Abstract
Ninety individuals with social phobia (social anxiety disorder) participated in a randomized controlled trial and completed cognitive–behavioral group therapy, exposure group therapy without explicit cognitive interventions, or a wait-list control condition. Both treatments were superior to the wait-list group in reducing social anxiety but did not differ from one another at posttest. Changes in estimated social cost mediated treatment changes in both treatment conditions from pre- to posttest. However, only participants who received cognitive–behavioral therapy showed continued improvement from posttest to 6-month follow-up, which was associated with a reduction of estimated social cost from pretest to posttest. These results suggest that cognitive intervention leads to better maintenance of treatment gains, which is mediated through changes in estimated social cost.
Social phobia is the most common type of anxiety disorder and the third most common mental disorder in the U.S. population (Kessler et al., 1994). Numerous studies have demonstrated the efficacy of psychological treatments for social phobia, especially cognitive–behavioral therapy and exposure therapy (e.g., Clark et al., 2003; Feske & Chambless, 1995; Heimberg et al., 1998; Taylor, 1996). It has been argued that social phobia treatments involving explicit cognitive strategies should be superior to pure exposure therapy because cognitive interventions are directly aimed at changing dysfunctional thinking (Butler, 1985; Butler, Cullington, Munby, Amies, & Gelder, 1984; Stopa & Clark, 1993). This assumption, however, is not clearly supported by the empirical data. There are eight controlled clinical studies in the literature in which investigators directly compared cognitive–behavioral therapy with exposure therapy without explicit cognitive interventions (Butler et al., 1984; Emmelkamp, Mersch, Vissia, & van der Helm, 1985; Gelernter et al., 1991; Hope, Heimberg, & Bruch, 1995; Mattick & Peters, 1988; Mattick, Peters, & Clark, 1989; Scholing & Emmelkamp, 1993a, 1993b). In only two of the trials did the effects of cognitive–behavioral therapy exceed those of exposure alone at posttreatment (Butler et al., 1984; Mattick & Peters, 1988). Furthermore, a number of meta-analyses suggested that both cognitive–behavioral therapy and exposure therapy produce very similar dropouts and pre/post and pre/follow-up effects for self-report measures of social phobia, cognitive symptoms, and depressed–anxious mood (Feske & Chambless, 1995; Gould, Buckminster, Pollack, Otto, & Yap, 1997; Taylor, 1996). Finally, the results of a dismantling study conducted by Hope, Heimberg, and Bruch (1995) suggest that exposure alone is at least as effective as exposure plus cognitive intervention in the treatment of social phobia.
These findings raise important questions about the mechanism of treatment changes and the variables that are involved in this change process (i.e., the mediators of change). The cognitive model of social phobia posits that certain beliefs about the social situation are responsible for the maintenance of the disorder. Furthermore, it is assumed that changes in social anxiety during cognitive therapy are due to the modification of those beliefs about the anxiety-producing situation. More specifically, the cognitive model by Clark and Wells (1995) assumes that individuals with social phobia believe that “(1) they are in danger of behaving in an inept and unacceptable fashion, and (2) that such behavior will have disastrous consequences in terms of loss of status, loss of worth, and rejection” (pp. 69–70). Similarly, Foa and Kozak (1986) proposed earlier that social phobia is particularly distinguished by exaggerated social cost. This model assumes that estimated social cost is the primary mediating variable of cognitive treatment change. In an attempt to test this hypothesis, Foa, Franklin, Perry, and Herbert (1996) treated 15 generalized social phobic individuals with a modified version of Heimberg’s cognitive–behavioral group therapy (CBGT; Heimberg, 1991). Before and after treatment, all patients and 15 nonanxious controls filled out the Social Probability Questionnaire (SPQ; Foa et al., 1996) and Social Cost Questionnaire (SCQ; Foa et al., 1996) to measure overestimation of negative social events and estimated social cost, respectively. Consistent with the authors’ hypothesis, patients evidenced socially relevant judgmental biases prior to treatment, which were attenuated following treatment. Moreover, the analyses showed that a decrease in both estimated social cost and overestimation of negative social events was highly associated with posttreatment level of symptom severity as measured with the Social Phobia and Anxiety Inventory (SPAI; Turner et al., 1989). This relationship remained strong for estimated social cost after controlling for change in estimated probabilities but not vice versa. The partial correlations between posttreatment scores and estimated social cost and social probability were .76 and .27, respectively. Furthermore, appraisals of cost and probability of negative social events were highly correlated (r = .74), suggesting that estimated social cost was the best single predictor for treatment outcome in this study. The authors concluded that estimated social cost may be an important mediator of treatment change.
The purpose of this study was to further examine the possible role of estimated social cost as a cognitive mediator in the treatment of social phobia. Treatments that directly modify judgmental biases through cognitive strategies should be more closely associated with changes in estimated social cost than treatments without explicit cognitive interventions. For the analyses, we adopted the recent recommendations by Kraemer, Wilson, Fairburn, and Agras (2002) for testing mediation, which is an extension and modification of the procedure proposed by Baron and Kenny (1986). According to Kraemer et al. (2002), a mediational relationship exists if (a) the proposed mediator correlates with treatment choice, (b) the mediator has either a main or an interactive effect on outcome, and (c) changes in the mediator variable precede changes in the dependent variable. We predicted that estimated social cost mediates changes in social anxiety in individuals who receive cognitive–behavioral therapy but not among those who receive exposure therapy without explicit cognitive interventions.
