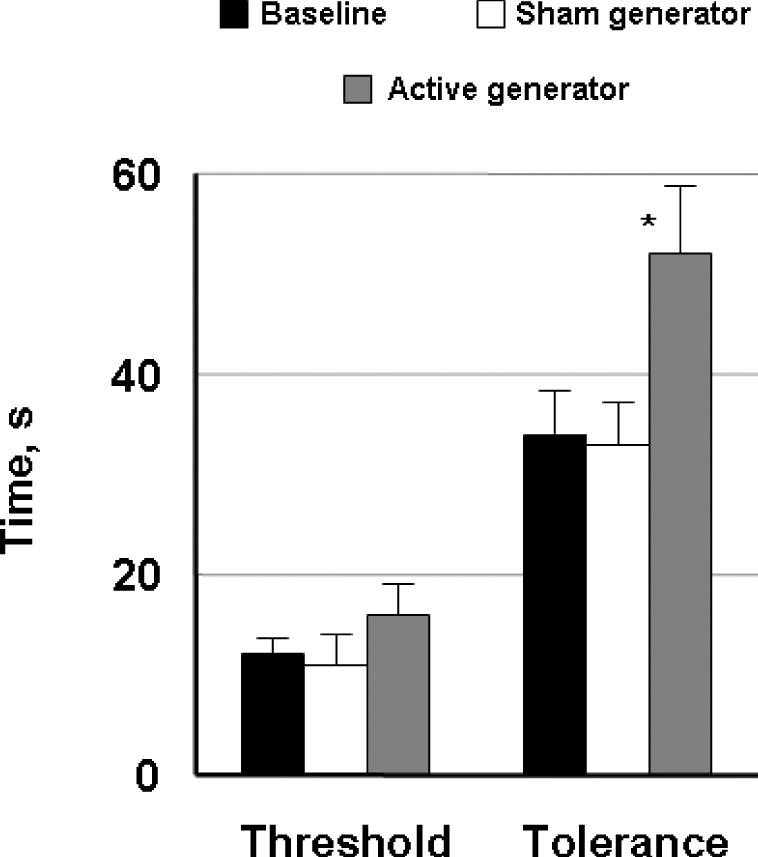
Both the threshold and tolerance of experimentally induced pain in 12 healthy volunteers increased after exposure to electromagnetic millimeter waves in comparison to sham procedure (details see in the text). Pain characteristics, measured in seconds, expressed here as means ± SEM, *difference is statistically significant (P < 0.05) (reproduced with permission from reference 21).
Clinical Trials
Headache
In a retrospective analysis of 204 patients with atherosclerosis of extracranial arteries, treated only with MW, Kuz’menko described the complete relief of headache in 122 out of 177 patients with pre-stroke forms of cerebrovascular pathology (22). Depending on the localization of clinical symptoms, areas of carotid sinus or vertebral arteries were exposed to broadband frequency MW of 54–78 GHz and power density of 1–3 µW cm−2. The duration of exposure was 10–20 min, the total number of treatment sessions ranged from 4 to 6. Along with the improvement of incomplete cognitive, motor and sensory deficits after MWT the author reported increased concentration of high-density lipoproteins, decrease of triglycerides and increased number of T-lymphocytes in comparison with baseline. A prospective controlled follow-up study revealed that 65% of patients treated with MWT remained in remission for ∼1 year versus 20% of patients from the matched control group, who received standard medication.
In another RCT on treatment of 56 patients with essential hypertension with MW versus intravascular laser application, Nikula et al. noticed that 18 out of 20 patients of MWT group reported the complete relief of their headache already during the first MWT session, whereas the patients of the laser group reported pain relief after the second session (23). MW noise of 60–63 GHz was applied bilaterally to acupuncture points ST 32 (20 min of exposure), PC 7 and PC 8 (10 min of exposure for each point). The total number of MWT sessions was 7. The nomenclature of acupuncture points is given according to the international classification approved by the experts of World Health Organization (24).
