Investigators in the field of urology, oncology, and pathology have been attempting to unravel the mystery of early diagnosis, treatment, and monitoring of men with prostate cancer for several decades. Recently a great deal of attention has been focused on obtaining a better understanding, both pathologically as well as clinically, of the pre-malignant lesion of prostatic intraepithelial neoplasia. Although not diagnostic of prostate cancer on a needle biopsy, many morphologic, molecular, histopathological, epidemiological, and genetic studies have offered strong evidence that high-grade prostatic intraepithelial neoplasia (HGPIN) is in fact a precursor lesion to development of invasive prostatic adenocarcinoma. Early studies in the literature that first characterized this relationship suggested that histologic evidence of HGPIN on a prostate biopsy predicted a nearly 50% risk of finding prostate cancer on a subsequent prostate biopsy. Through the years, much larger, prospective, population-based studies have suggested that this likelihood is more in the range of 25% to 30%. Knowing that the likelihood of finding prostate cancer after a “negative prostate biopsy” ranges between 10% and 25% if a repeat biopsy were performed brings into question the need or clinical utility of recommending immediate repeat prostate biopsy when HGPIN is seen on initial prostate biopsy.
Kronz and associates from the Department of Pathology at the Johns Hopkins Hospital in Baltimore, Maryland have recently published their work investigating how various HGPIN-related factors other than clinical and pathological variables can be used for cancer prediction following an initial diagnosis of HGPIN on a needle biopsy. This important research, published in The American Journal of Surgical Pathology this year, should be required reading for all urologists performing and interpreting the results of prostate needle biopsies within their practice.
Predicting Cancer Following a Diagnosis of High-Grade Prostatic Intraepithelial Neoplasia on Needle Biopsy: Data on Men with More than One Follow-Up Biopsy
Kronz JD, Allan CH, Shaikh AA, Epstein JI.
Am J Surg Pathol. 2001;25:1079–1085.
Kronz, Epstein, and colleagues questioned the dogma of the need for repeat prostate biopsy following an initial diagnosis of HGPIN. In their retrospective analysis of 245 men in whom the only abnormal finding on the initial prostate biopsy was HGPIN and who had at least one follow-up biopsy, they found that repeat prostate biopsy identified cancer in 32.2% of the men overall. In men in whom only one follow-up biopsy had been performed, only 24.5% of the men were found to have cancer. The only independent histologic predictor of prostate cancer diagnosis on a subsequent biopsy was “the number of cores with HGPIN.” The risk of prostate cancer increased as the number of cores found to have HGPIN on the initial biopsy increased. Those men with 1 to 2 cores had a 30% chance of having cancer on a subsequent biopsy, whereas men with 3 or more than 3 cores with a diagnosis of HGPIN had a 40% and 75% chance of having cancer on a subsequent biopsy, respectively (see Figure 1). Several variables (eg, number of HGPIN glands, maximum percentage of glands involved by HGPIN, nucleolar prominence, percentage of cells with prominent nucleoli, pattern of high HGPIN, digital rectal examination findings, transrectal ultrasound findings, family history of prostate cancer, prostate-specific antigen [PSA] levels at the time of initial prostate biopsy, and the rate of change in serum PSA) demonstrated no predictive value in whether or not a subsequent prostate biopsy would have cancer. The authors conclude that HGPIN does in fact carry with it a clinically significant likelihood of finding cancer in a subsequent prostate biopsy (30% overall), and that with increasing number of cores with HGPIN the likelihood of finding prostate cancer increases (to as much as 75% when more than three cores are found to have this histologic abnormality). They also caution that if cancer is not found on the first two follow-up biopsies after the initial diagnosis of HGPIN, it is unlikely that cancer will be found with subsequent biopsies, and the patient should be followed appropriately with yearly exams and PSA testing. Figure 1 graphically demonstrates the likelihood of having prostate cancer on a subsequent biopsy for all cases within this study, as well as those cases in which multiple prostate biopsies were performed after the initial diagnosis of HGPIN.
Figure 1.
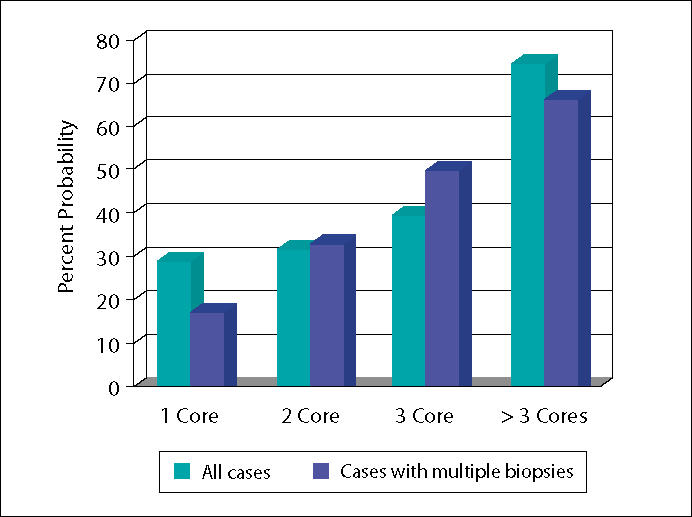
Risk of cancer on subsequent biopsy by number of cores with high-grade prostatic intraepithelial neoplasia. Data from Konz JD, Allen CH, Shaikh AA, Epstein JI. Predicting cancer following a diagnosis of high-grade prostatic intraepithelial neoplasia on needle biopsy. Am J Surg Pathol. 2000;25:1079–1085.
This study highlights the importance of recognizing HGPIN on prostate biopsies and the associated risk of finding adenocarcinoma on subsequent biopsies, which ranges between 30% and 75%, depending on how much HGPIN was seen on the initial biopsy. These results should be analyzed keeping in mind the known false-negative prostate biopsy rates, which can range between 10% and 25%, depending on the number of cores and the biopsy template used. In summary, although the finding of HGPIN places an individual man at a higher risk of having cancer on subsequent biopsy than if the biopsy were benign, the increased risk overall is only 30% and not that much different than the risk of finding prostate cancer on a repeat biopsy if his biopsy were benign (in some studies it is as great as 25%). Additional factors are obviously needed to completely determine if there are subgroups of men with HGPIN who are clearly at a higher risk for subsequent diagnosis of prostate cancer, requiring immediate repeat prostate biopsy. This important study was the first to document that the volume of HGPIN (eg, number of cores involved) carries with it important risk stratification information. If these findings are validated in future prospective and/or multiinstitutional studies, a more rational re-biopsy strategy for men with HGPIN on additional prostate biopsy may be needed.