Method
Participants
Ninety individuals participated in this study. These participants were randomly selected from individuals who sought outpatient treatment at the Center for Anxiety and Related Disorders at Boston University between 1998 and 2001. Exclusion criteria for this study included (a) prior nonresponse to adequately delivered study treatment, (b) current diagnosis of psychoactive substance abuse or dependence, (c) currently active suicidal potential, (d) current diagnosis of bipolar disorder, and (e) current diagnoses of schizophrenia and other psychotic disorders. In addition, participants had to report at least moderate public speaking anxiety, which was defined by a self-report rating of 4 or greater on an 8-point Likert scale ranging from 0 (no anxiety at all) to 8 (extreme anxiety). This inclusion criterion was chosen because repeated exposure to speech situations was an important component of one of the treatment protocols (exposure group therapy). Although this intervention utilizes only public speaking situations as in-session exposure practices, we found in previous studies that the treatment effects easily generalize to other social situations (Hofmann, Newman, Becker, Taylor, & Roth, 1995; Newman, Hofmann, Trabert, Roth, & Taylor, 1994). The majority of individuals with social phobia who presented at the center for treatment (88.9%) met all study criteria and were invited to participate in the study.
Participants were assigned to one of three conditions: cognitive–behavioral group therapy (CBGT), which is a comprehensive cognitive–behavioral treatment protocol (Heimberg, 1991); exposure group therapy (EGT), which is an exposure treatment without explicit cognitive interventions; or a wait-list control group (WL). Patients from the WL group randomly received either CBGT or EGT after the waiting period. Their treatment data, however, were not included in these analyses.
Participants were randomly assigned to the three conditions until there were 30 completers per group. The attrition rates from CBGT, EGT, and WL were 14%, 21%, and 35%, respectively. As a result of missing data in some measures, the number of valid cases for the various analyses ranged between 27–30 cases for CBGT, 29–30 cases for EGT, and 26–30 cases for WL. This sample size provided the primary statistical test (linear regression with three predictors) with sufficient power (power > .9) to detect a large-size effect (f 2 = .35) at p < .05.
Seventy-six percent of the sample met criteria for the generalized subtype of social phobia. The proportion of participants with generalized social phobia was equally distributed across the three treatment conditions, p > .18. Forty-four percent of the present sample (n = 40) met criteria for at least one additional DSM–IV (Diagnostic and Statistical Manual of Mental Disorders, 4th ed; American Psychiatric Association, 1994) diagnosis (EGT, n = 18; CBGT, n = 12; WL, n = 20). The three most common additional diagnoses were major depressive disorder (EGT, n = 10; CBGT, n = 5; WL, n = 8), generalized anxiety disorder (EGT, n = 2; CBGT, n = 4; WL, n = 6), and panic disorder with or without agoraphobia (EGT, n = 2; CBGT, n = 0; WL, n = 2). The difference between the groups in the number of individuals with clinical depression was not statistically significant, p > .30.
No group differences were found in gender ( p > .2), race ( p > .6), or marital status ( p > .6). Although a comparison between groups in age was not statistically significant, F(2, 87) = 2.79, p < .067, the overall effect size (η2 = .06) suggested that there may be a small effect that was not shown to be statistically significant in this study. The results suggest that participants from the CBGT group tended to be younger (M = 28.8, SD = 7.2) than individuals from the EGT group (M = 34.0, SD = 9.3) or the WL group (M = 33.3, SD = 11.2). Most of the participants were male (54%), Caucasian (90%), and single (66%), with an average age of 32 years (SD = 9.5).
Attrition from the study was not associated with the diagnostic subtype of social phobia ( p > .6) or any demographic variables, including age ( p > .4), sex ( p > .5), race ( p > .3), and marital status ( p > .2). Furthermore, participants who prematurely terminated the study did not differ from completers in the SPAI social phobia subscale scores ( p >.6) or the SCQ scores at pretest ( p > .19). We were unable to perform an intent-to-treat analysis because insufficient information was available from individuals who terminated treatment.1
Treatments
The two study treatments consisted of 12 weekly sessions, which were conducted in a group format with two therapists and 5–7 participants per group and delivered according to structured treatment protocols. Nine therapists with comparable experience were trained to implement the two treatments. The training consisted of: (a) reading the detailed treatment protocol, (b) listening to an audiotaped first treatment session (in which the treatment rationale was presented), (c) attending weekly supervision meetings, and (d) coleading at least one complete treatment group. A total of six EGT groups and six CBGT groups were conducted. All therapists were advanced doctoral students in clinical psychology. Three were cross trained and led both types of treatment groups. Harlan Juster, who is a senior therapist and former collaborator of Richard G. Heimberg, provided weekly telephone supervision meetings of the CBGT groups. The EGT therapists were supervised weekly by Stefan G. Hofmann, who developed the EGT manual. The EGT protocol included repeated in-session in vivo exposures to social performance situations, video feedback, didactic training, and weekly homework assignments. Although participants feared numerous social situations, this intervention focused primarily on the patients’ public speaking anxiety. In contrast, patients in the CBGT groups were taught skills to identify negative cognitions, observe the covariation between anxious mood and cognitions, examine thinking errors (including overestimation of social cost), and formulate rational alternatives to these errors. Exposure exercises were conducted in session and assigned for homework. Exposures were explained as a means by which patients could scientifically test the validity of anxious predictions. In addition to the difference in the emphasis on cognitive strategies, the two protocols also differed in the treatment rationale, which was based on the cognitive model of anxiety in the case of CBGT and on a basic habituation rationale in the case of EGT. The results from previous meta-analyses (Feske & Chambless, 1995; Gould et al., 1997; Taylor, 1996) have suggested that both treatment protocols produce comparable short-term treatment effects.
Assessments
Before treatment, all participants received the full version of the Anxiety Disorders Interview Schedule for DSM–IV: Lifetime version (ADIS–IV–L; DiNardo, Brown, & Barlow, 1994). This interview took between 4–6 hours per participant and was conducted by advanced doctoral students of clinical psychology, who were unaware of the objective of this study. The kappa coefficient between two independent raters at the center is .77 for social phobia as a principal diagnosis and also .77 for social phobia as a principal or additional diagnosis. The reliability coefficients (kappa) for the other anxiety diagnoses range between .67 (generalized anxiety disorders) and .86 (specific phobias), and between .22 (dysthymia) and .72 (major depressive disorder) for mood disorders (Brown, DiNardo, Lehman, & Campbell, 2001).