Joint Pain
Bakaliuk et al. studied the effects of MWT in patients with primary osteoarthritis (OA), applied additionally to conventional medication. One hundred and fourteen patients were randomized either to treatment with conventional medication (NSAIDs and chondroprotective agents, N = 20, group I) or to conventional medication + MWT (N = 94, group II). MW with frequency 55–62 GHz and power density 10 µW cm−2 were applied to 4–5 acupuncture points according to the OA localization, widely using the painful points around the affected joints (25). The time of exposure was 20 min and the total number of sessions was 10. The authors reported reduced pain intensity, expressed as a joint pain index, diminished joint stiffness and lower level of C-reactive protein (CRP) in group II in comparison with group I after treatment. Also they found an increased number of T- and decreased number of B-lymphocytes and immunoglobulins (Ig) A and M in patients treated additionally with MW. They noticed that the pain-relief and anti-inflammatory effect of MWT had already taken place after the second or at least third treatment session, whereas the effect of other forms of treatment wasn't seen until after several days. It remains unclear whether the patients and investigators were blinded to MWT.
Shliapak et al. reported the beneficial effects of MW in the treatment of children with juvenile rheumatoid arthritis (26). One hundred thirty-eight children were randomly assigned to three intervention groups. In group I the MW with fixed frequency 53.5 GHz were applied directly to the affected joints 30 min every day for 10 days. In group II the MW with the same parameters were applied bilaterally to the same acupuncture points (GV 20, GB 20, ST 36, LI 4 and BL 40) in all patients, independent of the localization of the affected joints. The number of the treatments was 6, the duration of exposure to MW was 30 min for every acupuncture point. In patients from group III MWT was applied to 2 acupuncture points. One of them (CV 22) was situated in the jugular notch and was exposed to MW during each treatment. The second point was chosen near the most effected (painful and swollen) joint (e.g. GB 34, near the knee joint; BL 60, ankle; LI 5, wrist; GB 30, hip joint).
The intensity of joint pain decreased by 50% in all three groups after MWT. The duration of morning stiffness and the circumference of the affected joints also decreased, and the functional joint status improved in 80–90% of children. The relief of joint symptoms was more pronounced in patients of group III, where the MW were applied to the acupuncture points situated near the thymic zone and the most affected joints (27). Moreover, the authors reported that the concentration of circulating immune complexes, B-lymphocytes and immunoglobulin G decreased and the number of T-lymphocytes and IgA increased during the course of MWT in patients from group III in comparison with the patients from other 2 study groups.
Encouraged by these findings, we applied MW for treatment of chronic joint pain in patients with diffuse connective tissue diseases (DCTD) (27). Twelve patients with joint pain syndromes of DCTD origin received MWT in addition to their analgesic medication with non-steroidal anti-inflammatory drugs. MWT procedure included the exposure of tender sites around the painful joints to electromagnetic MW with band frequency 54–78 GHz and power density 2.5 mW cm−2. The time of exposure was 35 ± 5 min and the total number of sessions ranged from 5 to 10 depending on the course of underlying DCTD. Intensity of joint pain, medication requirement and joint stiffness were taken before, during and immediately after the treatment, and after a 6-month follow-up. Pain intensity, joint stiffness and required medication decreased after the treatment and remained at the same level throughout the follow-up period. MWT applied to tender points around the affected joints was safe under the conditions of this case series study.
Thus as a next step in order to verify the effects of MW in the treatment of joint pain we started a randomized patient-evaluator blinded study in patients with rheumatoid arthritis (RA) (28). Twelve patients with RA were exposed to MW with band frequency 54–64 GHz and power density 2.5 mW cm−2. MW were applied to the acupuncture points painful on palpation situated near the affected joints. Four acupuncture points (two symmetric pairs) were consecutively exposed to MW during one session. Total duration of exposure was 40 min. The total number of sessions ranged from 5 to 9 (median 7) over 2 weeks. Double blinding of the treatment was provided by a computer, which was programmed to randomize patients into three groups and drive MW generators. According to the study design, group I received only real MWT sessions, group II only sham MWT procedure. Group III was exposed to MW in a random crossover manner. Pain intensity, joint stiffness and laboratory parameters were recorded before, during and immediately after the treatment. The study was discontinued because of beneficial therapeutic effects of MWT. Patients from group I (n = 4) reported significant pain relief and reduced joint stiffness during and after the course of therapy. Patients from group II (n = 4) revealed no improvement during the study. Patients from group III reported changes regarding pain and joint stiffness only after real MW sessions (Fig. 3). Monitored laboratory parameters: blood cell count, ESR and CRP did not change significantly after the treatment course in comparison to the baseline.
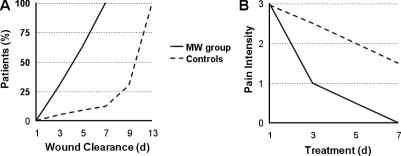
Figure 3.
Pain intensity according to a numerical rating scale from 0 to 10 (NRS-11, ranged from 0 = no pain to 10 = worst imaginable pain) in two patients with rheumatoid arthritis, who were exposed to MWT in crossover manner. Filled arrows, real; hollow arrows, sham MWT sessions (reproduced with permission from reference 28).
Postoperative Pain
Tyshkevich et al. reported the relief of postoperative pain after craniotomy in 42 patients aged 3–54 years when treated with MW in a case series study (29). MW with fixed frequencies 42.25 and 53.53 GHz (corresponding wavelengths 7.1 and 5.6 mm) and power density 10 mW cm−2 were applied to the palms of the hands and the soles of the feet for 2–7 min per field of exposure daily or every other day for 3 weeks after surgery. The total number of MWT sessions ranged from 5 to 10. An additional course of MWT, if indicated, was performed 2 months after the first treatment. The authors observed complete relief of postoperative cranial pain after 3–5 MWT sessions followed by improvement of cognitive brain function, although these parameters were described only qualitatively. Out of 42 patients studied, 30 suffered postoperative epilepsy (focal and generalized seizures). During the MWT the incidence of seizure episodes was reduced without additional pharmacological treatment. The clinical improvement was accompanied by a normalization of the bioelectric brain activity (stabilization of α-rhythm) and disappearance of the pathologically slow δ-waves monitored by means of electroencephalography (25). Because the study did not have a control group, it is impossible to distinguish the described improvement from the natural course of postoperative recovery.
Based on their previous experimental success in treatment with electromagnetic MW of wounds infected with Staphylococcis aureus in rabbits (30), Korpan and Saradeth performed a randomized patient-evaluator blinded clinical trial on the effects of MWT for wound treatment in patients after abdominal surgery (31). One hundred forty-one patients were randomly divided into two groups: group I (N = 71) received MWT with frequency 37 GHz and power density 1 mW cm−2, group II (control group) was treated with an inactive MWT generator (sham procedure). MW were applied directly to the wound areas for 30 min on 7 consecutive days. The accelerated wound healing was accompanied by clinically remarkable reduction of postoperative pain in group I, treated with the active device in comparison with the control group. The intensity of postoperative pain, measured on the numerical rating scale NRS-4 decreased already on the third postoperative day in >90% of patients in group I, whereas in group II satisfying wound healing took place in only 25% within the same period (Fig. 4).
Figure 4.
The accelerated wound healing in patients treated with millimeter waves (MW) after abdominal surgery (A) was accompanied by pronounced reduction of postoperative pain (B) in comparison with the control group (‘d’ means days on the x-axis). The significant reduction of postoperative pain intensity, measured on numerical rating scale NRS-4, was registered on the third day after the surgery in more than 90% of patients treated with MW (modified according to reference 31).