Before the treatment or waiting period (pretest) and after the treatment or waiting period (posttest), participants were asked to fill out the SPAI (Turner et al., 1989) to measure social anxiety and the SCQ (Foa et al., 1996) to measure estimated social cost. The SPAI (Turner et al., 1989) is a 109-item self-report instrument that has been widely used to assess the cognitive, somatic, and behavioral dimensions of social phobia. This measure is capable of discriminating socially phobic persons from those with other anxiety disorders and from normal controls (Beidel et al., 1989). Test–retest and internal reliability have been high for this scale (Turner et al., 1989). Convergent and discriminant validity of this instrument have also been demonstrated (Beidel, Borden, Turner, & Jacob, 1989; Turner et al., 1989).
The SCQ instructs the person to rate the cost associated with a number of hypothetical events by indicating on a 9-point Likert scale ranging from 0 (not at all bad) to 8 (extremely bad) how bad or distressing it would be if a number of events happened. Sample items include: How bad would it be for you to have somebody leave while you are talking to several people? How bad would it be to unexpectedly be called in to see your supervisor at work? The scale consists of 40 items: 20 negative nonsocial events and 20 negative social events. The social events scale, which was used to measure estimated social cost in the present study, consists of 10 performance situations and 10 nonperformance social situations. Foa et al. (1996) reported high internal consistency and satisfactory test–retest reliability of this instrument.
In addition, participants underwent a social stress test at pre- and posttest to examine their behavioral anxiety response. For this task, participants were given a list of three randomly chosen controversial topics (the list of possible topics included: abortion, the U.S. health care system, the death penalty, mandatory seat belt laws, and speed limits on highways). Participants were informed that they could use one, two, or all three of these topics for their speech and that there were no restrictions in what to say about these topics. The topics were randomly chosen, but no participant received the same topic at both assessment points. Participants were asked to speak for as long as 10 min. If they wanted to terminate this task earlier, they were asked to hold up an index card on which the word STOP was written. The experimenter recorded the duration of the speech to the nearest second. In addition, participants’ self-statements were recorded using an open-ended thought-listing procedure. The results of these analyses are reported in a separate article.
To estimate the long-term effects of the treatments on social anxiety, all participants who received therapy were invited to fill out the SPAI a third time 6 months after the posttest assessment. Twenty individuals from the EGT group (66.7%) and 17 individuals from the CBGT group (56.7%) returned this instrument. Participants who returned the SPAI at 6-month follow-up were not significantly different from those who did not return the instrument in any relevant variables at the pre-treatment assessment, including the SPAI social phobia scores ( p > .9), SCQ score ( p > .6), age ( p > .3), diagnostic subtype specifier ( p > .8), gender ( p > .2), or marital status ( p > .9).
Results
Treatment Integrity
All treatment sessions were audiotaped, and a sample of 41 audiotapes (19 different CBGT sessions and 22 different EGT sessions) were randomly selected to be evaluated blindly for protocol adherence and therapist competence by a 5th-year doctoral student in clinical psychology. This student had been trained in various empirically supported interventions and closely supervised in her clinical work by experienced and licensed clinicians. She was familiar with both treatment protocols involved in the study as recommended by Waltz, Addis, Koerner, and Jacobson (1993). To examine the reliability of the rating system, a second graduate student also conducted a blind evaluation of a random subsample of 22 taped sessions (11 CBGT tapes and 11 EGT tapes). The raters evaluated each tape according to various criteria, using a 5-point Likert scale ranging from 1 (not at all/very poor) to 5 (great deal/excellent).
Overall therapist adherence to the two protocols was determined by rating the following items: The therapists used a ‘purely’ behavioral model of social phobia (i.e., without specific cognitive interventions), and the therapists used cognitive-restructuring techniques. Interrater agreement was estimated with intraclass correlation coefficients (ICC; Shrout & Fleiss, 1979). Specifically, we used Shrout and Fleiss’s (1979)ICC (2, 1) equation in which the two raters are considered random effects. The two raters showed high agreement in their assessment of the extent to which therapists used a “purely” behavioral model (ICC = .82, p < .0001). Moreover, the two raters showed very high agreement in their assessment of the extent to which therapists used cognitive-restructuring techniques (ICC = .995, p < .0001). Compared with the CBGT therapists, the EGT therapists used more of a purely behavioral model (Ms = 1.0 vs. 4.7), t(21) = 20.36, p < .0001. In contrast, the CBGT therapists used more cognitive restructuring techniques than the EGT therapists (Ms = 4.7 vs. 1.3), t(39) = 15.12, p < .0001.
All 41 tapes were further evaluated for therapist competency as measured by the Vanderbilt Psychotherapy Process Scale (Suh, Strupp, & O’Malley, 1986). This scale does not directly measure the competence of the implementation of the treatment techniques. Instead, it measures various characteristics of the psychotherapy process that are considered to be relevant for therapy outcome. Previous studies have shown that ratings of patient involvement and therapist-offered relationship are predictors of treatment outcome (O’Malley, Suh, & Strupp, 1983; Windholz, & Silberschatz, 1988).
Both treatment groups (means of CBGT vs. EGT) were rated high on the general quality of the relationship between the group members and the therapists (Ms = 4.5 vs. 4.6), on their productivity (Ms = 4.6 vs. 4.4), and on how well the therapists and the group members worked together (Ms = 4.7 vs. 4.8). Furthermore, the therapists’ demeanor during the sessions was rated as being involved (Ms = 5.0 vs. 4.9), optimistic (Ms = 4.5 vs. 4.5), and respectful (Ms = 4.9 vs. 4.9). In contrast, therapists from neither group appeared to be annoyed (Ms = 1.1 vs. 1.0), authoritative (Ms = 1.3 vs. 1.2), defensive (Ms = 1.0 vs. 1.0), or judgmental (Ms = 1.1 vs. 1.0; all ps > .1).