Other Reported Applications with Pain Relief
The research group from the Oral Medicine Department of Sichuan University, China, studied clinical and immunological effects of millimeter waves in patients with oral lichen planus (OLP). Thirty patients with OLP were randomly assigned to receive either MWT or conventional medication (N = 15 per group). After the MWT with frequency 43 GHz (corresponding wavelength 7.1 mm) and power density 10 mW cm−2, along with the decrease of CD8+ positive T-lymphocytes in patients from MWT group, the authors found decreased pain intensity in comparison with the control group (32).
The same research group studied the effects of MWT in patients with ‘burning mouth’ syndrome (BMS). Eighty patients were randomized into four groups: group I, MWT and conventional medication; group II, MWT alone; group III, sham MWT and conventional medication; group IV, medication alone. After MWT was applied to the perioral zone with the same output parameters as in their previous study the authors registered decreased pain intensity in the groups I and II treated with MW in comparison with group IV (conventional medication) but not with sham MWT + medication, suggesting the placebo effect of MWT (33).
Megdiatov et al. reported effective application of MWT in patients with trigeminal neuralgia. Fifty-two patients were randomly allocated to receive either MW (group I) or sham procedure—inactive MW generator (group II) additionally to conventional medication. The MW radiation with 42.25 GHz and power density 10 mW cm−2 was applied to areas where branches of the trigeminal nerve approach the skin. The number of MWT sessions was 10, duration of each session was 15 min. Out of 27 patients from group I (real MWT), 19 reported reduced pain intensity and decreased incidence of neuralgia attacks in comparison to 4 out of 25 patients from the control group, who received sham MWT procedure (34).
In a case series study of the MWT effects in 39 patients with chronic neuropathic pain from cancer of abdominal origin Grubnik et al. described pain relief effect already during the first treatment session (35). During the course of MWT all patients gradually reduced and completely stopped their analgesic medication with opioid drugs. An improvement of night sleep, appetite and intestinal function was registered after MWT in 36 patients. Thirty-two patients reported an improvement in life quality.
Immediate pain relief from MWT (during the first treatment session) was reported in a number of retrospective studies without control group, where MW was used to treat vertebral osteochondrosis. An analysis of these studies is precluded by insufficient description of the study methods as well as the absence of clear outcome measures (36,37).
Side Effects
In the studies reviewed the authors did not report any health-related side effects of MWT. Slight paresthesias, previously mentioned in several case reports and non-controlled case series (10,11), appeared in almost 50% of patients in studies where the effects of MWT were carefully described (21,27,28,31). The paresthesias were of short duration and reported as pleasant (‘warmth’) or neutral. General fatigue and sleepiness during the treatment sessions in almost 80% of the patients was a rather desirable side effect of MWT, as also described in previous reviews on biomedical effects of MWT (10,11,21,27,28).
Methodological Quality of Reviewed Studies
Only three (21,28,31) out of the nine randomized controlled studies described a randomization method, which was appropriate for this purpose. Also only two out of three these studies mentioned the withdrawal criteria and defined the analgesic effect as the primary endpoint of investigation, expressed either as pain intensity/tolerance or analgesic requirement (21,28). The majority of other studies reported the analgesic effect of MW as an additional finding. For future studies on the effectiveness of MWT for pain relief such primary endpoints as pain intensity and analgesics requirement are probably the most suitable outcome measures. Owing to the individual variability of patients’ responses to both placebo and active treatment, more than 40 per group are recommended by the experts (38).
Common Biological Features of MWT
The most characteristic feature of the pain-relief effect of MW described was the immediate onset of analgesia/hypoalgesia during the application of MWT. Pain relief from MW was already detectable after several minutes of exposure and lasted from several hours to several days. A typical example is presented on the graph of individual pain intensity measurement during the course of MWT, where the real and sham MWT sessions were applied intermittently [Figure 3 from (29)]. The improvement of other clinical (wound clearance, joint stiffness) and laboratory parameters (inflammation and immunological values) was delayed several days (Fig. 4).