Short-Term Treatment Effects
To evaluate the short-term (pre- to posttest) effects of treatment, we conducted a 3 (Group: WL, CBGT, EGT) × 2 (Time: pre- vs. posttest) repeated measures multivariate analysis of variance, (dependent variables: SPAI, log-transformed length of speech duration,2 and SCQ). The results (Wilks’s lambda) showed a significant effect of time, F(3, 76) = 22.92, p < .0001, η2 = 0.48, and Group × Time, F(6, 152) = 5.07, p < .0001, η2 = 0.17. The group effect was not statistically significant, F(6, 152) = 0.24, p > .2, η2 = 0.05. Similar results were found when including age as a covariate into the analysis. The results of this multivariate analysis of covariance (Wilks’s lambda) showed again a significant effect of time, F(3, 75) = 3.92, p < .02, η2 = 0.14, and Group × Time, F(6, 150) = 4.78, p < .0001, η2 = 0.16. The group effect, F(6, 150) = 1.26, p > .2, η2 = 0.05; age effect, F(3, 75) = 1.06, p > .3, η2 = 0.04, and time × age interaction effect, F(3, 75) = 1.58, p > .2, η2 = 0.06, were not statistically significant. As a result of missing data, the number of participants per group for these analyses ranged between 27 and 30.
To estimate the magnitude of the treatment effects, we further calculated Smith and Glass’s (1977)d[(MWL/post − MTx/post)/SDWL/post] for the two treatment conditions. The CBGT group showed a moderate reduction in SPAI scores (d = .72), a moderate increase in speech duration (d = 0.50), and a large reduction in the SCQ scores (d = 0.92). Similarly, the EGT group showed a moderate reduction in the SPAI (d = 0.52) and a moderate increase in the speech duration (d = 0.57). The reduction in the SCQ scores was moderately strong (d = 0.49). Figure 1 shows the means of the SPAI (social phobia subscale) scores of the three groups at pretest and posttest. In addition, the figure includes the results of the 6-month follow-up assessments, which are reported further below.
Figure 1.
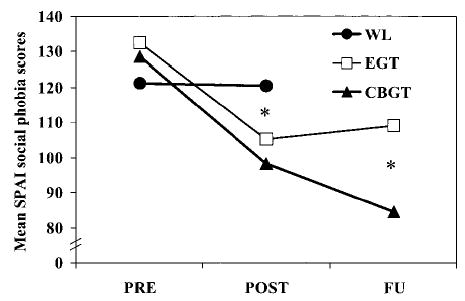
Social phobia subscale scores of the Social Phobia and Anxiety Inventory (SPAI; Turner et al., 1989) at pretest (PRE), posttest (POST), and 6-month follow-up assessment (FU) reported by participants from the wait-list control group (WL), exposure group therapy (EGT), and cognitive-behavioral group therapy (CBGT). The asterisks signify statistically significant differences among groups ( p < .05).
Orthogonal sets of linear contrasts showed that the two treatment groups had significantly lower scores in the SCQ and SPAI, and spoke for longer than the wait-list control group at posttest (all ps < .05). However, the two treatment groups did not differ in any of these variables at posttest (all ps > .1). Moreover, the three groups showed no difference in these variables at pretest (all ps >.1). These data indicate that the two treatments were similarly effective in reducing social anxiety and estimated social cost, and in increasing speaking time.
Similar results were found when comparing the three groups in the number of individuals who terminated the speech task prematurely (i.e., before the 10 min were over). The three groups showed no difference in the termination rate at pretest, χ2(2, N = 90) = 0.95, p > .9. On average, 61.1% of participants terminated the speech task prematurely at pretest. However, more participants from the WL group terminated the speech task at posttest (66.7%) than participants who received EGT (46.7%) and CBGT (33.3%), χ2(2, N = 90) = 6.76, p < .04.
Longer Term Treatment Effects
Participants who received either CBGT or EGT were assessed a third time 6 months after the posttest assessment. Individuals from the WL group received treatment after the waiting period and were therefore not included in the analyses of the long-term effects. The results of a 2 (Group: CBGT vs. EGT) × 2 (Time: pretest vs. 6-month follow-up) repeated measure analysis of variance with the SPAI (social phobia subscale) scores as the dependent variable showed a significant effect of time, F(1, 35) = 64.54, p < .0001, η2 = 0.65; and Group × Time, F(1, 35) = 6.65, p < .02, η2 = 0.16. The group effect was not statistically significant, F(1, 35) = 1.97, p > .17, η2 = 0.05. The results of an analysis of covariance with age as a covariate, group as the between-subjects factor, and time (post vs. 6-month follow-up) as the within-subjects factor, showed again a significant Group × Time interaction effect, F(1, 34) = 6.78, p < .02, η2 = 0.17. The time effect, F(1, 34) = 2.82, p > .102, η2 = 0.08; age effect, F(1, 34) = 1.88, p > .108, η2 = 0.05, and Time × Age interaction effect, F(1, 34) = .27, p > .6, η2 = 0.01, were not statistically significant. As shown in Figure 1, only participants who received CBGT showed continued improvement after treatment was terminated, which resulted in lower SPAI scores in the CBGT group than in the EGT group at follow-up ( p < .04). To compare the magnitude of change between the two treatments from pretest to the 6-month follow-up, we calculated uncontrolled effect sizes for each treatment modality using the formula: (Mpre − MFU)/SDpre. This effect size was 0.68 for EGT and 1.55 for CBGT.
Mediation Analyses
Kraemer et al. (2002) suggested using a linear model to compare a treatment group (T) with a control group (C). The independent variables of this model are T, M (the possible mediator), and the T × M interaction. To show that M is a mediator of treatment, M would have to measure a change occurring during treatment, must correlate with treatment group membership, and have either a main or interactive effect on the outcome. Following these recommendations, we examined the linear models comparing each of the two treatments (coded +1/2) with the wait-list control condition (coded − 1/2) using group membership, the centered pre–post changes in the hypothesized mediator, and the interaction between the changes in the proposed mediator and group membership as the independent variables. Table 1 shows the results of the linear regression analyses with group membership, the centered pre–post difference scores of the SCQ (SCQDIF, CTR), and the interaction term as the predictor variables. The dependent variables of the regression analyses were the pre–post difference scores of the social phobia subscale of the SPAI (SPAIDIF). The findings revealed a significant group effect and a significant main effect on outcome, which is consistent with the conjectured mediation model.3 However, a simple pre–post comparison does not allow for testing of temporal precedence of the proposed mediator compared with the dependent variable. To examine this mediation criterion, we therefore conducted additional analyses using the follow-up assessment data. Complete 6-month follow-up data were available from 20 individuals who completed EGT and 17 individuals who completed CBGT. These analyses deviate from the Kraemer et al. (2002) proposed test for mediation in randomized controlled trials because follow-up data were only available from participants who completed either of the two treatment groups of the study (individuals from the WL group received treatment after the posttest assessment).
Table 1.
Linear Regression Analyses for Testing SCQ as a Mediator of Treatment Change in Social Anxiety
| Comparison and predictor | B | SE B | β |
|---|---|---|---|
| EGT vs. WLa | |||
| Group | 20.55 | 8.21 | 0.34* |
| SCQDIF, CTR | 0.52 | 0.18 | 0.38* |
| SCQDIF, CTR × Group | 0.42 | 0.36 | 0.14 |
| Intercept | 12.87** | 4.10 | |
| CBGT vs. WLb | |||
| Group | 22.60 | 8.89 | 0.34* |
| SCQDIF, CTR | 0.45 | 0.18 | 0.38* |
| SCQDIF, CTR × Group | 0.27 | 0.36 | 0.11 |
| Intercept | 13.89** | 4.45 | |
Note. n = 30 per group. The dependent variable of the analyses is the pre–post difference scores in the social phobia subscale of the Social Phobia and Anxiety Inventory (Turner et al., 1989). The predictors are the group effect (Group; coded + .5 for individuals in the treatment groups and − .5 for those in the WL group), the centered pre–post difference score of the SCQ (SCQDIF, CTR), and the interaction term, SCQDIF, CTR × Group. SCQ = Social Cost Questionnaire; EGT = exposure group therapy; WL = wait-list control group; CBGT = cognitive–behavioral group therapy.
EGT vs. WL: R2 = .40, R2 (adjusted) = .37, R = .64, p < .0001.
CBGT vs. WL: R2 = .41, R2 (adjusted) = .37, R = .64, p < .0001.
p < .05.
p < .005.
To examine the extent to which treatment changes in estimated social cost influence later changes in social anxiety, we correlated the residual gain scores of SCQ scores from the pretest to the posttest with the residual gain scores of the SPAI scores from the pretest to the 6-month follow-up interval. Residual gain scores control for initial differences between individuals and measurement error inherent in the use of repeated measures on the same instrument (Beutler & Hamblin, 1986; Manning & DuBois, 1962; Mintz, Luborsky, & Christoph, 1979; Steketee & Chambless, 1992). Specifically, the residual gain scores of the SCQ (RGSCQ) were calculated by subtracting the standardized pretest scores (zSCQ/pre), multiplied by the correlation between the standardized scores at pretest and posttest, r(SCQ/pre × SCQ/post), from the posttest scores (zSCQ/post): RGSCQ = zSCQ/post − zSCQ/pre × r(SCQ/pre × SCQ/post).
To examine whether these pre–post changes in estimated social cost are associated with long-term (pretest to 6-month follow-up) changes in social anxiety, we correlated RGSCQ scores with the residual gain scores of the SPAI from pretest to 6-month follow-up (RGSPAI). This latter variable was calculated by subtracting the standardized pretest SPAI scores (zSPAI/pre), multiplied by the correlation between the standardized scores at pretest and at 6-month follow-up (r[SPAI/pre × SPAI/6mFU]) from the 6-month follow-up scores (zSPAI/6mFU): RGSPAI = zSPAI/6moFU − zSPAI/pre × r[SPAI/pre × SPAI/6moFU].
The results showed that the Pearson correlation coefficient between the two residual gain scores (RGSPAI and RGSCQ) was .60 ( p < .02) in the CBGT group (n = 17) and .42 ( p > .06) in the EGT group (n = 20). The difference between the correlation coefficients in the two treatment groups (using Fisher Z-transformation) was not statistically significant, z = 0.68, p > .2.
Discussion
Cognitive-behavioral therapy, such as Heimberg’s CBGT, is an effective intervention for social phobia as already demonstrated in a number of previous studies (Heimberg et al., 1990, 1998; Heimberg, Salzman, Holt, & Blendell, 1993). Another effective form of intervention is exposure therapy without any explicit cognitive intervention (Feske & Chambless, 1995; Gould et al., 1997; Taylor, 1996). Despite the demonstrated efficacy of these interventions, very little is known about the underlying variables that lead to treatment change (Hofmann, 2000b). What mediates changes in these treatment modalities, and are those changes unique to a particular type of intervention? The cognitive model of social phobia predicts that estimated social cost is an important mediator of treatment change (Clark & Wells, 1995; Foa et al., 1996; Rapee & Heimberg, 1997). Furthermore, an intervention that specifically targets cognitions to reduce the patients’ overestimation of social cost should be more effective than a treatment that does not directly target cognitions. To test these hypotheses, we compared CBGT, EGT without explicit cognitive interventions, and a wait-list control group in their effects of changes in estimated social cost on changes in social anxiety. We measured estimated social cost with the Foa et al. SCQ (1996) and applied some of the Kraemer et al. (2002) recent recommendations to examine mediation.