MW probably influences the immune system: at least it was shown in patients with disorders where the immune system was affected (25,26,32). Radzievsky et al. recently showed an intriguing aspect of the involvement of the endogenous opioid system in the anticancer effect of MW. They exposed the murine experimental model of subcutaneous melanoma to MW with frequency 61.22 GHz and power density 13.3 mW cm−2 during 15 min for 5 days. MW exposures started at the fifth day following melanoma cell injection suppressed subcutaneous tumor growth. Pretreatment with naloxone (a non-specific antagonist of opioid receptors) completely abolished the MWT-induced suppression of melanoma growth (39).
The other common finding was the effect of MW remote to the site of exposure. Almost all the authors applied MW to acupuncture points or equivalent sites (Table 1). The other application sites of MW were the lower part of the sternum, tender points, painful joints, wounds, etc. All these are considered acupuncture points (or the parts of impaired energy flow along the meridians) from the point of view of Traditional Chinese Medicine (40). According to the existing data it is not possible yet to evaluate the role of the site of exposure. It should be verified in rigorously controlled trials.
The time of exposure ranged from 10 to 60 min in the studies reviewed. However, there is still no data on the influence of shorter or longer exposure on the outcome of MWT.
So far there are no clinical studies comparing the effectiveness of the noise electromagnetic MW radiation versus fixed frequencies. The claim of several authors that the frequencies 45.25, 53.57 and 61.22 GHz possess therapeutic properties and are free from side effects was not verified by sufficient data (10,41,42). Sharp resonance-like frequency dependence was described for effects of low-intensity MW only in vitro (8,9,43–45). Samosiuk et al. provided the evidence for an optimal frequency of MW in pain treatment in an animal experiment. The authors compared the fixed frequencies 60 and 118 GHz with noise MW radiation of frequency range 42–95 and 90–140 GHz in the model of formalin-induced nociceptive behavior reaction (licking of wounded hind paw) in experimental mice. They found out that the strongest analgesia was achieved under the exposure to the noise MW radiation of 42–95 GHz (46).
Almost all findings were described using MW with power density ranged 1–10 mW cm−2. This power of MWT has been reported to be safe and free of health hazards (13). The data from experimental research have clearly shown that the increase of the radiation power of MW does not increase the biological effect, i.e. there was a sealing effect in the range of maximally 10 mW cm−2 (43). This power might be sufficient to achieve optimal clinical effects of MWT, although the appropriate studies have not been yet reported.
Conclusion and Directions for Future Research
We conclude that there is promising data from pilot case series and small-scale randomized controlled trials for analgesic/hypoalgesic effects of electromagnetic millimeter waves in frequency range 30–70 GHz. Large-scale randomized controlled trials on the effectiveness of this non-invasive therapeutic technique are necessary. The effects of MW applied with selected frequencies should be compared with those of broadband MW. The most intriguing question for future research might be the evaluation of the role of the exposure site, especially in relation to the topography of the acupuncture meridian system.
Acknowledgments
We thank Dr Boris Rudko from Scientific Research Center ‘Vidhuk’ (Kiev, Ukraine) for his assistance in the preparation of illustrations.