The two treatments did not significantly differ at posttreatment but were significantly more effective than the wait-list control group. These results are consistent with previous studies that reported no significant differences between exposure therapy and cognitive-behavioral therapy at posttest (Emmelkamp et al., 1985; Gelernter et al., 1991; Hope, Heimberg, & Bruch, 1995; Mattick et al., 1989; Scholing & Emmelkamp, 1993a, 1993b). However, an examination of the effect sizes tends to favor CBGT over EGT in some measures. Specifically, CBGT was associated with a moderate reduction in the SPAI (d = 0.72) and a large reduction in the SCQ (d = 0.92) from pre- to posttest. In contrast, EGT was associated with a slightly weaker reduction in the SPAI (d = 0.52) and only a moderate reduction in SCQ scores (d = 0.49) from pre-to posttest. Although not statistically significant, slightly more participants prematurely terminated the speech task after EGT (46.7%) than CBGT (33.3%) at posttest. The difference between the treatment groups in self-reported social anxiety became significant at the 6-month follow-up. The effect size of the reduction of SPAI scores from pretest to the 6-month follow-up was 0.68 and 1.55 for the EGT and CBGT group, respectively. These findings support the notion that treatments that are directly aimed at changing dysfunctional cognitions have a more lasting effect on social anxiety (e.g., Butler, 1985; Butler et al., 1984; Stopa & Clark, 1993). It should be noted that the EGT protocol was developed by Stefan G. Hofmann and successfully applied in a number of previous trials (Hofmann, 2000a; Hofmann et al., 1995; Newman et al., 1994). An earlier version of the EGT protocol was further included in three meta-analyses (Feske & Chambless, 1995; Gould et al., 1997; Taylor, 1996), which reported that it was comparable in its efficacy to other interventions, including CBGT. Therefore, experimenter biases, such as expectancy and allegiance effects, are unlikely to explain the outcome of the present study. Nevertheless, the findings of the follow-up data have to be interpreted with caution given the fairly high attrition rate.
Consistent with the proposed mediation model, estimated social cost correlated with treatment choice and had a main effect on outcome in both treatment modalities. These findings support the notion that changes in estimated social cost may be an important mediator of treatment change, as suggested by Clark and Wells’s (1995) cognitive model of social phobia. To further examine the temporal relationship between changes in estimated social cost and social anxiety, we correlated the pre–post residual gain scores in estimated social cost with the residual gain scores in social anxiety from pretest to the 6-month follow-up assessment. The short-term (pre–post) changes in estimated social cost significantly correlated with the long-term (pre- to 6-month follow-up) changes in social anxiety among individuals receiving CBGT (r = .60), but not among those receiving EGT (r = .42). However, the difference between these two correlation coefficients was not statistically significant. These findings suggest that early changes in estimated social cost are associated with later changes in social anxiety among participants receiving CBGT, which is consistent with the proposed mediation model. A similar but smaller effect was found for the EGT group. It should be noted, however, that the number of participants with 6-month follow-up data was relatively small, which might have been the reason why the correlation between pre–post changes in estimated social cost and later changes in social anxiety only reached statistical significance among individuals who received CBGT.
On the basis of these findings, one might hypothesize that repeated exposure to feared social situations in the absence of negative consequences inadvertently forces individuals to reevaluate certain dysfunctional cognitions, including the cognitive biases that lead to the overestimation of social cost. This is consistent with an earlier study that reported changes in cognitions during the course of a behavioral treatment without explicit cognitive strategies (Newman et al., 1994). Psychotherapy is a complex and interactive process to promote change in clients through means of communication. Therefore, measures of treatment integrity, which only examine the delivery aspect of treatment, are unable to capture the full process of therapy, especially the part of treatment that is actually received by the client. Future studies that compare different treatment modalities should therefore attempt to capture both aspects of therapy.
An important limitation of the present study is related to the nature of the two treatments. The EGT protocol was specifically developed as a treatment for social phobia without any explicit cognitive interventions. However, EGT was not simply a reduced version of the CBGT protocol. In addition to the difference in the emphasis on cognitive strategies, the two protocols also differed in the treatment rationale, which was based on the cognitive model of anxiety in the case of CBGT and on a basic habituation rationale in the case of EGT. Another important limitation is related to the external validity of the results. Some studies suggest that substance use disorder, especially alcohol abuse, may be functionally related to social anxiety in some people (e.g., Carrigan & Randall, 2003). However, neither of the two therapy protocols provided specific guidelines for the treatment management of those cases. Therefore, similar to other clinical trials (e.g., Heimberg et al., 1998), individuals with current substance use problems were excluded from the study. Furthermore, only individuals with at least moderate public speaking anxiety were eligible to participate in the study. The majority (89.9%) of all people who presented at the center for treatment were eligible to participate in this study (and reported significant public speaking anxiety). Nevertheless, it remains uncertain whether changes in estimated social cost would have also mediated treatment changes in individuals who were excluded from the study. Further, the study design was less than ideal to examine the temporal precedence criterion of mediation (Kraemer et al., 2002). Multiple assessments during the course of treatment or even session-by-session assessments of the proposed mediator and the dependent variable would have provided data for a finer analysis of the temporal relationship between these variables. Newer statistical procedures (e.g., hierarchical linear modeling) can examine treatment changes in a combined sample of treatment completers and treatment dropouts when conducting multiple assessments throughout treatment. Finally, there was a small and nonsignificant age difference among the three groups. Participants in the CBGT group tended to be younger than the rest of the sample. However, the effects of the experimental manipulation on the proposed mediator and the dependent variable were not affected when considering age as a possible covariate. Furthermore, age was not a significant covariate in these analyses.
Despite these limitations, this study provides evidence for the role of estimated social cost as a mediator of treatment change in cognitive–behavioral therapy and provides support for the cognitive model of social phobia. Furthermore, the results suggest that cognitive-behavioral therapy leads to more lasting treatment changes than exposure therapy without explicit cognitive interventions, possibly because of the relatively greater influence cognitive–behavioral therapy has on cognitive errors related to overestimation of social cost.
Acknowledgments
This research was supported by National Institute of Mental Health (NIMH) Grant MH-57326. Part of these results were presented at the NIMH workshop Psychotherapeutic Interventions: How and Why They Work (December 9–10, 2001). We thank Helena C. Kraemer for her statistical advice and Harlan Juster for providing supervision to some of the therapists.
Footnotes
The estimated effects of treatment completers are most likely to be higher than the treatment effects that are based on intent-to-treat analyses. However, our primary objective was to examine mediation of treatment change rather than to demonstrate superiority of one treatment over the other. For examination of treatment mediation with the currently available statistical methods, it is necessary to study changes in the dependent variable and the proposed mediator over the same time interval(s) for all participants (Kraemer et al., 2002). Otherwise, it would be problematic to combine all participants in the same analysis. Therefore, the mediation analyses following Kraemer et al.’s recommendations are necessarily restricted to participants who completed the treatment or wait-list period.
The distribution of the speech durations deviated from normality, but a logarithmic transformation [log 10 (speech duration + 1)] was successful to normalize the data.
We conducted additional analyses with the nonsocial events subscale of the SCQ to examine the possible role of nonsocial cost estimates as a potential treatment mediator. The results of these analyses showed that the centered pre–post difference scores of this subscale did not predict group membership when comparing EGT with WL, β= − .11, p > .3; or CBGT with WL, β= − .01, p > .9. Given these results and the objective of this study, no further mediation analyses of this subscale are reported here.
References
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Borden JW, Turner SM, Jacob RG. The Social Phobia and Anxiety Inventory: Concurrent validity with a clinic sample. Behaviour Research and Therapy. 1989;27:573–576. doi: 10.1016/0005-7967(89)90093-4. [DOI] [PubMed] [Google Scholar]
- Beutler LE, Hamblin DL. Individualized outcome measures of internal change: Methodological considerations. Journal of Consulting and Clinical Psychology. 1986;23:305–310. doi: 10.1037//0022-006x.54.1.48. [DOI] [PubMed] [Google Scholar]
- Brown TA, DiNardo PA, Lehman CL, Campbell LA. Reliability of DSM–IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Butler G. Exposure and treatment of social phobia: Some instructive difficulties. Behaviour Research and Therapy. 1985;23:651–657. doi: 10.1016/0005-7967(85)90060-9. [DOI] [PubMed] [Google Scholar]
- Butler G, Cullington A, Munby M, Amies P, Gelder M. Exposure and anxiety management in the treatment of social phobia. Journal of Consulting and Clinical Psychology. 1984;52:642–650. doi: 10.1037//0022-006x.52.4.642. [DOI] [PubMed] [Google Scholar]
- Carrigan MH, Randall CL. Self-medication in social phobia. A review of the alcohol literature. Addictive Behavior. 2003;28:269–284. doi: 10.1016/s0306-4603(01)00235-0. [DOI] [PubMed] [Google Scholar]
- Clark DM, Ehlers A, McManus F, Hackman A, Fennell M, Campbell H, et al. Cognitive therapy versus fluoxetine in generalized social phobia: A randomized placebo-controlled trial. Journal of Consulting and Clinical Psychology. 2003;71:1058–1067. doi: 10.1037/0022-006X.71.6.1058. [DOI] [PubMed] [Google Scholar]
- Clark, D. M., & Wells, A. (1995). A cognitive model of social phobia. In R. G. Heimberg, M. R. Liebowitz, D. A. Hope, & F. R. Schneier (Eds.), Social phobia: Diagnosis, assessment and treatment (pp. 69–93). New York: Guilford Press.
- DiNardo, P. A., Brown, T. A., & Barlow, D. H. (1994). Anxiety disorders interview schedule for DSM–IV: Lifetime version (ADIS-IV-L). San Antonio, TX: Psychological Corporation/Graywind Publications.
- Emmelkamp PMG, Mersch PP, Vissia E, van der Helm M. Social phobia: A comparative evaluation of cognitive and behavioral interventions. Behaviour Research and Therapy. 1985;23:365–369. doi: 10.1016/0005-7967(85)90015-4. [DOI] [PubMed] [Google Scholar]
- Feske U, Chambless DL. Cognitive behavioral versus exposure only treatment for social phobia: A meta-analysis. Behavior Therapy. 1995;26:695–720. [Google Scholar]
- Foa EB, Franklin ME, Perry KJ, Herbert JD. Cognitive biases in generalized social phobia. Journal of Abnormal Psychology. 1996;105:433–439. [PubMed] [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Gelernter CS, Uhde TW, Cimbolic P, Arnkoff DB, Vittone BJ, Tancer ME, Bartko JJ. Cognitive–behavioral and pharmacological treatments of social phobia. Archives of General Psychiatry. 1991;48:938–945. doi: 10.1001/archpsyc.1991.01810340070009. [DOI] [PubMed] [Google Scholar]
- Gould RA, Buckminster S, Pollack MH, Otto MW, Yap L. Cognitive–behavioral and pharmacological treatment for social phobia: A meta-analysis. Clinical Psychology: Science and Practice. 1997;4:291–306. [Google Scholar]
- Heimberg, R. G. (1991). Cognitive–behavioral treatment of social phobia in a group setting: A treatment manual. Unpublished manuscript, State University of New York at Albany.