References
- 1.Dolin SJ, Cashman JN, Bland JM. Effectiveness of acute postoperative pain management: I. Evidence from published data. Br J Anaesth. 2002;89:409–23. [PubMed] [Google Scholar]
- 2.Joshi GP, Ogunnaike BO. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Anesthesiol Clin North America. 2005;23:21–36. doi: 10.1016/j.atc.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 3.Zhao SZ, Reynolds MW, Lejkowith J, Whelton A, Arellano FM. A comparison of renal-related adverse drug reactions between rofecoxib and celecoxib, based on the World Health Organization/Uppsala Monitoring Centre safety database. Clin Therap. 2001;23:1478–91. doi: 10.1016/s0149-2918(01)80121-1. [DOI] [PubMed] [Google Scholar]
- 4.Sturkenboom MC, Romano F, Simon G, Correa-Leite ML, Villa M, Nicolosi A, et al. The iatrogenic costs of NSAID therapy: a population study. Arthritis Rheum. 2002;47:132–40. doi: 10.1002/art.10268. [DOI] [PubMed] [Google Scholar]
- 5.Graham DJ, Campen D, Hui R, Spence M, Cheetham C, Levy G, et al. Risk of acute myocardial infarction and sudden cardiac death in patients treated with cyclo-oxygenase 2 selective and non-selective non-steroidal anti-inflammatory drugs: nested case-control study. Lancet. 2005;365:475–81. doi: 10.1016/S0140-6736(05)17864-7. [DOI] [PubMed] [Google Scholar]
- 6.Skurikhina LA. The therapeutic use of electromagnetic millimeter waves of nonthermal intensity millimeter-wave therapy. Vopr Kurortol Fizioter Lech Fiz Kult. 1988;5:65–72. [PubMed] [Google Scholar]
- 7.Gandhi OP. Some basic properties of biological tissues for potential biomedical applications of millimeter waves. J Microw Power. 1983;18:295–304. doi: 10.1080/16070658.1983.11689334. [DOI] [PubMed] [Google Scholar]
- 8.Webb SJ, Dodds DD. Inhibition of bacterial cell growth by 136 gc microwaves. Nature. 1968;218:374–5. doi: 10.1038/218374a0. [DOI] [PubMed] [Google Scholar]
- 9.Zaliubovskaia NP. Biological effect of the millimeter-range radiowaves. Vrach Delo. 1977;3:116–19. [PubMed] [Google Scholar]
- 10.Ryan KL, D'Andrea JA, Jauchem JR, Mason PA. Radio frequency radiation of millimeter wave length: potential occupational safety issues relating to surface heating. Health Phys. 2000;78:170–81. doi: 10.1097/00004032-200002000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Rojavin MA, Ziskin MC. Medical application of millimeter waves. Q J Med. 1998;91:57–66. doi: 10.1093/qjmed/91.1.57. [DOI] [PubMed] [Google Scholar]
- 12.Pakhomov AG, Akyel Y, Pakhomova ON, Stuck BE, Murphy MR. Current state and implications of research on biological effects of millimeter waves: a review of the literature. Bioelectromagnetics. 1998;19:393–413. doi: 10.1002/(sici)1521-186x(1998)19:7<393::aid-bem1>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 13.Enin LD, Akoev GN, Potekhina IL, Oleiner VD. Effect of extremely high-frequency electromagnetic radiation on the function of skin sensory endings. Patol Fiziol Eksp Ter. 1992;5-6:23–5. [PubMed] [Google Scholar]
- 14.Akoev GN, Avelev VD, Semenjkov PG. Reception of low-intensity millimeter-wave electromagnetic radiation by the electroreceptors in skates. Neuroscience. 1995;66:15–7. doi: 10.1016/0306-4522(95)00054-m. [DOI] [PubMed] [Google Scholar]
- 15.Rojavin MA, Cowan A, Radzievsky AA, Ziskin MC. Antipruritic effect of millimeter waves in mice: evidence for opioid involvement. Life Sci. 1998;63:251–7. doi: 10.1016/s0024-3205(98)00436-6. [DOI] [PubMed] [Google Scholar]
- 16.Radzievsky AA, Rojavin MA, Cowan A, Alekseev SI, Radzievsky AA, Jr, Ziskin MC. Peripheral neural system involvement in hypoalgesic effect of electromagnetic millimeter waves. Life Sci. 2001;68:1143–51. doi: 10.1016/s0024-3205(00)01016-x. [DOI] [PubMed] [Google Scholar]
- 17.Novikova NS, Kazakova TB, Rogers VJ, Korneva EA. C-fos gene expression induced in cells in specific hypothalamic structures by noxious mechanical stimulation and its modification by exposure of the skin to extremely high frequency irradiation. Neuro Endocrinol Lett. 2002;23:315–20. [PubMed] [Google Scholar]
- 18.Novikova NS, Kazakova TB, Rogers V, Korneva EA. Expression of the c-fos gene in spinal cord and brain cells in rats subjected to stress in conditions of exposure to various types of halothane anesthesia. Neurosci Behav Physiol. 2004;34:407–12. doi: 10.1023/b:neab.0000018753.29627.02. [DOI] [PubMed] [Google Scholar]
- 19. http://nccam.nih.gov/health/backgrounds/energymed.htm.