- Heimberg RG, Dodge CS, Hope DA, Kennedy CR, Zollo L, Becker RE. Cognitive-behavioral treatment for social phobia: Comparison with credible placebo control. Cognitive Therapy and Research. 1990;14:1–23. [Google Scholar]
- Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, Holt CS, Welkowitz LA, et al. Cognitive-behavioral group therapy vs. phenelzine therapy for social phobia: 12-week outcome. Archives of General Psychiatry. 1998;55:1133–1141. doi: 10.1001/archpsyc.55.12.1133. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Salzman D, Holt CS, Blendell K. Cognitive-behavioral group treatment for social phobia: Effectiveness at five year follow-up. Cognitive Therapy and Research. 1993;17:325–340. [Google Scholar]
- Hofmann SG. Self-focused attention before and after treatment of social phobia. Behaviour Research and Therapy. 2000a;38:717–725. doi: 10.1016/s0005-7967(99)00105-9. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Treatment of social phobia: Potential mediators and moderators. Clinical Psychology: Science and Practice. 2000b;7:3–16. doi: 10.1093/clipsy/7.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Newman MG, Becker E, Taylor CB, Roth WT. Social phobia with and without avoidant personality disorder: Preliminary behavior therapy outcome findings. Journal of Anxiety Disorders. 1995;9:427–438. [Google Scholar]
- Hope DA, Heimberg RG, Bruch MA. Dismantling cognitive-behavioral group therapy for social phobia. Behaviour Research and Therapy. 1995;33:637–650. doi: 10.1016/0005-7967(95)00013-n. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Shanyang Z, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson T, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Manning WH, DuBois PH. Correlational methods in research on human learning. Perceptual and Motor Skills. 1962;15:287–321. doi: 10.2466/pms.1963.16.3.831. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Peters L. Treatment of severe social phobia: Effects of guided exposure with and without cognitive restructuring. Journal of Consulting and Clinical Psychology. 1988;56:251–260. doi: 10.1037//0022-006x.56.2.251. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Peters L, Clark JC. Exposure and cognitive restructuring for social phobia: A controlled study. Behavior Therapy. 1989;20:3–23. [Google Scholar]
- Mintz J, Luborsky L, Christoph P. Measuring the outcomes of psychotherapy: Findings of the Penn psychotherapy project. Journal of Consulting and Clinical Psychology. 1979;47:319–334. doi: 10.1037//0022-006x.47.2.319. [DOI] [PubMed] [Google Scholar]
- Newman MG, Hofmann SG, Trabert W, Roth WT, Taylor CB. Does behavioral treatment of social phobia lead to cognitive changes? Behavior Therapy. 1994;25:503–517. [Google Scholar]
- O’Malley SS, Suh CS, Strupp HH. The Vanderbilt Psychotherapy Process Scale: A report on the scale development and a process–outcome study. Journal of Consulting and Clinical Psychology. 1983;51:581–586. doi: 10.1037//0022-006x.51.4.581. [DOI] [PubMed] [Google Scholar]
- Rapee RN, Heimberg RG. A cognitive–behavioral model of anxiety in social phobia. Behaviour Research and Therapy. 1997;35:741–756. doi: 10.1016/s0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Scholing A, Emmelkamp PMG. Cognitive and behavioural treatments of fear of blushing, sweating or trembling. Behaviour Research and Therapy. 1993a;31:155–170. doi: 10.1016/0005-7967(93)90067-5. [DOI] [PubMed] [Google Scholar]
- Scholing A, Emmelkamp PMG. Exposure with and without cognitive therapy for generalized social phobia: Effects of individual and group therapy. Behaviour Research and Therapy. 1993b;31:667–681. doi: 10.1016/0005-7967(93)90120-j. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Smith ML, Glass GV. Meta-analysis in psychotherapy outcome studies. American Psychologist. 1977;32:752–760. doi: 10.1037//0003-066x.32.9.752. [DOI] [PubMed] [Google Scholar]
- Steketee GS, Chambless DL. Methodological issues in the prediction of treatment outcome. Clinical Psychology Review. 1992;12:387–400. [Google Scholar]
- Stopa L, Clark DM. Cognitive processes in social phobia. Behaviour Research and Therapy. 1993;31:255–267. doi: 10.1016/0005-7967(93)90024-o. [DOI] [PubMed] [Google Scholar]
- Suh, C. S., Strupp, H. H., & O’Malley, S. S. (1986). The Vanderbilt process measure: The Psychotherapy Process Scale (VPPS) and the Negative Indicators Scale (VNIS). In L. S. Greenberg & William W. Pinsof (Eds.), The therapeutic process: A research handbook (pp. 285–323). New York: Guilford Publications.
- Taylor S. Meta-analysis of cognitive-behavioral treatments for social phobia. Journal of Behaviour Therapy and Experimental Psychiatry. 1996;27:1–9. doi: 10.1016/0005-7916(95)00058-5. [DOI] [PubMed] [Google Scholar]
- Turner SM, Beidel DC, Dancu CV, Stanley MA. An empirically derived inventory to measure social fears and anxiety: The Social Phobia and Anxiety Inventory. Psychological Assessment. 1989;1:35–40. [Google Scholar]
- Waltz J, Addis MF, Koerner K, Jacobson NS. Testing the integrity of a psychotherapy protocol: Assessment of adherence and competence. Journal of Consulting and Clinical Psychology. 1993;61:620–630. doi: 10.1037//0022-006x.61.4.620. [DOI] [PubMed] [Google Scholar]
- Windholz MJ, Silberschatz G. Vanderbilt Psychotherapy Process Scale: A replication with adult outpatients. Journal of Consulting and Clinical Psychology. 1988;56:56–60. doi: 10.1037//0022-006x.56.1.56. [DOI] [PubMed] [Google Scholar]