- 20.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 21.Radzievsky AA, Rojavin MA, Cowan A, Ziskin MC. Suppression of pain sensation caused by millimeter waves: a double-blinded, cross-over, prospective human volunteer study. Anesth Analg. 1999;88:836–40. doi: 10.1097/00000539-199904000-00029. [DOI] [PubMed] [Google Scholar]
- 22.Kuz'menko VM. The role of microwave resonance therapy in the combined treatment of patients with cerebral atherosclerosis. Lik Sprava. 1998;7:146–8. [PubMed] [Google Scholar]
- 23.Nikula TD, Karpenko VV, Voitovich NS, Karmazina EM. Comparative evaluation of the efficacy of quantum methods of treatment of patients with hypertensive disease. Lik Sprava. 1992;10:32–5. [PubMed] [Google Scholar]
- 24.Standard Acupuncture Nomenclature. 1993. Second Edition (ISBN 92 9061 105 7), WHO Regional Office for the Western Pacific, Manila.
- 25.Bakaliuk TG, Zoria LV, Pogorila MA. Microwave resonance therapy in primary osteoarthrosis: the pathogenetic validation of its clinical use. Patol Fiziol Eksp Ter. 1998;4:22–5. [PubMed] [Google Scholar]
- 26.Shliapak EA, Gabidova NT, Evseeva SN, Apanasevich ZK. The EHF therapy of children with juvenile rheumatoid arthritis. Vopr Kurortol Fizioter Lech Fiz Kult. 1996;6:19–21. [PubMed] [Google Scholar]
- 27.Usichenko TI, Herget HF. Treatment of chronic pain with millimetre wave therapy (MWT) in patients with diffuse connective tissue diseases: a pilot case series study. Eur J Pain. 2003;7:289–94. doi: 10.1016/S1090-3801(02)00125-8. [DOI] [PubMed] [Google Scholar]
- 28.Usichenko TI, Ivashkivsky OI, Gizhko VV. Treatment of rheumatoid arthritis with electromagnetic millimeter waves applied to acupuncture points—a randomized double blind clinical study. Acupunct Electrother Res. 2003;28:11–8. doi: 10.3727/036012903815901723. [DOI] [PubMed] [Google Scholar]
- 29.Tyshkevich TG, Bersnev VP, Stepanova TS. The use of millimeter waves in neurosurgery under electrophysiological control. Vopr Kurortol Fizioter Lech Fiz Kult. 1998;1:30–33. [PubMed] [Google Scholar]
- 30.Korpan NN, Resch KL, Kokoschinegg P. Continuous microwave enhances the healing process of septic and aseptic wounds in rabbits. J Surg Res. 1994;57:667–71. doi: 10.1006/jsre.1994.1198. [DOI] [PubMed] [Google Scholar]
- 31.Korpan NN, Saradeth T. Clinical effects of continuous microwave for postoperative septic wound treatment: a double-blind controlled trial. Am J Surg. 1995;170:271–6. doi: 10.1016/s0002-9610(05)80013-3. [DOI] [PubMed] [Google Scholar]
- 32.Jin Z, Lin M, Xia J, Zhuang J, Yang R, Li X, et al. A study of millimeter wave’s clinical and immunological effects on oral lichen planus patients. Hua Xi Kou Qiang Yi Xue Za Zhi. 2001;19:366–8. [PubMed] [Google Scholar]
- 33.He Y, Lin M, Li BQ, Xia J, Zeng GM. Effect of millimeter therapy in burning mouth syndrome. Zhonghua Kou Qiang Yi Xue Za Zhi. 2003;38:89–92. [PubMed] [Google Scholar]
- 34.Megdiatov RS, Vasilenko AM, Arkhipov VV, Kislov VYa, Kolesov VV, Smirnov VF. Use of a ‘Sharm’ therapeutic-diagnostic system in complex therapy of trigeminal nerve neuralgia. Proceedings of the 10th Russian Symposium with International Participation ‘MillimeterWaves in Medicine and Biology’; Moscow, Russia: Russian Academy of Sciences; 1995. pp. 83–4. [Google Scholar]
- 35.Grubnik BP, Sitko SP, Shalimov AA. Experience of using Sitko MRT technology for rehabilitation of III-IV stage oncologic patients. J Physics Alive. 1998;6:97–102. [Google Scholar]
- 36.Droviannikova DP, Volobuev AN, Romanchuk PI. The mechanism of the therapeutic action of the EHF therapy of spinal osteochondrosis. Vopr Kurortol Fizioter Lech Fiz Kult. 1995;2:25–6. [PubMed] [Google Scholar]
- 37.Miryutova NF, Levitskii EF, Kozhemyakin AM, Mavlyautdinova IM. Millimeter waves in the treatment of neurological manifestations of vertebral osteochondrosis. Crit Rev Biomed Eng. 2001;29:613–21. doi: 10.1615/critrevbiomedeng.v29.i56.30. [DOI] [PubMed] [Google Scholar]
- 38.Moore RA, Gavaghan D, Tramer MR, Collins SL, McQuay HJ. Size is everything—large amounts of information are needed to overcome random effects in estimating direction and magnitude of treatment effects. Pain. 1998;78:209–16. doi: 10.1016/S0304-3959(98)00140-7. [DOI] [PubMed] [Google Scholar]
- 39.Radzievsky AA, Gordiienko OV, Szabo I, Alekseev SI, Ziskin MC. Millimeter wave-induced suppression of B16 F10 melanoma growth in mice: involvement of endogenous opioids. Bioelectromagnetics. 2004;25:466–73. doi: 10.1002/bem.20018. [DOI] [PubMed] [Google Scholar]
- 40.Cheng Xinnong., editor. Principles of selecting points for acupuncture analgesia. Chinese Acupuncture and Moxibustion. 1st edition. Beijing: Foreign Languages Press; 1987. pp. 515–16. [Google Scholar]
- 41.Golant MB. Resonance effect of coherent millimeter-band electromagnetic waves on living organisms. Biofizika. 1989;34:1004–14. [PubMed] [Google Scholar]
- 42.Novikova LN, Kaminskaia GO, Efimova LN. Significance of the functional state of blood phagocytes in the choice of optimal regime of EHF therapy of patients with pulmonary tuberculosis. Probl Tuberk. 1995;6:17–20. [PubMed] [Google Scholar]
- 43.Vilenskaia RL, Smolianskaia AZ, Adamenko VG, Buldasheva ZP, Gel’vich EA. Induction of colicin synthesis by millimeter radiation. Biull Eksp Biol Med. 1972;73:52–4. [PubMed] [Google Scholar]
- 44.Grundler W, Keilmann F, Frölich H. Resonant growth rate response of yeast cells irradiated by weak microwaves. Phys Lett. 1977;62A:463. [Google Scholar]
- 45.Sevast’ianova LA. Characteristics of the biological action of millimeter-range radio waves and the potential for their utilization in medicine. Vestn Akad Med Nauk SSSR. 1979;2:65–8. [PubMed] [Google Scholar]
- 46.Samosiuk IZ, Kulikovich IuN, Tamarova ZA, Samosiuk NI, Kazhanova AK. Pain relief by low-intensity frequency-modulated millimeter waves acting on the acupuncture points. Vopr Kurortol Fizioter Lech Fiz Kult. 2000;4:7–11. [PubMed] [Google Scholar]